Comparison of the Masticatory Force (with 3D Models) of Complete Denture Base Acrylic Resins with Reline and Reinforcing Materials
Abstract
1. Introduction
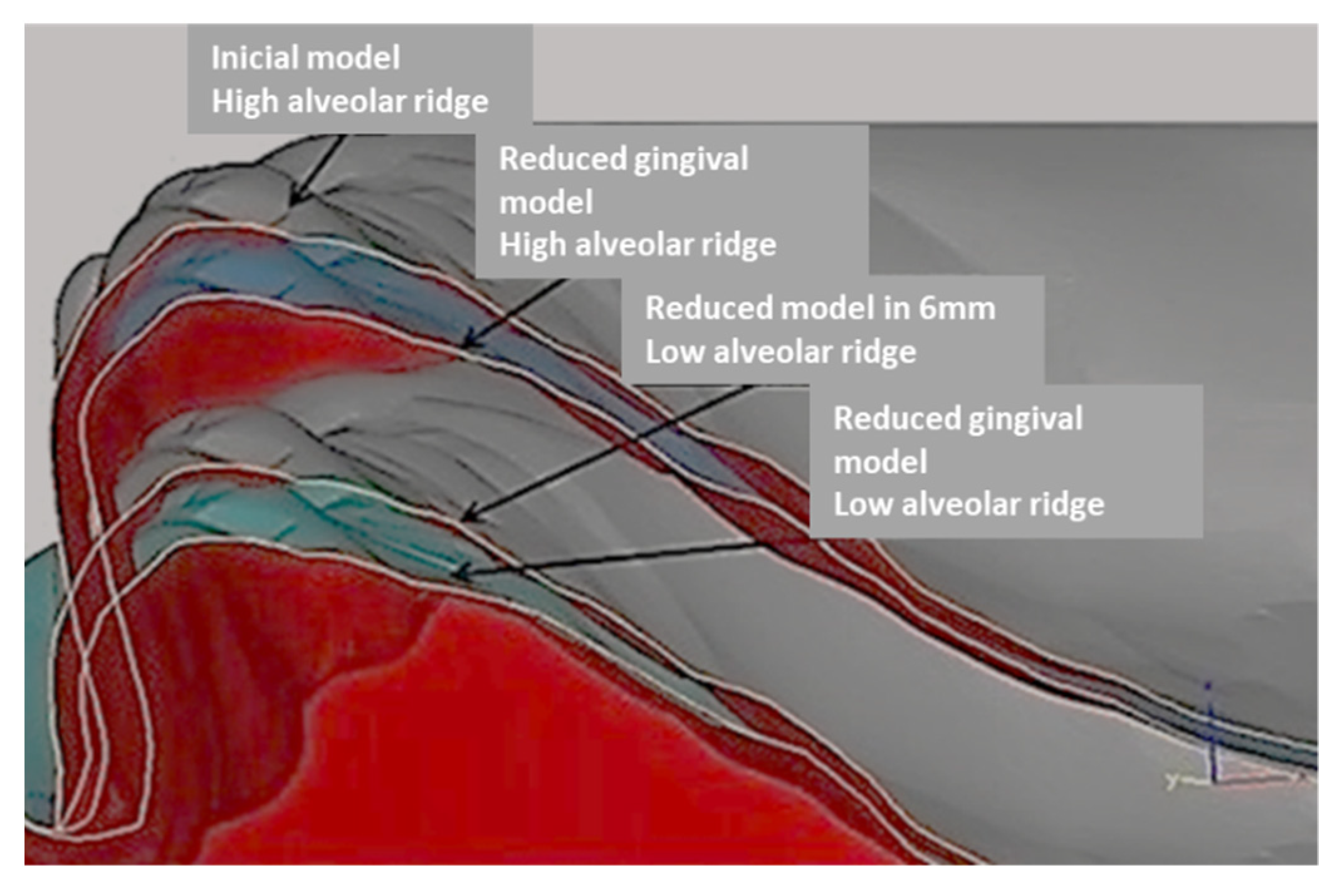
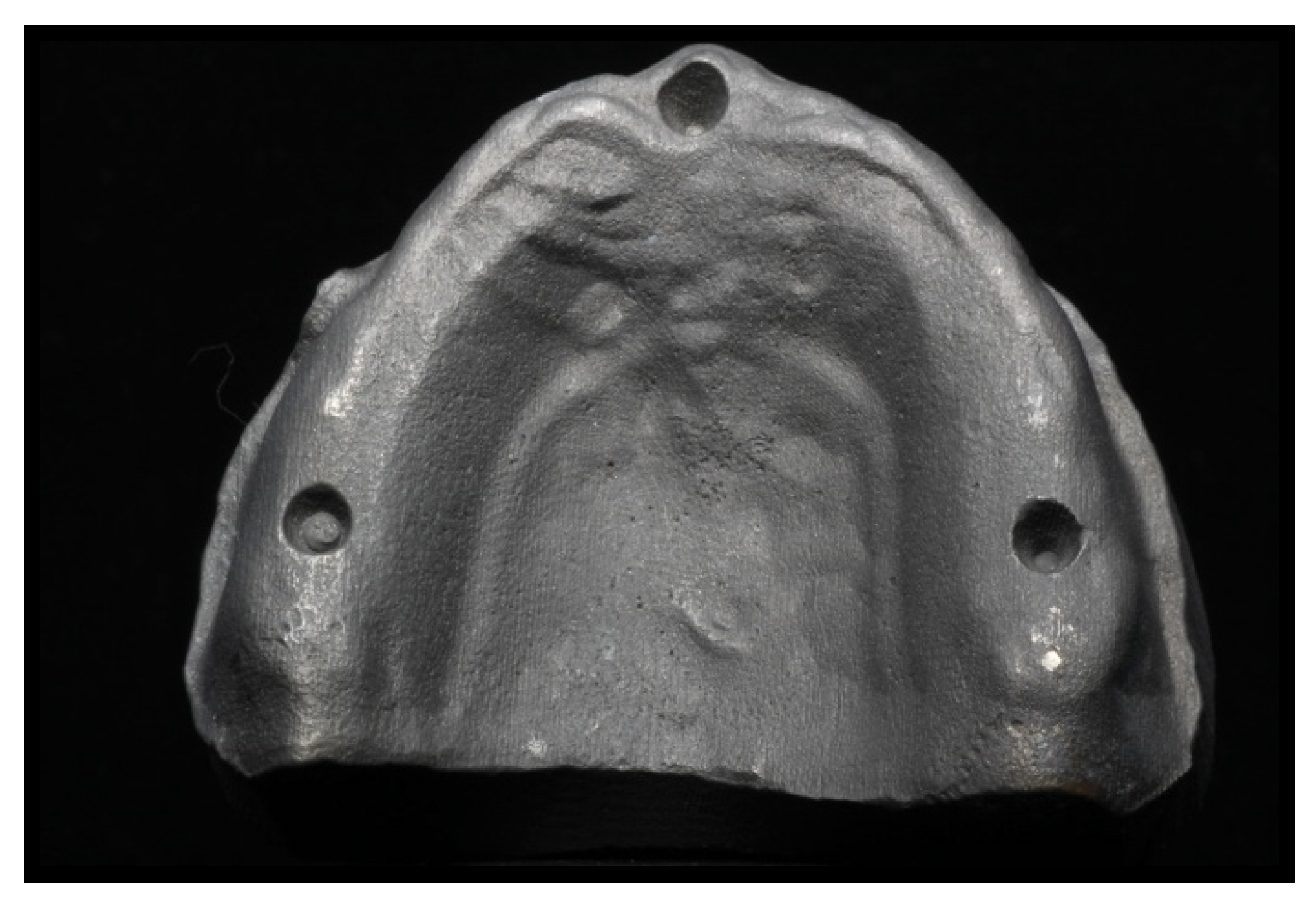
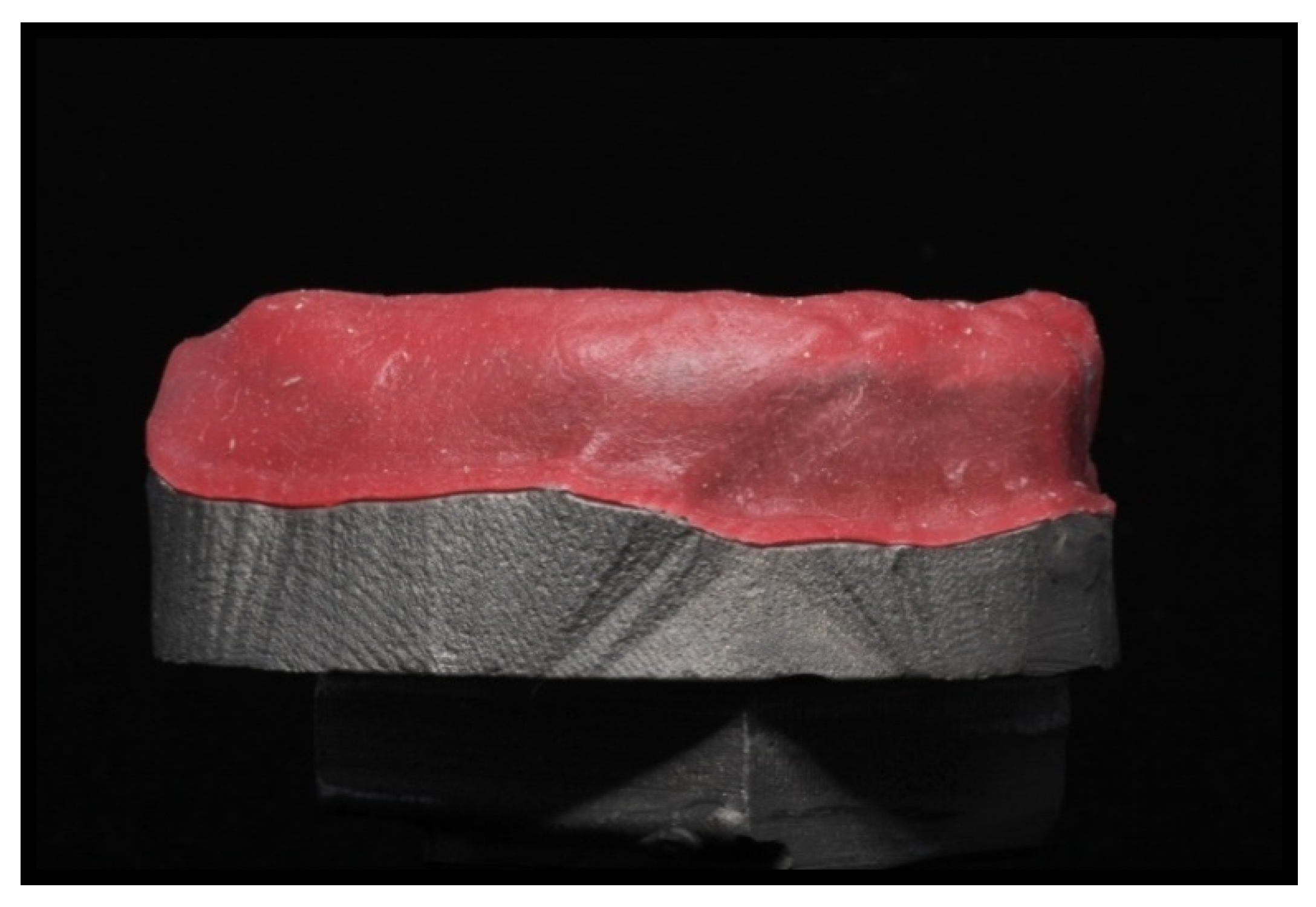
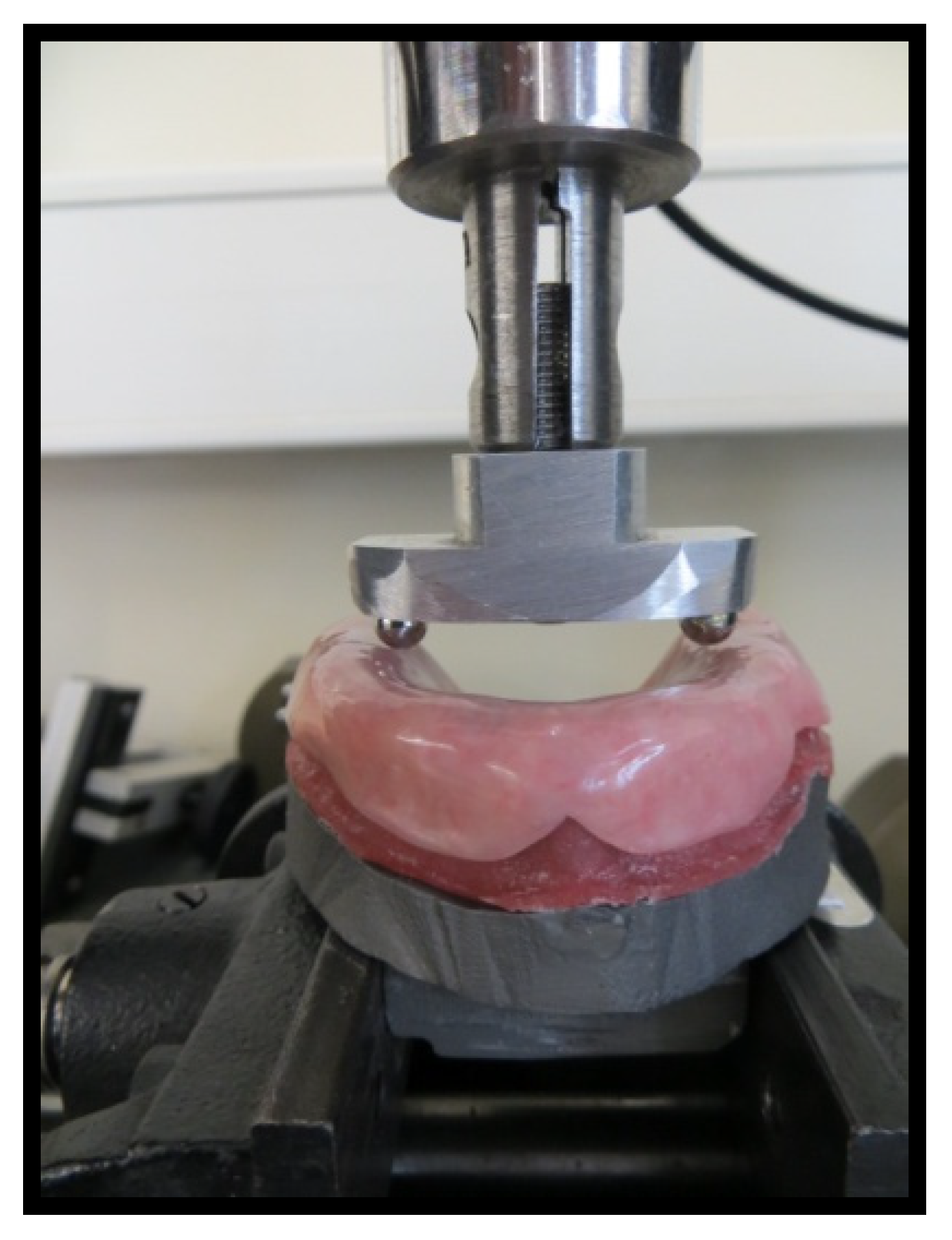
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vallittu, P.K. Flexural properties of acrylic resin polymers reinforced with unidirectional and woven glass fibers. J. Prosthet. Dent. 1999, 81, 318–326. [Google Scholar] [CrossRef]
- Praveen, B.; Babaji, H.V.; Prasanna, B.G.; Rajalbandi, S.K.; Sheeharsha, T.V.; Prashant, G.M. Comparison of Impact strength and fracture morphology of different heat Cure denture acrylic resins: An in vitro study. J. Int. Oral Health 2014, 6, 12–16. [Google Scholar] [PubMed]
- De Sá, J.; Vieira, F.; Aroso, C.M.; Cardoso, M.; Mendes, J.M.; Silva, A.S. The influence of saliva pH on the fracture resistance of three complete denture base acrylic resins. Int. J. Dent. 2020, 2020, 8941876. [Google Scholar] [PubMed]
- Silva, A.S.; Carvalho, A.; Barreiros, P.; de Sá, J.; Aroso, C.; Mendes, J.M. Comparison of fracture resistance in thermal and self-curing acrylic resins—An in vitro study. Polymers 2021, 13, 1234. [Google Scholar] [CrossRef] [PubMed]
- Jagger, D.; Harrison, A.; Vowles, R.; Jagger, R. The effect of the addition of surface treated chopped and continuous poly (methyl methacrylate) fibres on some properties of acrylic resins. J. Oral Rehabil. 2001, 28, 865–872. [Google Scholar] [CrossRef] [PubMed]
- Tsue, F.; Takahashi, Y.; Shimizu, H. Reinforcing effect of glass-fiber-reinforced composite on flexural strength at the proportional limit of denture base resin. Acta Odontol. Scand. 2007, 65, 141–148. [Google Scholar] [CrossRef]
- Yu, S.-H.; Cho, H.-W.; Oh, S.; Bae, J.-M. Effects of glass fiber mesh with different fiber content and structures on the compressive properties of complete dentures. J. Prosthet Dent. 2015, 113, 636–644. [Google Scholar] [CrossRef]
- Alla, R.K.; Sajjan, S.; Alluri, V.R.; Ginjupalli, K.; Upadhya, N. Influence of fiber reinforcement on the properties of denture base resins. J. Biomater. Nanobiotechnol. 2013, 4, 91–97. [Google Scholar] [CrossRef]
- Dogan, O.M.; Bolayir, G.; Keshin, S.; Dogan, A.; Bek, B. The evaluation of some flexural properties of a denture base resin reinforced with various aesthetic fibers. J. Mater. Sci. Mater. Med. 2008, 19, 2343–2349. [Google Scholar] [CrossRef]
- Mansour, M.M.; Wagner, W.C.; Chu, T.G. Effect of MICA reinforcement on the flexural strength and microhardness of polymethyl methacrylate denture resin. J. Prosthodont. 2013, 22, 179–183. [Google Scholar] [CrossRef]
- Xu, J.; Li, Y.; Yu, T.; Cong, L. Reinforcement of denture base resin with short vegetable fiber. Dent. Mater. 2013, 29, 1273–1279. [Google Scholar] [CrossRef]
- Polizzi, E.; Tetè, G.; Targa, C.; Gastaldi, G. Evaluation of the effectiveness of the use of the Diodo Laser in the reduction of the volume of the edematous gingival tissue after causal therapy. Int. J. Environ. Res. Public Health 2020, 17, 6192. [Google Scholar] [CrossRef]
- Mohammed, S.A.; Hassen, K.S. Evaluation of some properties of four silicon based soft dentures reliner materials. J. Bagh. Coll. Dent. 2011, 23, 36–42. [Google Scholar]
- Ciancaglini, R.; Gherlone, E.F.; Redaelli, S. The distribution of occlusal contacts in the intercuspal position and temporomandibular disorder. J. Oral Rehabil. 2002, 29, 1082–1090. [Google Scholar] [CrossRef] [PubMed]
- Vojvodic, D.; Komar, D.; Schauperl, Z.; Celebic, A.; Mehulic, K.; Zabarovic, D. Influence of different glass fiber reinforcements on denture base polymer strength (Fiber reinforcements of dental polymer). Med. Glass 2009, 6, 227–234. [Google Scholar]
- Takahashi, Y.; Yoshida, K.; Shimizu, H. Effect of location of glass fiber-reinforced composite reinforcement on the flexural properties of a maxillary complete denture in vitro. Acta Odontol. Scand. 2011, 69, 215–221. [Google Scholar] [CrossRef] [PubMed]
- Cattoni, F.; Tetè, G.; Calloni, A.M.; Manazza, F.; Gastaldi, G.; Capparè, P. Milled versus moulded mock-ups based on the superimposition of 3D meshehes from digital oral impressions: A comparative in vitro study in the aesthetic area. BMC Oral Health 2019, 19, 230. [Google Scholar] [CrossRef] [PubMed]
- Prombonas, A.E.; Vlissidis, D.S.; Maria, P.A.; Nikolas, P.A. The stress state of the fraenal notch region in complete upper dentures. Med. Eng. Phys. 2012, 34, 1477–1482. [Google Scholar] [CrossRef]
- Ates, M.; Çilingir, A.; Sülün, T.; Sunbuloglu, E.; Bozdag, E. The effect of occlusal contact localization on the stress distribution in complete maxillary denture. J. Oral Rehabil. 2006, 33, 509–513. [Google Scholar] [CrossRef]
- Hirajima, Y.; Takahashi, H.; Minakushi, S. Influence of a denture strengthener on the deformation of a maxillary complete denture. Dent. Mater. J. 2009, 28, 507–512. [Google Scholar] [CrossRef][Green Version]
- Vogdani, M.; Bagheri, R.; Khaledi, A.A.R. Effects of aluminum oxide addition on the flexural strength, surface hardness, and roughness of heat-polymerized acrylic resin. J. Dent. Sci. 2012, 7, 238–244. [Google Scholar] [CrossRef]
- Foo, S.H.; Lindquist, T.J.; Aquilino, S.A.; Schneider, R.L.; Williamson, D.L.; Boyer, D.B. Effect of polyaramid fiber reinforcement on the strength of 3 Denture Base polymethyl methacrylate resin. J. Prosthodont. 2001, 3, 148–153. [Google Scholar] [CrossRef] [PubMed]
- Balch, J.H.; Smith, P.D.; Marin, M.A.; Cagna, D.R. Reinforcement of a mandibular complete denture with internal metal framework. J. Prosthet. Dent. 2013, 109, 202–205. [Google Scholar] [CrossRef]
- Teraoka, F.; Nakagawa, M.; Takahashi, J. Adaptation of Acrylic dentures reinforced with metal wire. J. Oral Rehabil. 2001, 28, 937–942. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, H.; Mori, N.; Takahashi, Y. Use of metal conditioner on reinforcement wires. N. Y. State Dent. J. 2008, 74, 26. [Google Scholar]
- Yoshida, K.; Takashashi, Y.; Shimizu, H. Effect of embedded metal reinforcements and their location on the fracture resistance of acrylic resin complete dentures. J. Prosthodont. 2011, 20, 366–371. [Google Scholar] [CrossRef]
- Jagger, D.C.; Harrison, A.; Jandt, K.D. The reinforcement of dentures-review. J. Oral Rehabil. 1999, 26, 185–194. [Google Scholar] [CrossRef]
- Chen, S.Y.; Liang, W.M.; Yen, P.S. Reinforcement of acrylic denture base resin by incorporation of various fibers. J. Biomed. Mater. Res. 2001, 58, 203–208. [Google Scholar] [CrossRef]
- Bertassoni, L.E.; Marshall, G.W.; Souza, E.M.; Rached, R.N. Effect of pre and post polymerization on flexural strength and elastic modules of impregnated, fiber-reinforced denture base acrylic resins. J. Prosthet. Dent. 2008, 100, 449–457. [Google Scholar] [CrossRef]
- Kanie, T.; Arikawa, H.; Fujii, K.; Ban, S. Impact strength of acrylic denture base resin reinforced with woven glass fiber. Dent. Mater. J. 2003, 22, 30–38. [Google Scholar] [CrossRef]
- Koroglu, A.; Ozdemir, T.; Pamir, A.D.; Usanmaz, A. Residual acrylic monomer content of denture base resins with different fiber systems. J. Appl. Polym. Sci. 2012, 125, 471–476. [Google Scholar] [CrossRef]
- Takahashi, Y.; Yoshida, K.; Shimizu, H. Fracture resistance of maxillary complete dentures subjected to long term water immersion. Gerodontology 2012, 29, e1086–e1091. [Google Scholar] [CrossRef]
- Yu, S.-H.; Lee, Y.; Oh, S.; Cho, H.-W.; Oda, Y.; Bae, J.-M. Reinforcing effects of different fibers on denture base resin based on the fiber type, concentration, and combination. Dent. Mater. J. 2012, 31, 1039–1046. [Google Scholar] [CrossRef]
- Cheng, Y.Y.; Cheung, W.L.; Chow, T.W. Strain analysis of maxillary complete denture with three-dimensional finite element method. J. Prosthet. Dent. 2010, 103, 309–318. [Google Scholar] [CrossRef]
- Cheng, Y.Y.; Li, J.Y.; Cheung, W.L.; Chow, T.W. 3D FEA of high-performance polyethylene fiber reinforced maxillary dentures. Dent. Mater. 2010, 26, e211–e219. [Google Scholar] [CrossRef] [PubMed]
- Denir, H.; Dogan, A.; Dogan, O.M.; Keskin, S.; Bolayir, G.; Soygun, K. Peel bond strength of two silicone soft liners to a heat-cured denture base resin. J. Adhes. Dent. 2011, 13, 579–584. [Google Scholar]
- Hatamleh, M.M.; Maryan, C.J.; Silikas, N.; Watts, D.C. Effect of net fiber reinforcement surface treatment on soft denture liner retention and longevity. J. Prosthodont. 2010, 19, 258–262. [Google Scholar] [CrossRef] [PubMed]



| Material | Trademark | Lot | Characteristics |
|---|---|---|---|
| PMMA | Lucitone 199® by Dentsply Sirona | 110,517; York, PA, USA | Terminal acrylic Conventional |
| Glass fibre mesh | FiBER FORCE® by Synca | 13,176; Bio Composants MédicauxTM, Tullins, France | Pre-impregnated |
| Metal inox mesh | Dentaurum® | 440,990; Ispringen, Germany | - |
| Reline material | Molloplast B® | 160,526; Ettlingen, Germany | Permanent soft reline |
| Material | High Alveolar Ridge | Low Alveolar Ridge |
|---|---|---|
| Lucitone 199® | 10 | 10 |
| FiBER FORCE® | 10 | 10 |
| Metal mesh Dentaurum® | 10 | 10 |
| Permanent soft reline Molloplast-B® | 10 | 10 |
| n = 40 | n = 40 |
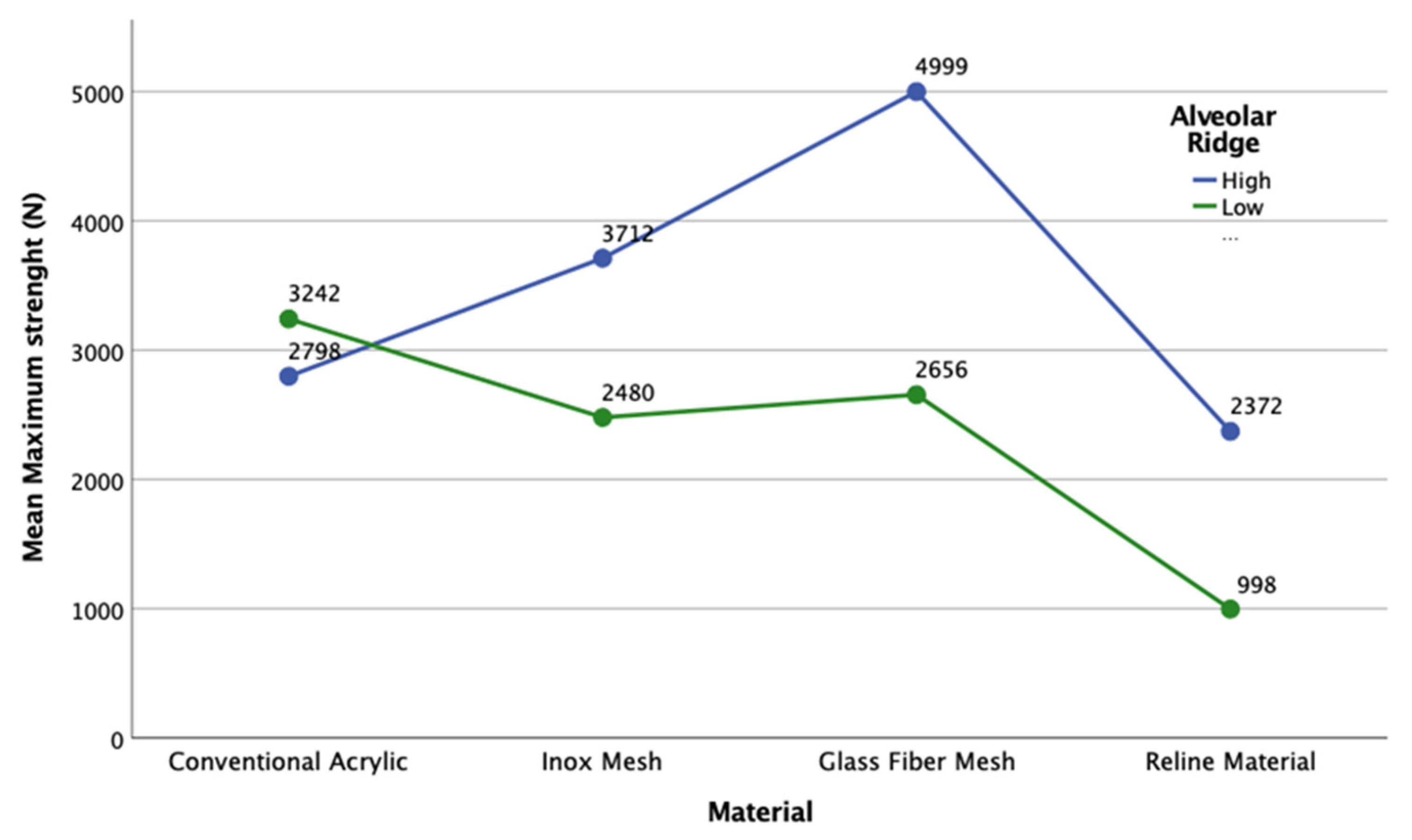
| Material | High Alveolar Ridge | Low Alveolar Ridge | p-Value † | |||
|---|---|---|---|---|---|---|
| Mean (N) | SD | Mean (N) | SD | Difference * (N) | ||
| Lucitone 199® | 2798.28 | 2055.13 | 3241.80 | 1661.34 | −443.51 | 0.786 |
| Metal mesh Dentaurum® | 3711.57 | 2227.96 | 2480.13 | 148.08 | 1231.44 | 0.440 |
| Glass fibre mesh FiBER FORCE® | 4999.07 | 0.48 | 2655.67 | 1127.52 | 2343.40 | 0.069 |
| Permanent soft reline Molloplast-B® | 2372.30 | 2273.92 | 997.93 | 157.59 | 1374.37 | 0.405 |
| p-Value ‡ | 0.394 | - | 0.118 | - | - | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Calamote, C.; Coelho, I.C.; Silva, A.S.; Esteves, J.L.; Moreira, L.; Pinto, A.C.; Manzanares-Céspedes, M.C.; Escuín, T. Comparison of the Masticatory Force (with 3D Models) of Complete Denture Base Acrylic Resins with Reline and Reinforcing Materials. Materials 2021, 14, 3308. https://doi.org/10.3390/ma14123308
Calamote C, Coelho IC, Silva AS, Esteves JL, Moreira L, Pinto AC, Manzanares-Céspedes MC, Escuín T. Comparison of the Masticatory Force (with 3D Models) of Complete Denture Base Acrylic Resins with Reline and Reinforcing Materials. Materials. 2021; 14(12):3308. https://doi.org/10.3390/ma14123308
Chicago/Turabian StyleCalamote, Catarina, Isabel Carolina Coelho, António Sérgio Silva, José Luís Esteves, Luís Moreira, António Correia Pinto, María Cristina Manzanares-Céspedes, and Tomás Escuín. 2021. "Comparison of the Masticatory Force (with 3D Models) of Complete Denture Base Acrylic Resins with Reline and Reinforcing Materials" Materials 14, no. 12: 3308. https://doi.org/10.3390/ma14123308
APA StyleCalamote, C., Coelho, I. C., Silva, A. S., Esteves, J. L., Moreira, L., Pinto, A. C., Manzanares-Céspedes, M. C., & Escuín, T. (2021). Comparison of the Masticatory Force (with 3D Models) of Complete Denture Base Acrylic Resins with Reline and Reinforcing Materials. Materials, 14(12), 3308. https://doi.org/10.3390/ma14123308








