Effect of Non-Thermal Atmospheric Plasma on Micro-Tensile Bond Strength at Adhesive/Dentin Interface: A Systematic Review
Abstract
:1. Introduction
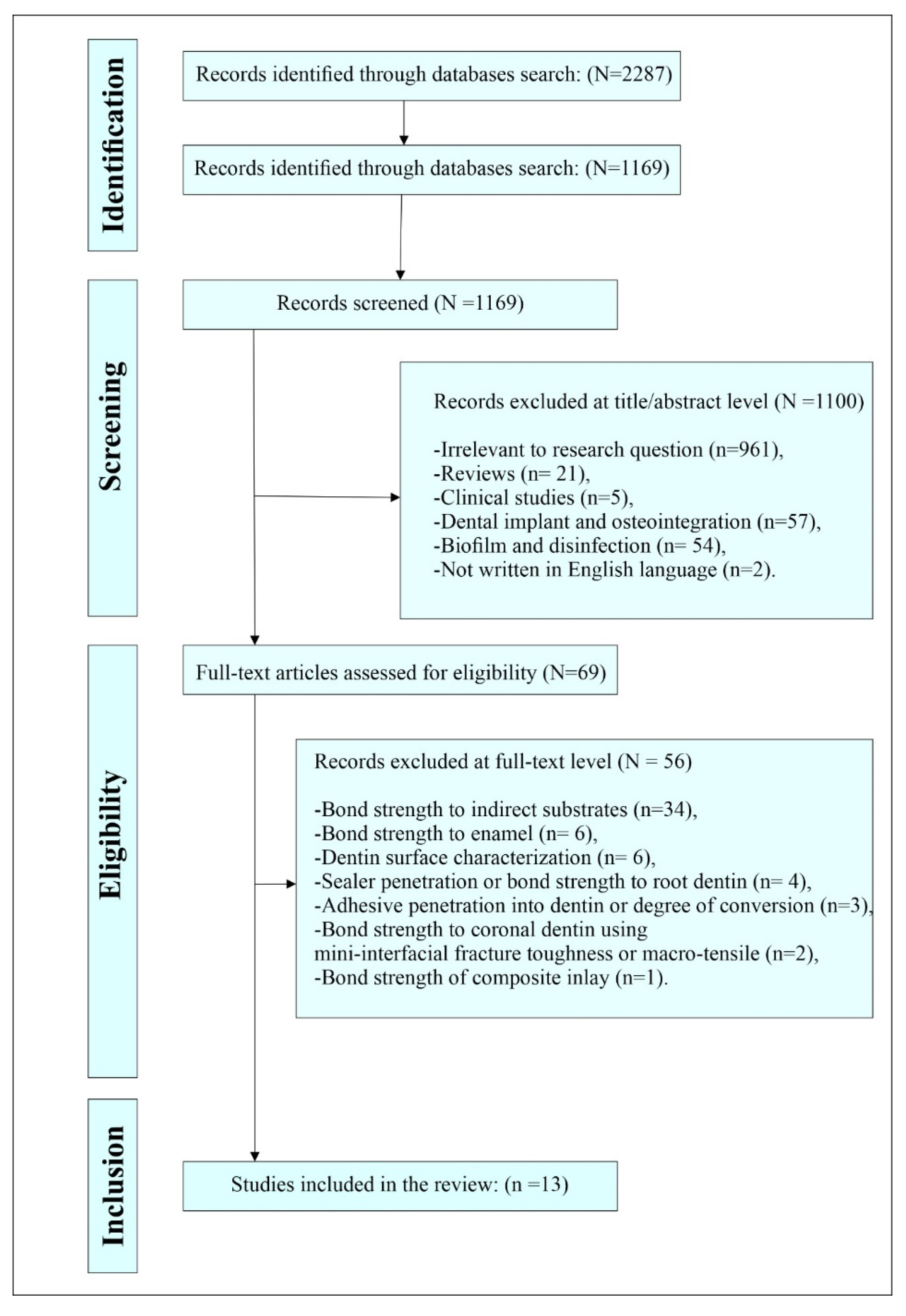
2. Methods
2.1. Methods
2.2. Information Sources and Systematic Search
2.3. Search Strategy
2.4. Data Extraction and Bias Risk Assessment for the Included Studies
3. Results
3.1. Search Results
3.2. Descriptive Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Carvalho, R.M.; Manso, A.P.; Geraldeli, S.; Tay, F.R.; Pashley, D.H. Durability of bonds and clinical success of adhesive restorations. Dent. Mater. 2012, 28, 72–86. [Google Scholar] [CrossRef] [Green Version]
- Breschi, L.; Maravic, T.; Cunha, S.R.; Comba, A.; Cadenaro, M.; Tjäderhane, L.; Pashley, D.H.; Tay, F.R.; Mazzoni, A. Dentin bonding systems: From dentin collagen structure to bond preservation and clinical applications. Dent. Mater. 2018, 34, 78–96. [Google Scholar] [CrossRef] [Green Version]
- Cuevas-Suarez, C.E.; da Rosa, W.L.O.; Lund, R.G.; da Silva, A.F.; Piva, E. Bonding Performance of Universal Adhesives: An Up-dated Systematic Review and Meta-Analysis. J. Adhes. Dent. 2019, 21, 726. [Google Scholar] [CrossRef]
- Cardoso, M.V.; Neves, A.D.A.; Mine, A.; Coutinho, E.; Van Landuyt, K.; De Munck, J.; Van Meerbeek, B. Current aspects on bonding effectiveness and stability in adhesive dentistry. Aust. Dent. J. 2011, 56, 31–44. [Google Scholar] [CrossRef] [PubMed]
- Perdigão, J. Dentin bonding—Variables related to the clinical situation and the substrate treatment. Dent. Mater. 2010, 26, e24–e37. [Google Scholar] [CrossRef]
- Van Meerbeek, B.; De Munck, J.; Yoshida, Y.; Inoue, S.; Vargas, M.; Vijay, P.; Van Landuyt, K.; Lambrechts, P.; Vanherle, G. Buonocore memorial lecture. Adhesion to enamel and dentin: Current status and future challenges. Oper. Dent. 2003, 28, 215–235. [Google Scholar]
- Carvalho, R.M.; Chersoni, S.; Frankenberger, R.; Pashley, D.H.; Prati, C.; Tay, F.R. A challenge to the conventional wisdom that simultaneous etching and resin infiltration always occurs in self-etch adhesives. Biomaterials 2005, 26, 1035–1042. [Google Scholar] [CrossRef]
- Elkaffas, A.A.; Hamama, H.H.; Mahmoud, S.H.; Fawzy, A.S. Effect of acid etching on dentin bond strength of ultra-mild self-etch adhesives. Int. J. Adhes. Adhes. 2020, 99, 102567. [Google Scholar] [CrossRef]
- Wang, Y.; Spencer, P. Quantifying adhesive penetration in adhesive/dentin interface using confocal Raman microspectroscopy. J. Biomed. Mater. Res. 2001, 59, 46–55. [Google Scholar] [CrossRef] [PubMed]
- Hanabusa, M.; Mine, A.; Kuboki, T.; Momoi, Y.; Van Ende, A.; Van Meerbeek, B.; De Munck, J. Bonding effectiveness of a new ‘multi-mode’ adhesive to enamel and dentine. J. Dent. 2012, 40, 475–484. [Google Scholar] [CrossRef] [PubMed]
- Hegde, M.; Manjunath, J. Bond Strength of Newer Dentin Bonding Agents in Different Clinical Situations. Oper. Dent. 2011, 36, 169–176. [Google Scholar] [CrossRef]
- Chiba, Y.; Rikuta, A.; Yasuda, G.; Yamamoto, A.; Takamizawa, T.; Kurokawa, H.; Ando, S.; Miyazaki, M. Influence of moisture conditions on dentin bond strength of single-step self-etch adhesive systems. J. Oral Sci. 2006, 48, 131–137. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, K.; Suzuki, K.; Suwa, S.; Miyaji, H.; Hirose, Y.; Inoue, M. Effects of Surface Wetness of Etched Dentin on Bonding Durability of a Total-etch Adhesive System: Comparison of Conventional and Dumbbell-shaped Specimens. Dent. Mater. J. 2005, 24, 187–194. [Google Scholar] [CrossRef]
- Reis, A.; Pellizzaro, A.; Dal-Bianco, K.; Gomes, O.M.; Patzlaff, R.; Loguercio, A.D. Impact of Adhesive Application to Wet and Dry Dentin on Long-term Resin-dentin Bond Strengths. Oper. Dent. 2007, 32, 380–387. [Google Scholar] [CrossRef] [Green Version]
- Tsujimoto, A.; Shimatani, Y.; Nojiri, K.; Barkmeier, W.W.; Markham, M.D.; Takamizawa, T.; Latta, M.A.; Miyazaki, M. Influence of surface wetness on bonding effectiveness of universal adhesives in etch-and-rinse mode. Eur. J. Oral Sci. 2018, 127, 162–167. [Google Scholar] [CrossRef]
- Choi, A.-N.; Lee, J.-H.; Son, S.-A.; Jung, K.-H.; Kwon, Y.H.; Park, J.-K. Effect of Dentin Wetness on the Bond Strength of Universal Adhesives. Materials 2017, 10, 1224. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kumagai, R.Y.; Hirata, R.; Pereira, P.N.R.; Reis, A.F. Moist vs. over-dried etched dentin: FE-SEM/TEM and bond strength evaluation of resin-dentin interfaces produced by universal adhesives. J. Esthet. Restor. Dent. 2019, 32, 325–332. [Google Scholar] [CrossRef]
- De Siqueira, F.S.F.; Pinto, T.F.; Carvalho, E.M.; Bauer, J.; Gonçalves, L.M.; Szesz, A.L.; Reis, A.; Cardenas, A.F.M.; Loguercio, A.D. Influence of dentinal moisture on the properties of universal adhesives. Int. J. Adhes. Adhes. 2020, 101, 102633. [Google Scholar] [CrossRef]
- Tay, F.R.; Gwinnett, J.A.; Wei, S.H. Micromorphological spectrum from overdrying to overwetting acid-conditioned dentin in water-free, acetone-based, single-bottle primer/adhesives. Dent. Mater. 1996, 12, 236–244. [Google Scholar] [CrossRef]
- Kim, J.; Arola, D.D.; Gu, L.; Kim, Y.K.; Mai, S.; Liu, Y.; Pashley, D.H.; Tay, F.R. Functional biomimetic analogs help remineralize apatite-depleted demineralized resin-infiltrated dentin via a bottom–up approach. Acta Biomater. 2010, 6, 2740–2750. [Google Scholar] [CrossRef] [Green Version]
- Frassetto, A.; Breschi, L.; Turco, G.; Marchesi, G.; Di Lenarda, R.; Tay, F.R.; Pashley, D.H.; Cadenaro, M. Mechanisms of degradation of the hybrid layer in adhesive dentistry and therapeutic agents to improve bond durability—A literature review. Dent. Mater. 2016, 32, e41–e53. [Google Scholar] [CrossRef]
- Liu, Y.; Tjäderhane, L.; Breschi, L.; Mazzoni, A.; Li, N.; Mao, J.; Pashley, D.; Tay, F. Limitations in Bonding to Dentin and Experimental Strategies to Prevent Bond Degradation. J. Dent. Res. 2011, 90, 953–968. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.; Chiba, A.; Scheffel, D.L.; Hebling, J.; Agee, K.; Tagami, J.; Tan, J.; Abuelenain, D.; Abu Nawareg, M.; Hassan, A.H.; et al. Cross-linked dry bonding: A new etch-and-rinse technique. Dent. Mater. 2016, 32, 1124–1132. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stape, T.H.S.; Seseogullari-Dirihan, R.; Tjäderhane, L.; Abuna, G.; Martins, L.R.M.; Tezvergil-Mutluay, A. A novel dry-bonding approach to reduce collagen degradation and optimize resin-dentin interfaces. Sci. Rep. 2018, 8, 16890. [Google Scholar] [CrossRef]
- Chen, M.; Zhang, Y.; Yao, X.; Li, H.; Yu, Q.; Wang, Y. Effect of a non-thermal, atmospheric-pressure, plasma brush on conversion of model self-etch adhesive formulations compared to conventional photo-polymerization. Dent. Mater. 2012, 28, 1232–1239. [Google Scholar] [CrossRef] [Green Version]
- Tendero, C.; Tixier, C.; Tristant, P.; Desmaison, J.; Leprince, P. Atmospheric pressure plasmas: A review. Spectrochim. Acta Part B At. Spectrosc. 2006, 61, 2–30. [Google Scholar] [CrossRef]
- Hirata, R.; Teixeira, H.; Ayres, A.P.A.; Machado, L.S.; Coelho, P.G.; Thompson, V.P.; Giannini, M. Long-term Adhesion Study of Self-etching Systems to Plasma-treated Dentin. J. Adhes. Dent. 2015, 17, 227–233. [Google Scholar]
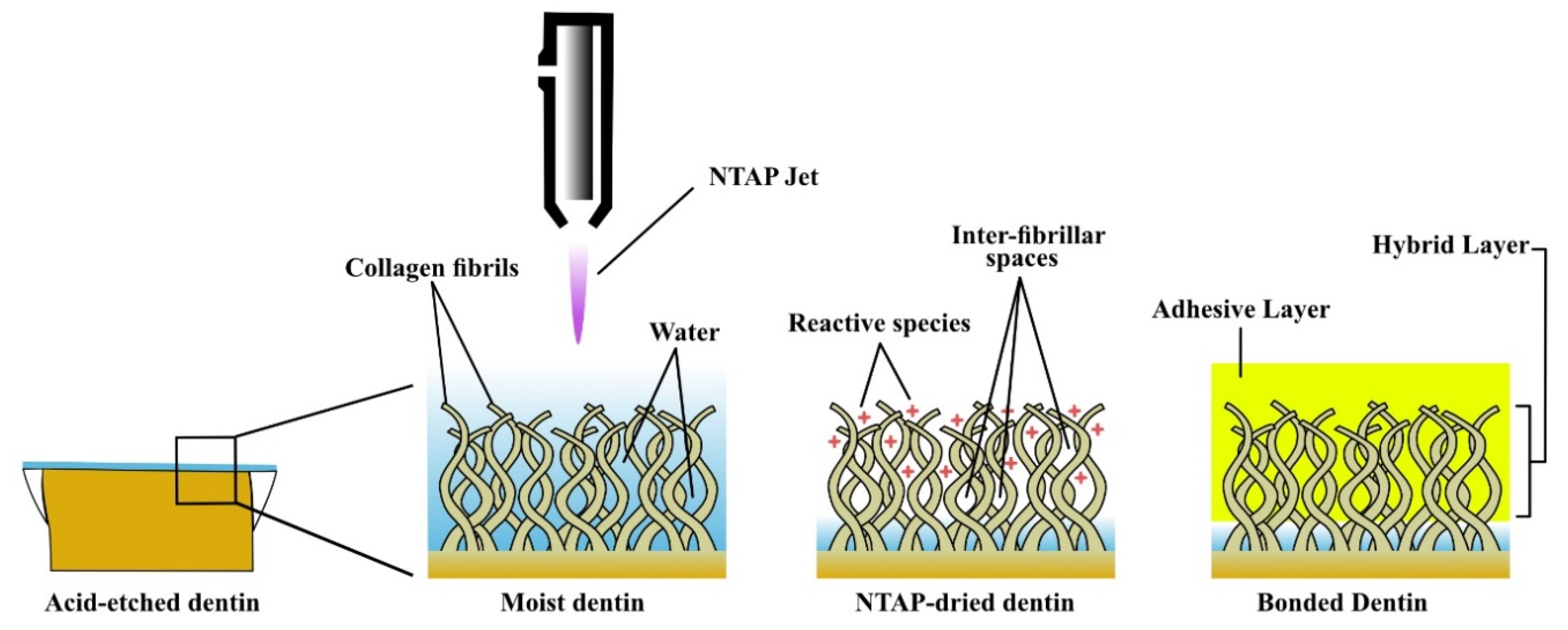
- Zhang, Y.; Yu, Q.; Wang, Y. Non-thermal atmospheric plasmas in dental restoration: Improved resin adhesive penetration. J. Dent. 2014, 42, 1033–1042. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, Y.; Liu, Q.; Yu, Q.; Wang, Y. Nonthermal Atmospheric Plasmas in Dental Restoration. J. Dent. Res. 2016, 95, 496–505. [Google Scholar] [CrossRef] [Green Version]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Sarkis-Onofre, R.; A Skupien, J.; Cenci, M.S.; Moraes, R.R.; Pereira-Cenci, T. The Role of Resin Cement on Bond Strength of Glass-fiber Posts Luted Into Root Canals: A Systematic Review and Meta-analysis of In Vitro Studies. Oper. Dent. 2014, 39, E31–E44. [Google Scholar] [CrossRef]
- da Rosa, W.L.D.O.; Piva, E.; da Silva, A.F. Bond strength of universal adhesives: A systematic review and meta-analysis. J. Dent. 2015, 43, 765–776. [Google Scholar] [CrossRef] [PubMed]
- Han, G.; Kim, J.; Cho, B.; Hwang, Y.; Kim, H. Improved resin-to-dentin bond strength and durability via non-thermal atmospheric pressure plasma drying of etched dentin. Eur. J. Oral Sci. 2018, 127, 170–178. [Google Scholar] [CrossRef] [PubMed]
- Ayres, A.P.; Freitas, P.H.; De Munck, J.; Vananroye, A.; Clasen, C.; Dias, C.D.S.; Giannini, M.; Van Meerbeek, B. Benefits of Nonthermal Atmospheric Plasma Treatment on Dentin Adhesion. Oper. Dent. 2018, 43, E288–E299. [Google Scholar] [CrossRef]
- Ayres, A.P.; Bonvent, J.J.; Mogilevych, B.; Soares, L.E.S.; Martin, A.A.; Ambrosano, G.M.; Nascimento, F.D.; Van Meerbeek, B.; Giannini, M. Effect of non-thermal atmospheric plasma on the dentin-surface topography and composition and on the bond strength of a universal adhesive. Eur. J. Oral Sci. 2018, 126, 53–65. [Google Scholar] [CrossRef] [PubMed]
- Zhu, X.-M.; Zhou, J.-F.; Guo, H.; Zhang, X.-F.; Liu, X.-Q.; Li, H.-P.; Tan, J.-G. Effects of a modified cold atmospheric plasma jet treatment on resin-dentin bonding. Dent. Mater. J. 2018, 37, 798–804. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhu, X.; Guo, H.; Zhou, J.; Zhang, X.; Chen, J.; Li, J.; Li, H.; Tan, J. Influences of the cold atmospheric plasma jet treatment on the properties of the demineralized dentin surfaces. Plasma Sci. Technol. 2018, 20, 044010. [Google Scholar] [CrossRef] [Green Version]
- Kim, J.; Han, G.; Kim, C.-K.; Oh, K.; Chung, S.; Chun, B.; Cho, B. Promotion of adhesive penetration and resin bond strength to dentin using non-thermal atmospheric pressure plasma. Eur. J. Oral Sci. 2015, 124, 89–95. [Google Scholar] [CrossRef] [PubMed]
- Hirata, R.; Sampaio, C.; Machado, L.S.; Coelho, P.G.; Thompson, V.P.; Duarte, S.; Ayres, A.P.A.; Giannini, M. Short- and Long-term Evaluation of Dentin-Resin Interfaces Formed by Etch-and-Rinse Adhesives on Plasma-treated Dentin. J. Adhes. Dent. 2016, 18, 215–222. [Google Scholar] [PubMed]
- De Abreu, J.L.B.; Prado, M.; Da Silva, E.M.; Dias, K.R.H.C.; Simão, R.A. Effect of Non-Thermal Argon Plasma on Bond Strength of a Self-Etch Adhesive System to NaOCl-Treated Dentin. Braz. Dent. J. 2016, 27, 446–451. [Google Scholar] [CrossRef] [Green Version]
- Dong, X.; Li, H.; Chen, M.; Wang, Y.; Yu, Q. Plasma treatment of dentin surfaces for improving self-etching adhesive/dentin interface bonding. Clin. Plasma Med. 2015, 3, 10–16. [Google Scholar] [CrossRef] [Green Version]
- Han, G.-J.; Kim, J.-H.; Chung, S.-N.; Chun, B.-H.; Kim, C.-K.; Cho, B.-H. Effect of Plasma Deposition Using Low-Power/Non-thermal Atmospheric Pressure Plasma on Promoting Adhesion of Composite Resin to Enamel. Plasma Chem. Plasma Process. 2014, 34, 933–947. [Google Scholar] [CrossRef]
- Dong, X.; Ritts, A.C.; Staller, C.; Yu, Q.; Chen, M.; Wang, Y. Evaluation of plasma treatment effects on improving adhesive-dentin bonding by using the same tooth controls and varying cross-sectional surface areas. Eur. J. Oral Sci. 2013, 121, 355–362. [Google Scholar] [CrossRef] [PubMed]
- Ritts, A.C.; Li, H.; Yu, Q.; Xu, C.; Yao, X.; Hong, L.; Wang, Y. Dentin surface treatment using a non-thermal argon plasma brush for interfacial bonding improvement in composite restoration. Eur. J. Oral Sci. 2010, 118, 510–516. [Google Scholar] [CrossRef]
- Sarkis-Onofre, R.; Pereira-Cenci, T.; Tricco, A.C.; Demarco, F.F.; Moher, D.; Cenci, M.S. Systematic reviews in restorative dentistry: Discussing relevant aspects. J. Esthet. Restor. Dent. 2019, 31, 222–232. [Google Scholar] [CrossRef]
- Cook, D.J.; Mulrow, C.D.; Haynes, R.B. Systematic Reviews: Synthesis of Best Evidence for Clinical Decisions. Ann. Intern. Med. 1997, 126, 376–380. [Google Scholar] [CrossRef]
- Stevens, A.; Shamseer, L.; Weinstein, E.; Yazdi, F.; Turner, L.; Thielman, J.; Altman, D.G.; Hirst, A.; Hoey, J.; Palepu, A.; et al. Relation of completeness of reporting of health research to journals’ endorsement of reporting guidelines: Systematic review. BMJ 2014, 348, g3804. [Google Scholar] [CrossRef] [Green Version]
- Salz, U.; Bock, T. Testing adhesion of direct restoratives to dental hard tissue—A review. J. Adhes. Dent. 2010, 12, 343–371. [Google Scholar] [PubMed]
- Pashley, D.H.; Carvalho, R.M.; Sano, H.; Nakajima, M.; Yoshiyama, M.; Shono, Y.; Fernandes, C.A.; Tay, F. The microtensile bond test: A review. J. Adhes. Dent. 1999, 1, 299–309. [Google Scholar]
- Sano, H.; Chowdhury, A.F.M.A.; Saikaew, P.; Matsumoto, M.; Hoshika, S.; Yamauti, M. The microtensile bond strength test: Its historical background and application to bond testing. Jpn. Dent. Sci. Rev. 2020, 56, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Van Meerbeek, B.; Peumans, M.; Poitevin, A.; Mine, A.; Van Ende, A.; Neves, A.; De Munck, J. Relationship between bond-strength tests and clinical outcomes. Dent. Mater. 2010, 26, e100–e121. [Google Scholar] [CrossRef] [PubMed]
- Heintze, S.D.; Rousson, V.; Mahn, E. Bond strength tests of dental adhesive systems and their correlation with clinical results—A meta-analysis. Dent. Mater. 2015, 31, 423–434. [Google Scholar] [CrossRef] [PubMed]
- Langer, A.; Ilie, N. Dentin infiltration ability of different classes of adhesive systems. Clin. Oral Investig. 2012, 17, 205–216. [Google Scholar] [CrossRef] [PubMed]
- Dong, X.; Chen, M.; Wang, Y.; Yu, Q. A mechanistic study of plasma treatment effects on demineralized dentin surfaces for improved adhesive/dentin interface bonding. Clin. Plasma Med. 2014, 2, 11–16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tjäderhane, L.; Nascimento, F.D.; Breschi, L.; Mazzoni, A.; Tersariol, I.L.; Geraldeli, S.; Tezvergil-Mutluay, A.; Carrilho, M.; Carvalho, R.M.; Tay, F.R.; et al. Strategies to prevent hydrolytic degradation of the hybrid layer—A review. Dent. Mater. 2013, 29, 999–1011. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, Y.; Spencer, P. Hybridization Efficiency of the Adhesive/Dentin Interface with Wet Bonding. J. Dent. Res. 2003, 82, 141–145. [Google Scholar] [CrossRef] [PubMed]
- Reis, A.; Chibinski, A.C.; Stanislawczuk, R.; Wambier, D.S.; Grande, R.H.M.; Loguercio, A.D. The role of dentin moisture in the degradation of resin-dentin interfaces under clinical and laboratory conditions. J. Am. Dent. Assoc. (1939) 2012, 143, e29–e36. [Google Scholar] [CrossRef]
- Chen, M.; Zhang, Y.; Driver, M.S.; Caruso, A.N.; Yu, Q.; Wang, Y. Surface modification of several dental substrates by non-thermal, atmospheric plasma brush. Dent. Mater. 2013, 29, 871–880. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lehmann, A.; Rueppell, A.; Schindler, A.; Zylla, I.-M.; Seifert, H.J.; Nothdurft, F.; Hannig, M.; Rupf, S. Modification of Enamel and Dentin Surfaces by Non-Thermal Atmospheric Plasma. Plasma Process. Polym. 2013, 10, 262–270. [Google Scholar] [CrossRef]
- Awad, M.M.; Alrahlah, A.; Matinlinna, J.P.; Hamama, H.H. Effect of adhesive air-drying time on bond strength to dentin: A systematic review and meta-analysis. Int. J. Adhes. Adhes. 2019, 90, 154–162. [Google Scholar] [CrossRef]
- Saikaew, P.; Matsumoto, M.; Chowdhury, A.; Carvalho, R.M.; Sano, H. Does Shortened Application Time Affect Long-Term Bond Strength of Universal Adhesives to Dentin? Oper. Dent. 2018, 43, 549–558. [Google Scholar] [CrossRef]
- Irmak, Ö.; Yaman, B.C.; Orhan, E.O.; Ozer, F.; Blatz, M.B. Effect of rubbing force magnitude on bond strength of universal adhesives applied in self-etch mode. Dent. Mater. J. 2018, 37, 139–145. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seo, Y.S.; Mohamed, A.-A.H.; Woo, K.C.; Lee, H.W.; Lee, J.K.; Kim, K.T. Comparative Studies of Atmospheric Pressure Plasma Characteristics between He and Ar Working Gases for Sterilization. IEEE Trans. Plasma Sci. 2010, 38, 2954–2962. [Google Scholar] [CrossRef]
- Antman, E.M.; Lau, J.; Kupelnick, B.; Mosteller, F.; Chalmers, T.C. A comparison of results of meta-analyses of randomized control trials and recommendations of clinical experts: Treatments for myocardial infarction. JAMA 1992, 268, 240–248. [Google Scholar] [CrossRef] [PubMed]
| Study | NTAP Specifications | NTAP Application | Adhesive | μTBS | Main Outcome | ||||
|---|---|---|---|---|---|---|---|---|---|
| Working Gas | Power Input | Time | Distance | - | Sample Size | Aging | - | ||
| 1. | Han et al., 2019 [33] | Helium Flow rate (FR): 5000 sccm | 3 W | 30 s | 5 mm | Adper Single Bond 2 Adhesive, 3M ESPE; St Paul, MN, USA. | (n = 6) Tooth | 24 h 10,000 Thermocycling (TC) | NTAP treatment enhanced resin-dentin μTBS, at 24 h and after thermocycling. |
| 2. | Ayres et al., 2018 [34] | Argon FR:5000 sccm | N/A | 10, 30 s | 10 mm | Scotchbond Universal, 3M ESPE; St Paul, MN, USA. | (n = 8) Tooth | One week Two years water storage (WS) | NTAP treatment (30 s) enhanced resin-dentin μTBS for ER mode after aging. NTAP treatment had no significant effect on resin–dentin μTBS for SE mode, at 1 week and after aging. |
| 3. | Ayres et al., 2018 [35] | Argon FR:5000 sccm | N/A | 10, 30 s | 10 mm | Scotchbond Universal 3M ESPE; St Paul, MN, USA. | (n = 8) Tooth | 24 h One year WS One year simulated pulpal pressure | NTAP treatment had no significant effect on resin–dentin μTBS for ER or SE modes, at 24 h or after aging using direct water storage. NTAP treatment enhanced resin-dentin μTBS for ER or SE modes, after aging for 1 year under simulated pulpal pressure. |
| 4. | Zhu et al., 2018 [36] | Helium FR:2000 sccm (Conventional) FR:4000 sccm (Modified) | Conventional: Vpp = 67 kV, Frequency = 13.56 MHz Modified: 15 W, Frequency = 13.56 MHz | 5, 10 s (conventional) 15, 30, 45, 60 s (modified) | 10 mm | Adper Single Bond Plus, 3M ESPE; St. Paul, MN, USA. | (n = 4) Tooth | 24 h 50,000 TC | Modified NTAP drying enhanced resin-dentin μTBS, at 24 h and after aging. Conventional NTAP (5 s) enhanced resin-dentin μTBS, while dentin treatment for 10 s had a negative effect on μTBS, at 24 h and after aging. |
| 5. | Zhu et al., 2018 [37] | Helium FR:4000 sccm | 15 W Frequency = 13.56 MHz | N/A | N/A | Adper Single Bond Plus, 3M ESPE; St. Paul, MN, USA. | (n = 4) Tooth | 24 h One year (chloramine solution storage) | NTAP drying enhanced resin-dentin μTBS, at 24 h and after aging. The highest μTBS was obtained at 30–45 s. |
| 6. | Kim et al., 2016 [38] | Helium FR:2000 sccm | 0.3 W | 20 s | 5 mm | Adper Single Bond 2, 3M ESPE; St Paul, MN, USA. | (n = 24) Hour-glass slabs | 24 h | NTAP drying enhanced resin-dentin μTBS. The rewetting after NTAP negatively affected the resin-dentin μTBS. |
| 7. | Hirata et al., 2016 [39] | Argon FR:5000 sccm | 8 W Frequency:1.1 MHz, 2 to 6 kV peak-to-peak | 30 s | 15 mm | Optibond FL, Kerr, Orange, CA, USA. XP Bond, Dentsply De Trey; Konstanz, Germany. | (n = 6) Tooth | One week WS One year WS | NTAP treatment before acid etching had no significant effect on resin-dentin μTBS of two-step ER adhesive, at 24 h or after aging. NTAP drying enhanced resin-dentin μTBS of two-step ER adhesive, at 24 h. However, this effect was not stable after aging. |
| 8. | Abreu et al., [40] 2016 | Argon FR:N/A | 60 W | 15, 30, 45 s | N/A | Clearfil SE Bond, Kuraray Noritake Dental; Kurashiki, Japan. | (n = 5) Tooth | 48 h WS | NTAP treatment (30 s) enhanced resin-dentin μTBS, promoting chemical changes in the dentin structure. |
| 9. | Hirata et al., 2015 [27] | Argon FR:5000 sccm | 8 W Frequency:1.1 MHz, 2 to 6 kV peak-to-peak | 30 s | 15 mm | Clearfil SE Bond, Kuraray Noritake Dental; Kurashiki, Japan. Scotchbond Universal, 3M ESPE; St Paul, MN, USA. | (n = 6) Tooth | One year WS | NTAP treatment enhanced resin-dentin μTBS for the universal adhesive, at 24 h. However, this positive effect was not stable after aging. NTAP treatment had no significant effect on resin-dentin μTBS for the two-step SE adhesive, at 24 h or after aging |
| 10. | Dong et al., 2015 [41] | Argon FR:3000 sccm | 2–3 W | 30 s | N/A | OptiBond All-In-One, Kerr; Romulus, MI, USA. | (n = 8) Tooth | 24 h WS 60 days WS | NTAP treatment enhanced resin-dentin μTBS, at 24 h and 60 days. |
| 11. | Han et al., 2014 [42] | Helium FR:2000 sccm | Conventional: 21.6 kW h Pulsed: 1.1 kW h | 30 s | 5 mm | Scotchbond Multi-Purpose Plus adhesive system, 3M ESPE; St Paul, MN, USA. | (n = 20) Hour-glass slabs | 24 h 5000 TC | Both types of NTAP drying enhanced resin-dentin μTBS at 24 h and after thermocycling. |
| 12. | Dong et al., 2013 [43] | Argon FR:3000 sccm | 2–3 W | 30 s | N/A | Adper Single Bond Plus, 3M ESPE; St. Paul, MN, USA. | (n = 8) Tooth | 24 h | NTAP drying enhanced resin-dentin μTBS. |
| 13. | Ritts et al., 2010 [44] | Argon FR:2500 sccm | 5 W | 30, 100, 300 s | N/A | Adaper Single bond plus, 3M ESPE; St Paul, MN, USA. | N/A | 24 h | NTAP drying (30 s) enhanced resin-dentin μTBS. Prolonged plasma treatment could lead to a weak interface and deteriorated dentin micromechanical properties. |
| Study | Adhesive Procedures | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Substrate (Dentin) | Acid Etching/Time | Dentin Moisture | NTAP Function | Rewetting | Adhesive | Bonded Material | ||||
| Application | Air-Drying | Light-Curing | ||||||||
| 1. | Han et al. 2019 [33] | NA | 35% H3PO4/ | Wet | Drying of demineralized dentin | No | N/A | Gently air-dried | 10 s | RBC |
| 2. | Ayres et al., 2018 [34] | Sound | 34% H3PO4/(ER), No (SE) | N/A | Dentin surface treatment Drying of demineralized dentin | No | Manufacturer’s Instructions | Manufacturer’s Instructions | Manufacturer’s Instructions | RBC |
| 3. | Ayres et al., 2018 [35] | Sound | 34% H3PO4/(ER), No (SE) | Blot-dried | Dentin surface treatment Drying of demineralized dentin | No | Manufacturer’s Instructions | Manufacturer’s Instructions | 10 s | RBC |
| 4. | Zhu et al., 2018 [36] | Sound | 32% H3PO4 | Blot-dried | Drying of demineralized dentin | Yes | N/A | Air-thined | 15 s | RBC |
| 5. | Zhu et al., 2018 [37] | Sound | 32% H3PO4 | Blot-dried | Drying of demineralized dentin | Yes | N/A | Air-thined | 15 s | RBC |
| 6. | Kim et al., 2016 [38] | Sound | 35% H3PO4 | N/A | Drying of demineralized dentin | Yes/No | N/A | Gently air-dried | 10 s | RBC |
| 7. | Hirata et al., 2016 [39] | Sound | 35% H3PO4 | N/A | Drying of demineralized dentin | No | Manufacturer’s Instructions | Manufacturer’s Instructions | Manufacturer’s Instructions | RBC |
| 8. | Abreu et al., 2016 [40] | 2.5% NaOCl | No | N/A | Dentin surface treatment | No | Manufacturer’s Instructions | Manufacturer’s Instructions | Manufacturer’s Instructions | RBC |
| 9. | Hirata et al., 2015 [27] | Sound | No | N/A | Dentin surface treatment | No | Manufacturer’s Instructions | Manufacturer’s Instructions | Manufacturer’s Instructions | RBC |
| 10. | Dong et al., 2015 [41] | Sound | No | Moist | Dentin surface treatment | Yes | Manufacturer’s Instructions | Manufacturer’s Instructions | 10 s | RBC |
| 11. | Han et al., 2014 [42] | Sound | 35% H3PO4 | Blot-dried | Drying of demineralized dentin | Yes | Manufacturer’s Instructions | Manufacturer’s Instructions | 10 s | RBC |
| 12. | Dong et al., 2013 [43] | Sound | 37% H3PO4 | Blot-dried | Drying of demineralized dentin | Yes | N/A | N/A | 10 s | RBC |
| 13. | Ritts et al., 2010 [44] | Sound | 37% H3PO4 | Blot-dried | Drying of demineralized dentin | Yes | N/A | N/A | 10 s | RBC |
| Study | Randomization | Caries Free | Similar Dimensions Samples | Sample Size Calculation | Blinding of Examiner | Failure Mode | NTAP Specifications and Application | Risk of Bias | |
|---|---|---|---|---|---|---|---|---|---|
| 1. | Han et al., 2019 [33] | Yes | No | Yes | No | No | Yes | Yes | Medium |
| 2. | Ayres et al., 2018 [34] | No | Yes | Yes | No | No | Yes | Yes | Medium |
| 3. | Ayres et al., 2018 [35] | Yes | Yes | Yes | No | No | Yes | Yes | Medium |
| 4. | Zhu et al., 2018 [36] | Yes | Yes | Yes | No | No | No | Yes | Medium |
| 5. | Zhu et al., 2018 [37] | Yes | Yes | Yes | No | No | No | No | Medium |
| 6. | Kim et al., 2016 [38] | Yes | Yes | Yes | No | No | Yes | Yes | Medium |
| 7. | Hirata et al., 2016 [39] | Yes | Yes | Yes | No | No | Yes | Yes | Medium |
| 8. | Abreu et al., 2016 [40] | No | No | Yes | Yes | No | Yes | No | Medium |
| 9. | Hirata et al., 2015 [27] | Yes | Yes | Yes | No | No | Yes | Yes | Medium |
| 10. | Dong et al., 2015 [41] | Yes | Yes | Yes | No | No | Yes | No | Medium |
| 11. | Han et al., 2014 [42] | Yes | Yes | Yes | No | No | Yes | Yes | Medium |
| 12. | Dong et al., 2013 [43] | No | Yes | Yes | No | No | Yes | No | Medium |
| 13. | Ritts et al., 2010 [44] | No | Yes | Yes | No | No | Yes | No | Medium |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Awad, M.M.; Alhalabi, F.; Alshehri, A.; Aljeaidi, Z.; Alrahlah, A.; Özcan, M.; Hamama, H.H. Effect of Non-Thermal Atmospheric Plasma on Micro-Tensile Bond Strength at Adhesive/Dentin Interface: A Systematic Review. Materials 2021, 14, 1026. https://doi.org/10.3390/ma14041026
Awad MM, Alhalabi F, Alshehri A, Aljeaidi Z, Alrahlah A, Özcan M, Hamama HH. Effect of Non-Thermal Atmospheric Plasma on Micro-Tensile Bond Strength at Adhesive/Dentin Interface: A Systematic Review. Materials. 2021; 14(4):1026. https://doi.org/10.3390/ma14041026
Chicago/Turabian StyleAwad, Mohamed M., Feras Alhalabi, Abdullah Alshehri, Zaid Aljeaidi, Ali Alrahlah, Mutlu Özcan, and Hamdi Hosni Hamama. 2021. "Effect of Non-Thermal Atmospheric Plasma on Micro-Tensile Bond Strength at Adhesive/Dentin Interface: A Systematic Review" Materials 14, no. 4: 1026. https://doi.org/10.3390/ma14041026
APA StyleAwad, M. M., Alhalabi, F., Alshehri, A., Aljeaidi, Z., Alrahlah, A., Özcan, M., & Hamama, H. H. (2021). Effect of Non-Thermal Atmospheric Plasma on Micro-Tensile Bond Strength at Adhesive/Dentin Interface: A Systematic Review. Materials, 14(4), 1026. https://doi.org/10.3390/ma14041026








