Universal Adhesive for Fixed Retainer Bonding: In Vitro Evaluation and Randomized Clinical Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. In Vitro Experimentation
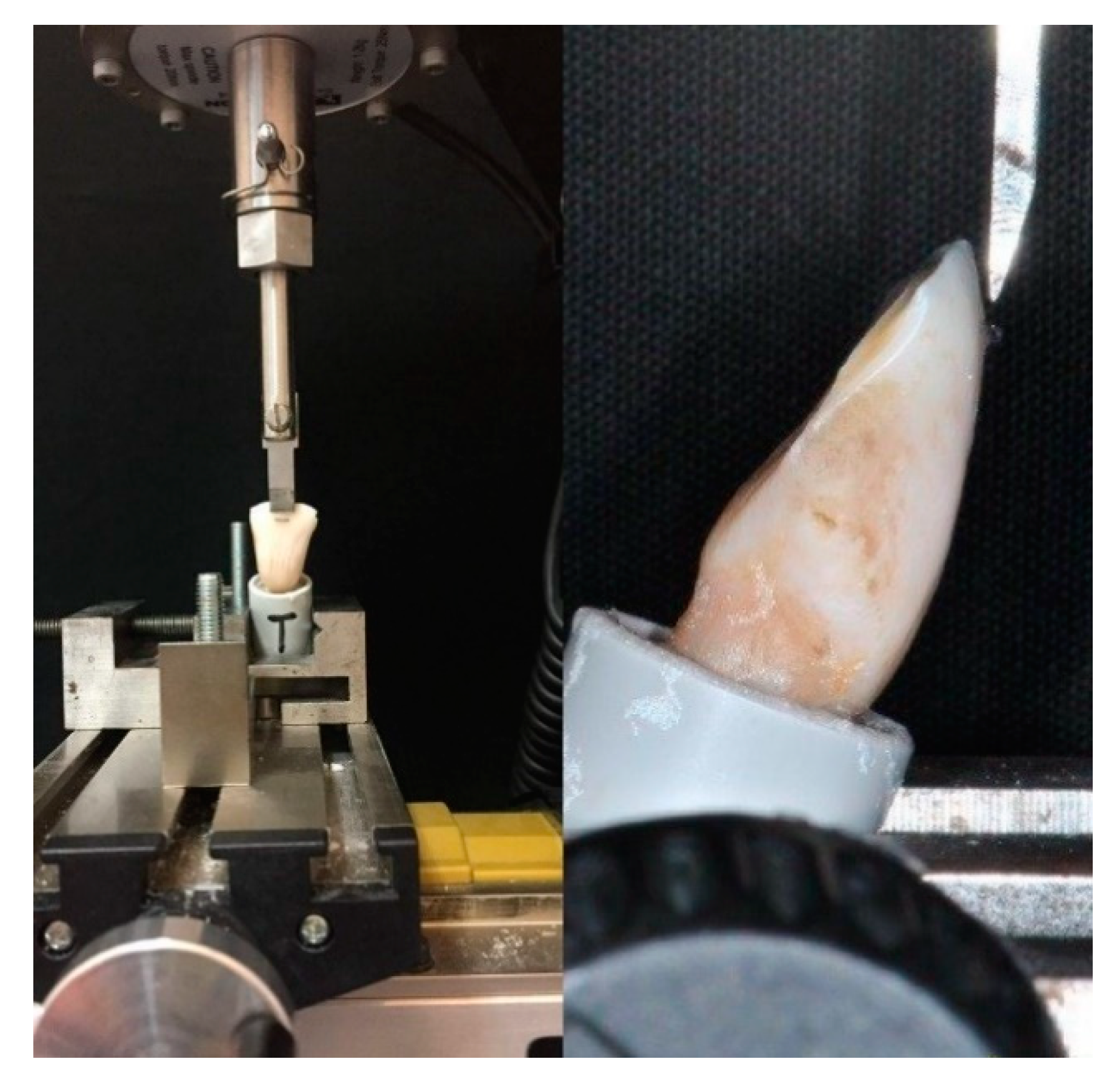
2.1.1. Shear Bond Strength (SBS) Test
2.1.2. Adhesive Remnant Index (ARI) Score
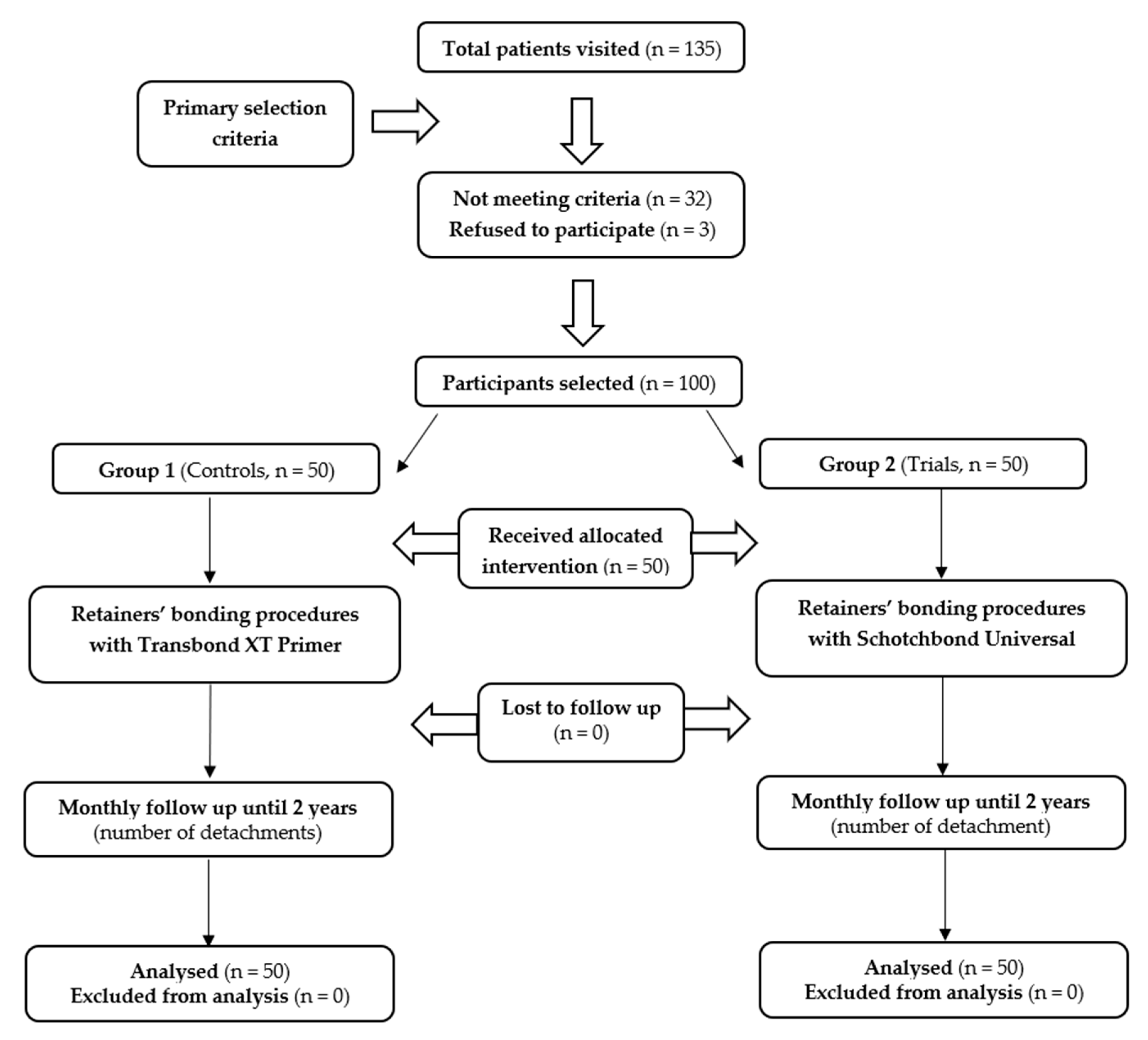
2.2. In Vivo Study
- Trial design
- Participants
- Interventions
- Outcomes
- Sample size
- Randomization and blinding
2.3. Statistical Analysis
3. Results
3.1. In Vitro Experimentation
3.1.1. Shear Bond Strength (SBS) Test
3.1.2. Adhesive Remnant Index (ARI) Score
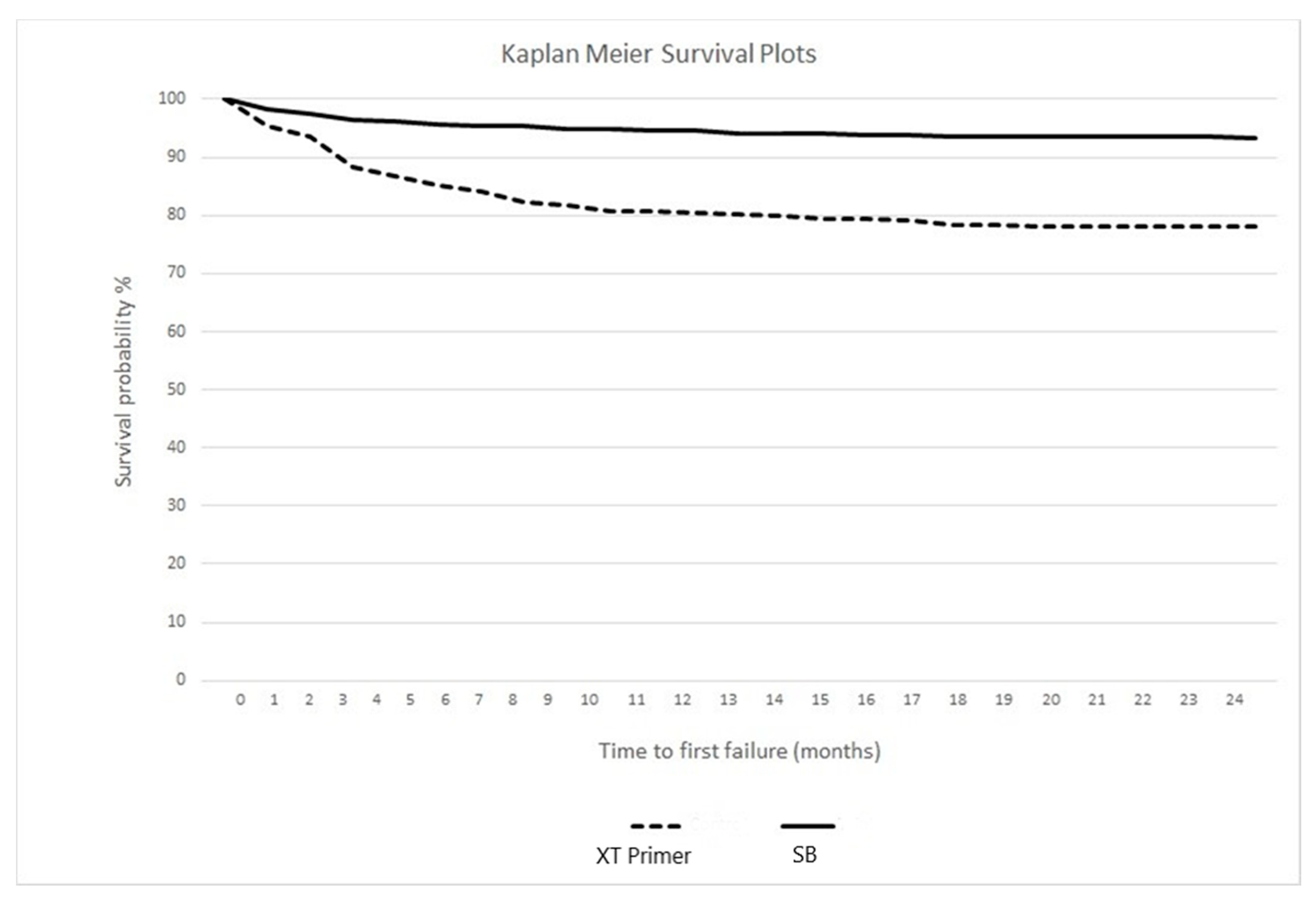
3.2. In Vivo Study
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Littlewood, S.J.; Millett, D.T.; Doubleday, B.; Bearn, D.R.; Worthington, H.V. Retention procedures for stabilising tooth position after treatment with orthodontic braces. Cochrane Database Syst. Rev. 2016, 2016, CD002283. [Google Scholar] [CrossRef] [PubMed]
- Redlich, M.; Rahamim, E.; Gaft, A.; Shoshan, S. The response of supraalveolar gingival collagen to orthodontic rotation movement in dogs. Am. J. Orthod. Dentofac. Orthop. 1996, 110, 247–255. [Google Scholar] [CrossRef]
- Blake, M.; Bibby, K. Retention and stability: A review of the literature. Am. J. Orthod. Dentofac. Orthop. 1998, 114, 299–306. [Google Scholar] [CrossRef]
- Kocher, K.E.; Gebistorf, M.C.; Pandis, N.; Fudalej, P.S.; Katsaros, C. Survival of maxillary and mandibular bonded retainers 10 to 15 years after orthodontic treatment: A retrospective observational study. Progr. Orthod. 2019, 20, 28. [Google Scholar] [CrossRef] [PubMed]
- Scribante, A.; Vallittu, P.K.; Özcan, M. Fiber-Reinforced Composites for Dental Applications. Biomed. Res. Int. 2018, 2018, 4734986. [Google Scholar] [CrossRef]
- Andriekute, A.; Vasiliauskas, A.; Sidlauskas, A. A survey of protocols and trends in orthodontic retention. Progr. Orthod. 2018, 18, 31. [Google Scholar] [CrossRef]
- Dahl, E.H.; Zachrisson, B.U. Long-term experience with direct-bonded lingual retainer. J. Clin. Orthod. 1991, 25, 619–630. [Google Scholar]
- Dietrich, P.; Patcas, R.; Pandis, N.; Eliades, T. Long-term follow-up of maxillary fixed retention: Survival rate and periodontal health. Eur. J. Orthod. 2015, 37, 37–42. [Google Scholar] [CrossRef]
- Scribante, A.; Sfondrini, M.F.; Broggini, S.; D’Allocco, M.; Gandini, P. Efficacy of Esthetic Retainers: Clinical Comparison between Multistranded Wires and Direct-Bond Glass Fiber-Reinforced Composite Splints. Int. J. Dent. 2011, 2011, 548356. [Google Scholar] [CrossRef]
- Sifakakis, I.; Zinelis, S.; Patcas, R.; Eliades, T. Mechanical properties of contemporary orthodontic adhesives used for lingual fixed retention. Biomed. Tech. 2017, 62, 289–294. [Google Scholar] [CrossRef]
- Kilponen, L.; Lassila, L.V.J.; Tolvanen, M.; Varrela, J.; Vallittu, P.K. Effect of removal of enamel on rebonding strength of resin composite to enamel. Biomed. Res. Int. 2016, 18188939. [Google Scholar] [CrossRef] [PubMed]
- Rosa, W.L.; Piva, E.; Silva, A.F. Bond strength of universal adhesives: A systematic review and meta-analysis. J. Dent. 2015, 43, 765–776. [Google Scholar] [CrossRef] [PubMed]
- Beltrami, R.; Chiesa, M.; Scribante, A.; Allegretti, J.; Poggio, C. Comparison of shear bond strength of universal adhesives on etched and nonetched enamel. J. Appl. Biomater. Funct. Mater. 2016, 14, e78–e83. [Google Scholar] [CrossRef] [PubMed]
- De Goes, M.F.; Shinohara, M.S.; Freitas, M.S. Performance of a New One-Step Multi-Mode Adhesive on Etched vs Non-Etched Enamel on Bond Strength and Interfacial Morphology. J. Adhes. Dent. 2014, 16, 243–250. [Google Scholar] [PubMed]
- Radlanski, R.J.; Zain, N.D. Stability of the Bonded Lingual Wire Retainer—A Study of the Initial Bond Strength. J. Orofac. Orthop. 2004, 65, 321. [Google Scholar] [CrossRef]
- Tabrizi, S.; Salemis, E.; Usumez, S. Flowable Composites for Bonding Orthodontic Retainers. Angle Orthod. 2010, 80, 195–200. [Google Scholar] [CrossRef] [PubMed]
- Aldrees, A.; Terki, K.; Al-Mutairi, T.K.; Hakami, Z.W.; Al-Malki, M.M. Bonded Orthodontic Retainers: A Comparison of Initial Bond Strength of Different Wire-and-Composite Combinations. J. Orofac. Orthop. 2010, 71, 290–299. [Google Scholar] [CrossRef]
- Reicheneder, C.; Hofrichter, B.; Faltermeier, A.; Proff, P.; Lippold, C.; Kirschneck, C. Shear bond strength of different retainer wires and bonding adhesives in consideration of the pretreatment process. Head Face Med. 2014, 10, 51. [Google Scholar] [CrossRef] [PubMed]
- Batra, C.; Nagpal, R.; Tyagi, S.P.; Singh, U.P.; Manuja, N. In vitro bonding effectiveness of three different one-step self-etch adhesives with additional enamel etching. J. Investig. Clin. Dent. 2014, 5, 226–236. [Google Scholar] [CrossRef]
- Erickson, R.L.; Barkmeier, W.W.; Latta, M.A. The role of etching in bonding to enamel: A comparison of self-etching and etch-and-rinse adhesive systems. Dent. Mater. 2009, 25, 1459–1967. [Google Scholar] [CrossRef]
- Khosravi, K.; Ataei, E.; Mousavi, M.; Khodaeian, N. Enamel Margins on the Microleakage of a Simplified All-in-One and a Self-etch Adhesive System. Oper. Dent. 2009, 34, 531–536. [Google Scholar] [CrossRef]
- Lührs, A.K.; Guhr, S.; Schilke, R.; Borchers, L.; Geurtsen, W.; Günay, H. Shear Bond Strength of Self-etch Adhesives to Enamel with Additional Phosphoric Acid Etching. Oper. Dent. 2008, 33, 155–162. [Google Scholar] [CrossRef] [PubMed]
- Manuja, N.; Nagpal, R.; Pandit, I.K. Dental Adhesion: Mechanism, Techniques and Durability. J. Clin. Pediatr. Dent. 2012, 36, 223–234. [Google Scholar] [CrossRef] [PubMed]
- Van Landuyt, K.L.; Kanumilli, P.; De Munck, J.; Peumans, M.; Lambrechts, P.; Van Meerbeek, B. Bond strength of a mild self-etch adhesive with and without prior acid-etching. J. Dent. 2006, 34, 77–85. [Google Scholar] [CrossRef]
- Van Meerbeek, B.; Kanumilli, P.; De Munck, J.; Van Landuyt, K.; Lambrechts, P.; Peumans, M. A randomized controlled study evaluating the effectiveness of a two-step self-etch adhesive with and without selective phosphoric-acid etching of enamel. Dent. Mater. 2005, 21, 375–383. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, T.; Takamizawa, T.; Barkmeier, W.W.; Tsujimoto, A.; Endo, H.; Erickson, R.L.; Latta, M.A.; Miyazaki, M. Influence of Etching Mode on Enamel Bond Durability of Universal Adhesive Systems. Oper. Dent. 2016, 41, 520–530. [Google Scholar] [CrossRef]
- Carrilho, E.; Cardoso, M.; Ferreira, M.M.; Marto, C.M.; Paula, A.; Coelho, A.S. 10-MDP Based Dental Adhesives: Adhesive Interface Characterization and Adhesive Stability—A Systematic Review. Materials 2019, 12, 790. [Google Scholar] [CrossRef]
- Edmunds, D.H.; Whittaker, D.K.; Green, R.M. Suitability of human, bovine, equine, and ovine tooth enamel for studies of artificial bacterial carious lesions. Caries Res. 1988, 22, 327–336. [Google Scholar] [CrossRef]
- Scribante, A.; Sfondrini, M.F.; Gatti, S.; Gandini, P. Disinclusion of unerupted teeth by mean of self-ligating brackets: Effect of blood contamination on shear bond strength. Med. Oral Patol. Oral Cir. Bucal. 2013, 18, e162–e167. [Google Scholar] [CrossRef]
- Scribante, A.; Gallo, S.; Turcato, B.; Trovati, F.; Gandini, P.; Sfondrini, M.F. Fear of the Relapse: Effect of Composite Type on Adhesion Efficacy of Upper and Lower Orthodontic Fixed Retainers: In Vitro Investigation and Randomized Clinical Trial. Polymers 2020, 12, 963. [Google Scholar] [CrossRef]
- Baysal, A.; Uysal, T. Resin-modified glass ionomer cements for bonding orthodontic retainers. Eur. J. Orthod. 2010, 32, 254–258. [Google Scholar] [CrossRef]
- Devanna, R.; Keluskar, K.M. Crystal growth vs. conventional acid etching: A comparative evaluation of etch patterns, penetration depths, and bond strengths. Indian J Dent Res. 2008, 19, 309–314. [Google Scholar] [CrossRef] [PubMed]
- Scribante, A.; Massironi, S.; Pieraccini, G.; Vallittu, P.; Lassila, L.; Sfondrini, M.F.; Gandini, P. Effects of nanofillers on mechanical properties of fiber-reinforced composites polymerized with light-curing and additional postcuring. J. Appl. Biomater. Funct. Mater. 2015, 13, e296–e299. [Google Scholar] [CrossRef]
- Scribante, A.; Sfondrini, M.F.; Collesano, V.; Tovt, G.; Bernardinelli, L.; Gandini, P. Dental Hygiene and Orthodontics: Effect of Ultrasonic Instrumentation on Bonding Efficacy of Different Lingual Orthodontic Brackets. Biomed. Res. Int. 2017, 2017, 3714651. [Google Scholar] [CrossRef] [PubMed]
- Sfondrini, M.F.; Gatti, S.; Scribante, A. Effect of blood contamination on shear bond strength of orthodontic brackets and disinclusion buttons. Br. J. Oral. Maxillofac. Surg. 2011, 49, 404–408. [Google Scholar] [CrossRef]
- Talic, N.F. Failure Rates of Orthodontic Fixed Lingual Retainers Bonded with Two Flowable Light-Cured Adhesives: A Comparative Prospective Clinical Trial. J. Contemp. Dent. Pract. 2016, 17, 630–634. [Google Scholar] [CrossRef] [PubMed]
- Nandhra, S.S.; Littlewood, S.J.; Houghton, N.; Luther, F.; Prabhu, J.; Munyombwe, T.; Wood, S.R. Do we need primer for orthodontic bonding? A randomized controlled trial. Eur. J. Orthod. 2015, 37, 147–155. [Google Scholar] [CrossRef] [PubMed]
- Cooke, M.E.; Sherriff, M. Debonding force and deformation of two multistrand lingual retainer wires bonded to incisor enamel: An in vitro study. Eur. J. Orthod. 2010, 32, 741–746. [Google Scholar] [CrossRef] [PubMed]
- Milheiro, A.; de Jager, N.; Feilzer, A.J.; Kleverlaan, C.J. In vitro debonding of orthodontic retainers analyzed with finite element analysis. Eur. J. Orthod. 2015, 37, 491–496. [Google Scholar] [CrossRef][Green Version]
- Scribante, A.; Contreras-Bulnes, R.; Montasser, M.A.; Vallittu, P.K. Orthodontics: Bracket Materials, Adhesives Systems, and Their Bond Strength. Biomed. Res. Int. 2016, 2016, 1329814. [Google Scholar] [CrossRef] [PubMed]
- Soares, F.M.Z.; Follak, A.; da Rosa, L.S.; Montagner, A.S.; Lenzi, T.L.; Rocha, R.O. Bovine tooth is a substitute for human tooth on bond strength studies: A systematic review and meta-analysis of in vitro studies. Dent. Mater. 2016, 32, 1385–1393. [Google Scholar] [CrossRef] [PubMed]
- Cal-Neto, J.P.; Castro, S.; Moura, P.M.; Ribeiro, D.; Miguel, J.A. Influence of enamel sandblasting prior to etching on shear bond strength of indirectly bonded lingual appliances. Angle Orthod. 2011, 81, 149–152. [Google Scholar] [CrossRef] [PubMed]
- Salehi, P.; Zarif Najafi, H.; Roeinpeikar, S.M. Comparison of survival time between two types of orthodontic fixed retainer: A prospective randomized clinical trial. Progr. Orthod. 2013, 14, 25. [Google Scholar] [CrossRef]
- Iliadi, A.; Kloukos, D.; Gkantidis, N.; Katsaros, C.; Pandis, N. Failure of fixed orthodontic retainers: A systematic review. J. Dent. 2015, 43, 876–896. [Google Scholar] [CrossRef]
- Tacken, M.P.; Cosyn, J.; De Wilde, P.; Aerts, J.; Govaerts, E.; Vannet, B.V. Glass fibre reinforced versus multistranded bonded orthodontic retainers: A 2 year prospective multi-centre study. Eur. J. Orthod. 2010, 32, 117–123. [Google Scholar] [CrossRef] [PubMed]
- Butera, A.; Gallo, S.; Maiorani, C.; Molino, D.; Chiesa, A.; Preda, C.; Esposito, F.; Scribante, A. Probiotic Alternative to Chlorhexidine in Periodontal Therapy: Evaluation of Clinical and Microbiological Parameters. Microorganisms 2021, 9, E69. [Google Scholar] [CrossRef]
- Al-Moghrabi, D.; Pandis, N.; Fleming, P.S. The effects of fixed and removable orthodontic retainers: A systematic review. Progr. Orthod. 2016, 17, 24. [Google Scholar] [CrossRef] [PubMed]
- Bovali, E.; Kiliaridis, S.; Cornelis, M.A. Indirect vs direct bonding of mandibular fixed retainers in orthodontic patients: A single center randomized controlled trial comparing placement time and failure over a 6-month period. Am. J. Orthod. Dentofac. Orthop. 2014, 146, 701–708. [Google Scholar] [CrossRef]
- Fox, N.A.; McCabe, J.F.; Buckley, J.G. A critique of bond strength testing in orthodontics. Br. J. Orthod. 1994, 21, 33–43. [Google Scholar] [CrossRef]
- Pickett, K.L.; Sadowsky, P.L.; Jacobson, A.; Lacefield, W. Orthodontic in vivo bond strength: Comparison with in vitro results. Angle Orthod. 2001, 71, 141–148. [Google Scholar]
| Material | Type | Composition | pH | Application Protocol |
|---|---|---|---|---|
| Transbond XT Primer | Filler-free, light-cured liquid resin | BisGMA, TEGDMA | - | 1. Teeth polishing with a non-fluoride oil-free pumice 2. Rinsing 3. Tooth isolation with cotton rolls 4. Etching 5. Thoroughly rinsing with water and thoroughly air-drying 1. Application of a thin uniform coat of Transbond XT Primer to each tooth surface to be bonded 2. Air-blow 3. Photopolymerization(10 seconds) |
| Scotchbond Universal | Universal adhesive | 10-MDP, HEMA, silane, dimethacrylate resins, VitrebondTM copolymer, filler, ethanol, water, initiators, catalysts | 2.7 | According to the total-etch mode: 1. Tooth isolation2. Etching 3. Rinsing and air-drying 4. Adhesive application and rubbing for 20 seconds 5. Gently air-drying for 5 seconds 6. Photopolymerization for 10 seconds |
| Transbond XT Light Cure Adhesive Paste | Filler-reinforced, light-cured paste | Silane treated quartz (70%–80%), Bis-GMA (10%–20%), Bisphenol A Bis(2-hydroxyethyl ether) dimethacrylate (5%–10%), Silane treated silica (<2%), DPIHFP (<0.2%) | - | 1. Apply around retainer 2. Photopolymerization for 20 seconds |
| Group | Adhesive/Primer | Mean | SD | Minimum | Median | Maximum | Significance |
|---|---|---|---|---|---|---|---|
| 1 | Transbond XT Primer | 11.05 | 2.43 | 8.39 | 10.51 | 18.63 | p > 0.05; t = 1.948, df = 38 |
| 2 | Scotchbond Universal | 12.77 | 2.75 | 8.35 | 12.66 | 20.01 |
| Score | Group 1 (XT Primer) | Group 2 (SB) |
|---|---|---|
| ARI = 0 | 0 | 0 |
| ARI = 1 | 5 | 10 |
| ARI = 2 | 90 | 80 |
| ARI = 3 | 5 | 10 |
| Group | Adhesive/Primer | Splinted Arch | Teeth | Teeth Bonded | Failures | Rate (%) | Significance |
|---|---|---|---|---|---|---|---|
| Group 1 | Transbond XT Primer | Upper | Canines | 100 | 7 | 7.00 | p < 0.05 |
| Group 1 | Transbond XT Primer | Upper | Incisors | 200 | 42 | 21.00 | |
| Group 1 | Transbond XT Primer | Lower | Canines | 100 | 14 | 14.00 | p < 0.05 |
| Group 1 | Transbond XT Primer | Lower | Incisors | 200 | 68 | 34.00 | |
| Group 2 | Scotchbond Universal | Upper | Canines | 100 | 3 | 3.00 | p < 0.05 |
| Group 2 | Scotchbond Universal | Upper | Incisors | 200 | 19 | 9.50 | |
| Group 2 | Scotchbond Universal | Lower | Canines | 100 | 2 | 2.00 | p < 0.05 |
| Group 2 | Scotchbond Universal | Lower | Incisors | 200 | 16 | 8.00 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sfondrini, M.F.; Gallo, S.; Turcato, B.; Montasser, M.A.; Albelasy, N.F.; Vallittu, P.K.; Gandini, P.; Scribante, A. Universal Adhesive for Fixed Retainer Bonding: In Vitro Evaluation and Randomized Clinical Trial. Materials 2021, 14, 1341. https://doi.org/10.3390/ma14061341
Sfondrini MF, Gallo S, Turcato B, Montasser MA, Albelasy NF, Vallittu PK, Gandini P, Scribante A. Universal Adhesive for Fixed Retainer Bonding: In Vitro Evaluation and Randomized Clinical Trial. Materials. 2021; 14(6):1341. https://doi.org/10.3390/ma14061341
Chicago/Turabian StyleSfondrini, Maria Francesca, Simone Gallo, Benedetta Turcato, Mona A. Montasser, Nehal Fouad Albelasy, Pekka K. Vallittu, Paola Gandini, and Andrea Scribante. 2021. "Universal Adhesive for Fixed Retainer Bonding: In Vitro Evaluation and Randomized Clinical Trial" Materials 14, no. 6: 1341. https://doi.org/10.3390/ma14061341
APA StyleSfondrini, M. F., Gallo, S., Turcato, B., Montasser, M. A., Albelasy, N. F., Vallittu, P. K., Gandini, P., & Scribante, A. (2021). Universal Adhesive for Fixed Retainer Bonding: In Vitro Evaluation and Randomized Clinical Trial. Materials, 14(6), 1341. https://doi.org/10.3390/ma14061341









