The Antibacterial and Remineralizing Effects of Biomaterials Combined with DMAHDM Nanocomposite: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Search Strategy and Study Selection
2.3. Data Extraction
2.4. Risk of Bias in the Included Studies
3. Results
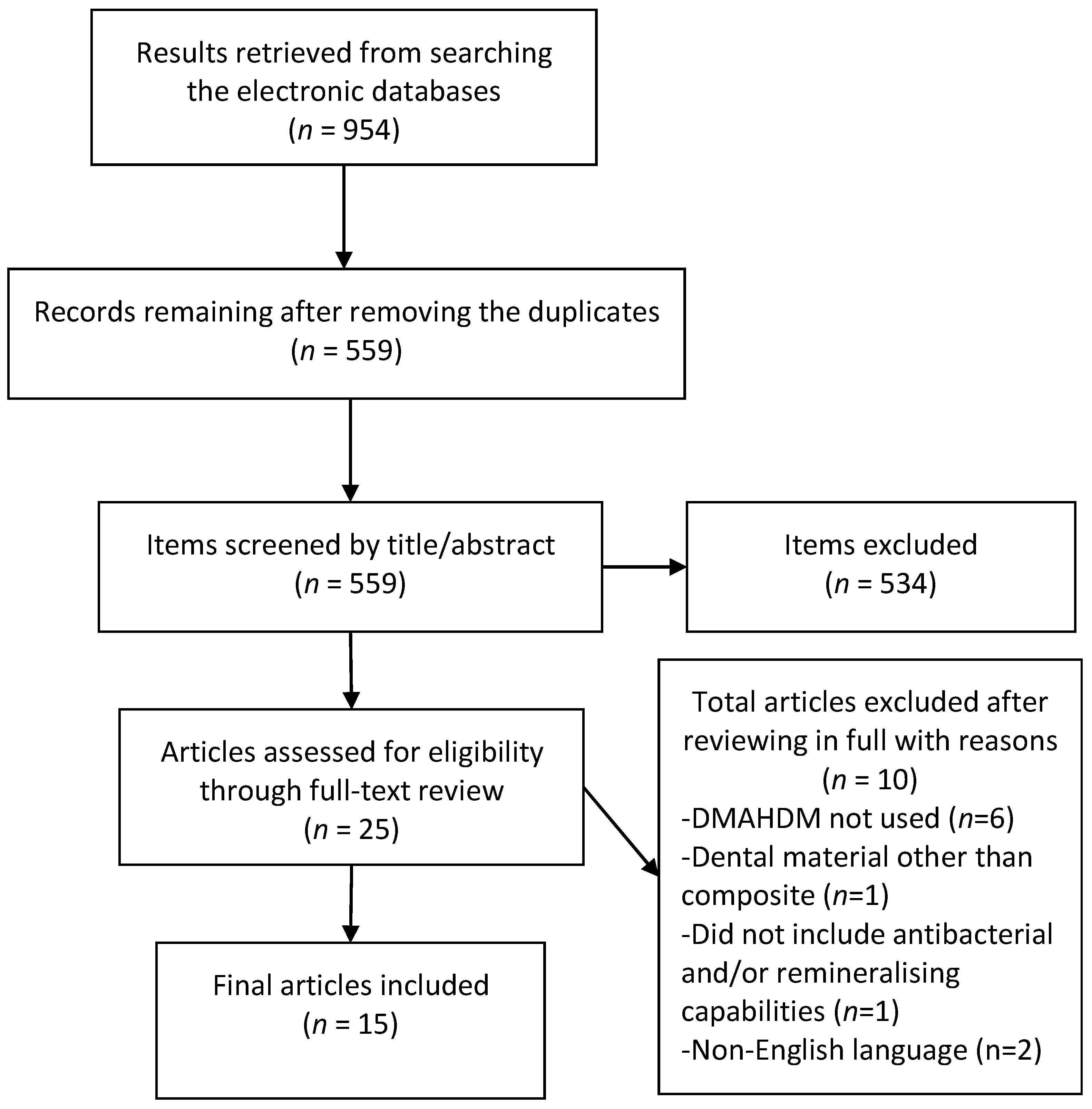
3.1. Study Selection
3.2. Study Characteristics
3.3. Risk of Bias
3.4. Antibacterial Results
3.4.1. Live/Dead Staining
3.4.2. CFU Counts
3.4.3. MTT Metabolic Assays
3.4.4. Lactic Acid Production
3.4.5. Protein Adsorption
3.4.6. Polysaccharide Production
3.4.7. Other Results
3.5. Remineralization Results
3.5.1. Calcium and Phosphate Ion Release
3.5.2. Other Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Al-Dulaijan, Y.A.; Cheng, L.; Weir, M.D.; Melo, M.A.S.; Liu, H.; Oates, T.W.; Wang, L.; Xu, H.H.K. Novel rechargeable calcium phosphate nanocomposite with antibacterial activity to suppress biofilm acids and dental caries. J. Dent. 2018, 72, 44–52. [Google Scholar] [CrossRef]
- Bhadila, G.; Baras, B.H.; Weir, M.D.; Wang, H.; Melo, M.A.S.; Hack, G.D.; Bai, Y.; Xu, H.H.K. Novel antibacterial calcium phosphate nanocomposite with long-term ion recharge and re-release to inhibit caries. Dent. Mater. J. 2020, 4, 678–689. [Google Scholar] [CrossRef]
- Wang, W.; Zhu, S.; Zhang, G.; Wu, F.; Ban, J.; Wang, L. Antibacterial and thermomechanical properties of experimental dental resins containing quaternary ammonium monomers with two or four methacrylate groups. RSC Adv. 2019, 9, 40681–40688. [Google Scholar] [CrossRef]
- Ferracane, J.L. Resin composite--state of the art. Dent. Mater. 2011, 27, 29–38. [Google Scholar] [CrossRef]
- Rasines Alcaraz, M.G.; Veitz-Keenan, A.; Sahrmann, P.; Schmidlin, P.R.; Davis, D.; Iheozor-Ejiofor, Z. Direct composite resin fillings versus amalgam fillings for permanent or adult posterior teeth. Cochrane Database Syst. Rev. 2014, 3. [Google Scholar] [CrossRef] [PubMed]
- Cheng, L.; Zhang, K.; Melo, M.A.S.; Weir, M.D.; Zhou, X.; Xu, H.H.K. Anti-biofilm dentin primer with quaternary ammonium and silver nanoparticles. J. Dent. Res. 2012, 91, 598–604. [Google Scholar] [CrossRef] [PubMed]
- Eltahlah, D.; Lynch, C.D.; Chadwick, B.L.; Blum, I.R.; Wilson, N.H.F. An update on the reasons for placement and replacement of direct restorations. J. Dent. 2018, 72, 1–7. [Google Scholar] [CrossRef]
- Xie, X.; Wang, L.; Xing, D.; Zhang, K.; Weir, M.D.; Liu, H.; Bai, Y.; Xu, H.H.K. Novel dental adhesive with triple benefits of calcium phosphate recharge, protein-repellent and antibacterial functions. Dent. Mater. 2017, 33, 553–563. [Google Scholar] [CrossRef] [PubMed]
- Askar, H.; Krois, J.; Göstemeyer, G.; Bottenberg, P.; Zero, D.; Banerjee, A.; Schwendicke, F. Secondary caries: What is it, and how it can be controlled, detected, and managed? Clin. Oral Investig. 2020, 24, 1869–1876. [Google Scholar] [CrossRef]
- Chrószcz, M.; Barszczewska-Rybarek, I. Nanoparticles of Quaternary Ammonium Polyethylenimine Derivatives for Application in Dental Materials. Polymers 2020, 12, 2551. [Google Scholar] [CrossRef]
- Xue, J.; Wang, J.; Feng, D.; Huang, H.; Wang, M. Application of Antimicrobial Polymers in the Development of Dental Resin Composite. Molecules 2020, 25, 4738. [Google Scholar] [CrossRef]
- Zhang, K.; Zhang, N.; Weir, M.D.; Reynolds, M.A.; Bai, Y.; Xu, H.H.K. Bioactive Dental Composites and Bonding Agents Having Remineralizing and Antibacterial Characteristics. Dent. Clin. N. Am. 2017, 61, 669–687. [Google Scholar] [CrossRef]
- Rego, G.F.; Vidal, M.L.; Viana, G.M.; Cabral, L.M.; Schneider, L.F.J.; Portela, M.B.; Cavalcante, L.M. Antibiofilm properties of model composites containing quaternary ammonium methacrylates after surface texture modification. Dent. Mater. 2017, 33, 1149–1156. [Google Scholar] [CrossRef]
- He, J.; Söderling, E.; Österblad, M.; Vallittu, P.K.; Lassila, L.V. Synthesis of methacrylate monomers with antibacterial effects against S. mutans. Molecules 2011, 16, 9755–9763. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Tang, Y.; Weir, M.D.; Gao, J.; Imazato, S.; Oates, T.W.; Lei, L.; Wang, S.; Hu, T.; Xu, H.H.K. Effects of S. mutans gene-modification and antibacterial monomer dimethylaminohexadecyl methacrylate on biofilm growth and acid production. Dent. Mater. 2020, 36, 296–309. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Weir, M.D.; Xu, H.H.K. Effects of quaternary ammonium chain length on antibacterial bonding agents. J. Dent. Res. 2013, 92, 932–938. [Google Scholar] [CrossRef]
- Makvandi, P.; Esposito Corcione, C.; Paladini, F.; Gallo, A.L.; Montagna, F.; Jamaledin, R.; Pollini, M.; Maffezzoli, A. Antimicrobial modified hydroxyapatite composite dental bite by stereolithography. Polym. Adv. Technol. 2018, 29, 364–371. [Google Scholar] [CrossRef]
- Zhou, H.; Li, F.; Weir, M.D.; Xu, H.H. Dental plaque microcosm response to bonding agents containing quaternary ammonium methacrylates with different chain lengths and charge densities. J. Dent. 2013, 41, 1122–1131. [Google Scholar] [CrossRef]
- Zhou, H.; Weir, M.D.; Antonucci, J.M.; Schumacher, G.E.; Zhou, X.D.; Xu, H.H.K. Evaluation of three-dimensional biofilms on antibacterial bonding agents containing novel quaternary ammonium methacrylates. Int. J. Oral Sci. 2014, 6, 77–86. [Google Scholar] [CrossRef]
- Zhang, K.; Cheng, L.; Weir, M.D.; Bai, Y.X.; Xu, H.H. Effects of quaternary ammonium chain length on the antibacterial and remineralizing effects of a calcium phosphate nanocomposite. Int. J. Oral Sci. 2016, 8, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Weir, M.D.; Chen, J.; Xu, H.H. Effect of charge density of bonding agent containing a new quaternary ammonium methacrylate on antibacterial and bonding properties. Dent. Mater. 2014, 30, 433–441. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.H.; Moreau, J.L.; Sun, L.; Chow, L.C. Nanocomposite containing amorphous calcium phosphate nanoparticles for caries inhibition. Dent. Mater. 2011, 27, 762–769. [Google Scholar] [CrossRef] [PubMed]
- Xiao, S.; Liang, K.; Weir, M.D.; Cheng, L.; Liu, H.; Zhou, X.; Ding, Y.; Xu, H.H.K. Combining Bioactive Multifunctional Dental Composite with PAMAM for Root Dentin Remineralization. Materials 2017, 10, 89. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Ferrando-magraner, E.; Bellot-arcís, C.; Paredes-gallardo, V.; Almerich-silla, J.M.; García-sanz, V.; Fernández-alonso, M.; Montiel-company, J.M. Antibacterial properties of nanoparticles in dental restorative materials. A systematic review and meta-analysis. Medicina 2020, 56, 55. [Google Scholar] [CrossRef] [PubMed]
- Sarkis-Onofre, R.; Skupien, J.; Cenci, M.; Moraes, R.; Pereira-Cenci, T. The role of resin cement on bond strength of glass-fiber posts luted into root canals: A systematic review and meta-analysis of in vitro studies. Oper. Dent. 2014, 39, E31–E44. [Google Scholar] [CrossRef]
- Beigi Burujeny, S.; Atai, M.; Yeganeh, H. Assessments of antibacterial and physico-mechanical properties for dental materials with chemically anchored quaternary ammonium moieties: Thiol-ene-methacrylate vs. conventional methacrylate system. Dent. Mater. 2015, 31, 244–261. [Google Scholar] [CrossRef] [PubMed]
- Zhou, C.; Weir, M.D.; Zhang, K.; Deng, D.; Cheng, L.; Xu, H.H. Synthesis of new antibacterial quaternary ammonium monomer for incorporation into CaP nanocomposite. Dent. Mater. 2013, 29, 859–870. [Google Scholar] [CrossRef]
- Cheng, L.; Weir, M.D.; Zhang, K.; Xu, S.M.; Chen, Q.; Zhou, X.; Xu, H.H. Antibacterial nanocomposite with calcium phosphate and quaternary ammonium. J. Dent. Res. 2012, 91, 460–466. [Google Scholar] [CrossRef]
- Wang, S.; Wang, H.; Ren, B.; Li, X.; Wang, L.; Zhou, H.; Weir, M.D.; Zhou, X.; Masri, R.M.; Oates, T.W.; et al. Drug resistance of oral bacteria to new antibacterial dental monomer dimethylaminohexadecyl methacrylate. Sci. Rep. 2018, 8, 5509. [Google Scholar] [CrossRef]
- Buruiana, T.; Melinte, V.; Popa, I.D.; Buruiana, E.C. New urethane oligodimethacrylates with quaternary alkylammonium for formulating dental composites. J. Mater. Sci. 2014, 25, 1183–1194. [Google Scholar] [CrossRef]
- Cheng, L.; Zhang, K.; Zhou, C.-C.; Weir, M.D.; Zhou, X.-D.; Xu, H.H.K. One-year water-ageing of calcium phosphate composite containing nano-silver and quaternary ammonium to inhibit biofilms. Int. J. Oral Sci. 2016, 8, 172–181. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Hu, X.; Ruan, J.; Arola, D.D.; Ji, C.; Weir, M.D.; Oates, T.W.; Chang, X.; Zhang, K.; Xu, H.H.K. Bonding durability, antibacterial activity and biofilm pH of novel adhesive containing antibacterial monomer and nanoparticles of amorphous calcium phosphate. J. Dent. 2019, 81, 91–101. [Google Scholar] [CrossRef] [PubMed]
- Campos, K.d.P.L.; Viana, G.M.; Cabral, L.M.; Portela, M.B.; Hirata Junior, R.; Cavalcante, L.M.; Lourenço, E.J.V.; Telles, D.d.M. Self-cured resin modified by quaternary ammonium methacrylates and chlorhexidine: Cytotoxicity, antimicrobial, physical, and mechanical properties. Dent. Mater. 2020, 36, 68–75. [Google Scholar] [CrossRef]
- Junling, W.; Qiang, Z.; Ruinan, S.; Ting, Z.; Jianhua, G.; Chuanjian, Z. Dental plaque microcosm biofilm behavior on a resin composite incorporated with nano-antibacterial inorganic filler containing long-chain alkyl quaternary ammonium salt. Hua Xi Kou Qiang Yi Xue Za Zhi. West China J. Stomatol. 2015, 33, 565–569. [Google Scholar] [CrossRef]
- Wu, J.; Zhang, Q.; Zhu, T.; Ge, J.; Zhou, C. Development of novel self-healing and antibacterial resin composite containing microcapsules filled with polymerizable healing monomer. Zhonghua Kou Qiang Yi Xue Za Zhi. Chin. J. Stomatol 2015, 50, 469–473. [Google Scholar]
- Wu, J.; Weir, M.D.; Melo, M.A.; Xu, H.H. Development of novel self-healing and antibacterial dental composite containing calcium phosphate nanoparticles. J. Dent. 2015, 43, 317–326. [Google Scholar] [CrossRef]
- Xiao, S.; Wang, H.; Liang, K.; Tay, F.; Weir, M.D.; Melo, M.A.S.; Wang, L.; Wu, Y.; Oates, T.W.; Ding, Y.; et al. Novel multifunctional nanocomposite for root caries restorations to inhibit periodontitis-related pathogens. J. Dent. 2019, 81, 17–26. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Zhou, H.; Weir, M.D.; Melo, M.A.; Levine, E.D.; Xu, H.H. Effect of dimethylaminohexadecyl methacrylate mass fraction on fracture toughness and antibacterial properties of CaP nanocomposite. J. Dent. 2015, 43, 1539–1546. [Google Scholar] [CrossRef]
- Zhang, N.; Ma, J.; Melo, M.A.; Weir, M.D.; Bai, Y.; Xu, H.H. Protein-repellent and antibacterial dental composite to inhibit biofilms and caries. J. Dent. 2015, 43, 225–234. [Google Scholar] [CrossRef]
- Melo, M.A.; Orrego, S.; Weir, M.D.; Xu, H.H.; Arola, D.D. Designing Multiagent Dental Materials for Enhanced Resistance to Biofilm Damage at the Bonded Interface. ACS Appl. Mater. Interfaces 2016, 8, 11779–11787. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Melo, M.A.; Weir, M.D.; Xie, X.; Reynolds, M.A.; Xu, H.H. Novel bioactive nanocomposite for Class-V restorations to inhibit periodontitis-related pathogens. Dent. Mater. 2016, 32, e351–e361. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Xie, X.; Imazato, S.; Weir, M.D.; Reynolds, M.A.; Xu, H.H. A protein-repellent and antibacterial nanocomposite for Class-V restorations to inhibit periodontitis-related pathogens. Mater. Sci. Eng. C Mater. Biol. Appl. 2016, 67, 702–710. [Google Scholar] [CrossRef]
- Xie, X.; Wang, L.; Xing, D.; Arola, D.D.; Weir, M.D.; Bai, Y.; Xu, H.H. Protein-repellent and antibacterial functions of a calcium phosphate rechargeable nanocomposite. J. Dent. 2016, 52, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Zhang, N.; Zhang, K.; Melo, M.A.; Weir, M.D.; Xu, D.J.; Bai, Y.; Xu, H.H. Effects of Long-Term Water-Aging on Novel Anti-Biofilm and Protein-Repellent Dental Composite. Int. J. Mol. Sci. 2017, 18, 186. [Google Scholar] [CrossRef]
- Wang, L.; Xie, X.; Qi, M.; Weir, M.D.; Reynolds, M.A.; Li, C.; Zhou, C.; Xu, H.H.K. Effects of single species versus multispecies periodontal biofilms on the antibacterial efficacy of a novel bioactive Class-V nanocomposite. Dent. Mater. 2019, 35, 847–861. [Google Scholar] [CrossRef]
- Zhou, W.; Zhou, X.; Huang, X.; Zhu, C.; Weir, M.D.; Melo, M.A.S.; Bonavente, A.; Lynch, C.D.; Imazato, S.; Oates, T.W.; et al. Antibacterial and remineralizing nanocomposite inhibit root caries biofilms and protect root dentin hardness at the margins. J. Dent. 2020. [Google Scholar] [CrossRef]
- Takahashi, N.; Nyvad, B. Ecological hypothesis of dentin and root caries. Caries Res. 2016, 50, 422–431. [Google Scholar] [CrossRef]
- Ishihara, K.; Nomura, H.; Mihara, T.; Kurita, K.; Iwasaki, Y.; Nakabayashi, N. Why do phospholipid polymers reduce protein adsorption? J. Biomed. Mater. Res. 1998, 39, 323–330. [Google Scholar] [CrossRef]
- Wang, L.; Li, C.; Weir, M.D.; Zhang, K.; Zhou, Y.; Xu, H.H.K.; Reynolds, M.A. Novel multifunctional dental bonding agent for Class-V restorations to inhibit periodontal biofilms. RSC Adv. 2017, 7, 29004–29014. [Google Scholar] [CrossRef]
- Acosta-Torres, L.S.; Mendieta, I.; Nuñez-Anita, R.E.; Cajero-Juárez, M.; Castaño, V.M. Cytocompatible antifungal acrylic resin containing silver nanoparticles for dentures. Int. J. Nanomed. 2012, 7, 4777. [Google Scholar]
- Lotfi, M.; Vosoughhosseini, S.; Ranjkesh, B.; Khani, S.; Saghiri, M.; Zand, V. Antimicrobial efficacy of nanosilver, sodium hypochlorite and chlorhexidine gluconate against Enterococcus faecalis. Afr. J. Biotechnol. 2011, 10, 6799–6803. [Google Scholar]
- Samiei, M.; Aghazadeh, M.; Lotfi, M.; Shakoei, S.; Aghazadeh, Z.; Pakdel, S.M.V. Antimicrobial efficacy of mineral trioxide aggregate with and without silver nanoparticles. Iran. Endod. J. 2013, 8, 166. [Google Scholar] [PubMed]
- Chen, G.; Lu, J.; Lam, C.; Yu, Y. A novel green synthesis approach for polymer nanocomposites decorated with silver nanoparticles and their antibacterial activity. Analyst 2014, 139, 5793–5799. [Google Scholar] [CrossRef]
- Gudikandula, K.; Charya Maringanti, S. Synthesis of silver nanoparticles by chemical and biological methods and their antimicrobial properties. J. Exp. Nanosci. 2016, 11, 714–721. [Google Scholar] [CrossRef]
- Beyene, H.D.; Werkneh, A.A.; Bezabh, H.K.; Ambaye, T.G. Synthesis paradigm and applications of silver nanoparticles (AgNPs), a review. Sustain. Mater. Technol. 2017, 13, 18–23. [Google Scholar] [CrossRef]
- Ipe, D.S.; Kumar, P.T.S.; Love, R.M.; Hamlet, S.M. Silver Nanoparticles at Biocompatible Dosage Synergistically Increases Bacterial Susceptibility to Antibiotics. Front. Microbiol. 2020, 11, 1074. [Google Scholar] [CrossRef] [PubMed]
- Bhat, R.; Deshpande, R.; Ganachari, S.V.; Huh, D.S.; Venkataraman, A. Photo-irradiated biosynthesis of silver nanoparticles using edible mushroom pleurotus Florida and their antibacterial activity studies. Bioinorg. Chem. Appl. 2011, 2011, 650979. [Google Scholar] [CrossRef]
- Yasin, S.; Liu, L.; Yao, J. Biosynthesis of silver nanoparticles by bamboo leaves extract and their antimicrobial activity. J. Fiber Bioeng. Inf. 2013, 6, 77–84. [Google Scholar]
- Dickens, S.H.; Flaim, G.M.; Takagi, S. Mechanical properties and biochemical activity of remineralizing resin-based Ca–PO4 cements. Dent. Mater. 2003, 19, 558–566. [Google Scholar] [CrossRef]
- Gao, Y.; Liang, K.; Li, J.; Yuan, H.; Liu, H.; Duan, X.; Li, J. Effect and stability of poly (amido amine)-induced biomineralization on dentinal tubule occlusion. Materials 2017, 10, 384. [Google Scholar] [CrossRef]
- Liang, K.; Yuan, H.; Li, J.; Yang, J.; Zhou, X.; He, L.; Cheng, L.; Gao, Y.; Xu, X.; Zhou, X. Remineralization of Demineralized Dentin Induced by Amine-Terminated PAMAM Dendrimer. Macromol. Mater. Eng. 2015, 300, 107–117. [Google Scholar] [CrossRef]
- Liang, K.; Wang, S.; Tao, S.; Xiao, S.; Zhou, H.; Wang, P.; Cheng, L.; Zhou, X.; Weir, M.D.; Oates, T.W.; et al. Dental remineralization via poly(amido amine) and restorative materials containing calcium phosphate nanoparticles. Int. J. Oral Sci. 2019, 11, 1–12. [Google Scholar] [CrossRef]
- Cocco, A.R.; da Rosa, W.L.d.O.; da Silva, A.F.; Lund, R.G.; Piva, E. A systematic review about antibacterial monomers used in dental adhesive systems: Current status and further prospects. Dent. Mater. 2015, 31, 1345–1362. [Google Scholar] [CrossRef]
| Serial Numbers (#) | Search Term |
|---|---|
| #1 | dental composite [All Fields] |
| #2 | composite resin [All Fields] |
| #3 | dental nanocomposite [All Fields] |
| #4 | dental monomer [All Fields] |
| #5 | (#1 OR #2 OR #3 OR #4) |
| #6 | DMAHDM [All Fields] |
| #7 | dimethylaminohexadecyl methacrylate [All Fields] |
| #8 | QAM [All Fields] |
| #9 | quaternary ammonium methacrylate [All Fields] |
| #10 | quaternary ammonium monomers [All Fields] |
| #11 | quaternary ammonium compounds [All Fields] |
| #12 | quaternary ammonium salts [All Fields] |
| #13 | (#5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12) |
| Final search term: #5 AND #13 |
| Antibacterial Outcomes | Remineralizing Outcomes |
|---|---|
|
|
| Reference | Sample Size Calculation | Adequate Control Group | Use of Materials According to Manufacturer’s Instruction | Standardized Sample Production Process | Standardized Antibacterial/ Remineralizing Assessment | Evaluation of Antibacterial/ Remineralizing Properties by a Single Operator | Adequate Statistical Analysis | Risk of Bias * |
|---|---|---|---|---|---|---|---|---|
| Wu et al., 2015 [37] | No | Yes | No | Yes | Yes | No | Yes | Medium risk |
| Wu et al., 2015 [39] | No | Yes | No | Yes | Yes | No | Yes | Medium risk |
| Zhang et al., 2015 [40] | No | Yes | No | Yes | Yes | No | Yes | Medium risk |
| Melo et al., 2016 [41] | No | Yes | No | Yes | Yes | No | Yes | Medium risk |
| Wang et al., 2016 [42] | No | Yes | No | Yes | Yes | No | Yes | Medium risk |
| Wang et al., 2016 [43] | No | Yes | No | Yes | Yes | No | Yes | Medium risk |
| Xie et al., 2016 [44] | No | Yes | No | Yes | Yes | No | Yes | Medium risk |
| Zhang et al., 2016 [20] | No | Yes | No | Yes | Yes | No | Yes | Medium risk |
| Xiao et al., 2017 [23] | No | Yes | No | Yes | Yes | No | Yes | Medium risk |
| Zhang et al., 2017 [45] | No | Yes | No | Yes | Yes | No | Yes | Medium risk |
| Al-Dulaijan et al., 2018 [1] | No | Yes | No | Yes | Yes | No | Yes | Medium risk |
| Wang et al., 2019 [46] | No | Yes | No | Yes | Yes | No | Yes | Medium risk |
| Xiao et al., 2019 [38] | No | Yes | No | Yes | Yes | No | Yes | Medium risk |
| Bhadila et al., 2020 [2] | No | Yes | No | Yes | Yes | No | Yes | Medium risk |
| Zhou et al., 2020 [47] | No | Yes | No | Yes | Yes | No | Yes | Medium risk |
| Reference | Biomaterial Combinations Used and Comparison Group/s | Microorganisms Tested | Time Points Assessed | Methodology Used to Assess Antibacterial Effectiveness | Results Summary |
|---|---|---|---|---|---|
| Wu et al., 2015 [37] | (1–5) Five variants with 10% DMAHDM + 20% NACP + 0%, 2.5%, 5%, 7.5% or 10%, respectively, of microcapsules of formaldehyde and urea Comparison group: (6) 20% NACP | Total microorganism Total streptococci Streptococcus mutans | 2 days | Live/dead assay | Biofilm was primarily alive in (6) (1) showed mostly dead bacteria. |
| Metabolic assay (MTT) | Metabolic activity of (1) was reduced by 96% compared to (6) | ||||
| Production of Lactic Acid | (1) reduced lactic acid production by 99% compared to (6) | ||||
| CFUc counts | (1) reduced the biofilm CFU by 3–4 times compared to (6) | ||||
| Wu et al., 2015 [39] | (1–4) Four variants with 20% NACP and DMAHDM mass fraction of 0.75%, 1.5%, 2.25% and 3%, respectively Comparison group: (5) 20% NACP | Total microorganisms Total streptococci S. mutans | 2 days | Live/dead assay | Biofilm was primarily alive in (5). Amounts of dead bacteria increased with increase in the mass fraction of DMAHDM |
| Metabolic assay (MTT) | Metabolic activity—(4) was 96% lower than (5) | ||||
| Production of Lactic Acid | Increasing DMAHDM mass fraction caused a monotonic decrease in the production of lactic acid | ||||
| CFUc counts | Antibacterial activity increased and CFU decreased with increase in the mass fraction of DMAHDM | ||||
| Zhang et al., 2015 [40] | (1) 1.5% DMAHDM (2) 3% MPC (3) 1.5% DMAHDM + 3% MPC Comparison groups: (4) 0% DMAHDM + 0% MPC (5) Heliomolar commercial composite | Total microorganisms Total streptococci S. mutans | 2 days | Live/dead assay | (1) demonstrated lower bacterial adhesion but most bacteria were alive (1) showed high amounts of dead bacteria |
| Metabolic assay (MTT) | (3) had the least metabolic activity and higher reduction in biofilm growth compared to (1) or (2) | ||||
| Production of Lactic Acid | (3) had the least lactic acid production | ||||
| CFU counts | (3) reduced CFU counts by >3 logs compared to (4) or (5) and had much less biofilm CFU than (1) or (2) | ||||
| Protein adsorption | (3) had less protein adsorption compared to controls than (1) or (2) | ||||
| Melo et al., 2016 [41] | (1) 5% DMAHDM + 0.1% AgNPs + 30% NACP Comparison group: (2) 0% DMAHDM + 0% AgNPs + 0% NACP | Did not specify | 7 days | Live/dead assay | Dental materials containing multiagents resulted in compromised bacteria at tooth-composite interface |
| Wang et al., 2016 [42] | (1) 3% DMAHDM + 20% NACP Comparison groups: (2) 20% NACP (3) Heliomolar commercial composite | P. gingivalis, P. intermedia, Prevotella nigrescens, A. actinomycetemcomitans, F. nucleatum, Enterococcus faecalis | 2 days | Live/dead assay | (1) mainly had dead bacteria while (2) and (3) had primarily live bacteria |
| CFU counts | (1) CFU reduction differed between the bacterial species differently, few by <3 log while others by >3 log | ||||
| Crystal violet biofilm biomass assay | (1) had a significantly decreased biomass value compared to (2) and (3) | ||||
| Polysaccharide production | (1) had greatly reduced polysaccharide production for all six species compared to (2) and (3) | ||||
| Wang et al., 2016 [43] | (1) 3% DMAHDM (2) 3% MPC (3) 3% DMAHDM + 3% MPC b Comparison groups: (4) 0% DMAHDM + 0% MPC (5) Heliomolar commercial composite | P. gingivalis, P. intermedia, A. actinomycetemcomitans, F. nucleatum | 2 days | Live/dead assay | (2) reduced the adhesion of bacteria, (3) demonstrated mostly dead bacteria |
| Metabolic activity (MTT) | (3) presented lower biofilm metabolic activity on all the tested periodontal pathogens compared to (4) and (5) | ||||
| CFU counts | Addition of DMAHDM or MPC independently into the composite decreased the CFU | ||||
| Protein adsorption | (1) had no effect on protein adsorption (2) substantially decreased the protein adsorption by one log compared to (4) and (5) | ||||
| Polysaccharide production | (3) had much less polysaccharide production compared to (4) and (5) | ||||
| Xie et al., 2016 [44] | (1) 30% NACP + 3% MPC (2) 30% NACP + 3% MPC + 1.5% DMAHDM (3) 30% NACP + 3% MPC + 3% DMAHDM Comparison groups: (4) 30% NACP (5) Heliomolar commercial composite | Total microorganisms Total streptococci S. mutans | 2 days (with 2-day biofilm) and 4 days (pH required 72 h of incubation) | Live/dead assay | (4) and (5) were completely covered by live bacteria. Bacterial adhesion was reduced by MPC, DMAHDM produced an antibacterial effect. (3) had the most dead bacteria followed by (2) and (1) |
| Metabolic assay (MTT) | Metabolic activity of biofilms of (3) < (2) < (1) (3) had the lowest metabolic activity of biofilms among all | ||||
| CFU counts | (3) had the least biofilm CFU, count reduced by 3 logs compared to (4) and (5). | ||||
| Protein adsorption | (1) had protein adsorption one log less than (5); (2) and (3) had no effect on the protein adsorption | ||||
| pH of biofilm culture medium | (3) maintained a pH above 6.5. | ||||
| Zhang et al., 2016 [20] | (1–5) Five variants with 20% NACP with QAM CL of 3, 6, 12, 16 and 18, respectively Comparison groups: (6) 20% NACP (7) Renamel Microfill commercial composite | Total microorganisms Total streptococci S. mutans | 30 days | Live/dead assay | (6) and (7) were covered by live bacteria. Dead bacteria increased progressively from CL3 up to CL16 with maximum antibacterial potency at CL16 before decreasing in potency at CL18 as indicated by some live bacteria. |
| Metabolic assay (MTT) | Metabolic activity of biofilms decreased with increase in CL from 3 to 16. CL16 had maximum reduction on metabolic activity, which remained constant with any increase in CL | ||||
| Production of Lactic Acid | The biofilms on (6) and (7) produced the most acid. Acid production capacity of biofilm increased with an increase in CL from 3 to 16 CL16 minimized lactic acid production by 10-fold compared to (6) and (7) | ||||
| CFU counts | CFU counts decreased with an increase in the CL from 3 to 16. Antibacterial activity was strongest at CL16, which lowered at C18. CL16 reduced all three CFU counts by 2 logs compared to (6) and (7) | ||||
| Zhang et al., 2017 [45] | (1) 1.5% DMAHDM (2) 3% MPC (3) 1.5% DMAHDM + 3% MPC Comparison group: (4) Heliomolar commercial composite | Total microorganisms Total streptococci S. mutans | 185 days | Live/dead assay | (3) had high levels of dead bacteria and lower bacterial attachment. Protein-repellent and anti-biofilm activities remained same from day 1 to 180 |
| Metabolic assay (MTT) | (1) and (2) showed higher reduction of biofilm viability than (4) (3) had the least metabolic activity Antibacterial function remained the same from day 1 to 180, being unimpacted by water-aging | ||||
| Production of Lactic Acid | (3) had the least lactic acid production | ||||
| CFU counts | (1) and (2) decreased the CFU compared to (4). (3) had greater antibacterial properties compared to (1) and (2) and was nearly 3 logs lower than (4), both at 1 day and 180 days of water-aging (p < 0.05). | ||||
| Protein adsorption | MPC greatly inhibited protein adsorption with no difference between 1 day and 180 days. (3) had the same protein adsorption as (2) (p > 0.1), which was about one tenth that of (4) and (1) (p < 0.05). | ||||
| Al-Dulaijan et al., 2018 [1] | (1) 20% NACP + 3% DMAHDM (2) 20% NACP Comparison group: (3) Heliomolar commercial composite | Total microorganisms Total streptococci S. mutans | 2 days | Live/dead assay | (1) had much less live bacteria compared to (2) and (3). |
| Metabolic assay (MTT) | (1) greatly decreased the metabolic activity of the biofilms compared to (2) and (3) (p < 0.05). (2) had similar metabolic activity to (3) indicating that NACP had little effect on biofilm viability. | ||||
| Production of Lactic Acid | (1) had the least lactic acid production. | ||||
| CFU counts | (1) decreased all three CFU counts by 3–4 logs compared to (2) and (3). | ||||
| Wang et al., 2019 [46] | (1) 3% MPC + 20% NACP (2) 3% DMAHDM + 20% NACP (3) 3% DMAHDM + 3% MPC + 20% NACP Comparison groups: (4) 20% NACP (5) Heliomolar commercial composite | (1) Biofilm with one species: P. gingivalis (2) Biofilm with three species: P. gingivalis, S. gordonii and F. nucleatum (3) Biofilm with six species: P. gingivalis, S. gordonii, F. nucleatum, A. naeslundii, P. intermedia and A. actinomycetemcomitans (4) Nine-species biofilm: P. gingivalis, S. gordonii, F. nucleatum, A. naeslundii, P. intermedia, A. actinomycetemcomitans, P. nigrescens, Tannerella forsythia and Parvimonas micra | 4 days | Live/dead assay | (2) had large quantity of dead bacteria, (1) showed lower bacterial adhesion. (3) had large quantity of dead bacteria but lower bacterial adhesion that (4) and (5) which were largely covered by live bacteria |
| Metabolic assay (MTT) | (1) and (2) reduced the metabolic activity greatly compared to (3) Killing power of DMAHDM decreased with increase in the number of species in the biofilm (3) had stronger killing efficacy on all biofilm types | ||||
| CFU | (3) had higher reduction of CFU than (1) and (2), by >3 log on all four biofilm types | ||||
| Protein adsorption | DMAHDM demonstrated no effect on protein adsorption (1) decreased the protein adsorption by approximately 1 log, compared to (2) and (5) | ||||
| Polysaccharide production | Single species biofilms produced less polysaccharides than multi species biofilms (1) and (2) decreased the amount of polysaccharide produced by biofilms, (3) showed least production in all the biofilm types | ||||
| Xiao et al., 2019 [38] | (1) 30% NACP + 3% MPC + 3% DMAHDM (2) 30% NACP + 3% MPC + 3% DMAHDM + 0.12% AgNPs a,c Comparison groups: (3) 30% NACP (4) Renamel Microfill commercial composite | (1) P. gingivalis (2) A. actinomycetemcomitans (3) F. nucleatum | 2 days | Live/dead assay | (1) and (2) had much less biofilms, with mostly dead bacteria compared to (3) and (4), which were mostly covered by live bacteria. |
| Metabolic assay (MTT) | Metabolic activity of (1) and (2) lower than (3) and (4) (2) showed lower biofilm metabolic activity for all three bacteria species than (1) | ||||
| Production of Lactic Acid | (1) had significantly decreased CFU counts for all three species, (2) showed the lowest CFU. (1) reduced the CFU counts by 4 logs on P. gingivalis and A. actinomycetemcomitans, while (2) reduced the CFU counts by 5 log. (1) and (2) reduced the CFU counts for F. nucleatum, by 3 and 5 logs, respectively. | ||||
| Protein adsorption | (1) and (2) decreased protein adsorption, it was e tenth of (3) and (4) | ||||
| Polysaccharide production | (1) had much less polysaccharide production than (3) and (4 The lowest production of polysaccharides from biofilms was caused by (2) | ||||
| Bhadila et al., 2020 [2] | (1) 20% NACP (2) 3% DMAHDM + 20% NACP Comparison group: (3) Heliomolar commercial composite | S. mutans | 2 days | Live/dead assay | (2) had primarily dead bacteria compared to (1) and (3) which were primarily covered by live bacteria. |
| Production of Lactic Acid | (2) caused lowest production of lactic acid production from biofilms than (1) and (3) | ||||
| CFU counts | (2) showed a CFU reduction of 3–4 logs less than (1) and (3). | ||||
| Zhou et al., 2020 [47] | (1) 30% NACP (2) 3% DMAHDM (3) 30% NACP + 3% DMAHDM Comparison groups: (4) 0% NACP + 0% DMAHDM (5) Heliomolar commercial composite | S. mutans L. acidophilus C. albicans Multi-species | 2 days | Live/dead assay | (2) had substantial dead bacteria for all species tested while (1), (4) and (5) were covered with live bacteria. |
| Metabolic assay (MTT) | (2) reduced the metabolic activity of biofilms significantly | ||||
| Production of Lactic Acid | (1), (4) and (5) showed higher lactic acid production from S. mutans and polymicrobial biofilms while (2) and (3) inhibited. All materials produced lower levels of lactic acid from L. acidophilus and C. albicans | ||||
| CFU counts | (2) and (3) greatly reduced S. mutans and C. albicans CFU levels by 5 and 3 logs respectively | ||||
| Polysaccharide production | (2) and (3) inhibited production of extracellular matrix from the bacterial associated with root caries |
| Reference | Biomaterial Combinations and Comparison Group/s | Time Points Assessed | Methodology Used to Assess Remineralization | Results Summary |
|---|---|---|---|---|
| Zhang et al., 2016 [20] | (1) 20% NACP with QAM CL16 a Comparison group: (2) 20% NACP | 1, 3, 7, 14, 21 and 28 days | Release of Ca and P ions | (1) released lower levels of Ca and P ions than (2) |
| Xiao et al., 2017 [23] | (1) 0.12% AgNPs + 3% MPC + 3% DMAHDM + 30% NACP (2) 0.12% AgNPs + 3% MPC + 3% DMAHDM + 30% NACP + PAMAM Comparison groups: (3) Demineralized root dentine specimen (4) Demineralized root dentine specimen + PAMAM | 1, 3, 5, 7, 10, 14 and 21 days | Concentration of Ca and P ions | (1) and (2) demonstrated greater concentrations of Ca and P concentrations than PAMAM and control groups |
| Acid neutralization | (1) and (2) had greater acid neutralization than PAMAM and comparison groups. | |||
| Dentine hardness | (2) had the greatest dentine hardness, remineralization and mineral growth. | |||
| SEMexamination | (2) had the greatest remineralization and mineral growth. | |||
| Al-Dulaijan et al., 2018 [1] | (1) 20% NACP + 3% DMAHDM (2) 20% NACP Comparison group: (3) Heliomolar commercial composite | 1, 3, 5, 7, 14, 21, 28, 35, 42, 49, 56, 63 and 70 days | Concentration of Ca and P ions | No differences in concentrations of Ca and P ions, their recharge and re-release between (1) and (2) groups |
| 1, 2, 3, 5, 9, 11 and 14 days | Recharge and rerelease of Ca and P | Specimens could release the ions for 42 days after one charge | ||
| Bhadila et al., 2020 [2] | (1) 20% NACP (2) 3% DMAHDM + 20% NACP Comparison group: (3) Heliomolar commercial composite | 1, 3, 5, 7, 14, 21, 28, 35, 42, 49, 56, 63 and 70 days | Release of Ca and P ions | No significant difference in Ca and P ion release between (1) and (2) |
| 1, 3, 5, 7, 9 and 14 days | Recharge and rerelease of Ca and P | Both composites showed increasing ion concentration with time, and release continued after each recharge. | ||
| Zhou et al., 2020 [47] | (1) 30% NACP (2) 3% DMAHDM (3) 30% NACP + 3% DMAHDM Comparison groups: (4) 0% NACP+ 0% DMAHDM (5) Heliomolar commercial composite | 1, 3, 7, 14, 21, 28, 35, 42, 49, 54, 63 and 70 days | Release of Ca and P ions | No difference in release of Ca and P ions between (1) and (3) Lower pH increased ion release |
| Dentine hardness | (3) caused the highest dentine hardness, which was twice more than that of controls. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Clarin, A.; Ho, D.; Soong, J.; Looi, C.; Ipe, D.S.; Tadakamadla, S.K. The Antibacterial and Remineralizing Effects of Biomaterials Combined with DMAHDM Nanocomposite: A Systematic Review. Materials 2021, 14, 1688. https://doi.org/10.3390/ma14071688
Clarin A, Ho D, Soong J, Looi C, Ipe DS, Tadakamadla SK. The Antibacterial and Remineralizing Effects of Biomaterials Combined with DMAHDM Nanocomposite: A Systematic Review. Materials. 2021; 14(7):1688. https://doi.org/10.3390/ma14071688
Chicago/Turabian StyleClarin, Alison, Daphne Ho, Jana Soong, Cheryl Looi, Deepak Samuel Ipe, and Santosh Kumar Tadakamadla. 2021. "The Antibacterial and Remineralizing Effects of Biomaterials Combined with DMAHDM Nanocomposite: A Systematic Review" Materials 14, no. 7: 1688. https://doi.org/10.3390/ma14071688
APA StyleClarin, A., Ho, D., Soong, J., Looi, C., Ipe, D. S., & Tadakamadla, S. K. (2021). The Antibacterial and Remineralizing Effects of Biomaterials Combined with DMAHDM Nanocomposite: A Systematic Review. Materials, 14(7), 1688. https://doi.org/10.3390/ma14071688






