One-Abutment One-Time Effect on Peri-Implant Marginal Bone: A Prospective, Controlled, Randomized, Double-Blind Study
Abstract
:1. Introduction
2. Materials and Methods
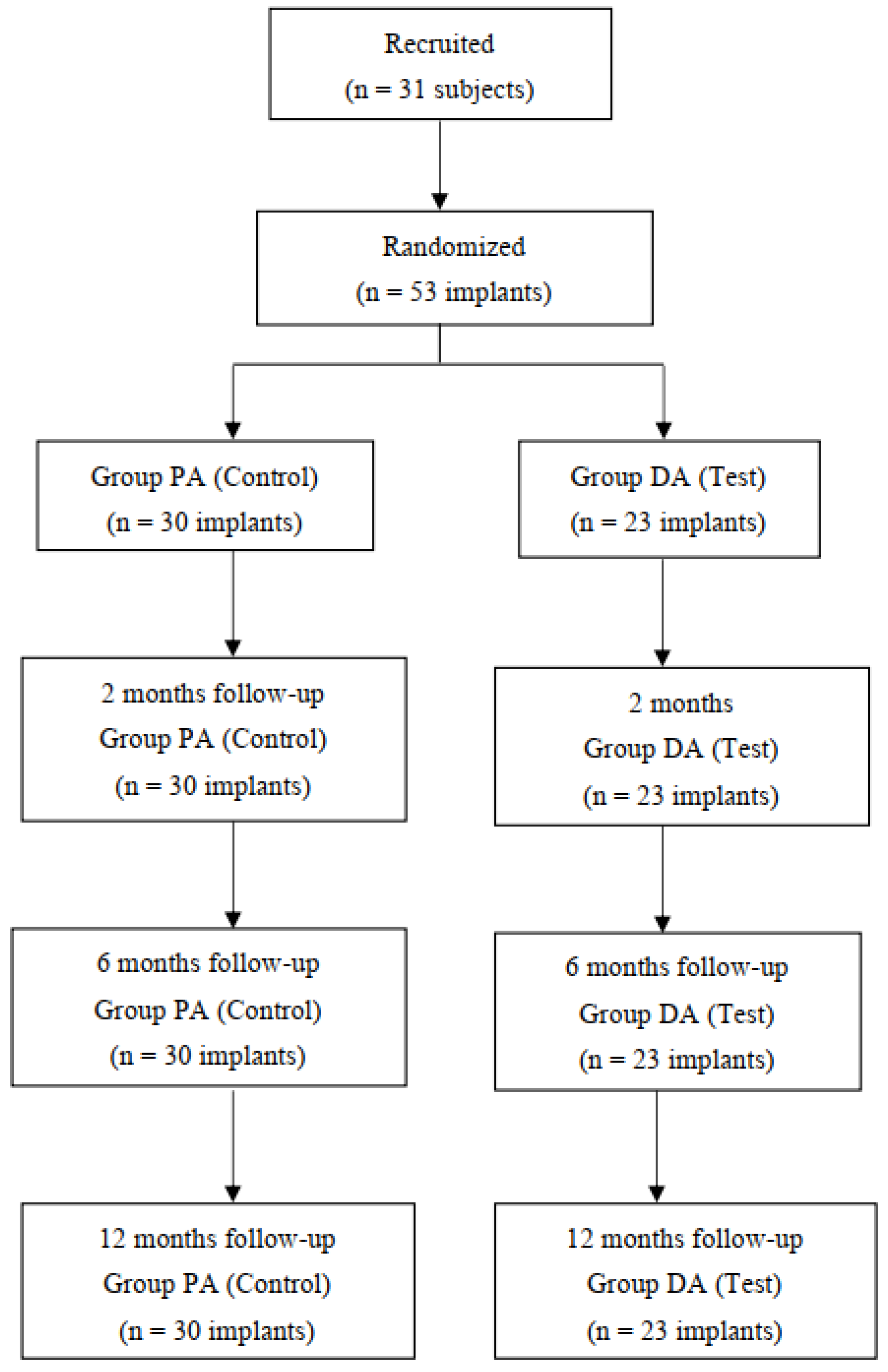
2.1. Study Design
2.2. Study Population
- Minimum of 18 years old;
- At least one adjacent missing tooth in the posterior maxilla or mandible (World Dental Federation positions 4–7) with no free-end unitary implant situation being allowed.
- Patients willing an implant-supported rehabilitation and compromised to attend the follow-up visits.
- Healing post-extraction period of more than 4 months.
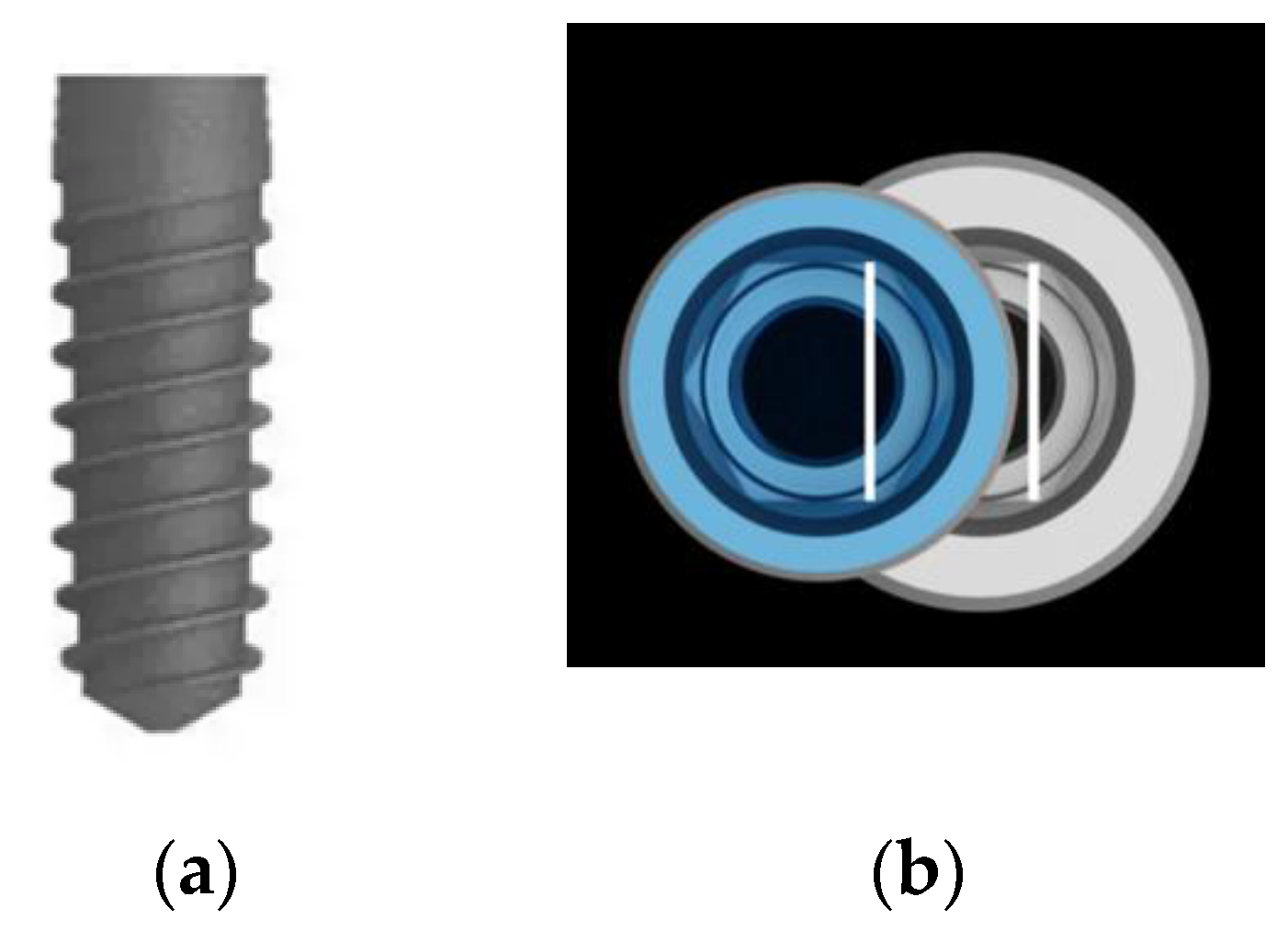
- Healed osseous architecture sufficient to receive a VEGA implant® (Klockner Implant System, SOADCO, S.L., Escaldes-Engordany, Andorra) with a diameter and lenght at least of 4 mm and 8 mm, respectively, allowing the existence of a minimum of 1.5 mm bone tissue width surrounding the implant.
- Natural teeth or fixed prosthesis as opposing dentition.
- No signs of periodontal disease: absence of suppuration, plaque index and bleeding less than 15% according to Mombelli’s criteria.
- Any illness afecting the immunitary system and/or bone metabolism.
- History of administration of bisphosphonates.
- Alterations in coagulation.
- History of radiotherapy of the head or neck.
- Uncontrolled systemic disorders.
- Alcohol and drug abuse.
- HIV+.
- Severe bruxists or with signs of temporomandibular joint (TMJ) pathology or muscle pain.
- Smokers of more than 10 cigarettes per day.
- Factors that, in the investigator’s opinion, complicate the patient’s participation in the study or in data analysis.
- Any local pathology that represents a contraindication for the treatment with dental implants.
- Nonhealed alveolar bone.
- Locations submitted to bone regeneration less than 6 months ago
- Bone defect around the contour of the implant requiring regeneration–bone augmentation representing 25% or more of the implant surface in fenestration type defects at the time of implant placement.
- Inadequate oral hygiene
- Active, recurrent or unresolved infections in the area adjacent to the implant installation
- Lack of primary stability of the implant.
- Inadequate implant position that compromises prosthetic requirements for the study.
- Need for additional regenerative techniques.
2.3. Sample Size
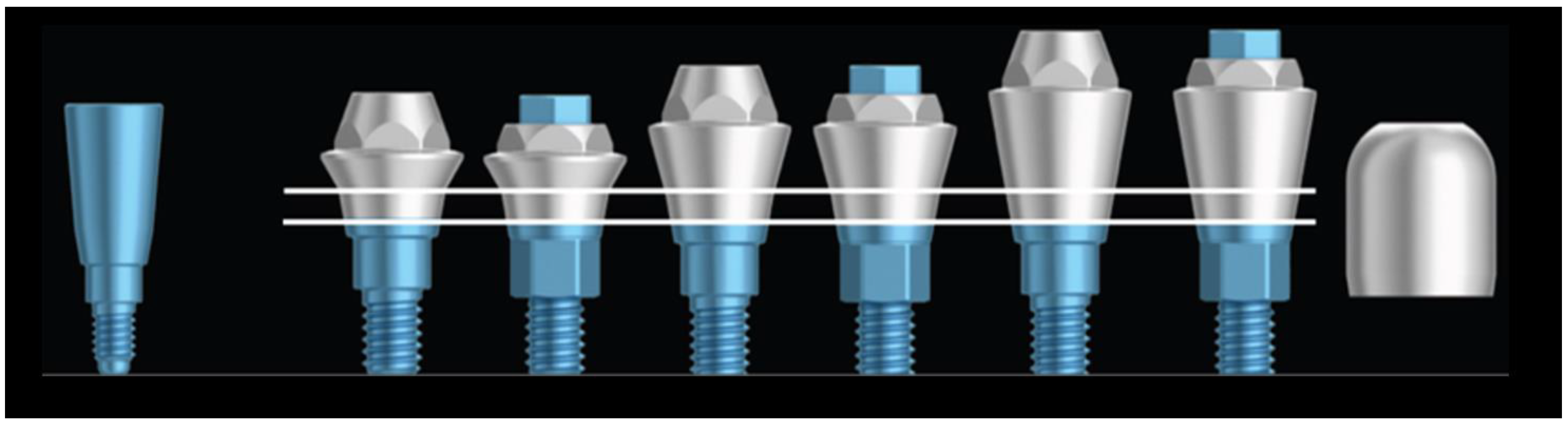
2.4. Implants and Abutments
2.5. Surgical Procedure and Randomization
2.6. Prosthetic Procedures
2.7. Clinical Examinations
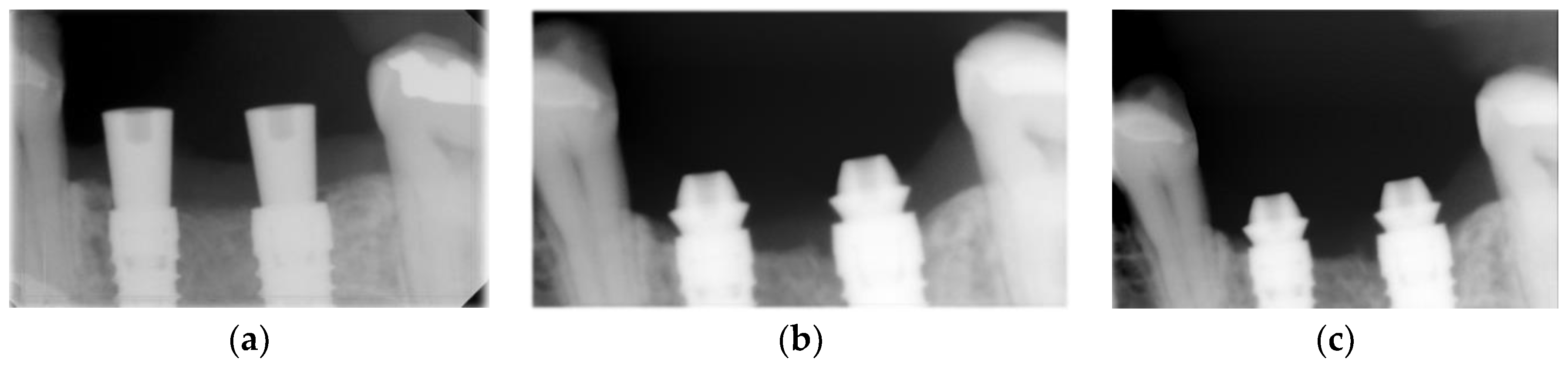
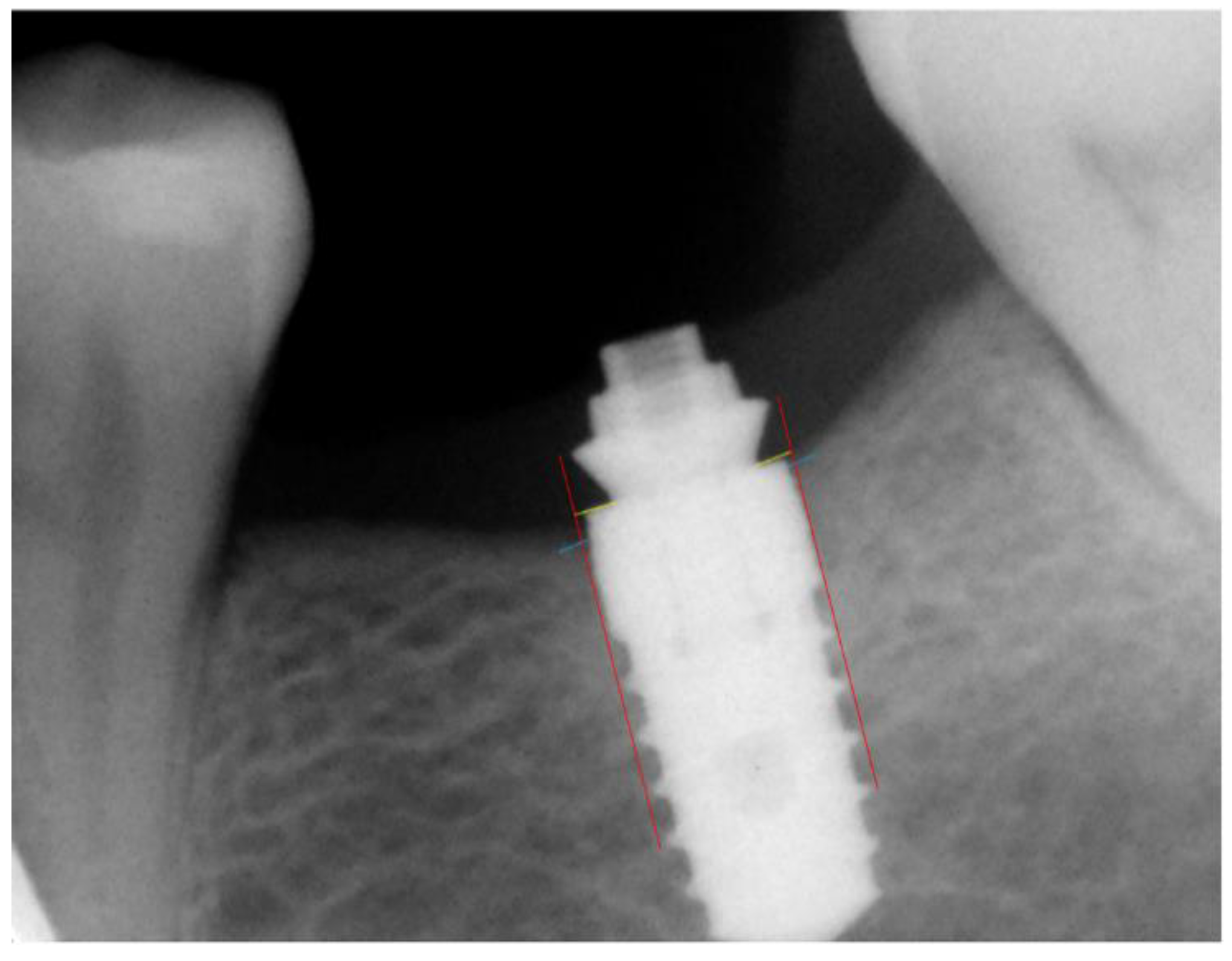
2.8. Radiographic Assessment
2.9. Statistical Analysis
3. Results
3.1. General Information
3.2. Analysis of Resonance Frequency Values in Both Groups
3.3. Changes in the Clinical Outcome Measurements
3.3.1. Modified Plaque Index
3.3.2. Modified Sulcus Bleeding Index
3.3.3. Probing Depth
3.4. Total Bone Loss over Time
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ISQ | implant stability quotient |
| DA | definitive abutment |
| PA | provisional abutment |
| MBL | marginal bone loss |
| PS | platform switching |
| FDI | world dental federation |
| TMJ | temporomandibular joint |
| JPEG | joint photographic experts group |
| DIB | distance between the implant platform and the first visible bone contact |
| ICC | intraclass correlation coefficient |
| TOST | two one-sided tests |
| mPLI | modified plaque index |
References
- Javed, F.; Ahmed, H.B.; Crespi, R.; Romanos, G.E. Role of primary stability for successful osseointegration of dental implants: Factors of influence and evaluation. Interv. Med. Appl. Sci. 2013, 5, 162–167. [Google Scholar] [CrossRef]
- Albrektsson, T.; Brånemark, P.-I.; Hansson, H.-A.; Lindström, J. Osseointegrated titanium implants:Requirements for ensuring a long-lasting, direct bone-to-implant anchorage in man. Acta Orthop. Scand. 1981, 52, 155–170. [Google Scholar] [CrossRef] [Green Version]
- Huang, H.; Wu, G.; Hunziker, E. The clinical significance of implant stability quotient (ISQ) measurements: A literature review. J. Oral Biol. Craniofacial Res. 2020, 10, 629–638. [Google Scholar] [CrossRef]
- Jivraj, S.; Chee, W. Treatment planning of implants in the aesthetic zone. Br. Dent. J. 2006, 201, 77–89. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kois, J.C. Predictable single-tooth peri-implant esthetics: Five diagnostic keys. Compend. Contin. Educ. Dent. 2004, 25, 895. [Google Scholar] [PubMed]
- Alsabeeha, N.H.; Atieh, M.A. Hydroxyapatite-coated oral implants: A systematic review and meta-analysis. Int. J. Oral Maxillofac. Implants 2012, 27, 1123–1130. [Google Scholar]
- Osman, R.B.; Swain, M.V.; Atieh, M.A.; Duncan, W. Ceramic implants (Y-TZP): Are they a viable alternative to titanium implants for the support of overdentures? A randomized clinical trial. Clin. Oral Implants Res. 2014, 25, 1366–1377. [Google Scholar] [CrossRef] [PubMed]
- Philipp, A.; Duncan, W.; Roos, M.; Hämmerle, C.H.; Attin, T.; Schmidlin, P.R. Comparison of SLA® or SLActive® implants placed in the maxillary sinus with or without synthetic bone graft materials—An animal study in sheep. Clin. Oral Implants Res. 2013, 25, 1142–1148. [Google Scholar] [CrossRef] [PubMed]
- Campbell, D.I.; Duncan, W.J. The effect of a keratin hydrogel coating on osseointegration: An histological comparison of coated and non-coated dental titanium implants in an ovine model. J. Maxillofac. Oral Surg. 2013, 13, 159–164. [Google Scholar] [CrossRef] [Green Version]
- Duncan, W.J.; Lee, M.H.; Bae, T.S.; Lee, S.J.; Gay, J.; Loch, C. Anodisation increases integration of unloaded titanium implants in sheep mandible. BioMed Res. Int. 2015, 2015, 857969. [Google Scholar] [CrossRef]
- Sharma, A.; McQuillan, A.J.; Sharma, L.A.; Waddell, J.; Shibata, Y.; Duncan, W. Spark anodization of titanium-zirconium alloy: Surface characterization and bioactivity assessment. J. Mater. Sci. Mater. Med. 2015, 26, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Alsabeeha, N.; Atieh, M.; Payne, A.G. Loading protocols for mandibular implant overdentures: A systematic review with meta-analysis. Clin. Implants Dent. Relat. Res. 2009, 12, e28–e38. [Google Scholar] [CrossRef]
- Atieh, M.A.; Alsabeeha, N.H.M.; Duncan, W.J.; de Silva, R.K.; Cullinan, M.P.; Schwass, D.; Payne, A.G.T. Immediate single implant restorations in mandibular molar extraction sockets: A controlled clinical trial. Clin. Oral Implants Res. 2012, 24, 484–496. [Google Scholar] [CrossRef]
- Atieh, M.A.; Atieh, A.H.; Payne, A.G.; Duncan, W.J. Immediate loading with single implant crowns: A systematic review and meta-analysis. Int. J. Prosthodont. 2009, 22, 378–387. [Google Scholar]
- Atieh, M.A.; Payne, A.G.; Duncan, W.J.; de Silva, R.K.; Cullinan, M.P. Immediate placement or immediate restoration/ loading of single implants for molar tooth replacement: A systematic review and meta-analysis. Int. J. Oral Maxillofac. Implants 2010, 25, 401–415. [Google Scholar]
- Atieh, M.A.; Ibrahim, H.M.; Atieh, A.H. Platform switching for marginal bone preservation around dental implants: A systematic review and meta-analysis. J. Periodontol. 2010, 81, 1350–1366. [Google Scholar] [CrossRef] [PubMed]
- Bateli, M.; Att, W.; Strub, J.R. Implant neck configurations for preservation of marginal bone level: A systematic review. Int. J. Oral Maxillofac. Implants 2011, 26, 290. [Google Scholar]
- Schwarz, F.; Hegewald, A.; Becker, J. Impact of implant abutment connection and positioning of the machined collar/microgap on crestal bone level changes: A systematic review. Clin. Oral Implants Res. 2014, 25, 417–425. [Google Scholar] [CrossRef] [PubMed]
- Alfonsi, F.; Borgia, V.; Barbato, L.; Tonelli, P.; Giammarinaro, E.; Marconcini, S.; Romeggio, S.; Barone, A. The clinical effects of insertion torque for implants placed in healed ridges: A two-year randomized controlled clinical trial. J. Oral Sci. Rehabil. 2016, 2, 62–73. [Google Scholar]
- Maeda, Y.; Miura, J.; Taki, I.; Sogo, M. Biomechanical analysis on platform switching: Is there any biomechanical rationale? Clin. Oral Implants Res. 2007, 18, 581–584. [Google Scholar] [CrossRef] [PubMed]
- Lazzara, R.J.; Porter, S.S. Platform switching: A new concept in implant dentistry for controlling post restorative crestal bone levels. Int. J. Periodontics Restor. Dent. 2006, 26, 9–17. [Google Scholar]
- Vigolo, P.; Givani, A. Platform-switched restorations on wide-diameter implants: A 5-year clinical prospective study. Int. J. Oral Maxillofac. Implants 2009, 24, 103–109. [Google Scholar]
- Canullo, L.; Goglia, G.; Iurlaro, G.; Iannello, G. Short-term bone level observations associated with platform switching in immediately placed and restored single maxillary implants: A preliminary report. Int. J. Prosthodont. 2009, 22, 277–282. [Google Scholar]
- Rocha, S.; Wagner, W.; Wiltfang, J.; Nicolau, P.; Moergel, M.; Messias, A.; Behrens, E.; Guerra, F. Effect of platform switching on crestal bone levels around implants in the posterior mandible: 3 years results from a multicentre randomized clinical trial. J. Clin. Periodontol. 2016, 43, 374–382. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, F.; Alcoforado, G.; Nelson, K.; Schaer, A.; Taylor, T.; Beuer, F.; Strietzel, F.P. Impact of implant-abutment connection, positioning of the machined collar/microgap, and platform switching on crestal bone level changes. Camlog Foundation Consensus Report. Clin. Oral Implants Res. 2014, 25, 1301–1303. [Google Scholar] [CrossRef] [PubMed]
- Becker, K.; Mihatovic, I.; Golubovic, V.; Schwarz, F. Impact of abutment material and dis-/re-connection on soft and hard tissue changes at implants with platform-switching. J. Clin. Periodontol. 2012, 39, 774–780. [Google Scholar] [CrossRef]
- Göthberg, C.; André, U.; Gröndahl, K.; Thomsen, P.; Slotte, C. Bone response and soft tissue changes around implants with/without abutments supporting fixed partial dentures: Results from a 3-year, prospective, randomized, controlled study. Clin. Implants Dent. Relat. Res. 2015, 18, 309–322. [Google Scholar] [CrossRef] [PubMed]
- Galindo-Moreno, P.; León-Cano, A.; Monje, A.; Ortega-Oller, I.; O’Valle, F.; Catena, A. Abutment height influences the effect of platform switching on peri-implant marginal bone loss. Clin. Oral Implants Res. 2015, 27, 167–173. [Google Scholar] [CrossRef] [PubMed]
- Puisys, A.; Linkevicius, T. The influence of mucosal tissue thickening on crestal bone stability around bone-level implants. A prospective controlled clinical trial. Clin. Oral Implants Res. 2015, 26, 123–129. [Google Scholar] [CrossRef]
- Schwarz, F.; Mihatovic, I.; Ferrari, D.; Wieland, M.; Becker, J. Influence of frequent clinical probing during the healing phase on healthy peri-implant soft tissue formed at different titanium implant surfaces: A histomorphometrical study in dogs. J. Clin. Periodontol. 2010, 37, 551–562. [Google Scholar] [CrossRef]
- Canullo, L.; Bignozzi, I.; Cocchetto, R.; Cristalli, M.P.; Iannello, G. Immediate positioning of a definitive abutment versus repeated abutment replacements in post-extractive implants: 3-year follow-up of a randomised multicentre clinical trial. Eur. J. Oral Implants 2010, 3, 285–296. [Google Scholar]
- Iglhaut, G.; Golubovic, V.; Becker, K.; Schliephake, H.; Mihatovic, I. The impact of dis-/reconnection of laser microgrooved and machined implant abutments on soft- and hard-tissue healing. Clin. Oral Implants Res. 2012, 24, 391–397. [Google Scholar] [CrossRef]
- Rodriguez, X.; Vela, X.; Segalà, M.; Tarnow, D.P.; Calvo-Guirado, J.L.; Méndez, V. The effect of abutment dis/reconnections on peri-implant bone resorption: A radiologic study of platform-switched and non-platform-switched implants placed in animals. Clin. Oral Implants Res. 2011, 24, 305–311. [Google Scholar] [CrossRef]
- Abrahamsson, I.; Berglundh, T.; Lindhe, J. The mucosal barrier following abutment dis/reconnection. An experimental study in dogs. J. Clin. Periodontol. 1997, 24, 568–572. [Google Scholar] [CrossRef]
- Alves, C.C.; Munoz, F.; Cantalapiedra, A.G.; Ramos, I.; Neves, M.; Blanco, J. Marginal bone and soft tissue behavior following platform switching abutment connection/disconnection- a dog model study. Clin. Oral Implants Res. 2014, 26, 983–991. [Google Scholar] [CrossRef] [Green Version]
- Degidi, M.; Nardi, D.; Daprile, G.; Piattelli, A. Nonremoval of immediate abutments in cases involving subcrestally placed postextractive tapered single implants: A randomized controlled clinical study. Clin. Implants Dent. Relat. Res. 2013, 16, 794–805. [Google Scholar] [CrossRef] [PubMed]
- Grandi, T.; Guazzi, P.; Samarani, R.; Maghaireh, H.; Grandi, G. One abutment-one time versus a provisional abutment in immediately loaded post-extractive single implants: A 1-year follow-up of a multicentre randomised controlled trial. Eur. J. Oral Implants 2014, 7, 141–149. [Google Scholar]
- Degidi, M.; Nardi, D.; Piattelli, A. One abutment at one time: Non-removal of an immediate abutment and its effect on bone healing around subcrestal tapered implants. Clin. Oral Implants Res. 2011, 22, 1303–1307. [Google Scholar] [CrossRef] [PubMed]
- Grandi, T.; Guazzi, P.; Samarani, R.; Garuti, G. Immediate positioning of definitive abutments versus repeated abutment replacements in immediately loaded implants: Effects on bone healing at the 1-year follow-up of a multicentre randomised controlled trial. Eur. J. Oral Implants 2012, 5, 9–16. [Google Scholar]
- Lakens, D. Equivalence tests: A practical primer for t-tests, correlations, and meta-analyses. Soc. Psychol. Personal. Sci. 2017, 8, 355–362. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Romero-Ruiz, M.M.; Gil-Mur, F.J.; Ríos-Santos, J.V.; Lázaro-Calvo, P.; Ríos-Carrasco, B.; Herrero-Climent, M. Influence of a novel surface of bioactive implants on osseointegration: A comparative and histomorfometric correlation and implant stability study in minipigs. Int. J. Mol. Sci. 2019, 20, 2307. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nedir, R.; Bischof, M.; Szmukler-Moncler, S.; Bernard, J.-P.; Samson, J. Predicting osseointegration by means of implant primary stability. A resonance-frequency analysis study with delayed and immediately loaded ITI SLA implants. Clin. Oral Implants Res. 2004, 15, 520–528. [Google Scholar] [CrossRef] [PubMed]
- Sennerby, L.; Meredith, N. Resonance frequency analysis: Measuring implant stability and osseointegration. Compend. Contin. Educ. Dent. 1998, 19, 493–498. [Google Scholar] [PubMed]
- Mombelli, A.; van Oosten, M.A.C.; Schürch, E., Jr.; Lang, N.P. The microbiota associated with successful or failing osseointegrated titanium implants. Oral Microbiol. Immunol. 1987, 2, 145–151. [Google Scholar] [CrossRef] [PubMed]
- Messias, A.; Tondela, J.P.; Rocha, S.; Reis, R.; Nicolau, P.; Guerra, F. Acrylic Customized X-Ray Positioning Stent for Prospective Bone Level Analysis in Long-Term Clinical Implant Studies. Open J. Radiol. 2013, 03, 136–142. [Google Scholar] [CrossRef] [Green Version]
- Koutouzis, T.; Koutouzis, G.; Gadella, H.; Neiva, R. The effect of healing abutment reconnection and disconnection on soft and hard peri-implant tissues: A short-term randomized controlled clinical trial. Int. J. Oral Maxillofac. Implants 2013, 28, 807–814. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Esposito, M.; Bressan, E.; Grusovin, M.G.; D’Avenia, F.; Neumann, K.; Sbricoli, L.; Luongo, G. Do repeated changes of abut-ments have any influence on the stability of peri-implant tissues? One-year post-loading results from a multicentre ran-domised controlled trial. Eur. J. Oral Implantol. 2017, 10, 57–72. [Google Scholar] [PubMed]
- Praça, L.D.F.G.; Teixeira, R.C.; Rego, R. Influence of abutment disconnection on peri-implant marginal bone loss: A randomized clinical trial. Clin. Oral Implants Res. 2020, 31, 341–351. [Google Scholar] [CrossRef]
- Molina, A.; Sanz-Sánchez, I.; Martín, C.; Blanco, J.; Sanz, M. The effect of one-time abutment placement on interproximal bone levels and peri-implant soft tissues: A prospective randomized clinical trial. Clin. Oral Implants Res. 2016, 28, 443–452. [Google Scholar] [CrossRef]
- Luongo, G.; Bressan, E.; Grusovin, M.G.; D’Avenia, F.; Neumann, K.; Sbricoli, L.; Esposito, M. Do repeated changes of abutments have any influence on the stability of peri-implant tissues? Four-month post-loading preliminary results from a multicentre randomised controlled trial. Eur. J. Oral Implants 2015, 8, 129–140. [Google Scholar]
- Romanos, G.E.; Aydin, E.; Gaertner, K.; Nentwig, G.-H. Long-term results after subcrestal or crestal placement of delayed loaded implants. Clin. Implants Dent. Relat. Res. 2013, 17, 133–141. [Google Scholar] [CrossRef]
- De Siqueira, R.A.C.; Junior, R.S.G.; dos Santos, P.G.F.; Sartori, I.A.D.M.; Wang, H.-L.; Fontão, F.N.G.K. Effect of different implant placement depths on crestal bone levels and soft tissue behavior: A 5-year randomized clinical trial. Clin. Oral Implants Res. 2019, 31, 282–293. [Google Scholar] [CrossRef]
- Albrektsson, T.; Chrcanovic, B.; Östman, P.-O.; Sennerby, L. Initial and long-term crestal bone responses to modern dental implants. Periodontol. 2000 2016, 73, 41–50. [Google Scholar] [CrossRef] [PubMed]
- Astrand, P.; Engquist, B.; Dahlgren, S.; Grondahl, K.; Engquist, E.; Feldmann, H. Astra Tech and Branemark system implants: A 5-year prospective study of marginal bone reactions. Clin. Oral Implants Res. 2004, 15, 413–420. [Google Scholar] [CrossRef] [PubMed]
- Berglundh, T.; Abrahamsson, I.; Lindhe, J. Bone reactions to longstanding functional load at implants: An experimental study in dogs. J. Clin. Periodontol. 2005, 32, 925–932. [Google Scholar] [CrossRef]
- Bressan, E.; Grusovin, M.G.; D’Avenia, F.; Neumann, K.; Sbricoli, L.; Luongo, G.; Esposito, M. The influence of repeated abutment changes on peri-implant tissue stability: 3-year post-loading results from a multicentre randomised controlled trial. Eur. J. Oral Implants 2017, 10, 373–390. [Google Scholar]
- Misawa, M.; Lindhe, J.; Araújo, M.G. The alveolar process following single-tooth extraction: A study of maxillary incisor and premolar sites in man. Clin. Oral Implants Res. 2015, 27, 884–889. [Google Scholar] [CrossRef]
- Sanz, M.; Cecchinato, D.; Ferrús, J.; Pjetursson, E.B.; Lang, N.P.; Lindhe, J. A prospective, randomized-controlled clinical trial to evaluate bone preservation using implants with different geometry placed into extraction sockets in the maxilla. Clin. Oral Implants Res. 2009, 21, 13–21. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.T.; Buser, D. Esthetic outcomes following immediate and early implant placement in the anterior maxilla—A systematic review. Int. J. Oral Maxillofac. Implants 2014, 29, 186–215. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferrus, J.; Cecchinato, D.; Pjetursson, E.B.; Lang, N.P.; Sanz, M.; Lindhe, J. Factors influencing ridge alterations following immediate implant placement into extraction sockets. Clin. Oral Implants Res. 2009, 21, 22–29. [Google Scholar] [CrossRef] [PubMed]
- Donati, M.; la Scala, V.; Billi, M.; di Dino, B.; Torrisi, P.; Berglundh, T. Immediate functional loading of implants in single tooth replacement: A prospective clinical multicenter study. Clin. Oral Implants Res. 2008, 19, 740–748. [Google Scholar] [CrossRef]
- Esposito, M.; Grusovin, M.G.; Maghaireh, H.; Worthington, H.V. Interventions for replacing missing teeth: Different times for loading dental implants. Cochrane Database Syst. Rev. 2013, 2013, CD003878. [Google Scholar] [CrossRef] [Green Version]
- Nicolau, P.; Korostoff, J.; Ganeles, J.; Jackowski, J.; Krafft, T.; Neves, M.; Divi, J.; Rasse, M.; Guerra, F.; Fischer, K. Immediate and early loading of chemically modified implants in posterior jaws: 3-year results from a prospective randomized multicenter study. Clin. Implants Dent. Relat. Res. 2011, 15, 600–612. [Google Scholar] [CrossRef]
- Linkevicius, T.; Vindasiute, E.; Puisys, A.; Peciuliene, V. The influence of margin location on the amount of undetected cement excess after delivery of cement-retained implant restorations. Clin. Oral Implants Res. 2011, 22, 1379–1384. [Google Scholar] [CrossRef] [PubMed]
- Linkevicius, T.; Puisys, A.; Vindasiute, E.; Linkeviciene, L.; Apse, P. Does residual cement around implant-supported restorations cause peri-implant disease? A retrospective case analysis. Clin. Oral Implants Res. 2012, 24, 1179–1184. [Google Scholar] [CrossRef] [PubMed]
- Souza, A.B.; Alshihri, A.; Kämmerer, P.W.; Araújo, M.G.; Gallucci, G.O. Histological and micro-CT analysis of peri-implant soft and hard tissue healing on implants with different healing abutments configurations. Clin. Oral Implants Res. 2018, 29, 1007–1015. [Google Scholar] [CrossRef] [PubMed]
- Piñeyro, A.; Tucker, L.M. One abutment-one time: The negative effect of uncontrolled abutment margin depths and excess cement—A case report. Compend. Contin. Educ. Dent. 2013, 34, 24564754. [Google Scholar]
- Wadhwani, C.; Piñeyro, A.; Hess, T.; Zhang, H.; Chung, K.-H. Effect of implant abutment modification on the extrusion of excess cement at the crown-abutment margin for cement-retained implant restorations. Int. J. Oral Maxillofac. Implants 2011, 26, 22167429. [Google Scholar]
- Canullo, L.; Cocchetto, R.; Marinotti, F.; Penarrocha-Oltra, D.; Diago, M.P.; Loi, I. Clinical evaluation of an improved cementation technique for implant-supported restorations: A randomized controlled trial. Clin. Oral Implants Res. 2016, 27, 1492–1499. [Google Scholar] [CrossRef]
- Bidra, A.S.; Kejriwal, S.; Bhuse, K. Should healing abutments and cover screws for dental implants be reused? A systematic review. J. Prosthodont. 2019, 29, 42–48. [Google Scholar] [CrossRef]
- Barreiros, P.; Braga, J.; Faria-Almeida, R.; Coelho, C.; Teughels, W.; Souza, J.C.M. Remnant oral biofilm and microorganisms after autoclaving sterilization of retrieved healing abutments. J. Periodontal Res. 2021, 56, 415–422. [Google Scholar] [CrossRef] [PubMed]
- Tallarico, M.; Caneva, M.; Meloni, S.M.; Xhanari, E.; Covani, U.; Canullo, L. Definitive abutments placed at implant insertion and never removed: Is it an effective approach? A systematic review and meta-analysis of randomized controlled trials. J. Oral Maxillofac. Surg. 2018, 76, 316–324. [Google Scholar] [CrossRef] [PubMed]
- Atieh, M.A.; Tawse-Smith, A.; Alsabeeha, N.H.M.; Ma, S.; Duncan, W.J. The one abutment-one time protocol: A systematic review and meta-analysis. J. Periodontol. 2017, 88, 1173–1185. [Google Scholar] [CrossRef]
- Perrotti, V.; Zhang, D.; Liang, A.; Wang, J.; Quaranta, A. The effect of one-abutment at one-time on marginal bone loss around implants placed in healed bone. Implants Dent. 2019, 28, 603–612. [Google Scholar] [CrossRef]
- Wang, Q.-Q.; Dai, R.; Cao, C.Y.; Fang, H.; Han, M.; Li, Q.-L. One-time versus repeated abutment connection for platform-switched implant: A systematic review and meta-analysis. PLoS ONE 2017, 12, e0186385. [Google Scholar] [CrossRef] [Green Version]
- Koutouzis, T.; Gholami, F.; Reynolds, J.; Lundgren, T.; Kotsakis, G. Abutment disconnection/reconnection affects peri-implant marginal bone levels: A meta-analysis. Int. J. Oral Maxillofac. Implants 2017, 32, 575–581. [Google Scholar] [CrossRef] [Green Version]
- Santos, J.S.; Santos, T.D.S.; Filho, P.R.S.M.; von Krockow, N.; Weigl, P.; Pablo, H. One abutment at one time concept for platform-switched morse implants: Systematic review and meta-analysis. Braz. Dent. J. 2018, 29, 7–13. [Google Scholar] [CrossRef] [Green Version]
- Albrektsson, T.; Canullo, L.; Cochran, D.; de Bruyn, H. “Peri-implantitis”: A complication of a foreign body or a man-made “disease”. Facts and fiction. Clin. Implants Dent. Relat. Res. 2016, 18, 840–849. [Google Scholar] [CrossRef]
- Canullo, L.; Tallarico, M.; Gracis, S.; Vela, X.; Rodriguez, X.; Covani, U. clinical considerations on strategies that avoid multiple connections and disconnections of implant abutments. Int. J. Periodontics Restor. Dent. 2020, 40, 9–17. [Google Scholar] [CrossRef]
| Treatment Group | ||||
|---|---|---|---|---|
| PA (Control, n = 30) | DA (Test, n = 23) | Total (n = 53) | p-Value | |
| Sex (n and % of subjects) | ||||
| Male | 9 (30%) | 9 (39.1%) | 18(34%) | 0.565 |
| Female | 21 (70%) | 14 (60.1%) | 35(66%) | |
| Center (n and % of subjects) | ||||
| 07 | 15 (50%) | 10 (43.5%) | 25 (42.2%) | 0.782 |
| 08 | 15 (50%) | 13 (56.5%) | 28 (52.8%) | |
| Age (years) | ||||
| Median | 49.5 | 50.9 | 50.7 | |
| Range | 35–61 | 32–67 | 32–67 | |
| Smoking (n and % of subjects) | ||||
| Non-smoker | 26 (86.7%) | 21 (91.3%) | 47 | 0.687 |
| Smoker < 10 cigs/day | 4 (13.3%) | 2 (8.7%) | 6 | |
| Diabetes | ||||
| No | 28 (93.3%) | 23 (100%) | 51 | 0.499 |
| Yes | 2 (6.7%) | 0 (0.0%) | 2 | |
| ASA classification | ||||
| Type I | 25 (83.3%) | 21 (91.3%) | 46 | |
| Type II | 4 (13.3%) | 0 (0.0%) | 4 | |
| Type III | 1 (3.4%) | 2 (8.7%) | 3 | |
| Number of implants placed | ||||
| Single units | 15 (50.0%) | 13 (56.5%) | 28 | 0.782 |
| Multiple units | 15 (50.0%) | 10 (43.5%) | 25 | |
| Implants position | ||||
| Maxilla | 10 (33.3%) | 11 (47.8%) | 21 | |
| Mandible | 20 (66.7%) | 12 (52.2%) | 32 | |
| Bone Quality | ||||
| Type I | 0 (0.0%) | 0 (0.0%) | 0 | 1.000 |
| Type II | 10 (33.3%) | 7 (30.4%) | 17 | |
| Type III | 20 (66.7%) | 16 (69.6%) | 36 | |
| Type IV | 0 (0.0%) | 0 (0.0%) | 0 | |
| Implant diameter | ||||
| 4 mm | 23 | 17 | 40 | 1.000 |
| 4.5 mm | 7 | 6 | 13 | |
| Implant length | ||||
| 8 | 11 | 6 | 17 | 0.647 |
| 10 | 11 | 11 | 22 | |
| 12 | 8 | 6 | 14 | |
| Primary stability (No/Yes) | 0/30 (0.0%/100%) | 0/23 (0.0%/100%) | 0/53 | |
| Primary rotational stability (No/Yes) | 0/30 (0.0%/100%) | 0/23 (0.0%/100%) | 0/53 | |
| Resorbed ridge classification | ||||
| Converging walls | 15 (50.0%) | 9 (39.1%) | 24 | 0.170 |
| Parallel walls | 15 (50.0%) | 11 (47.8%) | 26 | |
| Ridge with undercuts | 0 (0.0%) | 3 (13.0%) | 3 | |
| Knife-edged ridge form | 0 (0.0%) | 0 (0.0%) | 0 | |
| Implant platform position (n and % of subjects) | ||||
| Epicrestal | 12 (40.0%) | 7 (30.4%) | 0.569 | |
| Sub-crestal | 18 (60.0%) | 16 (69.4%) | ||
| DA | PA | TOTAL | p | ||
|---|---|---|---|---|---|
| ISQ-1 | N | 23 | 30 | 53 | |
| Minimum | 70 | 63 | 63 | ||
| Maximum | 91 | 88 | 91 | ||
| Average | 82,6 | 79,6 | 80,9 | 0.570 | |
| SD | |||||
| ISQ-2 | N | 23 | 30 | 53 | |
| Minimum | 57 | 74 | 57 | ||
| Maximum | 93 | 90 | 93 | ||
| Average | 77,9 | 81,6 | 80 | 0.102 | |
| SD | |||||
| ISQ-3 | N | 23 | 30 | 53 | |
| Minimum | 69 | 71 | 69 | ||
| Maximum | 97 | 97 | 97 | ||
| Average | 79,7 | 79,4 | 80,8 | 0.360 | |
| SD | |||||
| ISQ-4 | N | 23 | 30 | 53 | |
| Minimum | 71 | 72 | 71 | ||
| Maximum | 98 | 95 | 98 | ||
| Average | 81,3 | 80,2 | 80,7 | 0.628 | |
| SD |
| mPLI | Group | Group | ||||||
|---|---|---|---|---|---|---|---|---|
| DA 6 Months | PA 6 Months | Total | p | DA 12 Months | PA 12 Months | Total | p | |
| Visible with probe | 21 | 22 | 43 | 0.225 | 19 | 24 | 43 | 0.767 |
| Visible | 2 | 6 | 8 | 1 | 3 | 4 | ||
| Abundant | 0 | 2 | 2 | 3 | 3 | 6 | ||
| Total | 23 | 30 | 53 | 23 | 30 | 53 | ||
| Modified Bleeding Index | Group | Group | ||||||
|---|---|---|---|---|---|---|---|---|
| DA 6 Months | PA 6 Months | Total | p | DA 12 Months | PA 12 Months | Total | p | |
| Punctual | 22 | 26 | 48 | 0.374 | 23 | 29 | 52 | 1.000 |
| Line in groove | 1 | 4 | 5 | 0 | 1 | 1 | ||
| Total | 23 | 30 | 53 | 23 | 30 | 53 | ||
| PD | Group | p | Group | p | ||||
|---|---|---|---|---|---|---|---|---|
| DA 6 Months | PA 6 Months | Total | DA 12 Months | PA 12 Months | Total | |||
| 0 | 18 | 29 | 47 | 0.074 | 19 | 27 | 36 | 0.451 |
| 1 | 5 | 1 | 6 | 4 | 3 | 7 | ||
| Total | 23 | 30 | 53 | 23 | 30 | 53 | ||
| 0 Months | 6 Months | 12 Months | ||
|---|---|---|---|---|
| Group PA (control) | mean ± SD | 0.05 ± 0.08 | 0.23 ± 0.29 | 0.21 ± 0.27 |
| median (p25;p75) | 0.00 (0.00, 0.08) | 0.14 (0.00, 0.32) | 0.13 (0.00, 0.26) | |
| Group DA (test) | mean ± SD | 0.03 ± 0.06 | 0.14 ± 0.18 | 0.14 ± 0.21 |
| median (p25;p75) | 0.00 (0.00, 0.03) | 0.05 (0.00, 0.27) | 0.03 (0.00, 0.24) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moreira, F.; Rocha, S.; Caramelo, F.; Tondela, J.P. One-Abutment One-Time Effect on Peri-Implant Marginal Bone: A Prospective, Controlled, Randomized, Double-Blind Study. Materials 2021, 14, 4179. https://doi.org/10.3390/ma14154179
Moreira F, Rocha S, Caramelo F, Tondela JP. One-Abutment One-Time Effect on Peri-Implant Marginal Bone: A Prospective, Controlled, Randomized, Double-Blind Study. Materials. 2021; 14(15):4179. https://doi.org/10.3390/ma14154179
Chicago/Turabian StyleMoreira, Filipe, Salomão Rocha, Francisco Caramelo, and João P. Tondela. 2021. "One-Abutment One-Time Effect on Peri-Implant Marginal Bone: A Prospective, Controlled, Randomized, Double-Blind Study" Materials 14, no. 15: 4179. https://doi.org/10.3390/ma14154179
APA StyleMoreira, F., Rocha, S., Caramelo, F., & Tondela, J. P. (2021). One-Abutment One-Time Effect on Peri-Implant Marginal Bone: A Prospective, Controlled, Randomized, Double-Blind Study. Materials, 14(15), 4179. https://doi.org/10.3390/ma14154179






