Mineral Trioxide Aggregate (MTA) Upregulates the Expression of DMP1 in Direct Pulp Capping in the Rat Molar
Abstract
:1. Introduction
2. Materials and Methods
2.1. Experimental Animals and Ethics
2.2. Rat Molars and Direct Pulp Capping
2.3. Mineral Density Images and Analysis Using Micro-Focusing CT
2.4. Histological and Immunohistochemical Studies
2.5. Real-Time RT-PCR for DMP1 mRNA Expression
2.6. Statistical Analysis
3. Results
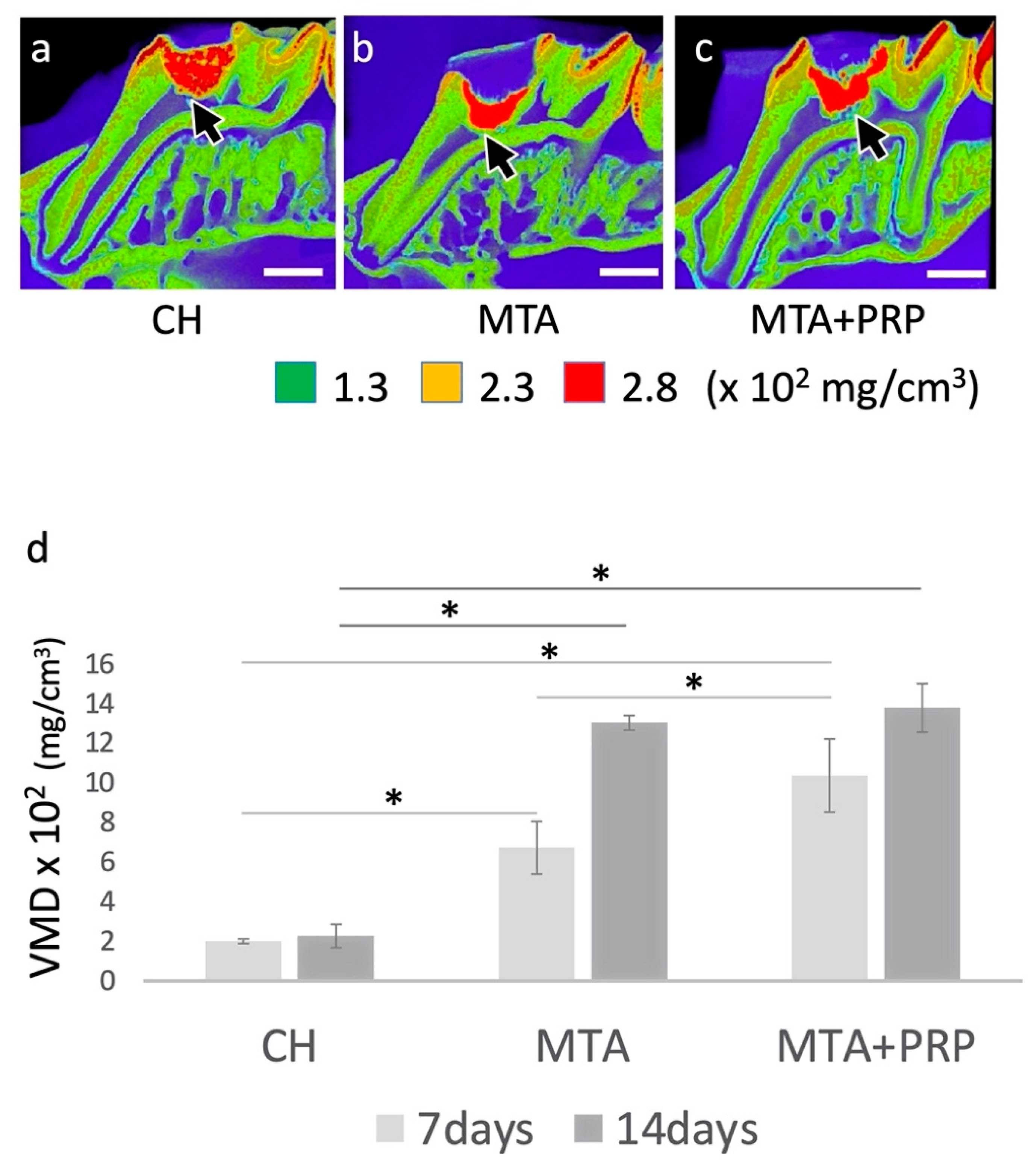
3.1. Photographic MD Images and VMD Differences
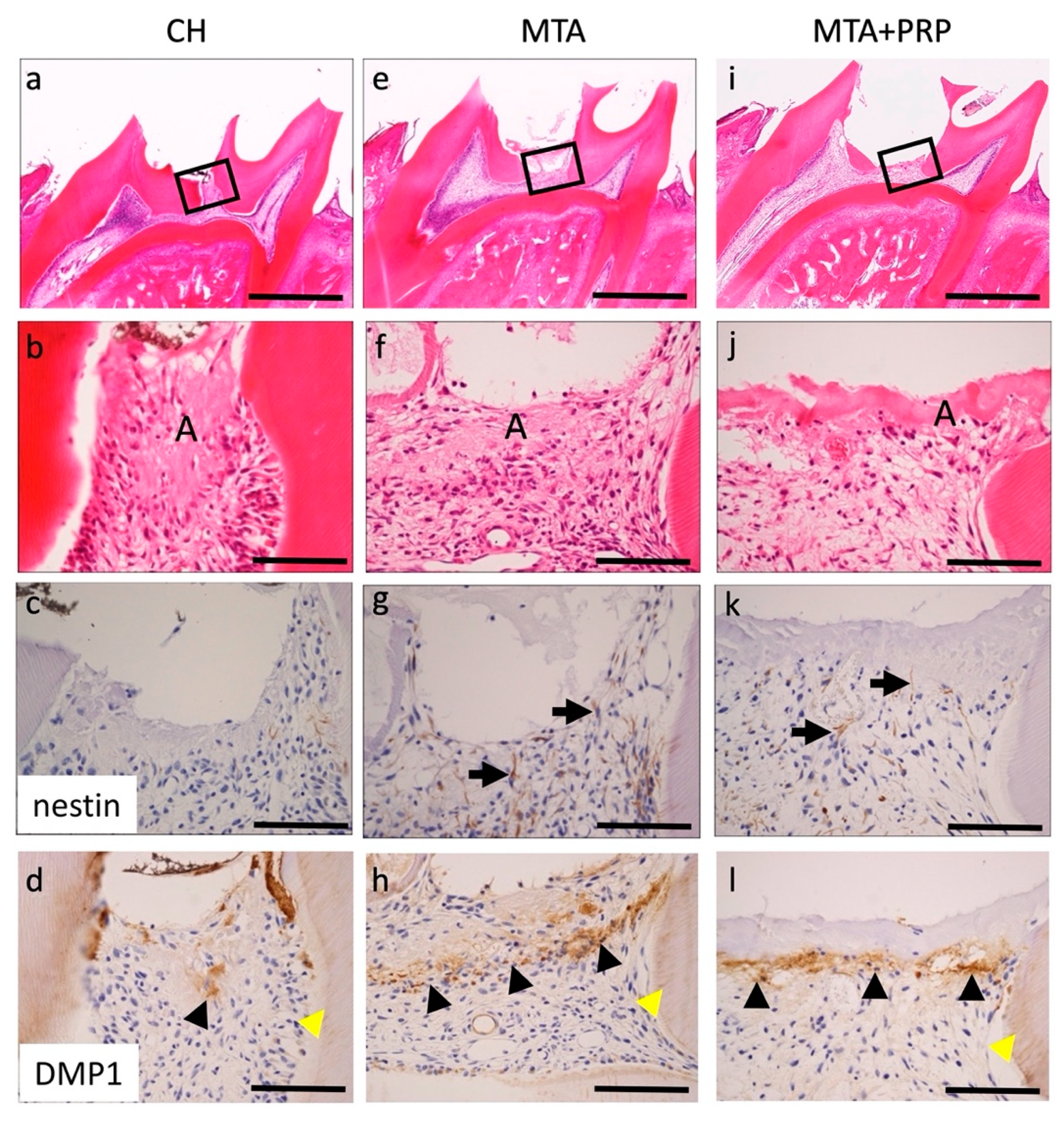
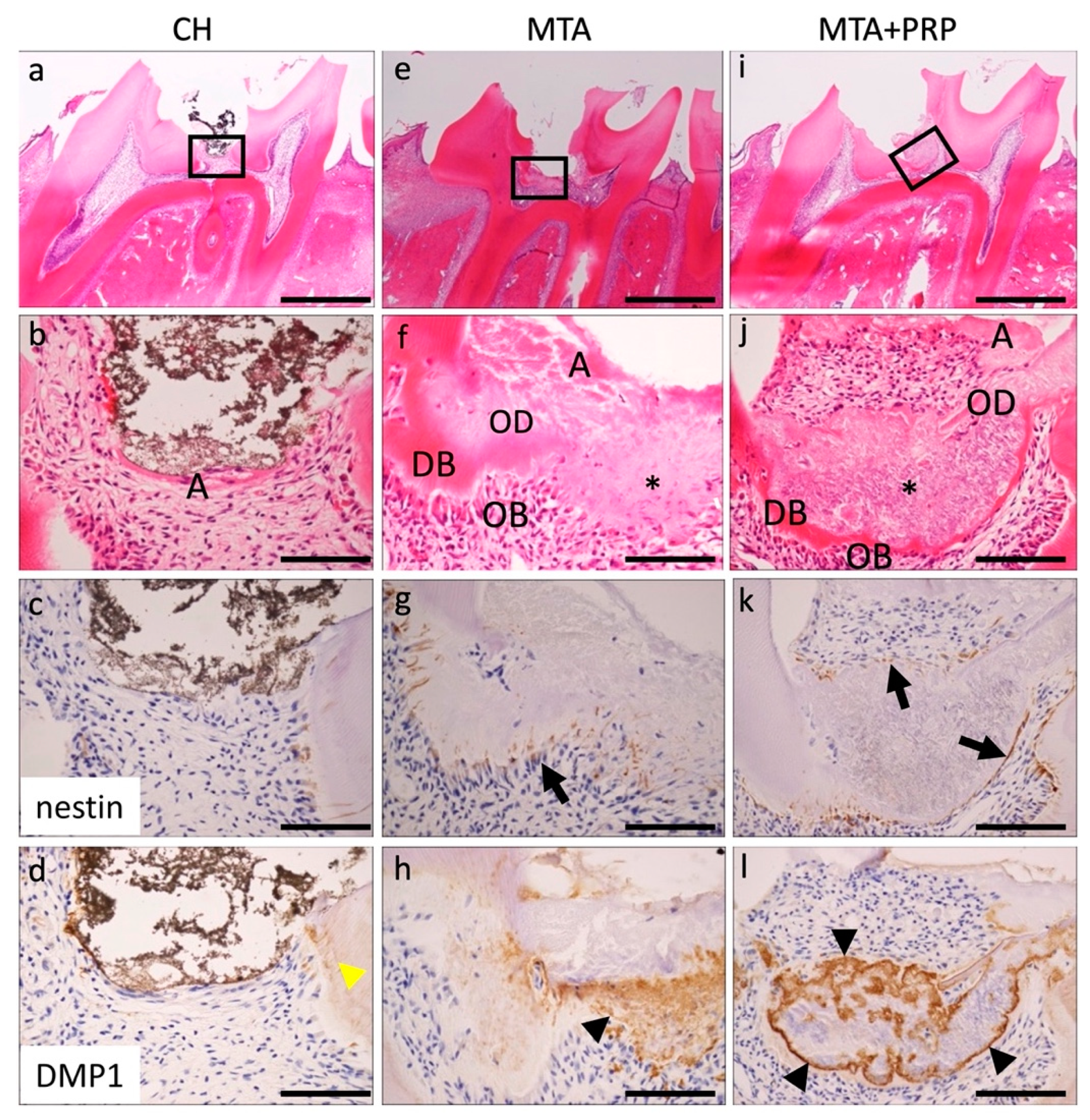
3.2. Histological and Immunohistological Findings
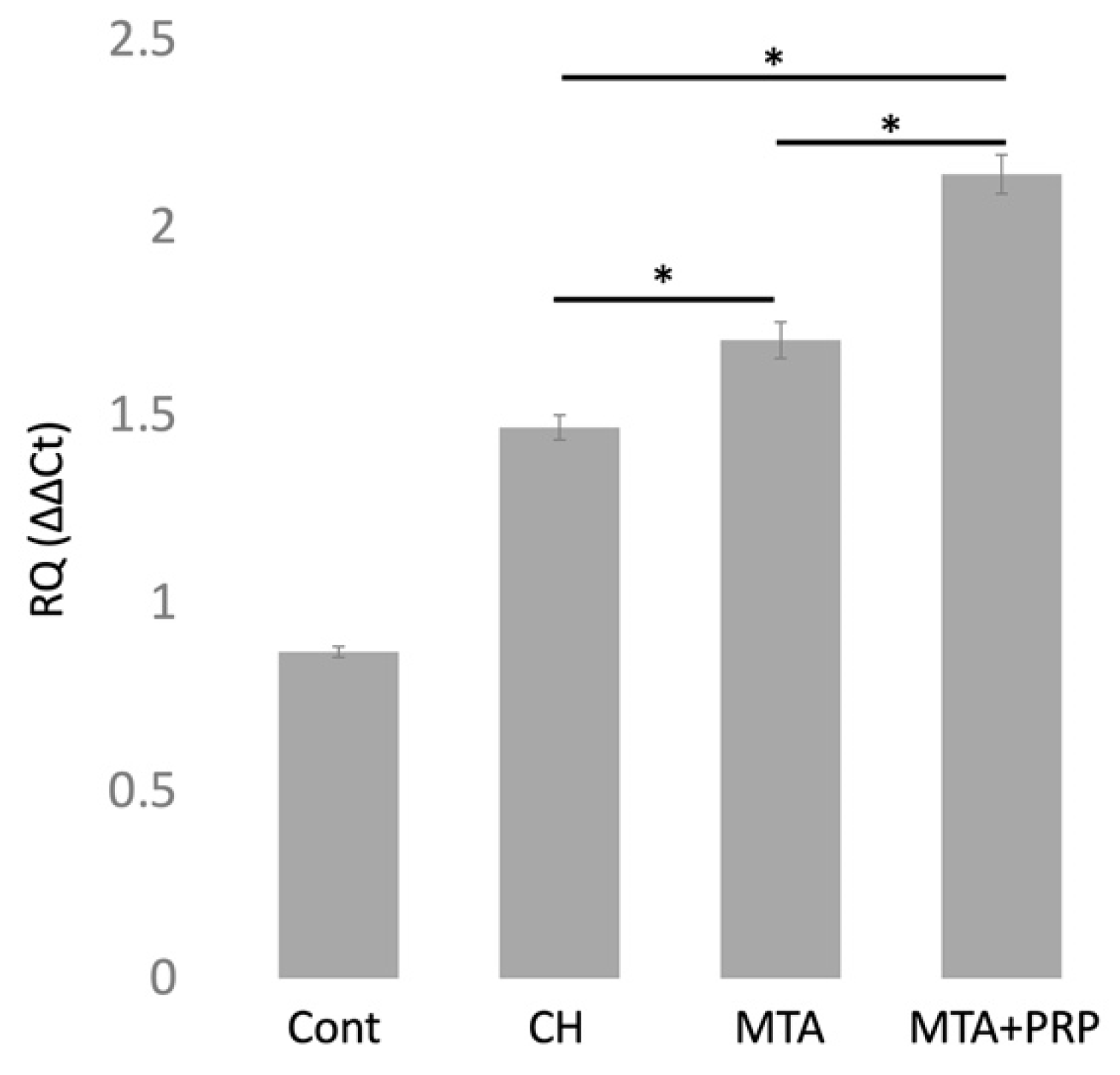
3.3. DMP1 mRNA Expression
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Schröder, U. Effects of calcium hydroxide-containing pulp-capping agents on pulp cell migration, proliferation, and differentiation. J. Dent. Res. 1985, 64, 541–548. [Google Scholar] [CrossRef] [PubMed]
- Witherspoon, D.E. Vital pulp therapy with new materials: New directions and treatment perspectives—Permanent teeth. J. Endod. 2008, 30, 220–224. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.J.; Monsef, M.; Torabinejad, M. Sealing ability of a mineral trioxide aggregate for repair of lateral root perforations. J. Endod. 1993, 19, 541–544. [Google Scholar] [CrossRef]
- Dammaschke, T.; Camp, J.H.; Bogen, G. MTA in vital pulp therapy. In Mineral Trioxide Aggregate: Properties and Clinical Applications, 1st ed.; Torabinejad, M., Ed.; Wiley Blackwell: Ames, IA, USA, 2014; pp. 77–99. [Google Scholar]
- Shabahang, S.; Witherspoon, D.E. Management of teeth with necrotic pulps and open apices. In Mineral Trioxide Aggregate: Properties and Clinical Applications, 1st ed.; Torabinejad, M., Ed.; Wiley Blackwell: Ames, IA, USA, 2014; pp. 122–139. [Google Scholar]
- Sarkar, N.K.; Caicedo, R.; Ritwik, P.; Moiseyeva, R.; Kawashima, I. Physicochemical basis of the biologic properties of mineral trioxide aggregate. J. Endod. 2005, 31, 97–100. [Google Scholar] [CrossRef] [PubMed]
- Camilleri, J.; Montesin, F.E.; Brady, K.; Sweeney, R.; Curtis, R.V.; Ford, T.R.P. The constitution of mineral trioxide aggregate. Dent. Mater. 2005, 21, 297–303. [Google Scholar] [CrossRef] [PubMed]
- Dammaschke, T.; Gerth, H.U.V.; Zuchner, H.; Schafer, E. Chemical and physical surface and bulk material characterization of white ProRoot MTA and two Portland cements. Dent. Mater. 2005, 21, 731–738. [Google Scholar] [CrossRef]
- Asgary, S.; Parirokh, M.; Eghbal, M.J.; Brink, F. Chemical differences between white and gray mineral trioxide aggregate. J. Endod. 2005, 31, 101–103. [Google Scholar] [CrossRef]
- Aguiar, M.; Arana-Chaves, V. Immunocytochemical detection of dentine matrix protein1 in experimentally induced reactionary and reparative dentine in rat incisors. Arch. Oral Biol. 2010, 55, 210–214. [Google Scholar] [CrossRef]
- D’Souza, R.N.; Cavender, A.; Sunavala, G.; Alvarez, J.; Ohshima, T.; Kulkarni, A.B.; MacDougall, M. Gene expression patterns of murine dentin matrix protein 1 (DMP1) and dentin sialophosphoprotein (DSPP) suggest distinct developmental functions in vivo. J. Bone Miner. Res. 1997, 12, 2040–2049. [Google Scholar] [CrossRef]
- Narayanan, K.; Srinivas, R.; Ramachandran, A.; Hao, J.; Quinn, B.; George, A. Differentiation of embryonic mesenchymal cells to odontoblast-like cells by overexpression of dentin matrix protein 1. Proc. Natl. Acad. Sci. USA 2001, 98, 4516–4521. [Google Scholar] [CrossRef] [Green Version]
- Narayanan, K.; Ramachandran, A.; Hao, J.; George, A. Transcriptional regulation of dentin matrix protein 1 (DMP1) by AP-1 (c-fos/c-jun) factors. Connect. Tissue Res. 2002, 43, 365–371. [Google Scholar] [CrossRef] [PubMed]
- Almushayt, A.; Narayanan, K.; Zaki, A.E.; George, A. Dentin matrix protein 1 induces cytodifferentiation of dental pulp stem cells into odontoblasts. Gene Ther. 2006, 13, 611–620. [Google Scholar] [CrossRef] [Green Version]
- Terling, C.; Rass, A.; Mitsiadis, T.A.; Fried, K.; Lendahl, U.; Wroblewski, J. Expression of the intermediate filament nestin during rodent tooth development. Int. J. Dev. Biol. 1995, 39, 947–956. [Google Scholar]
- About, I.; Laurent-Maquin, D.; Lendahl, U.; Mitsiadis, T.A. Nestin expression in embryonic and adult human teeth under normal and pathological conditions. Am. J. Pathol. 2000, 157, 287–295. [Google Scholar] [CrossRef] [Green Version]
- Yang, I.S.; Lee, D.S.; Park, J.T.; Kim, H.J.; Son, H.H.; Park, J.C. Tertiary dentin formation after direct pulp capping with odontogenic ameloblast-associated protein in rat teeth. J. Endod. 2010, 36, 1956–1962. [Google Scholar] [CrossRef]
- Kuratate, M.; Yoshiba, K.; Shigetani, Y.; Yoshiba, N.; Ohshima, H.; Okiji, T. Immunohistochemical analysis of nestin, osteopontin, and proliferating cells in the reparative process of exposed dental pulp capped with mineral trioxide aggregate. J. Endod. 2008, 34, 970–974. [Google Scholar] [CrossRef]
- Yamamura, T. Differentiation of pulpal cells and inductive influences of various matrices with reference to pulpal wound healing. J. Dent. Res. 1985, 64, 530–540. [Google Scholar] [CrossRef]
- Tziafas, D. Mechanisms controlling secondary initiation of dentinogenesis: A review. Int. Endod. J. 1994, 27, 61–74. [Google Scholar] [CrossRef]
- Goldberg, M.; Smith, A.J. Cells and extracellular matrices of dentin and pulp: A biological basis for repair and tissue engineering. Crit. Rev. Oral Biol. Med. 2004, 15, 13–27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Veis, A. The role of dental pulp—Thoughts on the session on pulp repair processes. J. Dent. Res. 1985, 64, 552–554. [Google Scholar] [CrossRef] [PubMed]
- Traub, W.; Arad, T.; Weiner, S. Origin of mineral crystal growth in collagen fibrils. Matrix 1992, 12, 251–255. [Google Scholar] [CrossRef]
- Saito, T.; Arsenault, A.L.; Yamauchi, M.; Kuboki, Y.; Crenshaw, M.A. Mineral induction by immobilized phosphoproteins. Bone 1997, 21, 305–311. [Google Scholar] [CrossRef]
- Hunter, G.K.; Hauschka, P.V.; Poole, A.R.; Rosenberg, L.C.; Goldberg, H.A. Nucleation and inhibition of hydroxyapatite formation by mineralized tissue proteins. Biochem. J. 1996, 317, 59–64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Butler, W.T.; Ritchie, H. The nature and functional significance of dentin extracellular matrix proteins. Int. J. Dev. Biol. 1995, 39, 169–179. [Google Scholar] [PubMed]
- Papagerakis, P.; Berdal, A.; Mesbah, M.; Peuchmaur, M.; Malaval, L.; Nydegger, J.; Simmer, J.; MacDougall, M. Investigation of osteocalcin, osteonectin, and dentin sialophosphoprotein in developing human teeth. Bone 2002, 30, 377–385. [Google Scholar] [CrossRef]
- He, G.; Dahl, T.; Veis, A.; George, A. Dentin matrix protein 1 initiates hydroxyapatite formation in vitro. Connect. Tissue Res. 2003, 44, 240–245. [Google Scholar] [CrossRef]
- George, A.; Sabsay, B.; Simonian, P.A.; Veis, A. Characterization of a novel dentin matrix acidic phosphoprotein. J. Biol. Chem. 1993, 268, 12624–12630. [Google Scholar] [CrossRef]
- MacDougall, M.; Gu, T.T.; Luan, X.; Simmons, D.; Chen, J. Identification of a novel isoform of mouse dentin matrix protein1: Spatial expression in mineralized tissues. J. Bone Miner. Res. 1998, 13, 422–431. [Google Scholar] [CrossRef]
- Camilleri, J.; Pitt Ford, T.R. Mineral trioxide aggregate: A review of the constituents and biological properties of the material. Int. Endod. J. 2006, 39, 747–754. [Google Scholar] [CrossRef]
- Roberts, H.W.; Toth, J.M.; Berzins, D.W.; Charlton, D.G. Mineral trioxide aggregate material use in endodontic treatment: A review of the literature. Dent. Mater. 2008, 24, 149–164. [Google Scholar] [CrossRef] [Green Version]
- Tziafas, D.; Pantelidou, O.; Alvanou, A.; Belibasakis, G.; Papadimitriou, S. The dentinogenic effect of mineral trioxide aggregate (MTA) in short-term capping experiments. Int. Endod. J. 2002, 35, 245–254. [Google Scholar] [CrossRef]
- Vanka, A.; Vishwakarma, S.K.; Bhat, M.K.; Vanka, S.; Wali, O.; Khan, A.A. Osteo/odontogenic differentiation of human mesenchymal stem cells with platelet-rich plasma and mineral trioxide aggregate. J. Contemp. Dent. Pract. 2019, 20, 1171–1178. [Google Scholar] [CrossRef] [PubMed]
- Paula, A.B.; Laranjo, M.; Marto, C.M.; Paulo, S.; Abrantes, A.M.; Fernandes, B.; Casalta-Lopes, J.; Marques-Ferreira, M.; Botelho, M.F.; Carrilho, E. Evaluation of dentinogenesis inducer biomaterials: An in vivo study. J. Appl. Oral Sci. 2019, 28, e20190023. [Google Scholar] [CrossRef] [PubMed]
- Andrei, M.; Vacaru, R.P.; Coricovac, A.; Ilinca, R.; Didilescu, A.C.; Demetrescu, I. The effect of calcium-silicate cements on reparative dentinogenesis following direct pulp capping on animal models. Molecules 2021, 26, 2725. [Google Scholar] [CrossRef] [PubMed]

| After Pulp Capping | 3 Days | 7 Days | 14 Days | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Pulp Capping Materials | CH | MTA | MTA + PRP | CH | MTA | MTA + PRP | CH | MTA | MTA + PRP |
| DB/OD | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 2 | 2 |
| nestin | 0 | 1 | 1 | 0 | 1 | 1 | 0 | 2 | 2 |
| DMP1 | 1 | 1 | 1 | 0 | 1 | 2 | 0 | 1 | 2 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yamada, M.; Nagayama, M.; Miyamoto, Y.; Kawano, S.; Takitani, Y.; Tanaka, M.; Ehara, M.; Nakao, J.; Ochiai, T.; Shibukawa, Y.; et al. Mineral Trioxide Aggregate (MTA) Upregulates the Expression of DMP1 in Direct Pulp Capping in the Rat Molar. Materials 2021, 14, 4640. https://doi.org/10.3390/ma14164640
Yamada M, Nagayama M, Miyamoto Y, Kawano S, Takitani Y, Tanaka M, Ehara M, Nakao J, Ochiai T, Shibukawa Y, et al. Mineral Trioxide Aggregate (MTA) Upregulates the Expression of DMP1 in Direct Pulp Capping in the Rat Molar. Materials. 2021; 14(16):4640. https://doi.org/10.3390/ma14164640
Chicago/Turabian StyleYamada, Maiko, Motohiko Nagayama, Yuka Miyamoto, Satoshi Kawano, Yoshiaki Takitani, Masashi Tanaka, Michiko Ehara, Juna Nakao, Takanaga Ochiai, Yoshihiro Shibukawa, and et al. 2021. "Mineral Trioxide Aggregate (MTA) Upregulates the Expression of DMP1 in Direct Pulp Capping in the Rat Molar" Materials 14, no. 16: 4640. https://doi.org/10.3390/ma14164640
APA StyleYamada, M., Nagayama, M., Miyamoto, Y., Kawano, S., Takitani, Y., Tanaka, M., Ehara, M., Nakao, J., Ochiai, T., Shibukawa, Y., & Yoshida, T. (2021). Mineral Trioxide Aggregate (MTA) Upregulates the Expression of DMP1 in Direct Pulp Capping in the Rat Molar. Materials, 14(16), 4640. https://doi.org/10.3390/ma14164640





