Comparison between Tissue Adhesive Cyanoacrylate and Suture for Palatal Fibromucosa Healing: A Randomized Controlled Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Patient Selection
2.2. Surgical Protocol
2.3. Study Variables
2.4. Statistical Analysis
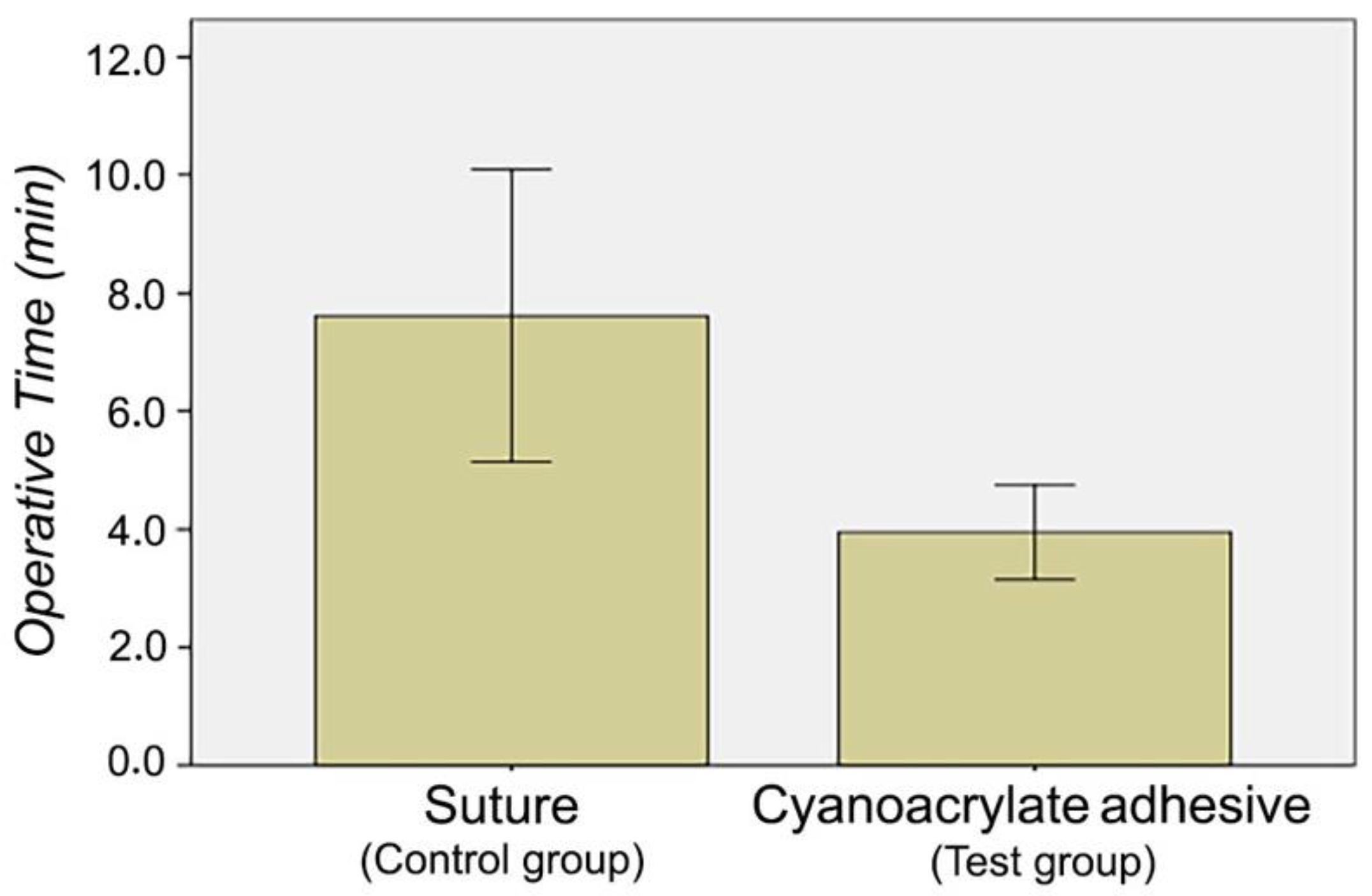
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cosyn, J.; Eeckhout, C.; Christiaens, V.; Eghbali, A.; Vervaeke, S.; Younes, F.; De Bruyckere, T. A Multi-Centre Randomized Controlled Trial Comparing Connective Tissue Graft with Collagen Matrix to Increase Soft Tissue Thickness at the Buccal Aspect of Single Implants: 3-Month Results. J. Clin. Periodontol. 2021, 3, 1–14. [Google Scholar] [CrossRef]
- Zucchelli, G.; Mele, M.; Stefanini, M.; Mazzotti, C.; Marzadori, M.; Montebugnoli, L.; de Sanctis, M. Patient Morbidity and Root Coverage Outcome after Subepithelial Connective Tissue and De-Epithelialized Grafts: A Comparative Randomized-Controlled Clinical Trial. J. Clin. Periodontol. 2010, 37, 728–738. [Google Scholar] [CrossRef]
- Burkhardt, R.; Hämmerle, C.H.F.; Lang, N.P. Research Group on Oral Soft Tissue Biology & Wound Healing Self-Reported Pain Perception of Patients after Mucosal Graft Harvesting in the Palatal Area. J. Clin. Periodontol. 2015, 42, 281–287. [Google Scholar] [CrossRef] [PubMed]
- Pall, E.; Cenariu, M.; Kasaj, A.; Florea, A.; Soancă, A.; Roman, A.; Georgiu, C. New Insights into the Cellular Makeup and Progenitor Potential of Palatal Connective Tissues. Microsc. Res. Tech. 2017, 80, 1270–1282. [Google Scholar] [CrossRef]
- Maino, G.N.E.; Valles, C.; Santos, A.; Pascual, A.; Esquinas, C.; Nart, J. Influence of Suturing Technique on Wound Healing and Patient Morbidity after Connective Tissue Harvesting. A Randomized Clinical Trial. J. Clin. Periodontol. 2018, 45, 977–985. [Google Scholar] [CrossRef] [PubMed]
- Ozcan, M.; Ucak, O.; Alkaya, B.; Keceli, S.; Seydaoglu, G.; Haytac, M.C. Effects of Platelet-Rich Fibrin on Palatal Wound Healing After Free Gingival Graft Harvesting: A Comparative Randomized Controlled Clinical Trial. Int. J. Periodontics Restor. Dent. 2017, 37, e270–e278. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tavelli, L.; Ravidà, A.; Saleh, M.H.A.; Maska, B.; Del Amo, F.S.-L.; Rasperini, G.; Wang, H.-L. Pain Perception Following Epithelialized Gingival Graft Harvesting: A Randomized Clinical Trial. Clin. Oral Investig. 2019, 23, 459–468. [Google Scholar] [CrossRef] [PubMed]
- Binnie, W.H.; Forrest, J.O. A Study of Tissue Response to Cyanoacrylate Adhesive in Periodontal Surgery. J. Periodontol. 1974, 45, 619–625. [Google Scholar] [CrossRef]
- Vastani, A.; Maria, A. Healing of Intraoral Wounds Closed Using Silk Sutures and Isoamyl 2-Cyanoacrylate Glue: A Comparative Clinical and Histologic Study. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2013, 71, 241–248. [Google Scholar] [CrossRef]
- Borie, E.; Rosas, E.; Kuramochi, G.; Etcheberry, S.; Olate, S.; Weber, B. Oral Applications of Cyanoacrylate Adhesives: A Literature Review. BioMed Res. Int. 2019, 2019, 8217602. [Google Scholar] [CrossRef] [PubMed]
- Inal, S.; Yilmaz, N.; Nisbet, C.; Güvenç, T. Biochemical and Histopathological Findings of N-Butyl-2-Cyanoacrylate in Oral Surgery: An Experimental Study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2006, 102, e14–e17. [Google Scholar] [CrossRef]
- Ochstein, A.J.; Hansen, N.M.; Swenson, H.M. A Comparative Study of Cyanoacrylate and Other Periodontal Dressings on Gingival Surgical Wound Healing. J. Periodontol. 1969, 40, 515–520. [Google Scholar] [CrossRef] [PubMed]
- Gümüş, P.; Buduneli, E. Graft Stabilization with Cyanoacrylate Decreases Shrinkage of Free Gingival Grafts. Aust. Dent. J. 2014, 59, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Stavropoulou, C.; Atout, R.N.; Brownlee, M.; Schroth, R.J.; Kelekis-Cholakis, A. A Randomized Clinical Trial of Cyanoacrylate Tissue Adhesives in Donor Site of Connective Tissue Grafts. J. Periodontol. 2019, 90, 608–615. [Google Scholar] [CrossRef]
- Edel, A. Clinical Evaluation of Free Connective Tissue Grafts Used to Increase the Width of Keratinised Gingiva. 1974. Periodontal Clin. Investig. Off. Publ. Northeast. Soc. Periodontists 1998, 20, 12–20. [Google Scholar]
- Langer, B.; Langer, L. Subepithelial Connective Tissue Graft Technique for Root Coverage. J. Periodontol. 1985, 56, 715–720. [Google Scholar] [CrossRef]
- Liu, C.-L.; Weisgold, A.S. Connective Tissue Graft: A Classification for Incision Design from the Palatal Site and Clinical Case Reports. Int. J. Periodontics Restor. Dent. 2002, 22, 373–379. [Google Scholar]
- Zuhr, O.; Bäumer, D.; Hürzeler, M. The Addition of Soft Tissue Replacement Grafts in Plastic Periodontal and Implant Surgery: Critical Elements in Design and Execution. J. Clin. Periodontol. 2014, 41 (Suppl. S15), S123–S142. [Google Scholar] [CrossRef]
- Lin, J.C.-Y.; Nevins, M.; Kim, D.M. Laser De-Epithelialization of Autogenous Gingival Graft for Root Coverage and Soft Tissue Augmentation Procedures. Int. J. Periodontics Restor. Dent. 2018, 38, 405–411. [Google Scholar] [CrossRef]
- Bertl, K.; Pifl, M.; Hirtler, L.; Rendl, B.; Nürnberger, S.; Stavropoulos, A.; Ulm, C. Relative Composition of Fibrous Connective and Fatty/Glandular Tissue in Connective Tissue Grafts Depends on the Harvesting Technique but Not the Donor Site of the Hard Palate. J. Periodontol. 2015, 86, 1331–1339. [Google Scholar] [CrossRef]
- Zucchelli, G.; Mounssif, I.; Mazzotti, C.; Montebugnoli, L.; Sangiorgi, M.; Mele, M.; Stefanini, M. Does the Dimension of the Graft Influence Patient Morbidity and Root Coverage Outcomes? A Randomized Controlled Clinical Trial. J. Clin. Periodontol. 2014, 41, 708–716. [Google Scholar] [CrossRef]
- Nevins, M.; Mendoza-Azpur, G.; De Angelis, N.; Kim, D.M. The Biocompatibility of Cyanoacrylate Tissue Adhesive in Conjunction with a Collagen Membrane for Providing Soft and Hard Tissue Regeneration in Extraction Socket Preservation Procedures. Int. J. Periodontics Restor. Dent. 2018, 38, s37–s42. [Google Scholar] [CrossRef]
- Hoexter, D.L. The Sutureless Free Gingival Graft. J. Periodontol. 1979, 50, 75–78. [Google Scholar] [CrossRef]
- Soni, A.; Narula, R.; Kumar, A.; Parmar, M.; Sahore, M.; Chandel, M. Comparing Cyanoacrylate Tissue Adhesive and Conventional Subcuticular Skin Sutures for Maxillofacial Incisions—A Prospective Randomized Trial Considering Closure Time, Wound Morbidity, and Cosmetic Outcome. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2013, 71, 2152.e1–2152.e8. [Google Scholar] [CrossRef]
- Tavelli, L.; Asa’ad, F.; Acunzo, R.; Pagni, G.; Consonni, D.; Rasperini, G. Minimizing Patient Morbidity Following Palatal Gingival Harvesting: A Randomized Controlled Clinical Study. Int. J. Periodontics Restor. Dent. 2018, 38, e127–e134. [Google Scholar] [CrossRef] [PubMed]
- Oladega, A.A.; James, O.; Adeyemo, W.L. Cyanoacrylate Tissue Adhesive or Silk Suture for Closure of Surgical Wound Following Removal of an Impacted Mandibular Third Molar: A Randomized Controlled Study. J. Cranio-Maxillo-fac. Surg. Off. Publ. Eur. Assoc. Cranio-Maxillo-fac. Surg. 2019, 47, 93–98. [Google Scholar] [CrossRef]
- Griffin, T.J.; Cheung, W.S.; Zavras, A.I.; Damoulis, P.D. Postoperative Complications Following Gingival Augmentation Procedures. J. Periodontol. 2006, 77, 2070–2079. [Google Scholar] [CrossRef] [PubMed]
- Escobar, M.; Pauletto, P.; Benfatti, C.A.M.; Cruz, A.C.C.; Flores-Mir, C.; Henriques, B.A.P.C. Effect of Cyanoacrylate Tissue Adhesive in Postoperative Palatal Pain Management: A Systematic Review. Clin. Oral Investig. 2020, 25, 3609–3622. [Google Scholar] [CrossRef] [PubMed]
- Soileau, K.M.; Brannon, R.B. A Histologic Evaluation of Various Stages of Palatal Healing Following Subepithelial Connective Tissue Grafting Procedures: A Comparison of Eight Cases. J. Periodontol. 2006, 77, 1267–1273. [Google Scholar] [CrossRef]
- Orozco-Razón, L.F.; Millán-Guerrero, R.O.; Vera-Rodríguez, S.E. Cyanoacrylate compared with traditional surgery in tension-free incision closure. Gac. Med. Mex. 2002, 138, 505–509. [Google Scholar]
- Galil, K.A.; Schofield, I.D.; Wright, G.Z. Effect of N-Butyl-2-Cyanoacrylate (Histoacryl Blue) on the Healing of Skin Wounds. J. Can. Dent. Assoc. 1984, 50, 565–569. [Google Scholar]
- Pagano, S.; Negri, P.; Coniglio, M.; Bruscoli, S.; Di Michele, A.; Marchetti, M.C.; Valenti, C.; Gambelunghe, A.; Fanasca, L.; Billi, M.; et al. Heat-Not-Burn Tobacco (IQOS), Oral Fibroblasts and Keratinocytes: Cytotoxicity, Morphological Analysis, Apoptosis and Cellular Cycle. An in Vitro Study. J. Periodontal Res. 2021, 56, 917–928. [Google Scholar] [CrossRef] [PubMed]
- Da Silva Neves, F.L.; Silveira, C.A.; Dias, S.B.F.; Santamaria Júnior, M.; de Marco, A.C.; Kerbauy, W.D.; de Melo Filho, A.B.; Jardini, M.A.N.; Santamaria, M.P. Comparison of Two Power Densities on the Healing of Palatal Wounds after Connective Tissue Graft Removal: Randomized Clinical Trial. Lasers Med. Sci. 2016, 31, 1371–1378. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Suture (n = 14) | Cyanoacrylate Tissue Adhesive (n = 10) | ||||||
|---|---|---|---|---|---|---|---|
| Pain | Median | Mean | SD | Median | Mean | SD | p-Value * |
| Day 1 | 3.00 | 4.21 | 2.89 | 3.50 | 3.20 | 1.87 | 0.625 |
| Day 2 | 2.00 | 2.79 | 2.29 | 3.00 | 2.30 | 1.89 | 0.841 |
| Day 3 | 1.50 | 2.14 | 1.99 | 2.00 | 1.90 | 1.97 | 0.796 |
| Day 4 | 2.00 | 2.00 | 1.62 | 2.50 | 2.10 | 2.08 | 0.977 |
| Day 5 | 2.50 | 2.14 | 1.66 | 2.00 | 1.80 | 2.39 | 0.312 |
| Day 6 | 1.50 | 2.21 | 2.19 | 0.50 | 1.30 | 2.45 | 0.122 |
| Day 7 | 1.00 | 1.29 | 1.33 | 0.00 | 1.10 | 2.47 | 0.259 |
| Day 14 | 0.00 | 0.50 | 0.94 | 0.00 | 0.70 | 2.21 | 0.546 |
| Suture (n = 14) | Cyanocrylate Tissue Adhesive (n = 10) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| None | Mild | Marked | Extreme | None | Mild | Marked | Extreme | p-Value * | |
| 7 days | 0% | 28.6% | 71% | 0% | 0% | 50% | 50% | 0% | 0.403 |
| 14 days | 14.3% | 57.1% | 28.6% | 0% | 10% | 80% | 10% | 0% | 0.470 |
| 21 days | 57.1% | 42.9% | 0% | 0% | 70% | 30% | 0% | 0% | 0.678 |
| Suture (n = 14) | Cyanoacrylate Tissue Adhesive (n = 10) | ||||
|---|---|---|---|---|---|
| Bleeding | NO | YES | NO | YES | p-Value * |
| 24 h | 42.9% | 57.1% | 90% | 10% | 0.033 |
| 48 h | 78.6% | 21% | 100% | 0% | 0.239 |
| 72 h | 85.7% | 14.3% | 100% | 0% | 0.493 |
| Suture (n = 14) | Cyanoacrylate Tissue Adhesive (n = 10) | ||
|---|---|---|---|
| Epithelium Formation | % | % | p-Value * |
| 14 days | 21.4% | 30% | 0.665 |
| 21 days | 78.6% | 70% | 0.665 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Castro-Gaspar, C.; Olmedo-Gaya, M.V.; Romero-Olid, M.N.; Lisbona-Gonzalez, M.J.; Vallecillo-Rivas, M.; Reyes-Botella, C. Comparison between Tissue Adhesive Cyanoacrylate and Suture for Palatal Fibromucosa Healing: A Randomized Controlled Study. Materials 2021, 14, 7009. https://doi.org/10.3390/ma14227009
Castro-Gaspar C, Olmedo-Gaya MV, Romero-Olid MN, Lisbona-Gonzalez MJ, Vallecillo-Rivas M, Reyes-Botella C. Comparison between Tissue Adhesive Cyanoacrylate and Suture for Palatal Fibromucosa Healing: A Randomized Controlled Study. Materials. 2021; 14(22):7009. https://doi.org/10.3390/ma14227009
Chicago/Turabian StyleCastro-Gaspar, Carlota, Maria Victoria Olmedo-Gaya, Maria Nuria Romero-Olid, Maria Jesús Lisbona-Gonzalez, Marta Vallecillo-Rivas, and Candela Reyes-Botella. 2021. "Comparison between Tissue Adhesive Cyanoacrylate and Suture for Palatal Fibromucosa Healing: A Randomized Controlled Study" Materials 14, no. 22: 7009. https://doi.org/10.3390/ma14227009
APA StyleCastro-Gaspar, C., Olmedo-Gaya, M. V., Romero-Olid, M. N., Lisbona-Gonzalez, M. J., Vallecillo-Rivas, M., & Reyes-Botella, C. (2021). Comparison between Tissue Adhesive Cyanoacrylate and Suture for Palatal Fibromucosa Healing: A Randomized Controlled Study. Materials, 14(22), 7009. https://doi.org/10.3390/ma14227009








