Treatment Prognosis of Restored Teeth with Crown Lengthening vs. Deep Margin Elevation: A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Protocol
2.2. Eligibility Criteria
2.2.1. Inclusion Criteria
- Clinical trial studies with a follow-up period of more than six months.
- Studies reporting the baseline and post-treatment measurements.
- Clinical measurements were obtained through the reference method.
- Studies published in the English language.
2.2.2. Exclusion Criteria
- Case reports, editorials, and clinical letters.
- Studies without subsequent restorative needs were also excluded on account of the emblematic differences in typical surgical sites and etiology.
2.3. Search Strategy and Study Selection
2.4. Quality Assessment
2.5. Data Extraction and Synthesis
3. Results
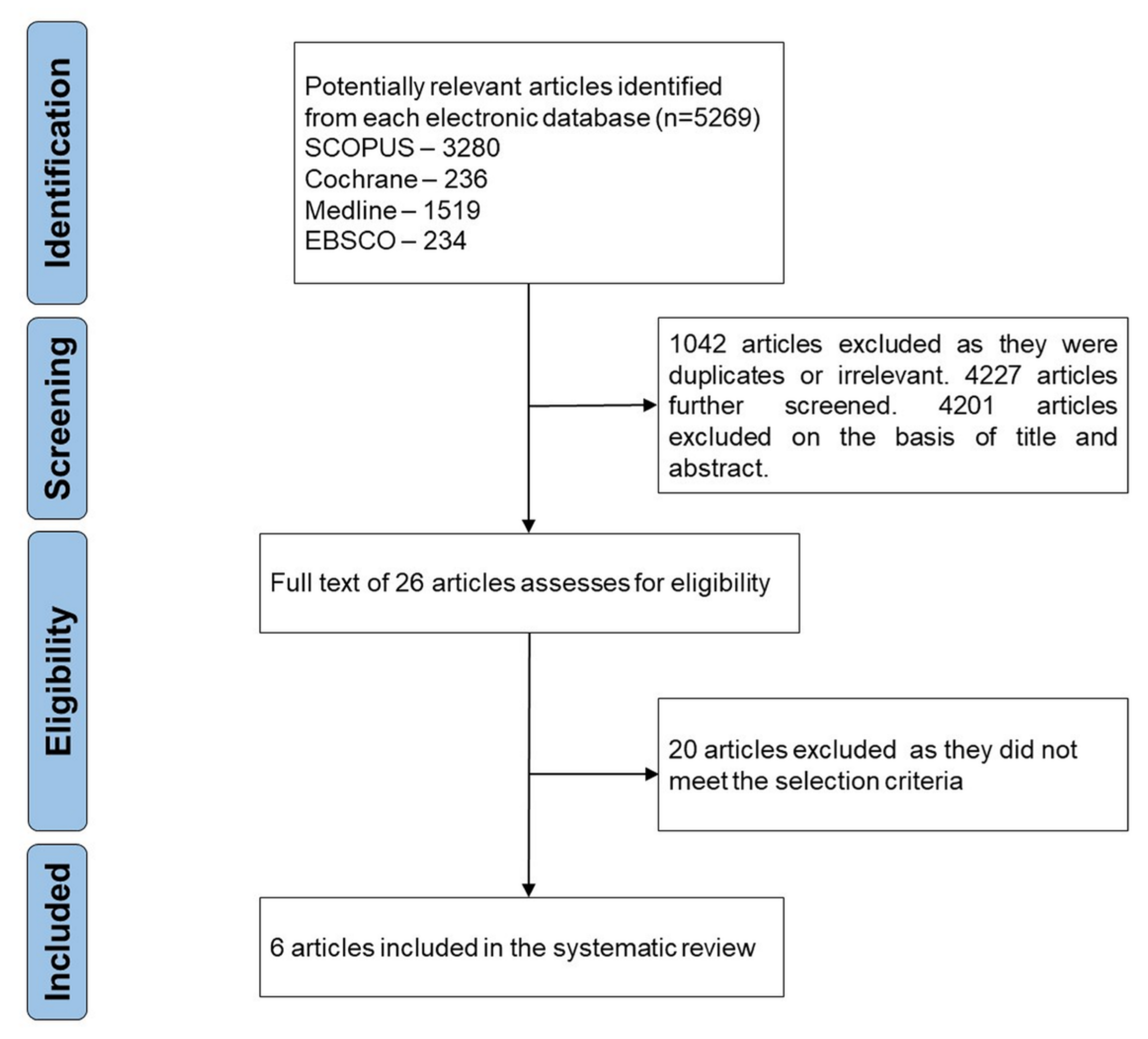
3.1. Study Selection
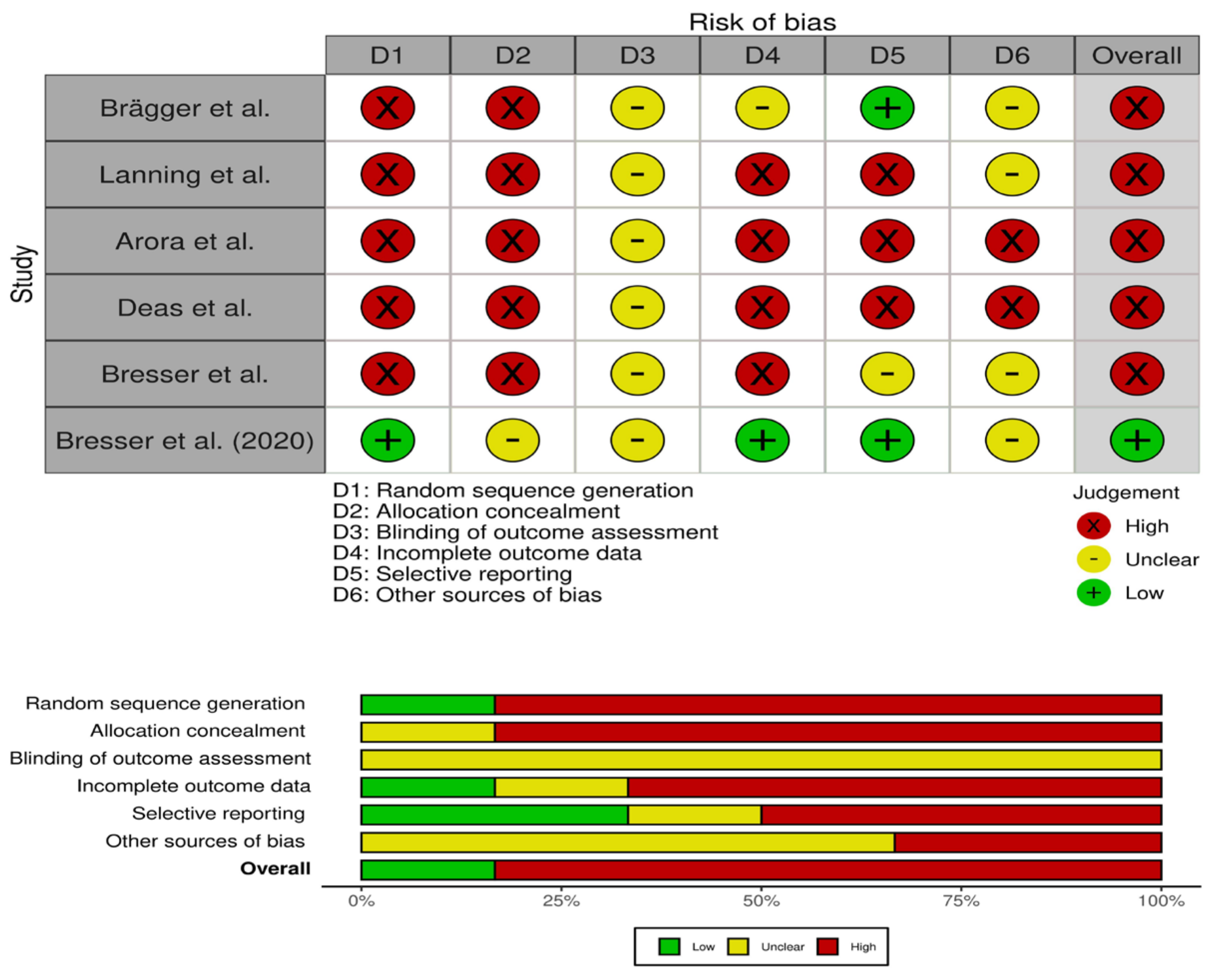
3.2. Quality Assessment
3.3. Characteristics of the Studies
| Study Year | Brägger et al. [21] 1992 | Lanning et al. [22] 2003 | Arora et al. [11] 2013 | Deas et al. [23] 2004 | ||||
|---|---|---|---|---|---|---|---|---|
| Study type | Clinical analysis | Clinical Evaluation | Clinical study | Clinical study | ||||
| Sample size (Gender) | 25 (NAD) 43 test and 42 control teeth | 23 18 (NAD) | 64 patients (M = 38 F = 26) | 25 patients (M = 18 F = 7) | ||||
| Mean Age (range) | 20–81 years (61) | 28–72 years (39) | 18–63 (34.5) | (NAD) | ||||
| Crown length after surgery (mm) | TT Control | 1.3 - | TT AA NA | - - - | TT AA NA | 2.5 + 0.72 1.89 + 0.83 1.18 + 0.73 | TT AA NA | 2.27 + 1.10 2.18 + 0.98 1.06 + 1.07 |
| Change in crown length after 6 months follow up (mm) | TT Control | 1.4 0.2 | TT AA NA | 3.33 + 0.15 2.82 + 0.24 2.78 + 0.28 | TT AA NA | 1.72 + 0.80 1.41 + 0.88 0.72 + 0.58 | TT AA NA | 1.69 + 1.01 1.43 + 0.96 0.84 + 0.85 |
| p-value | < 0.05 (for TT) | < 0.05 | < 0.005 | |||||
| Baseline Free gingival margin position (mm) | TT Control | 6.02 + 2.39 5.83 + 2.15 | TT AA NA | 4.57 + 0.29 4.65 + 0.24 4.51 + 0.26 | TT AA NA | - | TT AA NA | - |
| After surgery gingival margin position (mm) | TT Control | 7.34 + 2.30 - | TT AA NA | - - | TT AA NA | TT AA NA | 2.27 + 1.10 2.18 + 0.98 1.06 + 1.07 | |
| p value (baseline and after surgery) | p ≤ 0.05 | |||||||
| After 6 months follow up gingival margin position (mm) | TT Control | 7.39 + 2.00 6.01 + 1.93 | TT AA NA | 3.33 + 0.15 2.82 + 0.24 2.78 + 0.28 | TT AA NA | 1.72 + 0.11 1.41 + 0.12 0.72 + 0.08 | TT AA NA | 1.57 + 1.01 1.30 + 0.96 0.76 + 0.85 |
| p-value (baseline and after 6 months) | TT | p ≤ 0.05 | TT AA NA | p < 0.0001 p < 0.0001 p < 0.0001 | TT AA NA | p < 0.005 p < 0.005 p < 0.005 | ||
| BW and SGT at baseline (mm) | TT Control | - | TT AA NA | 2.26 + 0.13 2.23 ± 0.11 2.36 ± 0.08 | TT AA NA | 3.50 ± 0.83 3.73 ± 0.82 3.62 ± 0.64 | TT AA NA | - |
| BW and SGT at 6 months (mm) | TT Control | - | TT AA NA | −0.07 ± 0.09 −0.15 ± 0.07 −0.23 ± 0.06 | TT AA NA | −0.44 ± 0.12 −0.30 ± 0.12 −0.48 ± 0.08 | TT AA NA | - |
| p-value (baseline and after 6 months) | TT (not different from baseline) AA (p < 0.05) Na (p < 0.05) | TT (p = 0.001) AA (p = 0.049) NA (p = 0.000) | ||||||
| Bone level changes at 6 months (mm) | TT Control | - | TT AA NA | 3.50 ± 0.59 2.54 ± 0.76 2.47 ± 0.88 | TT AA NA | 1.27 ± 0.10 1.11 ± 0.08 0.23 ± 0.06 | TT AA NA | - |
| p-value (from baseline and 6 months) | TT (p < 0.0001) AA (p < 0.0001) NA (p < 0.0001) | TT AA NA | (ND) | |||||
4. Discussion
4.1. Completeness and Applicability of Evidence
4.2. Quality of Evidence
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Magne, P.; Spreafico, R.C. Deep Margin Elevation: A Paradigm Shift. Am. J. Esthet. Dent. 2012, 2, 86–96. [Google Scholar]
- Magne, P.; Dietschi, D.; Holz, J. Esthetic restorations for posterior teeth: Practical and clinical considerations. Int. J. Periodontics Restor. Dent. 1996, 16, 104–119. [Google Scholar] [PubMed]
- Veneziani, M. Adhesive restorations in the posterior area with subgingival cervical margins: New classification and differentiated treatment approach. Eur. J. Esthet. Dent. 2010, 5, 50–76. [Google Scholar]
- Magne, P.; So, W.-S.; Cascione, D. Immediate dentin sealing supports delayed restoration placement. J. Prosthet. Dent. 2007, 98, 166–174. [Google Scholar] [CrossRef]
- Fedorowicz, Z.; Carter, B.; de Souza, R.F.; de Andrade Lima Chaves, C.; Nasser, M.; Sequeira-Byron, P. Single crowns versus conventional fillings for the restoration of root filled teeth. Cochrane Database Syst. Rev. 2012, 16, CD009109. [Google Scholar] [CrossRef] [Green Version]
- Skupien, J.A.; Cenci, M.S.; Opdam, N.J.; Kreulen, C.M.; Huysmans, M.-C.; Pereira-Cenci, T. Crown vs. composite for post-retained restorations: A randomized clinical trial. J. Dent. 2016, 48, 34–39. [Google Scholar] [CrossRef]
- De Carvalho, M.A.; Lazari, P.C.; Gresnigt, M.; Del Bel Cury, A.A.; Magne, P. Current options concerning the endodontically-treated teeth restoration with the adhesive approach. Braz. Oral Res. 2018, 32, e74. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arora, R.; Narula, S.C.; Sharma, R.K.; Tewari, S. Evaluation of supracrestal gingival tissue after surgical crown lengthening: A 6-month clinical study. J. Periodontol. 2013, 84, 934–940. [Google Scholar] [CrossRef]
- Herrero, F.; Scott, J.B.; Maropis, P.S.; Yukna, R.A. Clinical comparison of desired versus actual amount of surgical crown lengthening. J. Periodontol. 1995, 66, 568–571. [Google Scholar] [CrossRef]
- Abou-Arraj, R.V.; Majzoub, Z.A.K.; Holmes, C.M.; Geisinger, M.L.; Geurs, N.C. Healing Time for Final Restorative Therapy After Surgical Crown Lengthening Procedures: A Review of Related Evidence. Clin. Adv. Periodontics 2015, 5, 131–139. [Google Scholar] [CrossRef]
- Shobha, K.S.; Mahantesha, H.S.; Mani, R.; Kranti, K. Clinical evaluation of the biological width following surgical crown-lengthening procedure: A prospective study. J. Indian Soc. Periodontol. 2010, 14, 160–167. [Google Scholar] [CrossRef]
- Dablanca-Blanco, A.B.; Blanco-Carrión, J.; Martín-Biedma, B.; Varela-Patiño, P.; Bello-Castro, A.; Castelo-Baz, P. Management of large class II lesions in molars: How to restore and when to perform surgical crown lengthening? Restor. Dent. Endod. 2017, 42, 240–252. [Google Scholar] [CrossRef] [Green Version]
- Neymark, A. An Alternative to Surgical Crown Lengthening: Margin Elevation Using a Two-Matrix System. 2018. Available online: https://www.perioimplantadvisory.com/restorative-dentistry/article/16412250/an-alternative-to-surgical-crown-lengthening-margin-elevation-using-a-twomatrix-system (accessed on 20 September 2021).
- Sarfati, A.; Tirlet, G. Deep margin elevation versus crown lengthening: Biologic width revisited. Int. J. Esthet. Dent. 2018, 13, 334–356. [Google Scholar]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions; John Wiley & Sons: Hoboken, NJ, USA, 2019; pp. 1–694. [Google Scholar] [CrossRef]
- Brägger, U.; Lauchenauer, D.; Lang, N.P. Surgical lengthening of the clinical crown. J. Clin. Periodontol. 1992, 19, 58–63. [Google Scholar] [CrossRef] [PubMed]
- Lanning, S.K.; Waldrop, T.C.; Gunsolley, J.C.; Maynard, J.G. Surgical crown lengthening: Evaluation of the biological width. J. Periodontol. 2003, 74, 468–474. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Deas, D.E.; Moritz, A.J.; McDonnell, H.T.; Powell, C.A.; Mealey, B.L. Osseous surgery for crown lengthening: A 6-month clinical study. J. Periodontol. 2004, 75, 1288–1294. [Google Scholar] [CrossRef] [PubMed]
- Bresser, R.A.; Gerdolle, D.; van den Heijkant, I.A.; Sluiter-Pouwels, L.M.A.; Cune, M.S.; Gresnigt, M.M.M. Up to 12 years clinical evaluation of 197 partial indirect restorations with deep margin elevation in the posterior region. J. Dent. 2019, 91, 103227. [Google Scholar] [CrossRef]
- Bresser, R.A.; van de Geer, L.; Gerdolle, D.; Schepke, U.; Cune, M.S.; Gresnigt, M.M.M. Influence of Deep Margin Elevation and preparation design on the fracture strength of indirectly restored molars. J. Mech. Behav. Biomed. Mater. 2020, 110, 103950. [Google Scholar] [CrossRef]
- Pontoriero, R.; Carnevale, G. Surgical crown lengthening: A 12-month clinical wound healing study. J. Periodontol. 2001, 72, 841–848. [Google Scholar] [CrossRef]
- Marzadori, M.; Stefanini, M.; Sangiorgi, M.; Mounssif, I.; Monaco, C.; Zucchelli, G. Crown lengthening and restorative procedures in the esthetic zone. Periodontology 2000 2018, 77, 84–92. [Google Scholar] [CrossRef]
- Oakley, E.; Rhyu, I.C.; Karatzas, S.; Gandini-Santiago, L.; Nevins, M.; Caton, J. Formation of the biologic width following crown lengthening in nonhuman primates. Int. J. Periodontics Restor. Dent. 1999, 19, 529–541. [Google Scholar]
- Planciunas, L.; Puriene, A.; Mackeviciene, G. Surgical lengthening of the clinical tooth crown. Stomatologija 2006, 8, 88–95. [Google Scholar] [PubMed]
- Fardal, Ø.; Grytten, J. A comparison of teeth and implants during maintenance therapy in terms of the number of disease-free years and costs—An in vivo internal control study. J. Clin. Periodontol. 2013, 40, 645–651. [Google Scholar] [CrossRef] [PubMed]
- Dreyer, H.; Grischke, J.; Tiede, C.; Eberhard, J.; Schweitzer, A.; Toikkanen, S.E.; Glöckner, S.; Krause, G.; Stiesch, M. Epidemiology and risk factors of peri-implantitis: A systematic review. J. Periodontal Res. 2018, 53, 657–681. [Google Scholar] [CrossRef] [PubMed]
- Ilgenstein, I.; Zitzmann, N.U.; Bühler, J.; Wegehaupt, F.J.; Attin, T.; Weiger, R.; Krastl, G. Influence of proximal box elevation on the marginal quality and fracture behavior of root-filled molars restored with CAD/CAM ceramic or composite onlays. Clin. Oral Investig. 2015, 19, 1021–1028. [Google Scholar] [CrossRef] [Green Version]
- Dibart, S.; Capri, D.; Kachouh, I.; Van Dyke, T.; Nunn, M.E. Crown lengthening in mandibular molars: A 5-year retrospective radiographic analysis. J. Periodontol. 2003, 74, 815–821. [Google Scholar] [CrossRef] [PubMed]
| Study Year | Bresser et al. [24] 2019 | Bresser et al. [25] 2020 | ||||||
|---|---|---|---|---|---|---|---|---|
| Study type | Clinical study | Clinical Evaluation | ||||||
| Sample size (Gender) | 197 indirect restorations in 120 patients (M = 78, F = 42) | InoD = 15 InWD = 15 OnoD = 15 OnWD = 15 (NAD) | ||||||
| Age mean (range) | 76 years (30–106 years) | - | ||||||
| Observation time (range) | 57.7 months (4–144 months) | - | ||||||
| Fracture Type N Inlay n (%) Outlay n (%) | - | I | II | III | IV | V | ||
| 2 | 16 | 6 | 0 | 36 | ||||
| 2 (100) | 14 (87.5) | 5 (83) | 0 | 9 (25) | ||||
| 0 | 2 (12.5) | 1 (17) | 0 | 27 (75) p < 0.0125 | ||||
| Repairability N Inlay n (%) Outlay n (%) | - | Repairable | Irreparable | |||||
| 24 | 36 | |||||||
| 21 (88) (p < 0.00625) | 9 (25) | |||||||
| 3 (12) | 27 (75) (p < 0.00625) | |||||||
| Failure of treatment | secondary caries (n = 5) pulpal necrosis (n = 1) periodontal breakdown (n = 1) fracture (n = 1), | |||||||
| Survival rate | 95.9% after > 10 years | |||||||
| USPHS (>3 years versus <3 years old) | more fracture of indirect restoration | χ2(2) = 42.03, p = 0.000 | ||||||
| fracture of the tooth | χ2(2) = 23.18, p = 0.000 | |||||||
| Carries | χ2(2) = 9.02, p = 0.000 | |||||||
| margin discoloration | χ2(2) = 9.02, p = 0.01 | |||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mugri, M.H.; Sayed, M.E.; Nedumgottil, B.M.; Bhandi, S.; Raj, A.T.; Testarelli, L.; Khurshid, Z.; Jain, S.; Patil, S. Treatment Prognosis of Restored Teeth with Crown Lengthening vs. Deep Margin Elevation: A Systematic Review. Materials 2021, 14, 6733. https://doi.org/10.3390/ma14216733
Mugri MH, Sayed ME, Nedumgottil BM, Bhandi S, Raj AT, Testarelli L, Khurshid Z, Jain S, Patil S. Treatment Prognosis of Restored Teeth with Crown Lengthening vs. Deep Margin Elevation: A Systematic Review. Materials. 2021; 14(21):6733. https://doi.org/10.3390/ma14216733
Chicago/Turabian StyleMugri, Maryam H., Mohammed E. Sayed, Binoy Mathews Nedumgottil, Shilpa Bhandi, A. Thirumal Raj, Luca Testarelli, Zohaib Khurshid, Saurabh Jain, and Shankargouda Patil. 2021. "Treatment Prognosis of Restored Teeth with Crown Lengthening vs. Deep Margin Elevation: A Systematic Review" Materials 14, no. 21: 6733. https://doi.org/10.3390/ma14216733
APA StyleMugri, M. H., Sayed, M. E., Nedumgottil, B. M., Bhandi, S., Raj, A. T., Testarelli, L., Khurshid, Z., Jain, S., & Patil, S. (2021). Treatment Prognosis of Restored Teeth with Crown Lengthening vs. Deep Margin Elevation: A Systematic Review. Materials, 14(21), 6733. https://doi.org/10.3390/ma14216733










