What the Surgeon Can Do to Reduce the Risk of Trunnionosis in Hip Arthroplasty: Recommendations from the Literature
Abstract
1. Introduction
2. Technical Aspects of Taper Connections in Hip Arthroplasty
3. Patient-Related Factors for Trunnionosis
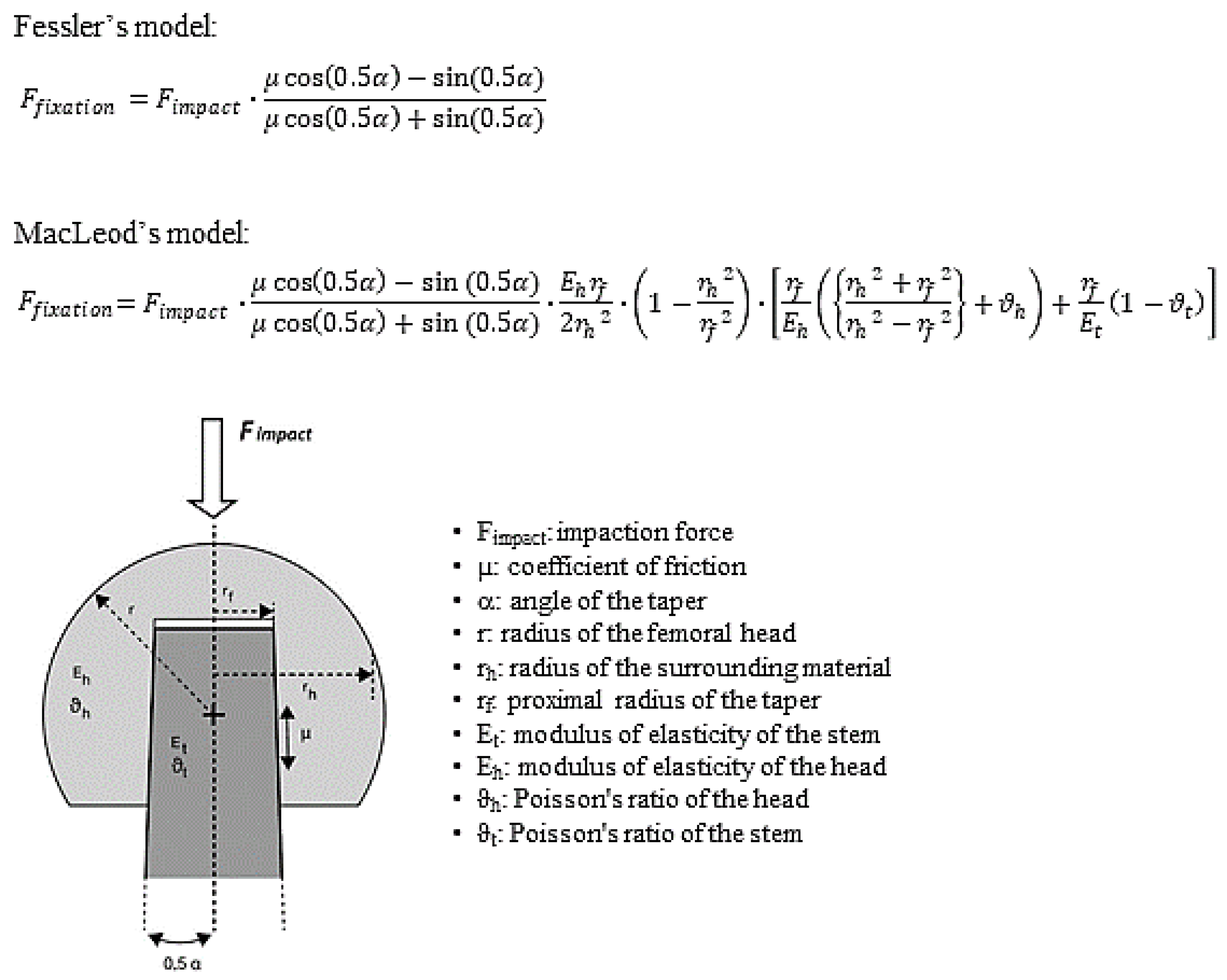
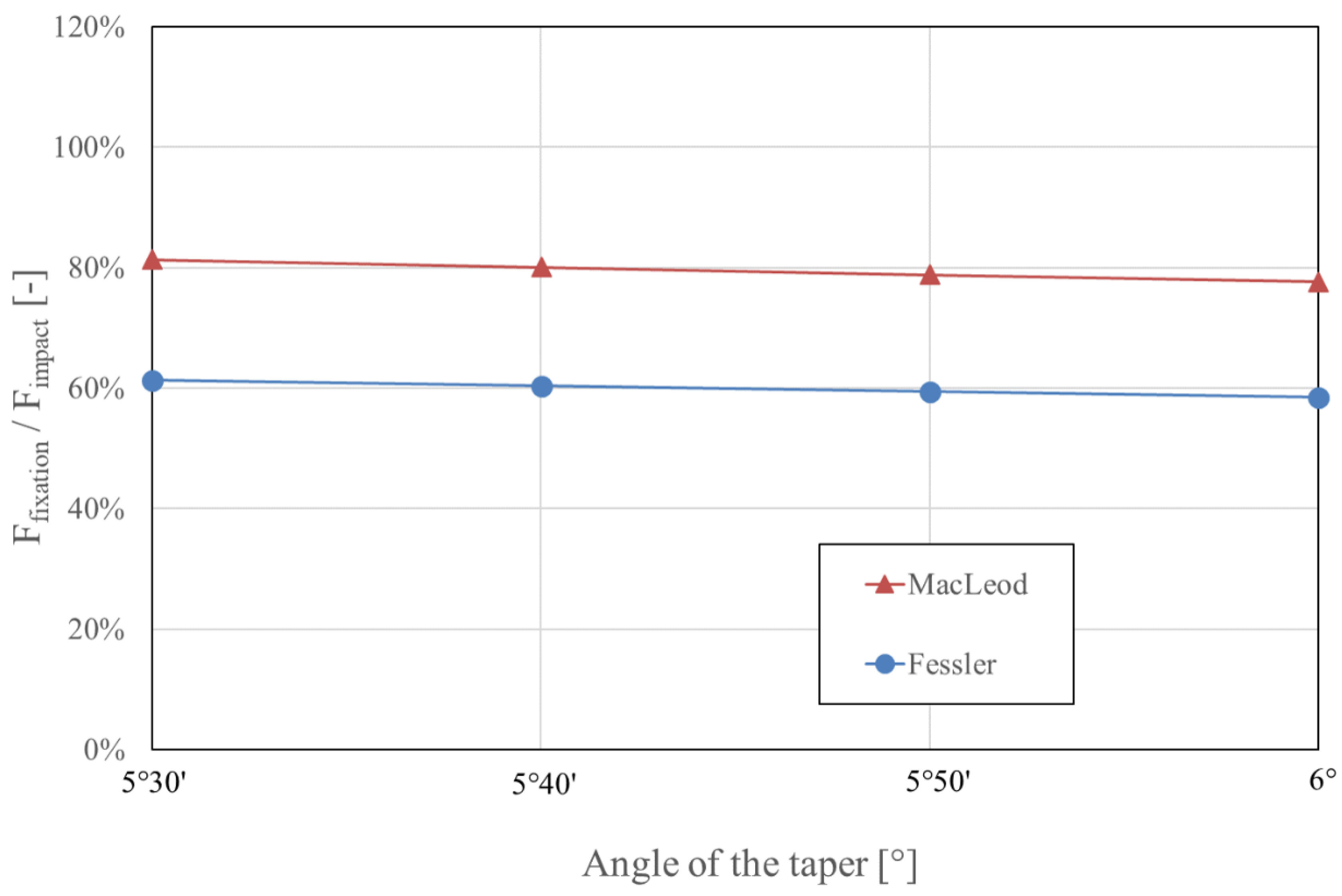
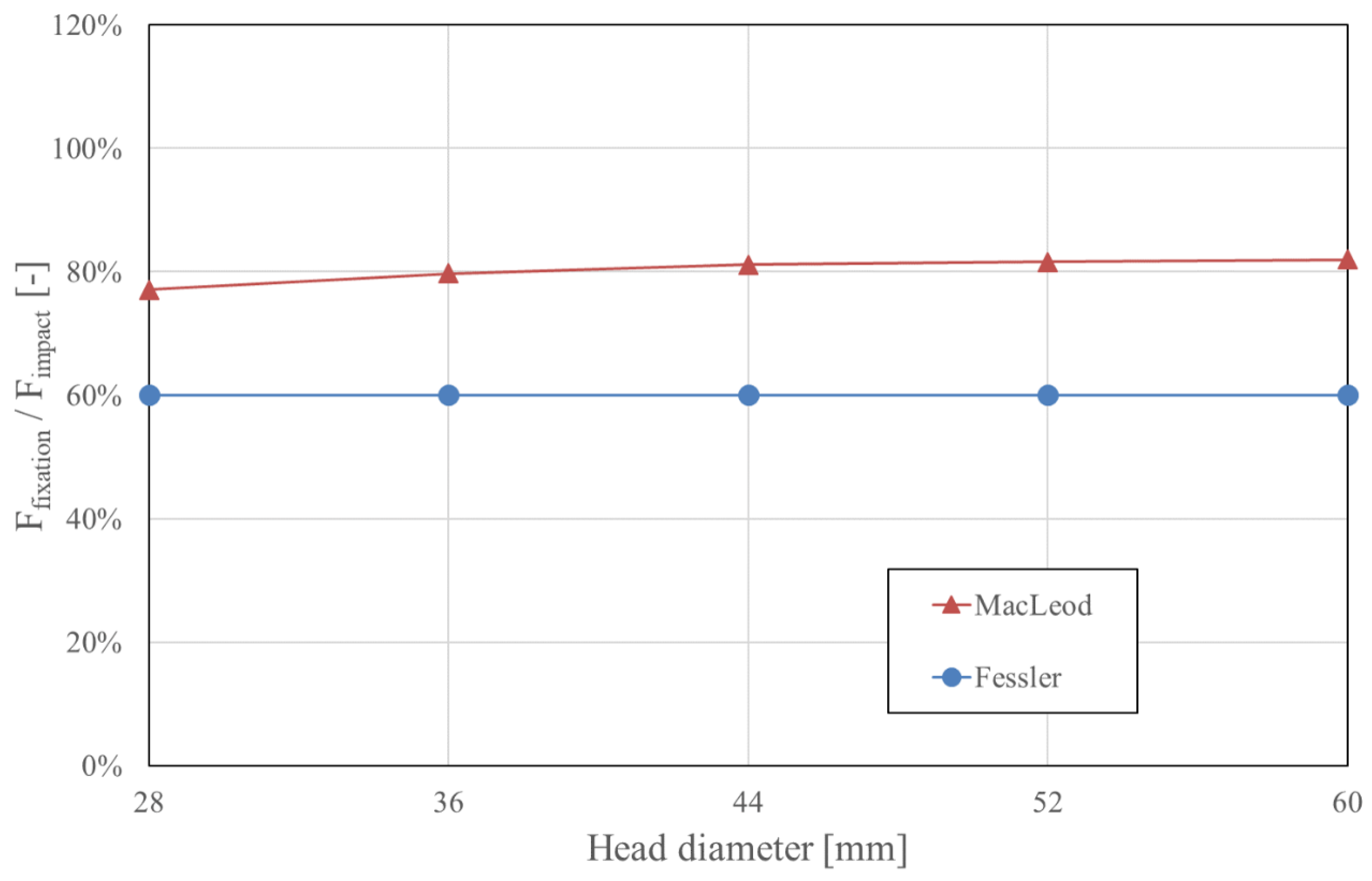
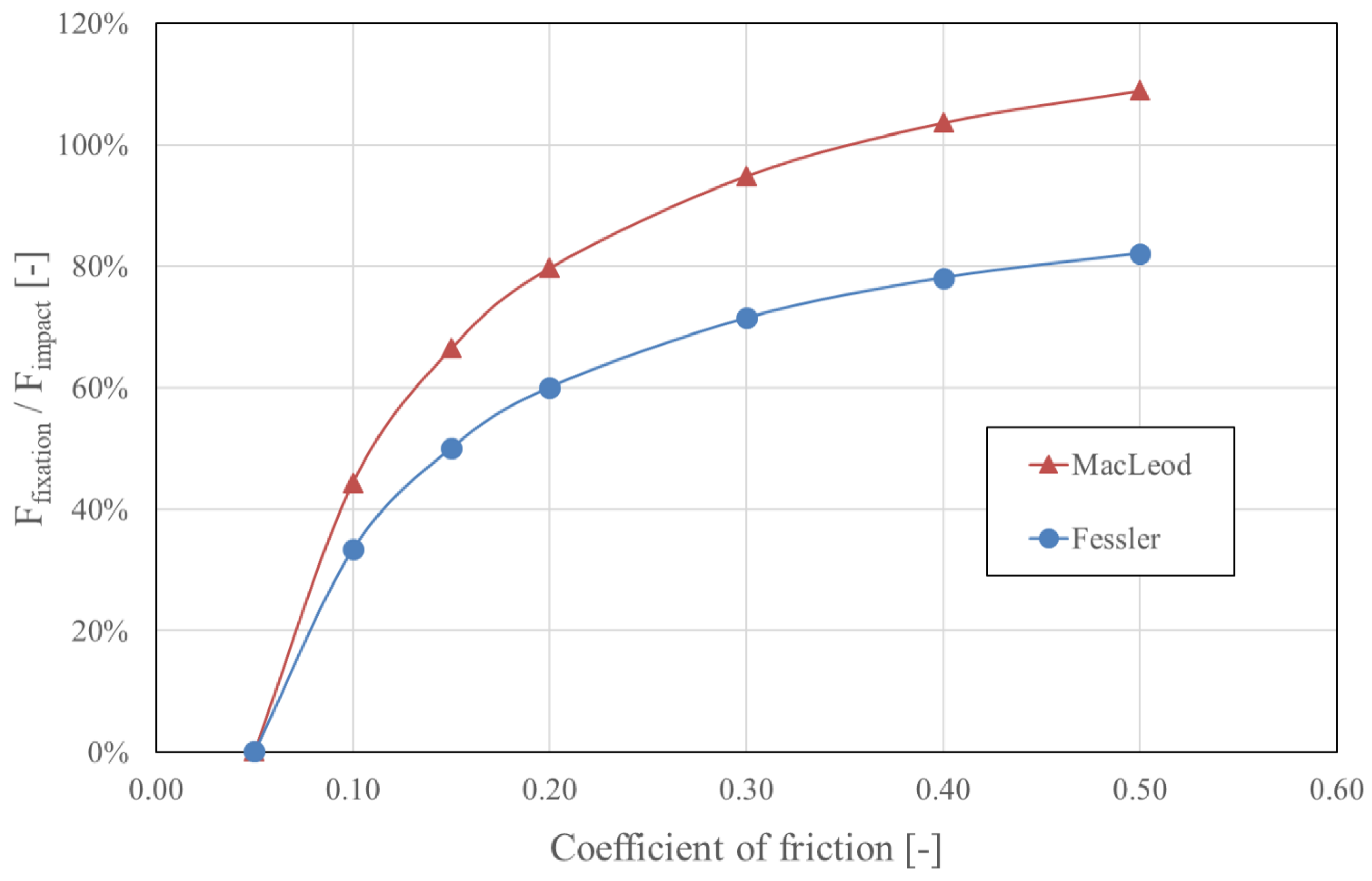
4. Surgeon-Related Factors Determining Taper Fixation
5. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Lindgren, J.V.; Wretenberg, P.; Karrholm, J.; Garellick, G.; Rolfson, O. Patient-reported outcome is influenced by surgical approach in total hip replacement: A study of the Swedish Hip Arthroplasty Register including 42,233 patients. Bone Jt. J. 2014, 96-B, 590–596. [Google Scholar] [CrossRef] [PubMed]
- Learmonth, I.D.; Young, C.; Rorabeck, C. The operation of the century: Total hip replacement. Lancet (Lond. Engl.) 2007, 370, 1508–1519. [Google Scholar] [CrossRef]
- Sadoghi, P.; Schroder, C.; Fottner, A.; Steinbruck, A.; Betz, O.; Muller, P.E.; Jansson, V.; Holzer, A. Application and survival curve of total hip arthroplasties: A systematic comparative analysis using worldwide hip arthroplasty registers. Int. Orthop. 2012, 36, 2197–2203. [Google Scholar] [CrossRef] [PubMed]
- Evans, J.T.; Evans, J.P.; Walker, R.W.; Blom, A.W.; Whitehouse, M.R.; Sayers, A. How long does a hip replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up. Lancet (Lond. Engl.) 2019, 393, 647–654. [Google Scholar] [CrossRef]
- Esposito, C.I.; Wright, T.M.; Goodman, S.B.; Berry, D.J.; Clinical, B.; Bioengineering Study Groups from Carl, T.B.W. What is the trouble with trunnions? Clin. Orthop. Relat. Res. 2014, 472, 3652–3658. [Google Scholar] [CrossRef]
- Rehmer, A.; Bishop, N.E.; Morlock, M.M. Influence of assembly procedure and material combination on the strength of the taper connection at the head-neck junction of modular hip endoprostheses. Clin. Biomech. (Bristolavon) 2012, 27, 77–83. [Google Scholar] [CrossRef]
- Barrack, R.L. Modularity of Prosthetic Implants. J. Am. Acad. Orthop. Surg. 1994, 2, 16–25. [Google Scholar] [CrossRef]
- Cameron, H.U. Modularity in primary total hip arthroplasty. J. Arthroplast. 1996, 11, 332–334; discussion 337–338. [Google Scholar] [CrossRef]
- McCarthy, J.C.; Bono, J.V.; O’Donnell, P.J. Custom and modular components in primary total hip replacement. Clin. Orthop. Relat. Res. 1997, 344, 162–171. [Google Scholar] [CrossRef]
- Lavernia, C.J.; Baerga, L.; Barrack, R.L.; Tozakoglou, E.; Cook, S.D.; Lata, L.; Rossi, M.D. The effects of blood and fat on Morse taper disassembly forces. Am. J. Orthop. (Belle Mead Nj) 2009, 38, 187–190. [Google Scholar]
- Cooper, H.J.; Della Valle, C.J.; Berger, R.A.; Tetreault, M.; Paprosky, W.G.; Sporer, S.M.; Jacobs, J.J. Corrosion at the head-neck taper as a cause for adverse local tissue reactions after total hip arthroplasty. J. Bone Jt. Surg. Am. 2012, 94, 1655–1661. [Google Scholar] [CrossRef] [PubMed]
- Hussey, D.K.; McGrory, B.J. Ten-Year Cross-Sectional Study of Mechanically Assisted Crevice Corrosion in 1352 Consecutive Patients with Metal-on-Polyethylene Total Hip Arthroplasty. J. Arthroplast. 2017, 32, 2546–2551. [Google Scholar] [CrossRef] [PubMed]
- Urish, K.L.; Hamlin, B.R.; Plakseychuk, A.Y.; Levison, T.J.; Higgs, G.B.; Kurtz, S.M.; DiGioia, A.M. Trunnion Failure of the Recalled Low Friction Ion Treatment Cobalt Chromium Alloy Femoral Head. J. Arthroplast. 2017, 32, 2857–2863. [Google Scholar] [CrossRef] [PubMed]
- Kurtz, S.M.; Kocagoz, S.B.; Hanzlik, J.A.; Underwood, R.J.; Gilbert, J.L.; MacDonald, D.W.; Lee, G.C.; Mont, M.A.; Kraay, M.J.; Klein, G.R.; et al. Do ceramic femoral heads reduce taper fretting corrosion in hip arthroplasty? A retrieval study. Clin. Orthop. Relat. Res. 2013, 471, 3270–3282. [Google Scholar] [CrossRef] [PubMed]
- Witt, F.; Bosker, B.H.; Bishop, N.E.; Ettema, H.B.; Verheyen, C.C.; Morlock, M.M. The relation between titanium taper corrosion and cobalt-chromium bearing wear in large-head metal-on-metal total hip prostheses: A retrieval study. J. Bone Jt. Surg. Am. 2014, 96, e157. [Google Scholar] [CrossRef] [PubMed]
- McGrory, B.J.; MacKenzie, J.; Babikian, G. A High Prevalence of Corrosion at the Head-Neck Taper with Contemporary Zimmer Non-Cemented Femoral Hip Components. J. Arthroplast. 2015, 30, 1265–1268. [Google Scholar] [CrossRef]
- Kwon, Y.M.; Khormaee, S.; Liow, M.H.; Tsai, T.Y.; Freiberg, A.A.; Rubash, H.E. Asymptomatic Pseudotumors in Patients with Taper Corrosion of a Dual-Taper Modular Femoral Stem: MARS-MRI and Metal Ion Study. J. Bone Jt. Surg. Am. 2016, 98, 1735–1740. [Google Scholar] [CrossRef]
- McGrory, B.J.; Payson, A.M.; MacKenzie, J.A. Elevated Intra-Articular Cobalt and Chromium Levels in Mechanically Assisted Crevice Corrosion in Metal-on-Polyethylene Total Hip Arthroplasty. J. Arthroplast. 2017, 32, 1654–1658. [Google Scholar] [CrossRef]
- Goldberg, J.R.; Gilbert, J.L.; Jacobs, J.J.; Bauer, T.W.; Paprosky, W.; Leurgans, S. A multicenter retrieval study of the taper interfaces of modular hip prostheses. Clin. Orthop. Relat. Res. 2002, 149–161. [Google Scholar] [CrossRef]
- Morlock, M.M. The taper disaster--how could it happen? Hip Int. 2015, 25, 339–346. [Google Scholar] [CrossRef] [PubMed]
- Falkenberg, A.; Biller, S.; Morlock, M.M.; Huber, G. Micromotion at the head-stem taper junction of total hip prostheses is influenced by prosthesis design-, patient- and surgeon-related factors. J. Biomech. 2019, in press. [Google Scholar] [CrossRef] [PubMed]
- Higgs, G.B.; Hanzlik, J.A.; MacDonald, D.W.; Gilbert, J.L.; Rimnac, C.M.; Kurtz, S.M.; Implant Research Center Writing, C. Is increased modularity associated with increased fretting and corrosion damage in metal-on-metal total hip arthroplasty devices?: A retrieval study. J. Arthroplast. 2013, 28, 2–6. [Google Scholar] [CrossRef]
- Morlock, M.; Bunte, D.; Guhrs, J.; Bishop, N. Corrosion of the Head-Stem Taper Junction-Are We on the Verge of an Epidemic?: Review Article. Hss J. 2017, 13, 42–49. [Google Scholar] [CrossRef] [PubMed]
- Hussenbocus, S.; Kosuge, D.; Solomon, L.B.; Howie, D.W.; Oskouei, R.H. Head-neck taper corrosion in hip arthroplasty. Biomed. Res. Int. 2015, 2015, 758123. [Google Scholar] [CrossRef] [PubMed]
- Pourzal, R.; Lundberg, H.J.; Hall, D.J.; Jacobs, J.J. What Factors Drive Taper Corrosion? J. Arthroplast. 2018, 33, 2707–2711. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, J.L.; Buckley, C.A.; Jacobs, J.J. In vivo corrosion of modular hip prosthesis components in mixed and similar metal combinations. The effect of crevice, stress, motion, and alloy coupling. J. Biomed. Mater. Res. 1993, 27, 1533–1544. [Google Scholar] [CrossRef]
- Jacobs, J.J.; Gilbert, J.L.; Urban, R.M. Corrosion of metal orthopaedic implants. J. Bone Jt. Surg. Am. 1998, 80, 268–282. [Google Scholar] [CrossRef]
- Chalmers, B.P.; Perry, K.I.; Taunton, M.J.; Mabry, T.M.; Abdel, M.P. Diagnosis of adverse local tissue reactions following metal-on-metal hip arthroplasty. Curr. Rev. Musculoskelet Med. 2016, 9, 67–74. [Google Scholar] [CrossRef]
- Kwon, Y.M.; Fehring, T.K.; Lombardi, A.V.; Barnes, C.L.; Cabanela, M.E.; Jacobs, J.J. Risk stratification algorithm for management of patients with dual modular taper total hip arthroplasty: Consensus statement of the American Association of Hip and Knee Surgeons, the American Academy of Orthopaedic Surgeons and the Hip Society. J. Arthroplast. 2014, 29, 2060–2064. [Google Scholar] [CrossRef]
- Krenn, V.; Morawietz, L.; Perino, G.; Kienapfel, H.; Ascherl, R.; Hassenpflug, G.J.; Thomsen, M.; Thomas, P.; Huber, M.; Kendoff, D.; et al. Revised histopathological consensus classification of joint implant related pathology. Pathol. Res. Pract. 2014, 210, 779–786. [Google Scholar] [CrossRef] [PubMed]
- Abu-Amer, Y.; Darwech, I.; Clohisy, J.C. Aseptic loosening of total joint replacements: Mechanisms underlying osteolysis and potential therapies. Arthritis Res. Ther. 2007, 9 (Suppl. 1), S6. [Google Scholar] [CrossRef] [PubMed]
- Banerjee, S.; Cherian, J.J.; Bono, J.V.; Kurtz, S.M.; Geesink, R.; Meneghini, R.M.; Delanois, R.E.; Mont, M.A. Gross trunnion failure after primary total hip arthroplasty. J. Arthroplast. 2015, 30, 641–648. [Google Scholar] [CrossRef] [PubMed]
- Bolarinwa, S.A.; Martino, J.M.; Moskal, J.T.; Wolfe, M.W.; Shuler, T.E. Gross trunnion failure after a metal-on-polyethylene total hip arthroplasty leading to dissociation at the femoral head-trunnion interface. Arthroplast. Today 2019, 5, 5–10. [Google Scholar] [CrossRef] [PubMed]
- Bansal, T.; Aggarwal, S.; Dhillon, M.S.; Patel, S. Gross trunnion failure in metal on polyethylene total hip arthroplasty-a systematic review of literature. Int. Orthop. 2020. [Google Scholar] [CrossRef]
- Hernigou, P.; Queinnec, S.; Flouzat Lachaniette, C.H. One hundred and fifty years of history of the Morse taper: From Stephen A. Morse in 1864 to complications related to modularity in hip arthroplasty. Int. Orthop. 2013, 37, 2081–2088. [Google Scholar] [CrossRef] [PubMed]
- Mueller, U.; Braun, S.; Schroeder, S.; Sonntag, R.; Kretzer, J.P. Same Same but Different? 12/14 Stem and Head Tapers in Total Hip Arthroplasty. J. Arthroplast. 2017, 32, 3191–3199. [Google Scholar] [CrossRef] [PubMed]
- Virtanen, S.; Milosev, I.; Gomez-Barrena, E.; Trebse, R.; Salo, J.; Konttinen, Y.T. Special modes of corrosion under physiological and simulated physiological conditions. Acta Biomater. 2008, 4, 468–476. [Google Scholar] [CrossRef]
- Bermudez Castefieda, A. Degradation of Modular Hip Joint Implants, a Corrosion and Tribocorrosion Approach. Ph.D. Thesis, Ecole Polytechnique de Lausanne, Lausanne, Switzerland, 2018. [Google Scholar]
- Panagiotidou, A.; Cobb, T.; Meswania, J.; Skinner, J.; Hart, A.; Haddad, F.; Blunn, G. Effect of impact assembly on the interface deformation and fretting corrosion of modular hip tapers: An in vitro study. J. Orthop. Res. Off. Publ. Orthop. Res. Soc. 2018, 36, 405–416. [Google Scholar] [CrossRef]
- Mali, S.A.; Gilbert, J.L. Correlating Fretting Corrosion and Micromotions in Modular Tapers: Test Method Development and Assessment. In Modularity and Tapers in Total Joint Replacement Devices; Greenwald, A., Kurtz, S., Lemons, J., Mihalko, W., Eds.; ASTM International: West Conshohocken, PA, USA, 2015; pp. 259–282. [Google Scholar] [CrossRef]
- Fessler, H.; Fricker, D.C. Friction in femoral prosthesis and photoelastic model cone taper joints. Proc. Inst. Mech. Eng. H 1989, 203, 1–14. [Google Scholar] [CrossRef]
- Fessler, H.; Fricker, D.C. A study of stresses in alumina universal heads of femoral prostheses. Proc. Inst. Mech. Eng. H 1989, 203, 15–34. [Google Scholar] [CrossRef]
- MacLeod, A.R.; Sullivan, N.P.; Whitehouse, M.R.; Gill, H.S. Large-diameter total hip arthroplasty modular heads require greater assembly forces for initial stability. Bone Jt. Res. 2016, 5, 338–346. [Google Scholar] [CrossRef] [PubMed]
- Krull, A.; Morlock, M.M.; Bishop, N.E. The Influence of Contamination and Cleaning on the Strength of Modular Head Taper Fixation in Total Hip Arthroplasty. J. Arthroplast. 2017, 32, 3200–3205. [Google Scholar] [CrossRef] [PubMed]
- Pennock, A.T.; Schmidt, A.H.; Bourgeault, C.A. Morse-type tapers: Factors that may influence taper strength during total hip arthroplasty. J. Arthroplast. 2002, 17, 773–778. [Google Scholar] [CrossRef]
- Nassutt, R.; Mollenhauer, I.; Klingbeil, K.; Henning, O.; Grundei, H. Relevance of the insertion force for the taper lock reliability of a hip stem and a ceramic femoral head. Biomed. Tech. (Berl) 2006, 51, 103–109. [Google Scholar] [CrossRef] [PubMed]
- Jauch-Matt, S.Y.; Miles, A.W.; Gill, H.S. Effect of trunnion roughness and length on the modular taper junction strength under typical intraoperative assembly forces. Med. Eng. Phys. 2017, 39, 94–101. [Google Scholar] [CrossRef] [PubMed]
- Ramoutar, D.N.; Crosnier, E.A.; Shivji, F.; Miles, A.W.; Gill, H.S. Assessment of Head Displacement and Disassembly Force with Increasing Assembly Load at the Head/Trunnion Junction of a Total Hip Arthroplasty Prosthesis. J. Arthroplast. 2017, 32, 1675–1678. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ouellette, E.S.; Shenoy, A.A.; Gilbert, J.L. The seating mechanics of head-neck modular tapers in vitro: Load-displacement measurements, moisture, and rate effects. J. Orthop. Res. 2018, 36, 1164–1172. [Google Scholar] [CrossRef]
- Scholl, L.; Schmidig, G.; Faizan, A.; TenHuisen, K.; Nevelos, J. Evaluation of surgical impaction technique and how it affects locking strength of the head-stem taper junction. Proc. Inst. Mech. Eng. H 2016, 230, 661–667. [Google Scholar] [CrossRef]
- Pierre, D.; Swaminathan, V.; Scholl, L.Y.; TenHuisen, K.; Gilbert, J.L. Effects of Seating Load Magnitude on Incremental Cyclic Fretting Corrosion in 5 degrees 40′ Mixed Alloy Modular Taper Junctions. J. Arthroplast. 2018, 33, 1953–1961. [Google Scholar] [CrossRef]
- Pierre, D.; Swaminathan, V.; Scholl, L.; TenHuisen, K.; Gilbert, J.L. Effects of seating load magnitude and load orientation on seating mechanics in 5 degrees 40′ mixed-alloy modular taper junctions. J. Biomech. 2019, 82, 251–258. [Google Scholar] [CrossRef]
- Bitter, T.; Khan, I.; Marriott, T.; Schreurs, B.W.; Verdonschot, N.; Janssen, D. Experimental Measurement of the Static Coefficient of Friction at the Ti-Ti Taper Connection in Total Hip Arthroplasty. J. Biomech. Eng. 2016, 138, 4032446. [Google Scholar] [CrossRef] [PubMed]
- English, R.; Ashkanfar, A.; Rothwell, G. The effect of different assembly loads on taper junction fretting wear in total hip replacements. Tribol. Int. 2016, 95, 199–210. [Google Scholar] [CrossRef]
- Swaminathan, V.; Gilbert, J.L. Fretting corrosion of CoCrMo and Ti6Al4V interfaces. Biomaterials 2012, 33, 5487–5503. [Google Scholar] [CrossRef] [PubMed]
- Cartner, J.; Aldinger, P.; Li, C.; Collins, D. Characterization of Femoral Head Taper Corrosion Features Using a 22-Year Retrieval Database. Hss J. 2017, 13, 35–41. [Google Scholar] [CrossRef] [PubMed]
- Langton, D.J.; Sidaginamale, R.; Lord, J.K.; Nargol, A.V.; Joyce, T.J. Taper junction failure in large-diameter metal-on-metal bearings. Bone Jt. Res. 2012, 1, 56–63. [Google Scholar] [CrossRef]
- Panagiotidou, A.; Meswania, J.; Hua, J.; Muirhead-Allwood, S.; Hart, A.; Blunn, G. Enhanced wear and corrosion in modular tapers in total hip replacement is associated with the contact area and surface topography. J. Orthop. Res. 2013, 31, 2032–2039. [Google Scholar] [CrossRef]
- Pourzal, R.; Hall, D.J.; Ha, N.Q.; Urban, R.M.; Levine, B.R.; Jacobs, J.J.; Lundberg, H.J. Does Surface Topography Play a Role in Taper Damage in Head-neck Modular Junctions? Clin. Orthop. Relat. Res. 2016, 474, 2232–2242. [Google Scholar] [CrossRef]
- Arnholt, C.M.; MacDonald, D.W.; Underwood, R.J.; Guyer, E.P.; Rimnac, C.M.; Kurtz, S.M.; Implant Research Center Writing, C.; Mont, M.A.; Klein, G.R.; Lee, G.C.; et al. Do Stem Taper Microgrooves Influence Taper Corrosion in Total Hip Arthroplasty? A Matched Cohort Retrieval Study. J. Arthroplast. 2017, 32, 1363–1373. [Google Scholar] [CrossRef]
- Dyrkacz, R.M.; Brandt, J.M.; Ojo, O.A.; Turgeon, T.R.; Wyss, U.P. The influence of head size on corrosion and fretting behaviour at the head-neck interface of artificial hip joints. J. Arthroplast. 2013, 28, 1036–1040. [Google Scholar] [CrossRef]
- Triantafyllopoulos, G.K.; Elpers, M.E.; Burket, J.C.; Esposito, C.I.; Padgett, D.E.; Wright, T.M. Otto Aufranc Award: Large Heads Do Not Increase Damage at the Head-neck Taper of Metal-on-polyethylene Total Hip Arthroplasties. Clin. Orthop. Relat. Res. 2016, 474, 330–338. [Google Scholar] [CrossRef]
- Damm, P.; Dymke, J.; Ackermann, R.; Bender, A.; Graichen, F.; Halder, A.; Beier, A.; Bergmann, G. Friction in total hip joint prosthesis measured in vivo during walking. PLoS ONE 2013, 8, e78373. [Google Scholar] [CrossRef] [PubMed]
- Kleinschnittger, P. Einfluss der Kontaktflächen auf die Höhe der Relativbewegung zwischen Prothesenkonus und -kopf. Bachelor’s Thesis, Technical University Hamburg - Harburg, Hamburg, Germany, November 2016. [Google Scholar]
- Haschke, H.; Konow, T.; Huber, G.; Morlock, M.M. Influence of flexural rigidity on micromotion at the head-stem taper interface of modular hip prostheses. Med. Eng. Phys. 2019, 68, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Nassif, N.A.; Nawabi, D.H.; Stoner, K.; Elpers, M.; Wright, T.; Padgett, D.E. Taper design affects failure of large-head metal-on-metal total hip replacements. Clin. Orthop. Relat. Res. 2014, 472, 564–571. [Google Scholar] [CrossRef]
- Guhrs, J.; Krull, A.; Witt, F.; Morlock, M.M. The influence of stem taper re-use upon the failure load of ceramic heads. Med. Eng. Phys. 2015, 37, 545–552. [Google Scholar] [CrossRef] [PubMed]
- Mueller, U.; Panzram, B.; Braun, S.; Sonntag, R.; Kretzer, J.P. Mixing of Head-Stem Components in Total Hip Arthroplasty. J. Arthroplast. 2018, 33, 945–951. [Google Scholar] [CrossRef]
- Higgs, G.B.; MacDonald, D.W.; Gilbert, J.L.; Rimnac, C.M.; Kurtz, S.M.; Implant Research Center Writing, C. Does Taper Size Have an Effect on Taper Damage in Retrieved Metal-on-Polyethylene Total Hip Devices? J. Arthroplast. 2016, 31, 277–281. [Google Scholar] [CrossRef]
- Bergmann, G.; Bender, A.; Dymke, J.; Duda, G.; Damm, P. Standardized Loads Acting in Hip Implants. PLoS ONE 2016, 11, e0155612. [Google Scholar] [CrossRef]
- Bergmann, G.; Graichen, F.; Rohlmann, A.; Bender, A.; Heinlein, B.; Duda, G.N.; Heller, M.O.; Morlock, M.M. Realistic loads for testing hip implants. Biomed. Mater. Eng. 2010, 20, 65–75. [Google Scholar] [CrossRef]
- Lidder, S.; Epstein, D.J.; Scott, G. A systematic review of short metaphyseal loading cementless stems in hip arthroplasty. Bone Jt. Res. 2019, 5. [Google Scholar] [CrossRef]
- Porter, D.A.; Urban, R.M.; Jacobs, J.J.; Gilbert, J.L.; Rodriguez, J.A.; Cooper, H.J. Modern trunnions are more flexible: A mechanical analysis of THA taper designs. Clin. Orthop. Relat. Res. 2014, 472, 3963–3970. [Google Scholar] [CrossRef] [PubMed]
- Heiney, J.P.; Battula, S.; Vrabec, G.A.; Parikh, A.; Blice, R.; Schoenfeld, A.J.; Njus, G.O. Impact magnitudes applied by surgeons and their importance when applying the femoral head onto the Morse taper for total hip arthroplasty. Arch. Orthop. Trauma Surg. 2009, 129, 793–796. [Google Scholar] [CrossRef]
- Weisse, B.; Affolter, C.; Stutz, A.; Terrasi, G.P.; Kobel, S.; Weber, W. Influence of contaminants in the stem-ball interface on the static fracture load of ceramic hip joint ball heads. Proc. Inst. Mech. Eng. H 2008, 222, 829–835. [Google Scholar] [CrossRef]
- Faizan, A.; Longaray, J.; Nevelos, J.E.; Westrich, G.H. Effects of corrosion and cleaning method on taper dimensions: An in vitro investigation. Hip Int. 2020, 30, 87–92. [Google Scholar] [CrossRef]
- Krull, A.; Morlock, M.M.; Bishop, N.E. Maximizing the fixation strength of modular components by impaction without tissue damage. Bone Jt. Res. 2018, 7, 196–204. [Google Scholar] [CrossRef]
- Scholl, L.; Pierre, D.; Rajaravivarma, R.; Lee, R.; Faizan, A.; Swaminathan, V.; TenHuisen, K.; Gilbert, J.L.; Nevelos, J. Effect of the support systems’ compliance on total hip modular taper seating stability. Proc. Inst. Mech. Eng. H 2018, 232, 862–870. [Google Scholar] [CrossRef]
- Danoff, J.R.; Longaray, J.; Rajaravivarma, R.; Gopalakrishnan, A.; Chen, A.F.; Hozack, W.J. Impaction Force Influences Taper-Trunnion Stability in Total Hip Arthroplasty. J. Arthroplast. 2018, 33, S270–S274. [Google Scholar] [CrossRef]
- Frisch, N.B.; Lynch, J.R.; Banglmaier, R.F.; Silverton, C.D. The stability of dual-taper modular hip implants: a biomechanical analysis examining the effect of impact location on component stability. Arthroplast. Today 2017, 3, 119–124. [Google Scholar] [CrossRef]
- Noble, P.; Foley, E.; Simpson, J.; Gold, J.; Choi, J.; Ismaily, S.; Mathis, K.; Incavo, S. Inter-surgeon variability in the assembly of modular head-neck tapers in THA via the posterior approach. Proc. Orthop. Proc. 2017, 99B, 59. [Google Scholar]
- Svensson, O.; Mathiesen, E.B.; Reinholt, F.P.; Blomgren, G. Formation of a fulminant soft-tissue pseudotumor after uncemented hip arthroplasty. A case report. J. Bone Jt. Surg. Am. 1988, 70, 1238–1242. [Google Scholar] [CrossRef]
- Weiser, M.C.; Lavernia, C.J. Trunnionosis in Total Hip Arthroplasty. J. Bone Jt. Surg. Am. 2017, 99, 1489–1501. [Google Scholar] [CrossRef]
- Chana, R.; Esposito, C.; Campbell, P.A.; Walter, W.K.; Walter, W.L. Mixing and matching causing taper wear: Corrosion associated with pseudotumour formation. J. Bone Jt. Surg. Br. 2012, 94, 281–286. [Google Scholar] [CrossRef]
- Klug, A.; Gramlich, Y.; Hoffmann, R.; Pfeil, J.; Drees, P.; Kutzner, K.P. Trends in Total Hip Arthroplasty in Germany from 2007 to 2016: What Has Changed and Where Are We Now? Z Orthop. Unf. 2019. [Google Scholar] [CrossRef]
- Sariali, E.; Lazennec, J.Y.; Khiami, F.; Catonné, Y. Mathematical evaluation of jumping distance in total hip arthroplasty: Influence of abduction angle, femoral head offset, and head diameter. Acta Orthop. 2009, 80, 277–282. [Google Scholar] [CrossRef]
- Zijlstra, W.P.; De Hartog, B.; Van Steenbergen, L.N.; Scheurs, B.W.; Nelissen, R. Effect of femoral head size and surgical approach on risk of revision for dislocation after total hip arthroplasty. Acta Orthop. 2017, 88, 395–401. [Google Scholar] [CrossRef]
- Jameson, S.S.; Lees, D.; James, P.; Serrano-Pedraza, I.; Partington, P.F.; Muller, S.D.; Meek, R.M.; Reed, M.R. Lower rates of dislocation with increased femoral head size after primary total hip replacement: A five-year analysis of NHS patients in England. J. Bone Jt. Surg. Br. 2011, 93, 876–880. [Google Scholar] [CrossRef]
- Hanna, S.A.; Somerville, L.; McCalden, R.W.; Naudie, D.D.; MacDonald, S.J. Highly cross-linked polyethylene decreases the rate of revision of total hip arthroplasty compared with conventional polyethylene at 13 years’ follow-up. Bone Jt. J. 2016, 98-B, 28–32. [Google Scholar] [CrossRef]
- Elke, R.; Rieker, C.B. Estimating the osteolysis-free life of a total hip prosthesis depending on the linear wear rate and head size. Proc. Inst. Mech. Eng. H 2018, 232, 753–758. [Google Scholar] [CrossRef]
- Hruby, A.; Hu, F.B. The Epidemiology of Obesity: A Big Picture. Pharmacoeconomics 2015, 33, 673–689. [Google Scholar] [CrossRef]
- Bijukumar, D.R.; Salunkhe, S.; Zheng, G.; Barba, M.; Hall, D.J.; Pourzal, R.; Mathew, M.T. Wear particles induce a new macrophage phenotype with the potential to accelerate material corrosion within total hip replacement interfaces. Acta Biomater. 2020, 101, 586–597. [Google Scholar] [CrossRef]
- Hall, D.J.; Pourzal, R.; Lundberg, H.J.; Mathew, M.T.; Jacobs, J.J.; Urban, R.M. Mechanical, chemical and biological damage modes within head-neck tapers of CoCrMo and Ti6Al4V contemporary hip replacements. J. Biomed. Mater. Res. B Appl. Biomater. 2018, 106, 1672–1685. [Google Scholar] [CrossRef]
- Malik, M.H.; Jury, F.; Bayat, A.; Ollier, W.E.; Kay, P.R. Genetic susceptibility to total hip arthroplasty failure: a preliminary study on the influence of matrix metalloproteinase 1, interleukin 6 polymorphisms and vitamin D receptor. Ann. Rheum. Dis. 2007, 66, 1116–1120. [Google Scholar] [CrossRef]
- Kilb, B.K.J.; Kurmis, A.P.; Parry, M.; Sherwood, K.; Keown, P.; Masri, B.A.; Duncan, C.P.; Garbuz, D.S. Frank Stinchfield Award: Identification of the At-risk Genotype for Development of Pseudotumors Around Metal-on-metal THAs. Clin. Orthop. Relat. Res. 2018, 476, 230–241. [Google Scholar] [CrossRef]
- Goyal, N.; Ho, H.; Fricka, K.B.; Engh, C.A., Jr. Do you have to remove a corroded femoral stem? J. Arthroplast. 2014, 29, 139–142. [Google Scholar] [CrossRef]
- Whitehouse, M.R.; Endo, M.; Zachara, S.; Nielsen, T.O.; Greidanus, N.V.; Masri, B.A.; Garbuz, D.S.; Duncan, C.P. Adverse local tissue reactions in metal-on-polyethylene total hip arthroplasty due to trunnion corrosion: The risk of misdiagnosis. Bone Jt. J. 2015, 97-B, 1024–1030. [Google Scholar] [CrossRef]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rieker, C.B.; Wahl, P. What the Surgeon Can Do to Reduce the Risk of Trunnionosis in Hip Arthroplasty: Recommendations from the Literature. Materials 2020, 13, 1950. https://doi.org/10.3390/ma13081950
Rieker CB, Wahl P. What the Surgeon Can Do to Reduce the Risk of Trunnionosis in Hip Arthroplasty: Recommendations from the Literature. Materials. 2020; 13(8):1950. https://doi.org/10.3390/ma13081950
Chicago/Turabian StyleRieker, Claude B., and Peter Wahl. 2020. "What the Surgeon Can Do to Reduce the Risk of Trunnionosis in Hip Arthroplasty: Recommendations from the Literature" Materials 13, no. 8: 1950. https://doi.org/10.3390/ma13081950
APA StyleRieker, C. B., & Wahl, P. (2020). What the Surgeon Can Do to Reduce the Risk of Trunnionosis in Hip Arthroplasty: Recommendations from the Literature. Materials, 13(8), 1950. https://doi.org/10.3390/ma13081950




