Nanoparticles and Nanostructured Surface Fabrication for Innovative Cranial and Maxillofacial Surgery
Abstract
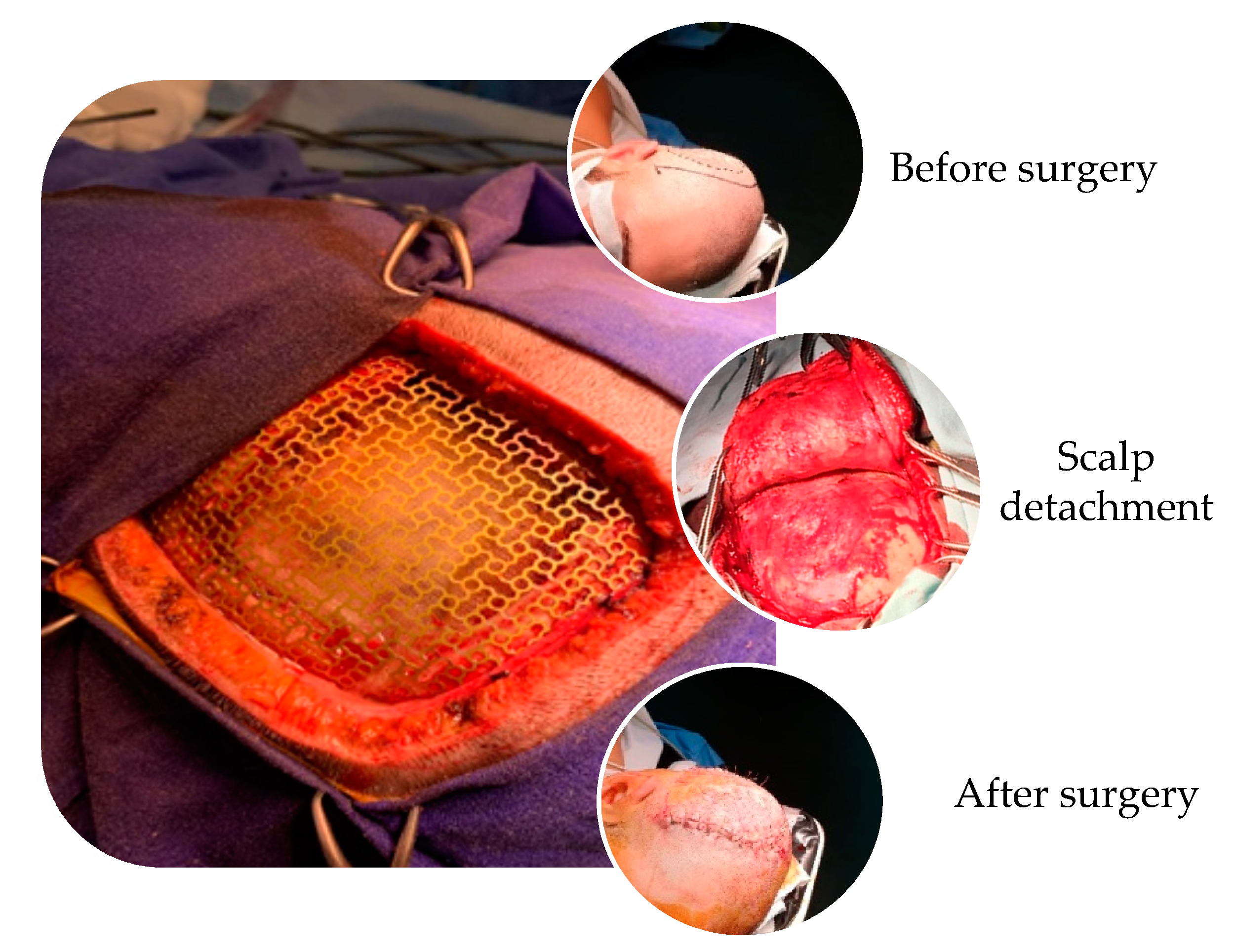
1. Introduction into Cranioplasty and Craniofacial Reconstruction Using Titanium Meshes and Plates for Major Cranial Defects
- perfect fit into the cranial defect in order to get fast and complete closure
- radiolucent
- resistance to infections
- heat non-deformable
- strengths comparable to that of the surrounding bone
- biomechanical resistance
- easy to manipulate and contour
- inexpensive
- fast application
2. The Importance of Nano-Structured Surface on Titanium Implants
2.1. Mechanical, Physical and Chemical a Methods for Creating Nano-Structured Titanium Surfaces
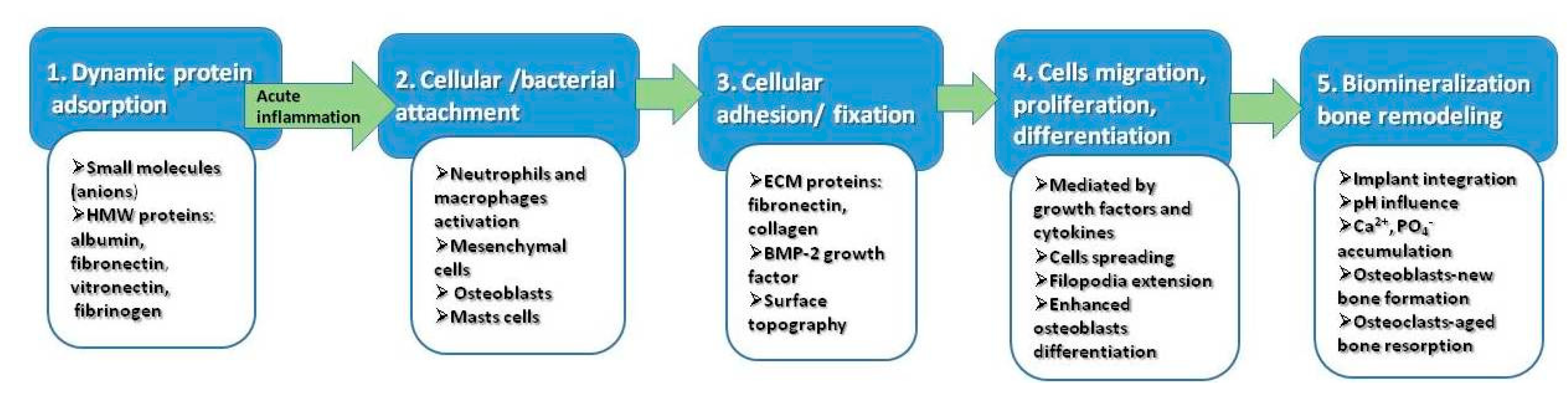
2.2. Improved Biological Properties of Nano-Structured Surfaces
3. Types of Nanoparticles Used for Surface Modification of Titanium Implants
4. Patented Solutions to Improve Osteointegration of Cranial Implants
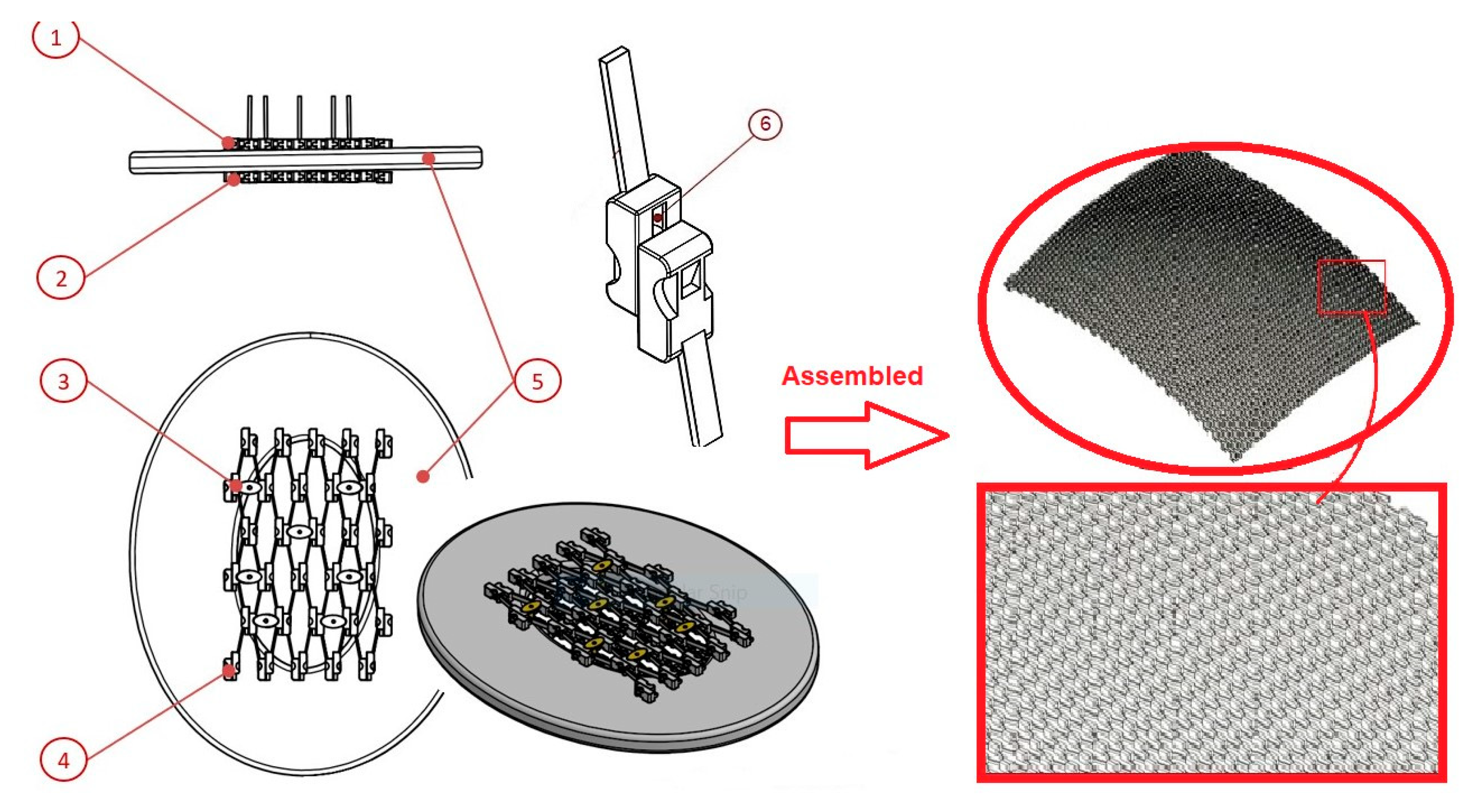
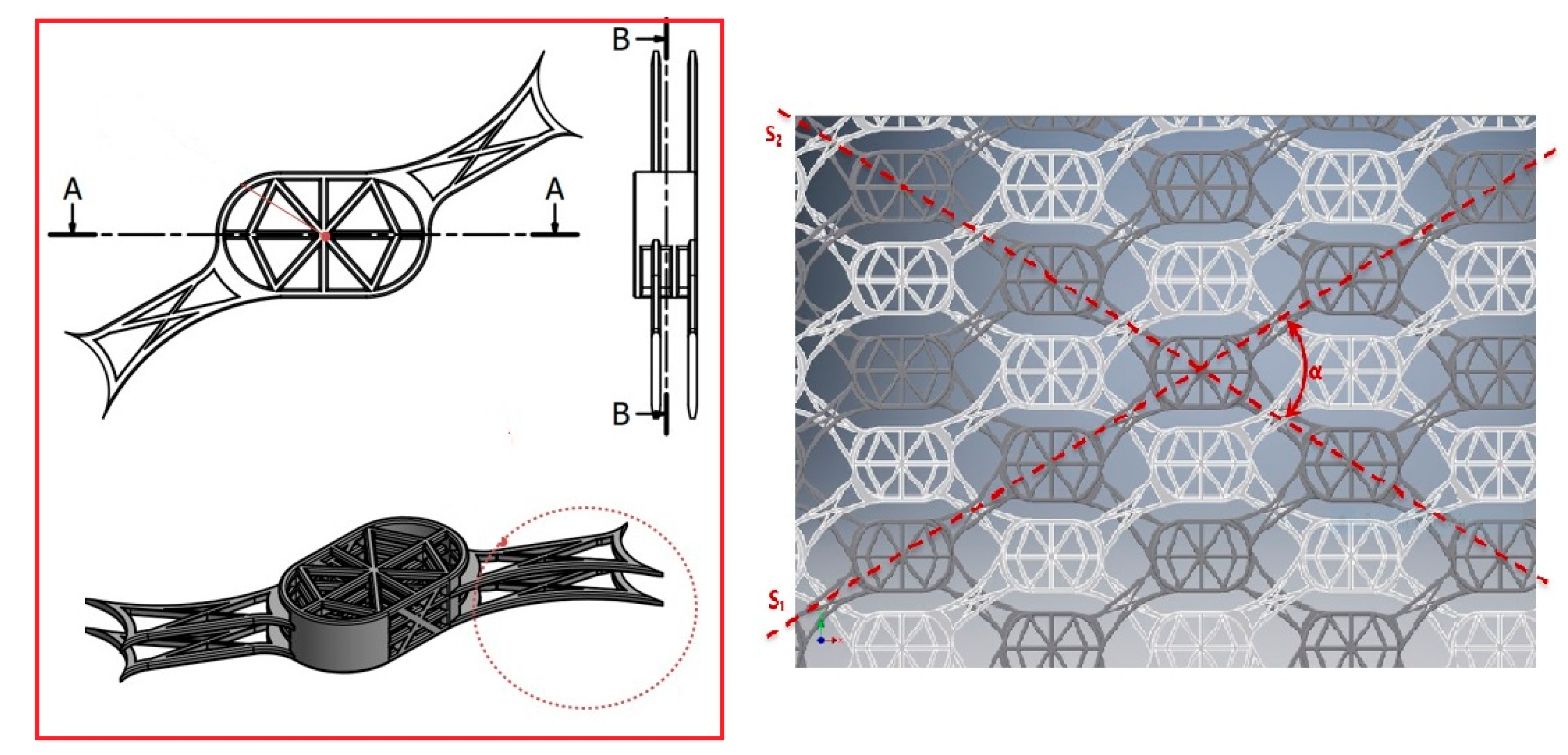
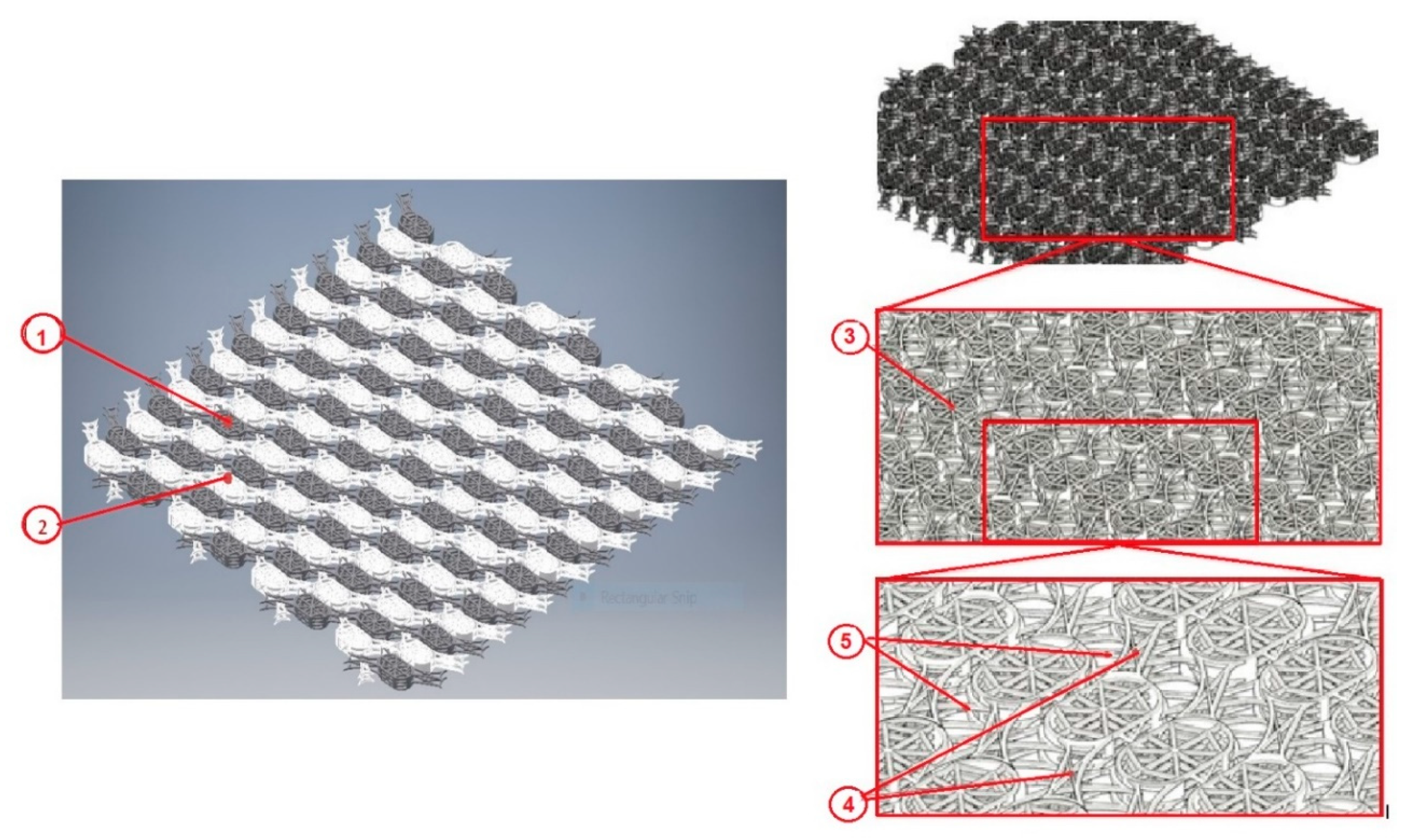
4.1. Cranial Endoprosthesis with Sliding System
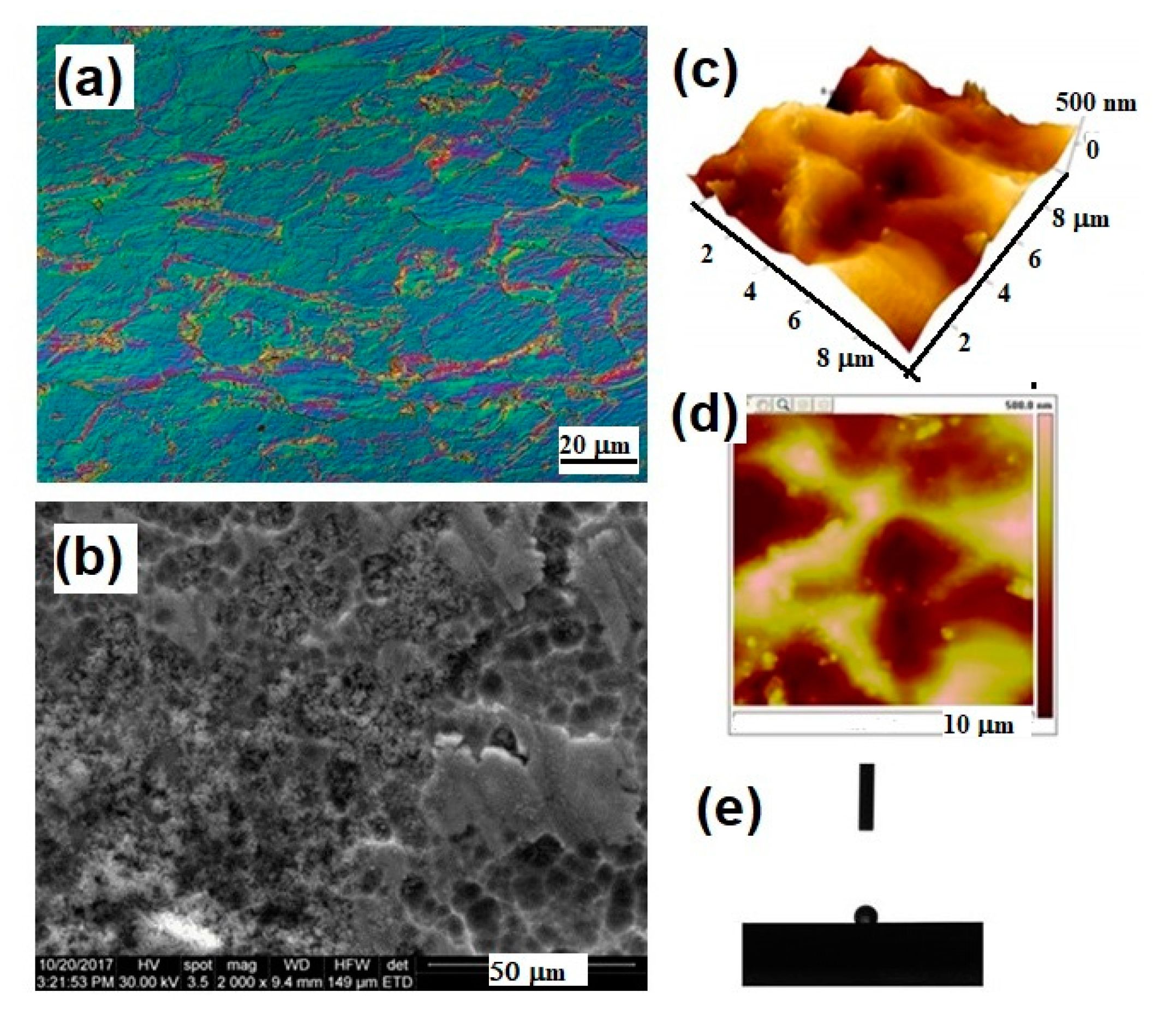
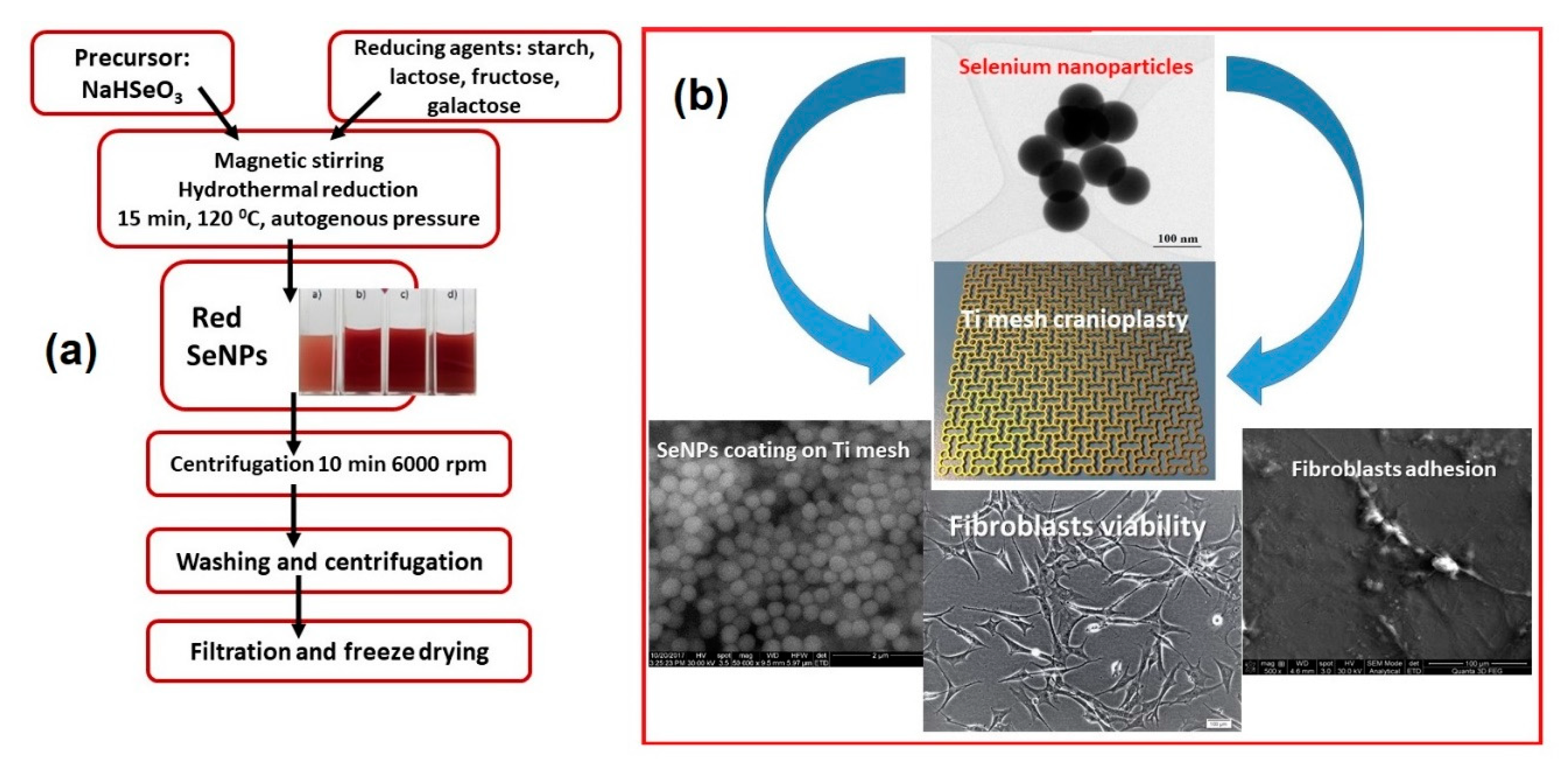
4.2. Titanium Mesh with Novel Geometry and Functional Nano-Coating Based on SeNPs
5. Conclusions and Future Perspective
6. Patent
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Sanan, A.; Haines, S.J. Repairing holes in the head: A history of cranioplasty. Neurosurgery 1997, 40, 588–603. [Google Scholar] [PubMed]
- Bonfield, C.M.; Kumar, A.R.; Gerszten, P.C. The history of military cranioplasty. Neurosurg. Focus 2014, 36, 18. [Google Scholar] [CrossRef] [PubMed]
- Prolo, D.J.; Oklund, S.A. Composite autogeneic human cranioplasty: Frozen skull supplemented with fresh iliac corticocancellous bone. Neurosurgery 1984, 15, 846–851. [Google Scholar]
- Kwarcinski, J.; Boughton, P.; Ruys, A.; Doolan, A.; Van Gelder, J. Cranioplasty and Craniofacial Reconstruction: A Review of Implant Material, Manufacturing Method and Infection Risk. Appl. Sci 2017, 7, 276. [Google Scholar] [CrossRef]
- Grant, G.A.; Jolley, M.; Ellenbogen, R.G.; Roberts, T.S.; Gruss, J.R.; Loeser, J.D. Failure of autologous bone-assisted cranioplasty following decompressive craniectomy in children and adolescents. J. Neurosurg. 2004, 100, 163–168. [Google Scholar] [CrossRef]
- Sheng, H.S.; Shen, F.; Lin, J.; Lin, F.C.; Yin, B.; Zhang, N. Titanium mesh implants exposure after cranioplasty in two children: Involvement of osteogenesis? Chin. Neurosurg. J. 2017, 3, 1–4. [Google Scholar] [CrossRef]
- Zins, J.E.; Langevin, C.J.; Nasir, S. Controversies in skull reconstruction. J. Craniofac. Surg. 2010, 21, 1755–1760. [Google Scholar] [CrossRef]
- Aydin, S.; Kucukyuruk, B.; Abuzayed, B.; Aydin, S.; Sanus, G.Z. Cranioplasty: Review of materials and techniques. J. Neurosci. Rural. Pract. 2011, 2, 162–167. [Google Scholar] [CrossRef] [PubMed]
- Cavalu, S.; Banica, F.; Simon, V.; Akin, I.; Goller, G. Surface Modification of Alumina/Zirconia Ceramics upon Different Fluoride-Based Treatments. Int. J. Appl. Cer. Technol. 2014, 11, 402–411. [Google Scholar] [CrossRef]
- Khader, B.A.; Towler, M.R. Materials and techniques used in cranioplasty fixation: A review. Mater. Sci. Eng. C Mater. Biol. Appl. 2016, 66, 315–322. [Google Scholar] [CrossRef] [PubMed]
- Marchac, D.; Greensmith, A. Long-term experience with methylmethacrylate cranioplasty in craniofacial surgery. J. Plast. Reconstr. Aesthetic Surg. 2008, 61, 744–752. [Google Scholar] [CrossRef] [PubMed]
- Rosinski, C.L.; Chaker, A.N.; Zakrzewski, J.; Geever, B.; Patel, S.; Chiu, R.; Rosenberg, D.; Parola, R.; Shah, K.; Behbahani, M.; et al. Autologous Bone Cranioplasty: A Retrospective Comparative Analysis of Frozen and Subcutaneous Bone Flap Storage Methods. World Neurosurg. 2019, 131, e312–e320. [Google Scholar] [CrossRef] [PubMed]
- Malis, L.I. Titanium Mesh and Acrylic Cranioplasty. Neurosurgersy 1989, 25, 351–355. [Google Scholar] [CrossRef]
- Brånemark, R.; I Brånemark, P.; Rydevik, B.; Myers, R.R. Osseointegration in skeletal reconstruction and rehabilitation: A review. J. Rehabil. Res. Dev. 2001, 38, 175–181. [Google Scholar]
- Chiriac, A.; Stan, G.E.; Iliescu, B.; Poeata, I. The influence of host bone substitute in titanium mesh cranioplasty. Digest J. Nanomat. Biostruct. 2013, 8, 729–735. [Google Scholar]
- Luo, J.; Liu, B.; Xie, Z.; Ding, S.; Zhuang, Z.; Lin, L.; Guo, Y.; Chen, H.; Yu, X. Comparison of manually shaped and computer-shaped titanium mesh for repairing large frontotemporoparietal skull defects after traumatic brain injury. Neurosurg. Focus 2012, 33, E13. [Google Scholar] [CrossRef]
- Mukherjee, S.; Thakur, B.; Haq, I.; Hettige, S.; Martin, A.J. Complications of titanium cranioplasty—A retrospective analysis of 174 patients. Acta Neurochir. 2014, 156, 989–998. [Google Scholar] [CrossRef]
- Hill, C.S.; Luoma, A.M.V.; Wilson, S.R.; Kitchen, N. Titanium cranioplasty and the prediction of complications. Br. J. Neurosurg. 2012, 26, 832–837. [Google Scholar] [CrossRef]
- Kim, J.-K.; Lee, S.-B.; Yang, S.-Y. Cranioplasty Using Autologous Bone versus Porous Polyethylene versus Custom-Made Titanium Mesh: A Retrospective Review of 108 Patients. J. Korean Neurosurg. Soc. 2018, 61, 737–746. [Google Scholar] [CrossRef]
- Verret, D.; Ducic, Y.; Oxford, L.; Smith, J. Hydroxyapatite Cement in Craniofacial Reconstruction. Otolaryngol. Neck Surg. 2005, 133, 897–899. [Google Scholar] [CrossRef]
- Sunderland, I.R.; Edwards, G.; Mainprize, J. A technique for intraoperative creation of patient-specific titanium mesh implants. Plast Surg. 2015, 23, 95–99. [Google Scholar] [CrossRef]
- Rosinski, C.L.; Patel, S.; Chaker, A.N.; Behbahani, M.; I Mehta, A. In Reply: A Retrospective Comparative Analysis of Titanium Mesh and Custom Implants for Cranioplasty. Neurosurgery 2020, 87, E268. [Google Scholar] [CrossRef] [PubMed]
- Mazaheri, M.; Eslahi, N.; Ordikhani, F.; Tanjid, E.; Simchi, A. Nanomedicine applications in orthopedic medicine: State of the art. Int. J. Nanomed. 2015, 10, 6039–6054. [Google Scholar]
- Jäger, M.; Jennissen, H.P.; Dittrich, F.; Fischer, A.; Köhling, H.L. Antimicrobial and Osseointegration Properties of Nanostructured Titanium Orthopaedic Implants. Materials 2017, 10, 1302. [Google Scholar] [CrossRef] [PubMed]
- Durmus, N.G.; Webster, T.J. Nanostructured titanium: The ideal material for improving orthopedic implant efficacy? Nanomedicine 2012, 7, 791–793. [Google Scholar] [CrossRef]
- Brunette, D.M.; Tengvall, P.; Textor, M.; Thomsen, P. Titanium in Medicine: Material Science, Surface Science, Engineering, Biological Responses and Medical Applications; Springer: Berlin/Heidelberg, Germany, 2001. [Google Scholar]
- Goldman, M.; Juodzbalys, G.; Vilkinis, V. Titanium Surfaces with Nanostructures Influence on Osteoblasts Proliferation: A Systematic Review. J. Oral Maxillofac. Res. 2014, 5, e1. [Google Scholar] [CrossRef]
- Lausmaa, J.; Kasemo, B.; Mattsson, H. Surface spectroscopic characterization of titanium implant materials. Appl. Surf. Sci. 1990, 44, 133–146. [Google Scholar] [CrossRef]
- Wang, Y.; Yu, Z.; Li, K.; Hu, J. Effects of surface properties of titanium alloys modified by grinding, sandblasting and acidizing and nanosecond laser on cell proliferation and cytoskeleton. Appl. Surf. Sci. 2020, 501, 144279. [Google Scholar] [CrossRef]
- Liu, X.; Chu, P.K.; Ding, C. Surface modification of titanium, titanium alloys, and related materials for biomedical applications. Mater. Sci. Eng. R Rep. 2004, 47, 49–121. [Google Scholar] [CrossRef]
- Kulkarni, M.; Mazare, A.; Schmuki, P.; Iglič, A. Biomaterial surface modification of titanium and titanium alloys for medical applications. In Nanomedicine; Chapter 5: Biomaterial Surface Modification of Titanium and Titanium Alloys for Medical Applications; Alexander, S., de Mel, A., Deepak, M.K., Eds.; One Central Press: Altrincham, UK, 2014. [Google Scholar]
- Kim, K.-H.; Narayanan, R.; Rautray, R.T. Surface Modification of Titanium for Biomaterial Applications. Nova Publ. Sci. Inc. 2010, 42, 201–228. [Google Scholar]
- Unal, O.; Karaoglanli, A.C.; Varol, R.; Kobayashi, A. Microstructure evolution and mechanical behavior of severe shot peened commercially pure titanium. Vacuum 2014, 110, 202–206. [Google Scholar] [CrossRef]
- Zhang, L.-C.; Chen, L.-Y.; Wang, L. Surface Modification of Titanium and Titanium Alloys: Technologies, Developments and Future Interests. Adv. Eng. Mater. 2020, 22, 1901258. [Google Scholar] [CrossRef]
- Wang, L.; Xie, L.; Shen, P.; Fan, Q.; Wang, W.; Wang, K.; Lu, W.; Hua, L.; Zhang, L.-C. Surface microstructure and mechanical properties of Ti-6Al-4V/Ag nanocomposite prepared by FSP. Mater. Charact. 2019, 153, 175–183. [Google Scholar] [CrossRef]
- Bagno, A.; Di Bello, C. Surface treatments and roughness properties of Ti-based biomaterials. J. Mater. Sci. Mater. Med. 2004, 15, 935–949. [Google Scholar] [CrossRef]
- Jelliti, S.; Richard, C.; Retraint, D.; Roland, T.; Chemkhi, M.; Demangel, C. Effect of surface nanocrystallization on the corrosion behavior of Ti–6Al–4V titanium alloy. Surf. Coat. Technol. 2013, 224, 82–87. [Google Scholar] [CrossRef]
- Guo, Z.; Jiang, N.; Chen, C.; Zhu, S.; Zhang, L.; Li, Y. Surface bioactivation through the nanostructured layer on titanium modified by facile HPT treatment. Sci. Rep. 2017, 7, 1–11. [Google Scholar] [CrossRef]
- Zhou, H.; Li, F.; Wang, J.; Sun, B.-D. Microstructure analyses and thermophysical properties of nanostructured thermal barrier coatings. J. Coat. Technol. Res. 2008, 6, 383–390. [Google Scholar] [CrossRef]
- Chen, H.; Zeng, Y.; Ding, C. Microstructural characterization of plasma-sprayed nanostructured zirconia powders and coatings. J. Eur. Ceram. Soc. 2003, 23, 491–497. [Google Scholar] [CrossRef]
- Yılmaz, Ş. An evaluation of plasma-sprayed coatings based on Al2O3 and Al2O3–13 wt.% TiO2 with bond coat on pure titanium substrate. Ceram. Int. 2009, 35, 2017–2022. [Google Scholar] [CrossRef]
- LeClair, P.; Berera, G.P.; Moodera, J.S. Titanium nitride thin films obtained by a modified physical vapor deposition proces. Thin Solid Film 2000, 1, 376–379. [Google Scholar]
- Jung, M.J.; Nam, K.H.; Shaginyan, L.R.; Han, J.G. Deposition of Ti thin film using the magnetron sputtering method. Thin Solid Film 2003, 435, 145–149. [Google Scholar] [CrossRef]
- Wang, Z.G.; Zu, X.; Xiang, X.; Zhu, S.; Wang, L.M. Surface modification of Ti-4Al-2V alloy by nitrogen implantation. J. Mater. Sci. 2006, 41, 3363–3367. [Google Scholar] [CrossRef]
- Rautray, T.R.; Narayanan, R.; Kwon, T.-Y.; Kim, K.-H. Surface modification of titanium and titanium alloys by ion implantation. J. Biomed. Mater. Res. Part B Appl. Biomater. 2010, 93, 581–591. [Google Scholar] [CrossRef] [PubMed]
- Shibata, Y.; Miyazaki, T. Anode glow discharge plasma treatment enhances calcium phosphate adsorption onto titanium plates. J. Dent. Res. 2002, 81, 841–844. [Google Scholar] [CrossRef]
- Aronsson, B.-O.; Lausmaa, J.; Kasemo, B. Glow discharge plasma treatment for surface cleaning and modification of metallic biomaterials. Biomed. Mater. Res. 1997, 35, 49. [Google Scholar] [CrossRef]
- Aziz, G.; Ghobeira, R.; Morent, R.; De Geyter, N. Plasma Polymerization for Tissue Engineering Purposes. In Recent Research in Polymerization; Cankaya, N., Ed.; IntechOpen: London, UK, 2017. [Google Scholar] [CrossRef]
- Lamolle, S.F.; Monjo, M.; Rubert, M.; Haugen, H.J.; Lyngstadaas, S.P.; Ellingsen, J.E. The effect of hydrofluoric acid treatment of titanium surface on nanostructural and chemical changes and the growth of MC3T3-E1 cells. Biomaterials 2009, 30, 736–742. [Google Scholar] [CrossRef]
- Wen, H.B.; Liu, Q.; De Wijn, J.R.; De Groot, K.; Cui, F.Z. Preparation of bioactive microporous titanium surface by a new two-step chemical treatment. J. Mater. Sci. Mater. Electron. 1998, 9, 121–128. [Google Scholar] [CrossRef]
- Lee, B.-H.; Kim, Y.D.; Shin, J.H.; Lee, K.H. Surface modification by alkali and heat treatments in titanium alloys. J. Biomed. Mater. Res. 2002, 61, 466–473. [Google Scholar] [CrossRef]
- Pan, J.; Thierry, D.; Leygraf, C. Hydrogen peroxide toward enhanced oxide growth on titanium in PBS solution: Blue coloration and clinical relevance. J. Biomed. Mater. Res. 1996, 30, 393. [Google Scholar] [CrossRef]
- Sul, Y.-T.; Johansson, C.B.; Kang, Y.; Jeon, D.-G.; Albrektsson, T. Bone Reactions to Oxidized Titanium Implants with Electrochemical Anion Sulphuric Acid and Phosphoric Acid Incorporation. Clin. Implant. Dent. Relat. Res. 2002, 4, 78–87. [Google Scholar] [CrossRef]
- Li, B.; Hao, J.; Min, Y.; Xin, S.; Guo, L.; He, F.; Liang, C.; Wang, H.; Li, H. Biological properties of nanostructured Ti incorporated with Ca, P and Ag by electrochemical method. Mater. Sci. Eng. C 2015, 51, 80–86. [Google Scholar] [CrossRef] [PubMed]
- Minagar, S.; Wang, J.; Berndt, C.C.; Ivanova, E.P.; Wen, C. Cell response of anodized nanotubes on titanium and titanium alloys—A review. J. Biomed. Mater. Res. Part A 2013, 101, 2726–2739. [Google Scholar] [CrossRef] [PubMed]
- Rats, D.; Vandenbulcke, L.; Herbin, R.; Benoit, R.; Erre, R.; Serin, V.; Sevely, J. Characterization of diamond films deposited on titanium and its alloys. Thin Solid Films 1995, 270, 177–183. [Google Scholar] [CrossRef]
- Baek, S.H.; Mihec, D.F.; Metson, J.B. The Deposition of Diamond Films by Combustion Assisted CVD on Ti and Ti-6Al-4V. Chem. Vap. Depos. 2002, 8, 29–34. [Google Scholar] [CrossRef]
- Brinker, C.; Scherer, G. Sol–Gel Science: The Physics and Chemistry of Sol–Gel Processing; American Press: San Diego, CA, USA, 1990. [Google Scholar]
- Piveteau, L.-D.; Gasser, B.; Schlapbach, L. Evaluating mechanical adhesion of sol–gel titanium dioxide coatings containing calcium phosphate for metal implant application. Biomaterials 2000, 21, 2193–2201. [Google Scholar] [CrossRef]
- Ao, H.; Xie, Y.; Tan, H.; Wu, X.; Liu, G.; Qin, A.; Zheng, X.; Tang, T. Improved hMSC functions on titanium coatings by type I collagen immobilization. J. Biomed. Mater. Res. Part A 2013, 102, 204–214. [Google Scholar] [CrossRef]
- Dettin, M.; Bagno, A.; Gambaretto, R.; Iucci, G.; Conconi, M.T.; Tuccitto, N.; Menti, A.M.; Grandi, C.; Di Bello, C.; Licciardello, A.; et al. Covalent surface modification of titanium oxide with different adhesive peptides: Surface characterization and osteoblast-like cell adhesion. J. Biomed. Mater. Res. Part A 2009, 90, 35–45. [Google Scholar] [CrossRef]
- Kanemura, Y.; Sakai, D.; Komasa, S.; Sekino, T.; Okazaki, J. In vitro behavior of surface-modified implants after chemical processing at room temperature. J. Osaka Dent. Univ. 2014, 48, 29–35. [Google Scholar]
- Karthega, M.; Nallaiyan, R. Hydrogen peroxide treatment on Ti–6Al–4V alloy: A promising surface modification technique for orthopaedic application. Appl. Surf. Sci. 2010, 256, 2176–2183. [Google Scholar] [CrossRef]
- Hampden-Smith, M.J.; Kodas, T.T. Chemical vapor deposition of metals: Part 2. Overview of selective CVD of Metals. Chem. Vap. Depos. 1995, 1, 39–48. [Google Scholar] [CrossRef]
- Frauchiger, V.; Schlottig, F.; Gasser, B.; Textor, M. Anodic plasma-chemical treatment of CP titanium surfaces for biomedical applications. Biomaterials 2004, 25, 593–606. [Google Scholar] [CrossRef]
- Indira, K.; Ningshen, S.; Mudali, K.; Rajendran, N. Effect of Anodization Temperature on the Surface Morphology of Anodized Titanium. In Thin Film and Nanomaterials; Jayakumar, S., Kannan, M.D., Balasundaraprabhu, R., Prassana, S., Eds.; Macmillan Publishers: New York, NY, USA, 2011. [Google Scholar]
- Gulati, K.; Santos, A.; Findlay, D.; Losic, D. Optimizing Anodization Conditions for the Growth of Titania Nanotubes on Curved Surfaces. J. Phys. Chem. C 2015, 119, 16033–16045. [Google Scholar] [CrossRef]
- Bauer, S.; Schmuki, P.; Von Der Mark, K.; Park, J. Engineering biocompatible implant surfaces: Part I: Materials and surfaces. Prog. Mater. Sci. 2013, 58, 261–326. [Google Scholar] [CrossRef]
- Mas-Moruna, C.E.M.; Montufar, E.; Mestres, G.; Aparicio, D.; Javier, G.F.; Ginebra., M. Biomaterials Surface Science; Wiley-VCH: Weinheim, Germany, 2013. [Google Scholar]
- Roy, P.; Berger, S.; Schmuki, P. TiO2 Nanotubes: Synthesis and Applications. Angew. Chem. Int. Ed. 2011, 50, 2904–2939. [Google Scholar] [CrossRef] [PubMed]
- Wang, G.; Wan, Y.; Liu, Z. Construction of Complex Structures Containing Micro-Pits and Nano-Pits on the Surface of Titanium for Cytocompatibility Improvement. Materials 2019, 12, 2820. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Chu, P.K.; Ding, C. Surface nano-functionalization of biomaterials. Mater. Sci. Eng. R Rep. 2010, 70, 275–302. [Google Scholar] [CrossRef]
- Beauvais, S.; Drevelle, O.; Jann, J.; Lauzon, M.A.; Foruzanmehr, M.; Grenier, G.; Roux, S.; Faucheux, N. Interactions between bone cells and biomaterials: An update. Front. Biosci. 2016, 8, 227–263. [Google Scholar]
- Williams, D.F. On the mechanisms of biocompatibility. Biomaterials 2008, 29, 2941–2953. [Google Scholar] [CrossRef]
- Schwarcz, H.P.; Abueidda, D.; Jasiuk, I. The Ultrastructure of Bone and Its Relevance to Mechanical Properties. Front. Phys. 2017. [Google Scholar] [CrossRef]
- Ratiu, C.; Brocks, M.; Costea, T.; Moldovan, L.; Cavalu, S. PRGF-Modified Collagen Membranes for Guided Bone Regeneration: Spectroscopic, Microscopic and Nano-Mechanical Investigations. Appl. Sci. 2019, 9, 1035. [Google Scholar] [CrossRef]
- Ormanci, O.; Akin, I.; Sahin, F.; Yucel, O.; Simon, V.; Cavalu, S.; Goller, G. Spark plasma sintered Al2O3-YSZ-TiO2 composites: Processing, characterization and in vivo evaluation. Mater. Sci. Eng. C-Mater. Biol. Appl. 2014, 40, 16–23. [Google Scholar] [CrossRef] [PubMed]
- Parnia, F.; Yazdani, J.; Javaherzadeh, V.; Dizaj, S.M. Overview of Nanoparticle Coating of Dental Implants for Enhanced Osseointegration and Antimicrobial Purposes. Pharm. Pharm. Sci. 2017, 20, 148–160. [Google Scholar] [CrossRef] [PubMed]
- Flemming, H.C.; Wingender, J.; Szewzyk, U.; Steinberg, P.; Rice, S.A.; Kjelleberg, S. Biofilms: An emergent form of bacterial life. Nat. Rev. Microbiol. 2016, 14, 563–575. [Google Scholar] [CrossRef] [PubMed]
- Radtke, A.; Topolski, A.; Jedrzejewski, T.; Kozak, W.; Sadowska, B.; Wieckowska-Szakiel, M.; Piszczek, P. Bioactivity Studies on Titania Coatings and the Estimation of Their Usefulness in the Modification of Implant Surfaces. Nanomaterials 2017, 7, 90. [Google Scholar] [CrossRef]
- Nathan, A.S.C.; Mohandoss, K.; Balasubramaniam, M.K. Comparative Evaluation of Antifungal Effect of Titanium, Zirconium and Aluminium Nanoparticles Coated Titanium Plates against C. albicans. J. Clin. Diagn. Res. 2016, 10, ZC56–ZC59. [Google Scholar]
- Shokuhfar, T.; Hamlekhan, A.; Chang, J.-Y.; Choi, C.K.; Sukotjo, C.; Friedrich, C. Biophysical evaluation of cells on nanotubular surfaces: The effects of atomic ordering and chemistry. Int. J. Nanomed. 2014, 9, 3737. [Google Scholar]
- Li, B.; Zhang, X.; Ma, J.; Zhou, L.; Li, H.; Liang, C.; Wang, H. Hydrophilicity of bioactive titanium surface with different structure, composition, crystal form and grain size. Mater. Lett. 2018, 182, 43–46. [Google Scholar] [CrossRef]
- Hu, H.; Zhang, W.; Qiao, Y.; Jiang, X.; Liu, X.; Ding, C. Antibacterial activity and increased bone marrow stem cell functions of Zn-incorporated TiO2 coatings on titanium. Acta Biomater. 2012, 8, 904–915. [Google Scholar] [CrossRef]
- Demirbaşa, Ç.; Aydaya, A. The influence of Nano-TiO2 and Nano-Al2O3 Particles in Silicate Based Electrolytes on Microstructure and Mechanical Properties of Micro Arc Coated Ti6Al4V Alloy. Mater. Res. 2018, 21, e20180092. [Google Scholar] [CrossRef]
- Mendonça, G.; Mendonça, D.B.; Simões, L.G.; Araújo, A.L.; Leite, E.R.; Duarte, W.R.; Cooper, L.F.; Aragão, F.J. Nanostructured alumina-coated implant surface: Effect on osteoblast-related gene expression and bone-to-implant contact in vivo. Int. J. Oral Maxillofac. Implants 2009, 24, 205–215. [Google Scholar]
- Lin, A.; Wang, C.J.; Kelly, J.; Gubbi, P.; Nishimura, I. The role of titanium implant surface modification with hydroxyapatite nanoparticles in progressive early bone-implant fixation in vivo. Int. J. Oral Maxillofac. Implants 2009, 24, 808–816. [Google Scholar] [PubMed]
- Kloss, F.R.; Singh, S.; Hächl, O.; Rentenberger, J.; Auberger, T.; Kraft, A.; Klima, G.; Mitterlechner, T.; Steinmüller-Nethl, D.; Lethaus, B. BMP-2 immobilized on nanocrystalline diamond–coated titanium screws; demonstration of osteoinductive properties in irradiated bone. Head Neck 2013, 35, 235–241. [Google Scholar] [CrossRef] [PubMed]
- Liao, J.; Zhu, Z.; Mo, A.; Li, L.; Zhang, J. Deposition of silver nanoparticles on titanium surface for antibacterial effect. Int. J. Nanomed. 2010, 5, 261–267. [Google Scholar]
- Memarzadeh, K.; Sharili, A.S.; Huang, J.; Rawlinson, S.C.; Allaker, R.P. Nanoparticulate zinc oxide as a coating material for orthopedic and dental implants. J. Biomed. Mat. Res. Part A 2015, 103, 981–989. [Google Scholar] [CrossRef] [PubMed]
- Zainali, K.; Danscher, G.; Jakobsen, T.; Baas, J.; Moller, P.; Bechtold, J.E.; Soballe, K. Assessment of modified gold surfaced titanium implants on skeletal fixation. J. Biomed. Mater. Res. A 2013, 101, 195–202. [Google Scholar] [CrossRef]
- Antoniac, V.I.; Cavalu, S.; Costoiu, M.C.; Doicin, C.V.; Doicin, I.E.; Mates, I.M.; Mohan, A.G.; Murzac, R.; Semenescu, A.; Saceleanu, V.; et al. Cranial implant with osteointegration structures and functional coatings. Patent RO132417B1, 30 October 2019. Available online: https://worldwide.espacenet.com/patent/search/family/061724843/publication/RO132417A0?q=pn%3DRO132417A0 (accessed on 16 October 2020).
- Cavalu, S.; Antoniac, I.V.; Fritea, L.; Mates, I.M.; Milea, C.; Laslo, V.; Vicas, S.; Mohan, A. Surface modifications of the titanium mesh for cranioplasty using selenium nanoparticles coating. J. Adhes. Sci. Technol. 2018, 22, 2509–2522. [Google Scholar] [CrossRef]
- Tran, P.; Webster, T.J. Enhanced osteoblast adhesion on nanostructured selenium compacts for anti-cancer orthopaedic applications. Int. J. Nanomed. 2008, 3, 391–396. [Google Scholar]
- Miller, D.; Webster, T.J. Anticancer orthopedic implants. In Cancer Nanotechnology American Scientific; Nalwa, H., Webster, T.J., Eds.; Springer: Berlin, Germany, 2007; pp. 307–316. [Google Scholar]
- Esfandiari, N.; Simchi, A.; Bagheri, R. Size tuning of Ag-decorated TiO2 nanotube arrays for improved bactericidal capacity of orthopedic implants. J. Biomed. Mater. Res. A 2014, 102, 2625–2635. [Google Scholar] [CrossRef]
- Park, J.-W.; Han, S.-H.; Hanawa, T. Effects of Surface Nanotopography and Calcium Chemistry of Titanium Bone Implants on Early Blood Platelet and Macrophage Cell Function. BioMed Res. Internat. 2018. [Google Scholar] [CrossRef]
- Whanger, P.; Vendeland, S.; Park, Y.C.; Xia, Y. Metabolism of subtoxic levels of selenium in animals and humans. Ann. Clin. Lab. Sci. 1996, 26, 99–113. [Google Scholar]
- Webster, T.J.; Ejiofor, J.U. Increased osteoblast adhesion on nanophase metals: Ti, Ti6Al4V, and CoCrMo. Biomaterials 2004, 25, 4731–4739. [Google Scholar] [CrossRef]
- Ercan, B.; Webster, T.J. The effect of biphasic electrical stimulation on osteoblast function at anodized nanotubular titanium surfaces. Biomaterials 2010, 31, 3684–3693. [Google Scholar] [CrossRef] [PubMed]
- Oh, S.; Brammer, K.S.; Li, Y.S.J.; Teng, D.; Engler, A.J.; Chien, S.; Jin, S. Stem cell fate dictated solely by altered nanotube dimension. Proc. Natl. Acad. Sci. USA 2009, 106, 2130–2135. [Google Scholar] [CrossRef] [PubMed]
- Gongadze, E.; Kabaso, D.; Bauer, S.; Slivnik, T.; Schmuki, P.; van Rienen, U.; Iglic, A. Adhesion of osteoblasts to a nanorough titanium implant surface. Int. J. Nanomed. 2011, 6, 1801–1816. [Google Scholar]
- Branemark, P.I.; Adell, R.; Albrektsson, T.; Lekholm, U.; Lundkvist, S.; Rockler, B. Osseointegrated titanium fixtures in the treatment of edentulousness. Biomaterials 1983, 4, 25–28. [Google Scholar] [CrossRef]
- Kubo, K.; Tsukimura, N.; Iwasa, F.; Ueno, T.; Saruwatari, L.; Aita, H.; Chiou, W.-A.; Ogawa, T. Cellular behavior on TiO2 nanonodular structures in a micro-to-nanoscale hierarchy model. Biomaterials 2009, 30, 5319–5329. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, T.; Saruwatari, L.; Takeuchi, K.; Aita, H.; Ohno, N. Ti nano-nodular structuring for bone integration and regeneration. J. Dent. Res. 2008, 87, 751–756. [Google Scholar] [CrossRef]
- Bral, A.; Mommaerts, M.Y. In vivo biofunctionalization of titanium patient-specific implants with nano hydroxyapatite and other nano calcium phosphate coatings: A systematic review. J. Cranio-Maxillofac. Surg. 2016. [Google Scholar] [CrossRef]
- Chen, Z.; Klein, T.; Murray, R.Z.; Crawford, R.; Chang, J.; Wu, C.; Xiao, Y. Osteoimmunomodulation for the development of advanced bone biomaterials. Mater. Today 2016, 19, 304–321. [Google Scholar] [CrossRef]
- Goh, R.C.W.; Chang, C.N.; Lin, C.L.; Lo, L.J. Customised fabricated implants after previous failed cranioplasty. J. Plast. Reconstr. Aesthet. Surg. 2010, 63, 1479–1484. [Google Scholar] [CrossRef]
- Wohlers, T.; Caffrey, T. Wohlers Report 2015: 3D Printing and Additive Manufacturing State of the Industry Annual Worldwide Progress Report; Wohlers Associates: Fort Collins, CO, USA, 2015. [Google Scholar]
- Li, A.; Azad, T.D.; Veeravagu, A.; Bhatti, I.; Long, C.; Ratliff, J.K.; Li, G. Cranioplasty Complications and Costs: A National Population-Level Analysis Using the MarketScan Longitudinal Database. World Neurosurg. 2017, 102, 209–220. [Google Scholar] [CrossRef] [PubMed]
- Mrad, M.A.; Murrad, K.; Antonyshyn, O. Analyzing the Cost of Autogenous Cranioplasty versus Custom-Made Patient-Specific Alloplastic Cranioplasty. J. Craniofac. Surg. 2017, 28, 1260–1263. [Google Scholar] [CrossRef] [PubMed]
- Zanaty, M.; Chalouhi, N.; Starke, R.M.; Clark, S.W.; Bovenzi, C.D.; Saigh, M.; Schwartz, E.; Kunkel, E.S.I.; Efthimiadis-Budike, A.S.; Jabbour, P.; et al. Complications following cranioplasty: Incidence and predictors in 348 cases. J. Neurosurg. 2015, 123, 182–188. [Google Scholar] [CrossRef] [PubMed]
- Júnior, A.C.; Filho, P.T.; Gonçalves, M.P.; Neto, A.A.; Zanini, M. Cranioplasty: An Institutional Experience. J. Craniofacial Surg. 2018, 29, 1402–1405. [Google Scholar] [CrossRef]
- Liang, E.S.; Tipper, G.; Hunt, L.; Chiung Gan, P.Y. Cranioplasty outcomes and associated complications: A single-centre observational study. Br. J. Neurosurg. 2016, 30, 122–127. [Google Scholar] [CrossRef] [PubMed]
- Blake, D.P. The use of synthetics in cranioplasty: A clinical review. Mil Med. 1994, 159, 466–469. [Google Scholar] [CrossRef]
- Kuttenberger, J.J.; Hardt, N. Long-term results following reconstruction of craniofacial defects with titanium micro-mesh systems. J. Craniomaxillofac. Surg. 2001, 29, 75–81. [Google Scholar] [CrossRef]
- Antoniac, I. Handbook of Bioceramics and Biocomposites; Springer International Publishing: New York, NY, USA, 2016; pp. 1275–1307. [Google Scholar]
- Dumitru, M.; Nica, D.; Mohan, A.; Feder, B.; Ciurea, A.V. New concept in cranioplasty based on biomaterials performance in various clinical cases. Key Eng. Mater. 2016, 695, 185–188. [Google Scholar]
- Mohan, A.; Saceleanu, V.; Mohan, D.; Ciurea, A.V. Value of Dural Patches in Obliteration of Cranio-Ethmoidal Traumatic CSF Fistulas. Key Eng. Mater. 2016, 695, 196–199. [Google Scholar] [CrossRef]
- Shuo-Tsung, C.; Cheng-Jen, C.; Wei-Chin, S.; Lin-Wan, C.; Hsuan, C.I.; Muh-Shi, L. 3-D titanium mesh reconstruction of defective skull after frontal craniectomy in traumatic brain injury. Injury 2015, 46, 80–85. [Google Scholar]
- Stoodley, M.A.; Abbott, J.R.; Simpson, D.A. Titanium cranioplasty using 3-D computer modelling of skull defects. J. Clin. Neurosci. 1996, 3, 149–155. [Google Scholar] [CrossRef]
- Patel, M.F.; Langdon, J.D. Titanium mesh (TiMesh) osteosynthesis: A fast and adaptable method of semi-rigid fixation. Br. J. Oral Maxillofac. Surg. 1991, 29, 316–324. [Google Scholar] [CrossRef]
- Rosen, N.; Brady, B.R.; Buonanno, T.J.; Kistler, E.S.; Hinshaw, J.P.; Waldo, S. Potential hazards and artifacts of ferromagnetic and nonferromagnetic surgical devices in nuclear magnetic resonance imaging. Radiology 1982, 147, 139–148. [Google Scholar]
- Cavalu, S.; Prokisch, J.; Laslo, V.; Vicas, S. Preparation, structural characterization and release study of novel hybrid microspheres entrapping nanoselenium, produced by green synthesis. IET Nanobiotechnol. 2016, 11, 426–432. [Google Scholar] [CrossRef] [PubMed]
- Shah, C.P.; Dwivedi, C.; Singh, K.K.; Kumar, M.; Bajaj, P.N. Riley oxidation: A forgotten name reaction for synthesis of selenium nanoparticles. Mat. Res. Bull. 2010, 45, 1213–1217. [Google Scholar] [CrossRef]
- Lin, Z.H.; Wang, C.R. Evidence on the size-dependent absorption spectral evolution of selenium nanoparticles. Mater. Chem. Phys. 2005, 92, 591–594. [Google Scholar] [CrossRef]
- Zhang, J.; Taylor, E.W.; Wan, X.; Peng, D. Impact of heat treatment on size, structure, and bioactivity of elemental selenium nanoparticles. Int. J. Nanomed. 2012, 7, 815–825. [Google Scholar] [CrossRef]
- Chen, Y.; Li, L.; D’ Ulivo, A.; Belzile, N. Extraction and determination of elemental selenium in sediments—A comparative study. Anal. Chim. Acta 2006, 577, 126–133. [Google Scholar] [CrossRef]
- Refat, M.; Elsabawy, S. Infrared spectra, Raman laser, XRD, DSC/TGA and SEM investigations on the preparations of selenium metal, (Sb2O3, Ga2O3, SnO and HgO) oxides and lead carbonate with pure grade using acetamide precursors. Bull. Mater. Sci. 2011, 34, 873. [Google Scholar] [CrossRef]
- Kannan, S.; Mohanraj, K.; Prabhu, K.; Barathan, S.; Sivakumar, G. Synthesis of selenium nanorods with assistance of biomolecule. Bull. Mater. Sci. 2014, 37, 1631–1635. [Google Scholar] [CrossRef]
| Mechanical Methods | ||
| Technologies | Texture/Roughness Size | Outcome/Reference |
| Machining Grinding Blasting | ~1 μm, rough surface formed by subtraction process | Specific surface topographies. Improved adhesion and bonding. Auxiliary method to remove contamination. Rarely solely used [25,26,27,28,29,30,31,32] |
| Shoot peening | 20–80 nm grains on the surface | Improved fatigue resistance, hardness and wear [33,34] |
| Friction stir processing (FSP) | <1 μm, ultrafine grained surface | Improved sliding friction and wear resistance. Incorporation of AgNPs, Zn with antibacterial effect [34,35] |
| Attrition | <100 nm grains on the surface | Improved tensile properties and surface hardness, higher hydrophilicity, better biological affinity [24,36,37] |
| Hydrothermal & pressure (HPT) | flake-like titanate layer on Ti substrate, pore size of 300–600 nm | Minimize the time-consumption and the manufacturing cost. Enhance the in vitro cell-material interactions [38] |
| Physical Methods | ||
| Technologies | Texture/Roughness Size | Outcome/Reference |
| Thermal (flame or plasma) spraying | ~30 to ~200 μm of coatings, such as TiO2, HA, CaP, Al2O3, ZrO2, TiO2 | Improved wear/corrosion resistance and biocompatibility [24,39,40,41] |
| Physical vapor deposition: evaporation, sputtering, ion plating | <1 μm, TiN, TiC, TiCN, TiO2, amorphous carbon films, full density | Improved wear/corrosion resistance and blood compatibility [34,36,42,43] |
| Ion implantation and deposition | ~10 nm of surface modified layer and/or thin film such | Improved hardness, wear, fatigue/corrosion resistance |
| as Ti–O, Ti–N films | and blood compatibility [44,45] | |
| Plasma treatment | <100 nm, TiO2, TiN, TiOH, TiCN layers, full density | Clean and sterilize surface, remove native oxide layer. Improved hardness, wear and corrosion resistances, fatigue limit and biocompatibility [46,47] |
| Plasma polymerization | Not reported | Bioactive surface. Improved cell adhesion [48] |
| Chemical Methods | ||
| Technologies | Texture/Roughness Size | Outcome/Reference |
| Acidic treatment (HF, HCl, H2SO4) | ~10 nm oxide layer on the surface | Remove oxide scales and contamination. Used in combination with other treatments (blasting), higher roughness promoting osteoblasts attachment [49,50] |
| Alkali treatment (NaOH, KOH) | ~1 μm sodium titanate gel on the surface | Improved biocompatibility, bioactivity or bone conductivity [32,51] |
| Hydrogen peroxide treatment | Inner oxide layer <10 nm; outer porous oxide layer up to 40 nm | Improved biocompatibility or bioactivity [34,52] |
| Passivation treatment (nitric acid, phosphoric acid) | ~2–30 nm oxide layer dominated by TiO2, uniform, full density | Enhanced corrosion, resistance and wear resistance, better bioactivity compared to mechanical treatment [34,53] |
| Electrochemical methods (anodization, electrodeposition) | ~10 nm–10 μm uniform, controllable thickness of TiO2 layer; adsorption and incorporation of electrolyte anions | Improved adhesive bonding, corrosion resistance, bioactivity, specific surface topographies [54,55] |
| Chemical vapor deposition | ~1 μm of TiN, TiC, TiCN, diamond and diamond-like carbon thin film, nearly full density | Extremely high hardness and wear resistance compared with Ti substrate. Improved corrosion resistance and blood compatibility [56,57] |
| Sol-gel | <10 μm of thin ceramic coatings, such as Ca3(PO4)2, TiO2, SiO2 | Highly homogeneity and improvement in bioactivity [58,59] |
| Biochemical methods (by soaking- peptide, proteins immobilization, functional molecules, drug loaded) | self-assembled monolayers, does not ensure controlled deposition | Improved bioactivity, biocompatibility, and/or antibacterial functions [60,61] |
| Type of NPs | Fabrication Method | Main Features/Purpose | Reference |
|---|---|---|---|
| TiO2 | direct oxidation | Nanofibers, nanoneedles/better hydrophilicity, biocompatibility and antimicrobial activity, compared to Ti6Al4V | [80] |
| Pulsed laser deposition | Nanorods/Nontoxicity, ability to increase the density of osteoblast cells on the implant, enhanced osseointegration, anticandidal effect, bone formation ability | [81] | |
| Anodic oxidation | Nanotubes incorporating Ca, P and Ag/cells migration on the Ti-based implants due to super hydrophilic properties of crystalline TiO2 nanotubes; apatite formation in simulated body fluid, enhanced MC3T3-E1 cell adhesion and proliferation, antibacterial effect against S. aureus. | [82,83] | |
| plasma electrolytic oxidation | Nanostructured Zn-incorporated TiO2 coatings, grains 20–100 nm/inhibition of S. aureus and E. coli | [84] | |
| Al3O3 | micro-arc oxidation | Nanostructured surface for improved microhardness and wear resistance | [81,85] |
| dipping | Nanostructured surface/promote MSC commitment to | [86] | |
| - | the osteoblast phenotype, increase in bone-implant contact area and torque removal | - | |
| Nano Hydroxyapatite | discrete crystalline deposition | Complex surface morphology via the bonded HA nanoparticles/progressive osseointegration profiles | [78,87] |
| Nano-crystalline diamond | Plasma spray | Nanosized crystallites/proteins immobilization on nanocrystalline diamond/osteoinductive effect in irradiated bone | [78,88] |
| Ag NPs | silanization method | Spherical morphology, 100 nm diameter, antibacterial and anti-adhesive activities towards S. aureus and E. coli. | [24,83,89] |
| ZnO NPs | EHDA spraying. | rod-shaped structure ~100 nm/significant antimicrobial activity against Staphylococcus aureus/early bone formation | [90] |
| Au Nps | Magnetron sputtering | 40–80 nm thin layer of pure gold/early mechanical fixation | [91] |
| Se Nps | Hydrothermal deposition | Spherical, rods, wire nanostructure, using different saccharides as reducing agent/favorable results on RBC osmotic fragility and fibroblasts adhesion to accelerate osseointegration, bone cancer treatment. | [92,93,94,95] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cavalu, S.; Antoniac, I.V.; Mohan, A.; Bodog, F.; Doicin, C.; Mates, I.; Ulmeanu, M.; Murzac, R.; Semenescu, A. Nanoparticles and Nanostructured Surface Fabrication for Innovative Cranial and Maxillofacial Surgery. Materials 2020, 13, 5391. https://doi.org/10.3390/ma13235391
Cavalu S, Antoniac IV, Mohan A, Bodog F, Doicin C, Mates I, Ulmeanu M, Murzac R, Semenescu A. Nanoparticles and Nanostructured Surface Fabrication for Innovative Cranial and Maxillofacial Surgery. Materials. 2020; 13(23):5391. https://doi.org/10.3390/ma13235391
Chicago/Turabian StyleCavalu, Simona, Iulian Vasile Antoniac, Aurel Mohan, Florian Bodog, Cristian Doicin, Ileana Mates, Mihaela Ulmeanu, Roman Murzac, and Augustin Semenescu. 2020. "Nanoparticles and Nanostructured Surface Fabrication for Innovative Cranial and Maxillofacial Surgery" Materials 13, no. 23: 5391. https://doi.org/10.3390/ma13235391
APA StyleCavalu, S., Antoniac, I. V., Mohan, A., Bodog, F., Doicin, C., Mates, I., Ulmeanu, M., Murzac, R., & Semenescu, A. (2020). Nanoparticles and Nanostructured Surface Fabrication for Innovative Cranial and Maxillofacial Surgery. Materials, 13(23), 5391. https://doi.org/10.3390/ma13235391








