Ball versus Locator® Attachments: A Retrospective Study on Prosthetic Maintenance and Effect on Oral-Health-Related Quality of Life
Abstract
:1. Introduction
2. Materials and Methods
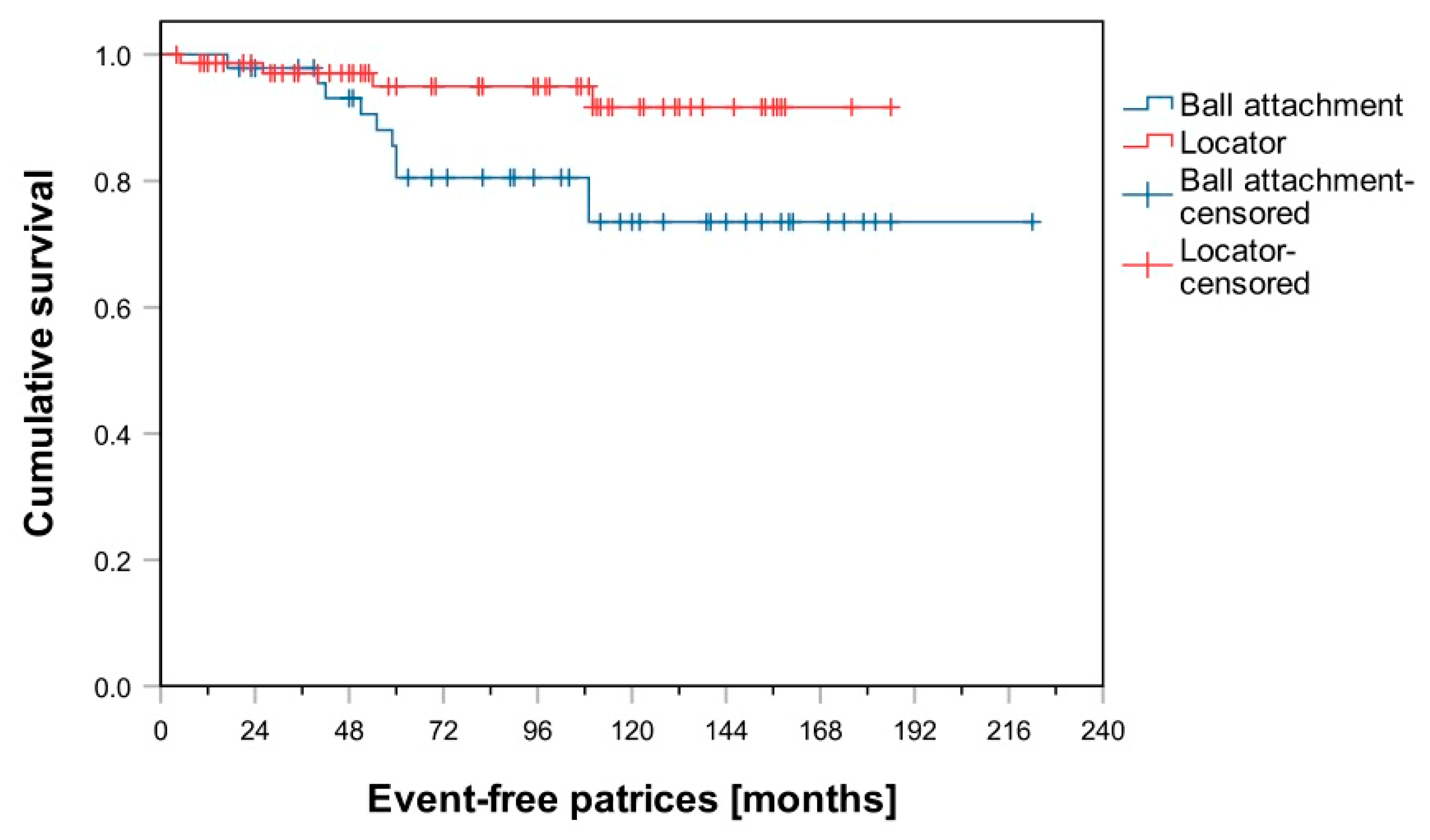
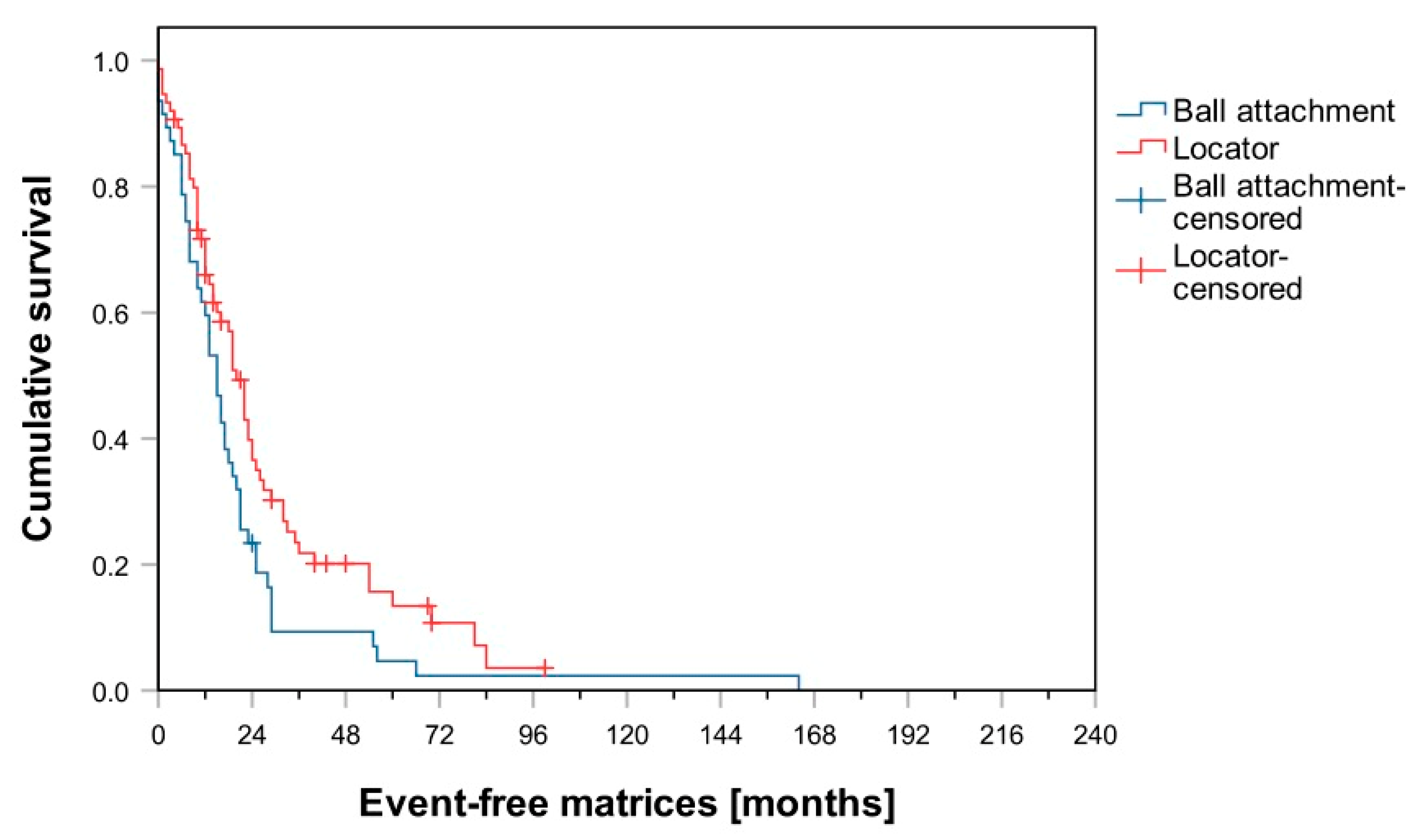
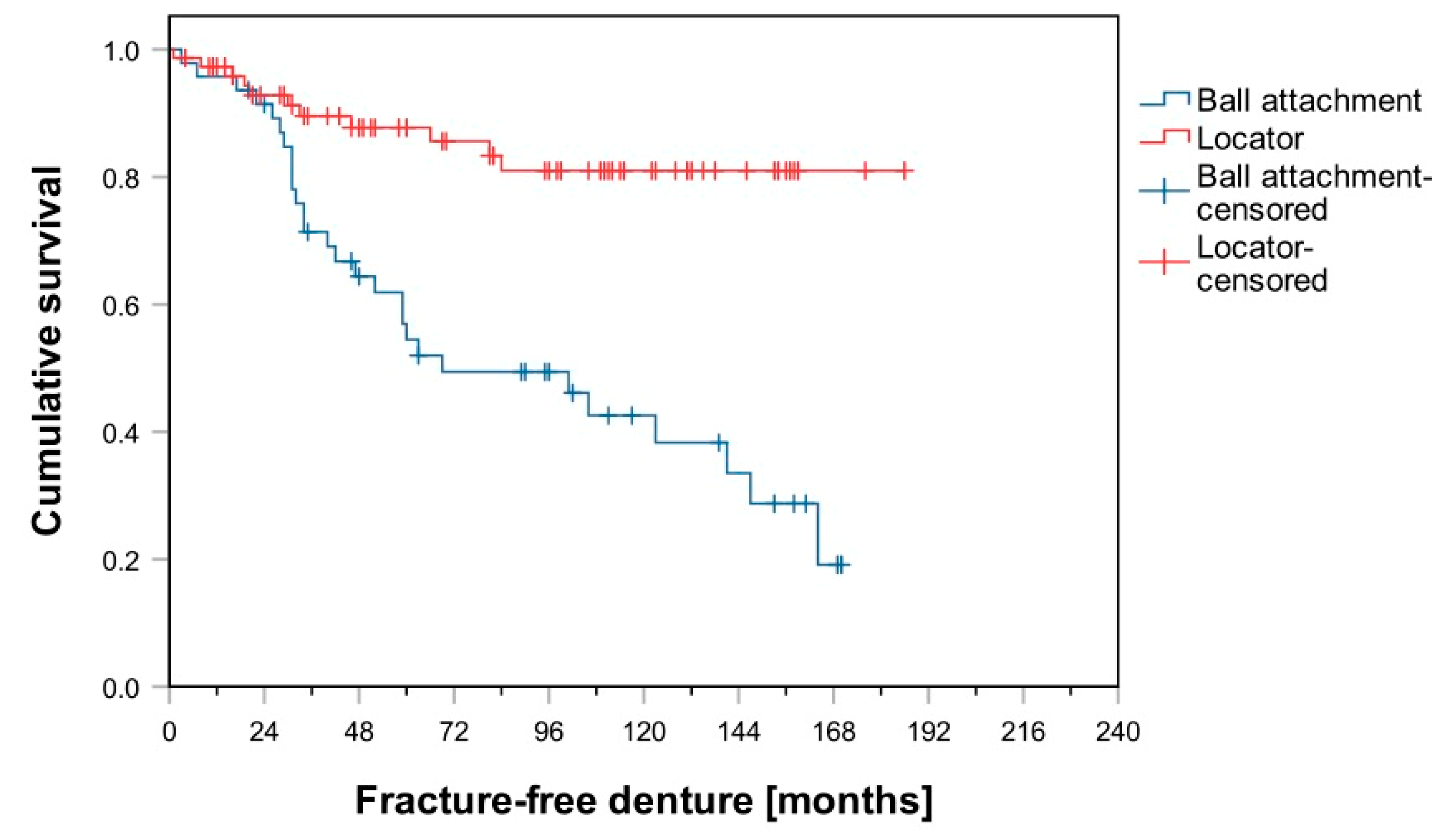
3. Results
4. Discussion
5. Conclusions
- Fewer maintenance measures were required for implant-retained overdentures retained by Locator® attachments than for those retained by ball attachments.
- Denture fracture occurred more frequently when ball attachments were applied.
- In both groups, the most common maintenance measures were matrix-related events, re-lining, and denture fractures.
- OHRQoL was significantly higher among patients in Group L than among patients in Group B.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Polzer, I.; Schimmel, M.; Muller, F.; Biffar, R. Edentulism as part of the general health problems of elderly adults. Int. Dent. J. 2010, 60, 143–155. [Google Scholar] [PubMed]
- Kern, J.S.; Kern, T.; Wolfart, S.; Heussen, N. A systematic review and meta-analysis of removable and fixed implant-supported prostheses in edentulous jaws: Post-loading implant loss. Clin. Oral. Implant. Res. 2016, 27, 174–195. [Google Scholar] [CrossRef]
- Thomason, J.M.; Kelly, S.A.; Bendkowski, A.; Ellis, J.S. Two implant retained overdentures--a review of the literature supporting the McGill and York consensus statements. J. Dent. 2012, 40, 22–34. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.J.; Nagrath, R.; Lahori, M. A comparative evaluation of chewing efficiency, masticatory bite force, and patient satisfaction between conventional denture and implant-supported mandibular overdenture: An in vivo study. J. Indian Prosthodont Soc. 2017, 17, 361–372. [Google Scholar] [CrossRef]
- Zhang, L.; Lyu, C.; Shang, Z.; Niu, A.; Liang, X. Quality of life of implant-supported overdenture and conventional complete denture in restoring the edentulous mandible: A systematic review. Implant. Dent. 2017, 26, 945–950. [Google Scholar] [CrossRef] [PubMed]
- Elsyad, M.A.; Shawky, A.F. Masticatory function with ball and resilient telescopic anchors of mandibular implant-retained overdentures: A crossover study. Quintessence Int. 2017, 48, 615–623. [Google Scholar]
- Elsyad, M.A.; Hegazy, S.A.; Hammouda, N.I.; Al-Tonbary, G.Y.; Habib, A.A. Chewing efficiency and electromyographic activity of masseter muscle with three designs of implant-supported mandibular overdentures. A cross-over study. Clin. Oral. Implants Res. 2014, 25, 742–748. [Google Scholar] [CrossRef]
- Brandt, S.; Brandt, J.; Ketabi, A.R.; Lauer, H.C.; Kunzmann, A. Locator® versus ceramic/electroplated double-crown attachments: A prospective study on the intraindividual comparison of implant-supported mandibular prostheses. Clin. Oral. Investig. 2019, 23, 763–770. [Google Scholar] [CrossRef]
- Naert, I.; Alsaadi, G.; Quirynen, M. Prosthetic aspects and patient satisfaction with two-implant-retained mandibular overdentures: A 10-year randomized clinical study. Int. J. Prosthodont 2004, 17, 401–410. [Google Scholar] [CrossRef]
- Gotfredsen, K.; Holm, B. Implant-supported mandibular overdentures retained with ball or bar attachments: A randomized prospective 5-year study. Int. J. Prosthodont 2000, 13, 125–130. [Google Scholar]
- Khurana, N.; Rodrigues, S.; Shenoy, S.; Saldanha, S.; Pai, U.; Shetty, T.; Mahesh, M.; Hegde, P. A Comparative Evaluation of Stress Distribution with Two Attachment Systems of Varying Heights in a Mandibular Implant-Supported Overdenture: A Three-Dimensional Finite Element Analysis. J. Prosthodont 2019, 28, e795–e805. [Google Scholar] [CrossRef]
- Dashti, M.H.; Atashrazm, P.; Emadi, M.I.; Mishaeel, S.; Banava, S. The effects of two attachment types on the stresses introduced to the mandibular residual ridge: A 3D finite element analysis. Quintessence Int 2013, 44, 585–590. [Google Scholar] [PubMed]
- Krennmair, G.; Seemann, R.; Weinlander, M.; Piehslinger, E. Comparison of ball and telescopic crown attachments in implant-retained mandibular overdentures: A 5-year prospective study. Int. J. Oral. Maxillofac. Implants 2011, 26, 598–606. [Google Scholar] [PubMed]
- Vere, J.; Hall, D.; Patel, R.; Wragg, P. Prosthodontic maintenance requirements of implant-retained overdentures using the Locator attachment system. Int. J. Prosthodont 2012, 25, 392–394. [Google Scholar]
- Liu, W.; Zhang, X.; Qing, H.; Wang, J. Effect of LOCATOR attachments with different retentive forces on the stability of 2-implant-retained mandibular overdenture. J. Prosthet. Dent. 2019, 124, 224–229. [Google Scholar] [CrossRef]
- Matthys, C.; Vervaeke, S.; Besseler, J.; Doornewaard, R.; Dierens, M.; De Bruyn, H. Five years follow-up of mandibular 2-implant overdentures on Locator or ball abutments: Implant results, patient-related outcome, and prosthetic maintenance. Clin. Implant. Dent. Relat Res. 2019, 21, 835–844. [Google Scholar] [CrossRef] [PubMed]
- Zweers, J.; van Doornik, A.; Hogendorf, E.A.; Quirynen, M.; Van der Weijden, G.A. Clinical and radiographic evaluation of narrow- vs. regular-diameter dental implants: A 3-year follow-up. A retrospective study. Clin. Oral. Implants Res. 2015, 26, 149–156. [Google Scholar] [CrossRef]
- Turk, P.E.; Geckili, O.; Turk, Y.; Gunay, V.; Bilgin, T. In vitro comparison of the retentive properties of ball and Locator attachments for implant overdentures. Int. J. Oral. Maxillofac. Implants 2014, 29, 1106–1113. [Google Scholar] [CrossRef]
- Krennmair, G.; Seemann, R.; Fazekas, A.; Ewers, R.; Piehslinger, E. Patient preference and satisfaction with implant-supported mandibular overdentures retained with ball or Locator attachments: A crossover clinical trial. Int. J. Oral. Maxillofac. Implants 2012, 27, 1560–1568. [Google Scholar]
- Slade, G.D. Derivation and validation of a short-form oral health impact profile. Community Dent. Oral. Epidemiol. 1997, 25, 284–290. [Google Scholar] [CrossRef]
- John, M.T.; Miglioretti, D.L.; LeResche, L.; Koepsell, T.D.; Hujoel, P.; Micheelis, W. German short forms of the Oral Health Impact Profile. Community Dent. Oral. Epidemiol. 2006, 34, 277–288. [Google Scholar] [CrossRef]
- Sato, N.; Koyama, S.; Mito, T.; Izumita, K.; Ishiko, R.; Yamauchi, K.; Miyashita, H.; Ogawa, T.; Kosaka, M.; Takahashi, T.; et al. Changes in oral health-related quality of life after oral rehabilitation with dental implants in patients following mandibular tumor resection. J. Oral. Sci. 2019, 61, 406–411. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kleis, W.K.; Kammerer, P.W.; Hartmann, S.; Al-Nawas, B.; Wagner, W. A comparison of three different attachment systems for mandibular two-implant overdentures: One-year report. Clin. Implant. Dent. Relat. Res. 2010, 12, 209–218. [Google Scholar] [CrossRef]
- ELsyad, M.A.; Dayekh, M.A.; Khalifa, A.K. Locator Versus Bar Attachment Effect on the Retention and Stability of Implant-Retained Maxillary Overdenture: An In Vitro Study. J. Prosthodont 2019, 28, e627–e636. [Google Scholar] [CrossRef] [PubMed]
- Evtimovska, E.; Masri, R.; Driscoll, C.F.; Romberg, E. The change in retentive values of Locator attachments and hader clips over time. J. Prosthodont 2009, 18, 479–483. [Google Scholar] [CrossRef] [PubMed]
- Sultana, N.; Bartlett, D.W.; Suleiman, M. Retention of implant-supported overdentures at different implant angulations: Comparing Locator and ball attachments. Clin. Oral. Implants Res. 2017, 28, 1406–1410. [Google Scholar] [CrossRef]
- Teimoori, H.; Shayegh, S.S.; Zavaree, M.A.; Hakimaneh, S.M.; Khodadad, F.; Shidfar, S.; Baghani, M.T. Effects of Excessive Implant Angulation on Retention of Two Types of Overdenture Attachments during Cyclic Loading. J. Contemp. Dent. Pract. 2018, 19, 1221–1227. [Google Scholar]
- Vahidi, F.; Pinto-Sinai, G. Complications associated with implant-retained removable prostheses. Dent. Clin. North. Am. 2015, 59, 215–226. [Google Scholar] [CrossRef]
- Fernandez-Estevan, L.; Montero, J.; Selva Otaolaurruchi, E.J.; Sola Ruiz, M.F. Interventions to Maintain Locator-Retained Mandibular Overdentures on Both External Hex and Internal Connection Implants: A Retrospective Study. Int. J. Oral. Maxillofac. Implants 2018, 33, 838–846. [Google Scholar] [CrossRef]
- Nguyen, C.T.; Masri, R.; Driscoll, C.F.; Romberg, E. The effect of denture cleansing solutions on the retention of pink Locator attachments: An in vitro study. J. Prosthodont 2010, 19, 226–230. [Google Scholar] [CrossRef]
- Fouda, S.M.; Al-Attar, M.S.; Virtanen, J.I.; Raustia, A. Effect of Patient’s Personality on Satisfaction with Their Present Complete Denture and after Increasing the Occlusal Vertical Dimension: A Study of Edentulous Egyptian Patients. Int. J. Dent. 2014, 2014, 635943. [Google Scholar] [CrossRef] [Green Version]
- Prombonas, A.E.; Vlissidis, D.S. Comparison of the midline stress fields in maxillary and mandibular complete dentures: A pilot study. J. Prosthet. Dent. 2006, 95, 63–70. [Google Scholar] [CrossRef]
- ELsyad, M.A.; Errabti, H.M.; Mustafa, A.Z. Mandibular Denture Base Deformation with Locator and Ball Attachments of Implant-Retained Overdentures. J. Prosthodont 2016, 25, 656–664. [Google Scholar]
- Aroso, C.; Silva, A.S.; Ustrell, R.; Mendes, J.M.; Braga, A.C.; Berastegui, E.; Escuin, T. Effect of abutment angulation in the retention and durability of three overdenture attachment systems: An in vitro study. J. Adv. Prosthodont 2016, 8, 21–29. [Google Scholar] [CrossRef] [Green Version]
- Yabul, A.; Dayan, C.; Geckili, O.; Bilhan, H.; Tuncer, N. Evaluation of volumetric wear of abutments on the retention loss of ball attachment systems in implant-retained overdentures: An in vitro study. Clin. Implant. Dent. Relat. Res. 2018, 20, 778–784. [Google Scholar] [CrossRef] [PubMed]
- John, M.T.; Micheelis, W.; Biffar, R. Normwerte mundgesundheitsbezogener Lebensqualität für Kurzversionen des Oral Health Impact Profile [Reference values in oral health-related quality of life for the abbreviated version of the Oral Health Impact Profile]. Schweiz Monatsschr. Zahnmed 2004, 114, 784–791. [Google Scholar]
- Knipfer, C.; Bocklet, T.; Noeth, E.; Schuster, M.; Sokol, B.; Eitner, S.; Nkenke, E.; Stelzle, F. Speech intelligibility enhancement through maxillary dental rehabilitation with telescopic prostheses and complete dentures: A prospective study using automatic, computer-based speech analysis. Int. J. Prosthodont 2012, 25, 24–32. [Google Scholar] [PubMed]
- Müller, F.; Hernandez, M.; Grütter, L.; Aracil-Kessler, L.; Weingart, D.; Schimmel, M. Masseter muscle thickness, chewing efficiency and bite force in edentulous patients with fixed and removable implant-supported prostheses: A cross-sectional multicenter study. Clin Oral Implants Res. 2012, 23, 144–150. [Google Scholar] [CrossRef] [Green Version]
- Khalid, T.; Yunus, N.; Ibrahim, N.; Elkezza, A.; Masood, M. Patient-reported outcome and its association with attachment type and bone volume in mandibular implant overdenture. Clin. Oral. Implants Res. 2017, 28, 535–542. [Google Scholar] [CrossRef]
- Deeb, M.A.; Abduljabbar, T.; Vohra, F.; Zafar, M.S.; Hussain, M. Assessment of factors influencing oral health-related quality of life (OHRQoL) of patients with removable dental prosthesis. Pak. J. Med. Sci. 2020, 36, 213–218. [Google Scholar] [CrossRef] [Green Version]
- Kuoppala, R.; Näpänkangas, R.; Raustia, A. Quality of Life of Patients Treated With Implant-Supported Mandibular Overdentures Evaluated With the Oral Health Impact Profile (OHIP-14): A Survey of 58 Patients. J. Oral. Maxillofac. Res. 2013, 4, e4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reich, S.; Schierz, O. Chair-side generated posterior lithium disilicate crowns after 4 years. Clin. Oral Investig. 2013, 17, 1765–1772. [Google Scholar] [CrossRef] [PubMed]
- Guédat, C.; Nagy, U.; Schimmel, M.; Muller, F.; Srinivasan, M. Clinical performance of LOCATOR® attachments: A retrospective study with 1–8 years of follow-up. Clin. Exp. Dent. Res. 2018, 4, 132–145. [Google Scholar] [CrossRef] [PubMed]
| Maintenance Measure | Group B | Group L |
|---|---|---|
| Matrix-related events per denture | - | - |
| Readjusted | 5.1 ± 4.1 | 2.8 ± 3.1 |
| Reattached | 0.3 ± 0.5 | 0 ± 0.2 |
| Replaced | 0.8 ± 0.8 | 0.1 ± 0.5 |
| Total | 6.1 ± 4.9 | 3.0 ± 3.5 |
| Denture relining | 2.28 ± 1.75 | 1.23 ± 1.11 |
| Denture fracture | 1.09 ± 1.21 | 0.21 ± 0.58 |
| Patrix-related events per denture | - | - |
| Reattached | 0.1 ± 0.4 | 0.1 ± 0.2 |
| Replaced | 0.1 ± 0.3 | 0 ± 0.2 |
| Total | 0.3 ± 0.6 | 0.1 ± 0.4 |
| Denture re-fabrication | 0.57 ± 0.77 | 0.25 ± 0.50 |
| Total number of documented events | 10.28 ± 7.66 | 4.75 ± 4.84 |
| Maintenance Measure | Within 24 Months | Within 60 Months | ||
|---|---|---|---|---|
| Group B | Group L | Group B | Group L | |
| Patrix-related events | 2.1 ± 2.1 | 1.4 ± 1.3 | 19.5 ± 6.2 | 5.1 ± 2.9 |
| Denture refabrication | 0 | 2.8 ± 2 | 12.7 ± 5.3 | 11.9 ± 4.3 |
| Denture fracture | 8.6 ± 4.1 | 7.2 ± 3.1 | 45.5 ± 7.6 | 12.3 ± 4.1 |
| Denture relining | 55.7 ± 7.3 | 46.1 ± 6 | 72 ± 6.7 | 72.9 ± 5.8 |
| Matrix-related events | 76.6 ± 6.2 | 60.2 ± 6 | 95.3 ± 3.2 | 86.6 ± 4.6 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brandt, S.; Lauer, H.-C.; Fehrenz, M.; Güth, J.-F.; Romanos, G.; Winter, A. Ball versus Locator® Attachments: A Retrospective Study on Prosthetic Maintenance and Effect on Oral-Health-Related Quality of Life. Materials 2021, 14, 1051. https://doi.org/10.3390/ma14041051
Brandt S, Lauer H-C, Fehrenz M, Güth J-F, Romanos G, Winter A. Ball versus Locator® Attachments: A Retrospective Study on Prosthetic Maintenance and Effect on Oral-Health-Related Quality of Life. Materials. 2021; 14(4):1051. https://doi.org/10.3390/ma14041051
Chicago/Turabian StyleBrandt, Silvia, Hans-Christoph Lauer, Michael Fehrenz, Jan-Frederik Güth, Georgios Romanos, and Anna Winter. 2021. "Ball versus Locator® Attachments: A Retrospective Study on Prosthetic Maintenance and Effect on Oral-Health-Related Quality of Life" Materials 14, no. 4: 1051. https://doi.org/10.3390/ma14041051
APA StyleBrandt, S., Lauer, H.-C., Fehrenz, M., Güth, J.-F., Romanos, G., & Winter, A. (2021). Ball versus Locator® Attachments: A Retrospective Study on Prosthetic Maintenance and Effect on Oral-Health-Related Quality of Life. Materials, 14(4), 1051. https://doi.org/10.3390/ma14041051







