Piezoelectric Implant Site Preparation: Influence of Handpiece Movements on Temperature Elevation
Abstract
:1. Introduction
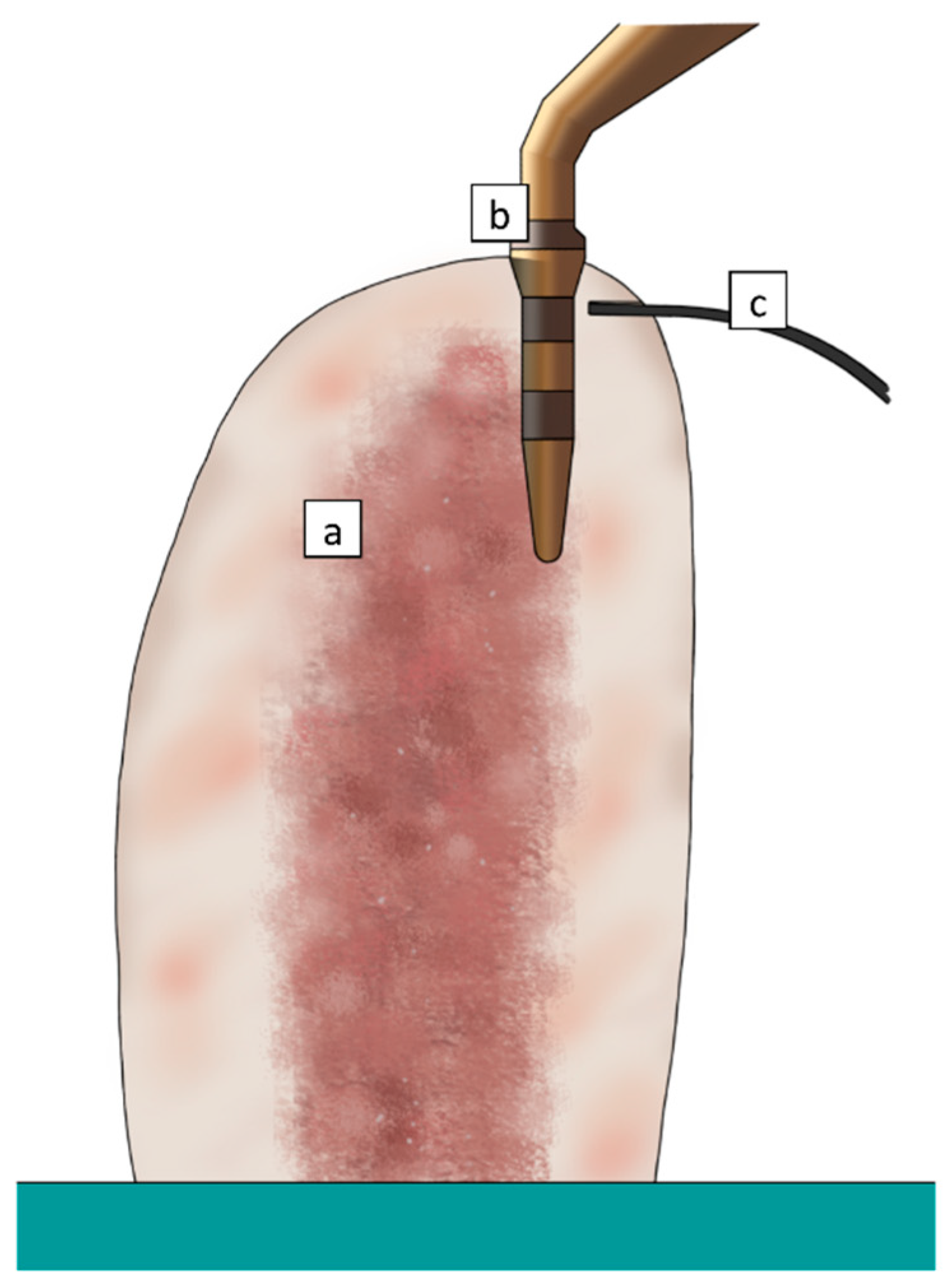
2. Experimental Section
- -
- Duration (s): Time necessary to perform each osteotomy to a 10 mm depth;
- -
- Cycles: Number of cycles necessary to perform each osteotomy to a 10 mm depth;
- -
- Tmax (°C): Highest recorded temperature;
- -
- Tmax (°C): Highest recorded temperature;
- -
- T±30 (°C): Arithmetic mean of all temperature data points recorded from 30 s before to 30 s after the highest recorded temperature.
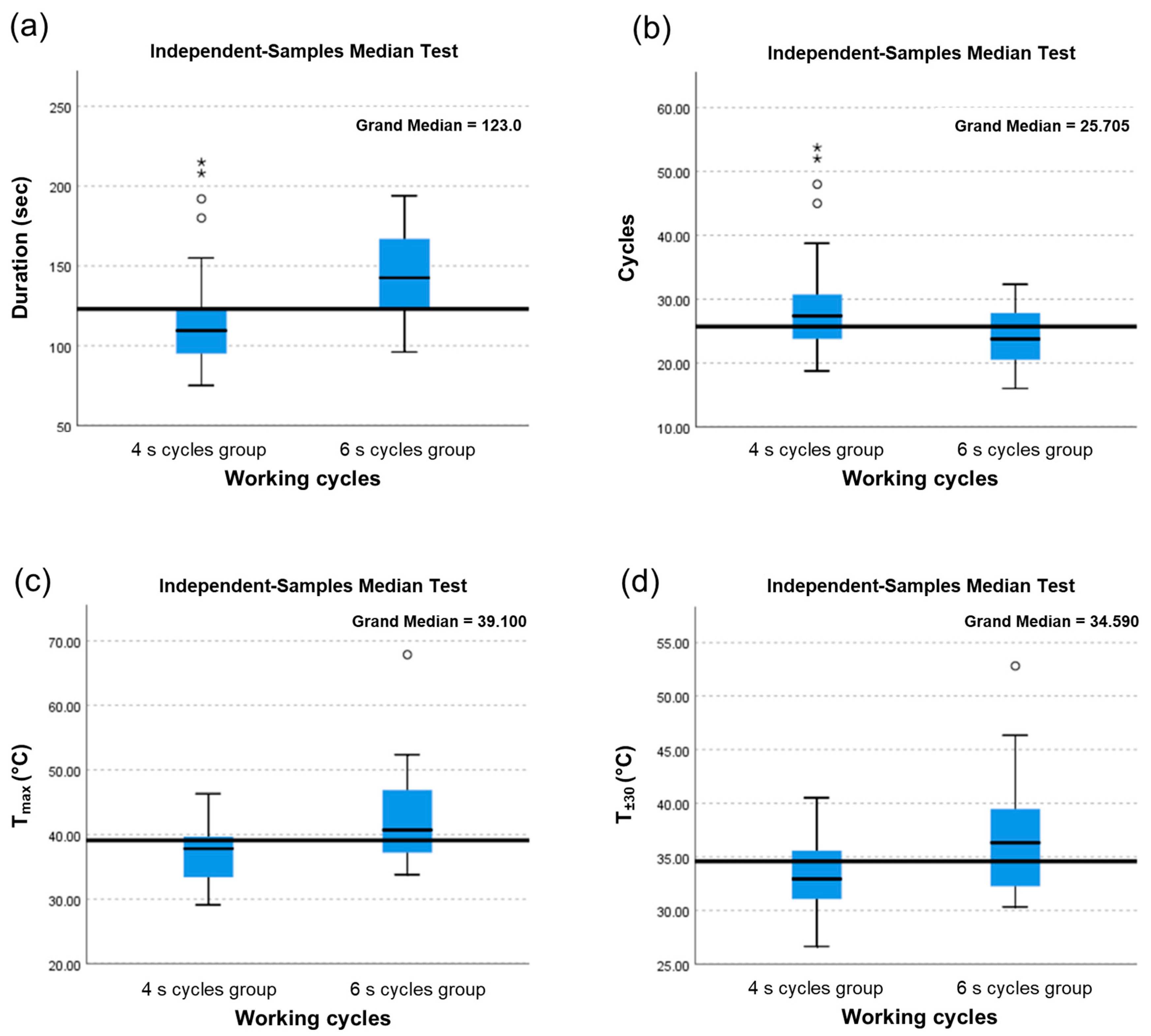
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Stacchi, C.; Bassi, F.; Troiano, G.; Rapani, A.; Lombardi, T.; Jokstad, A.; Sennerby, L.; Schierano, G. Piezoelectric bone surgery for implant site preparation compared with conventional drilling techniques: A systematic review, meta-analysis and trial sequential analysis. Int. J. Oral Implantol. 2020, 13, 141–158. [Google Scholar]
- Atieh, M.A.; Alsabeeha, N.H.M.; Tawse-Smith, A.; Duncan, W.J. Piezoelectric versus conventional implant site preparation: A systematic review and meta-analysis. Clin. Implant Dent. Relat. Res. 2018, 20, 261–270. [Google Scholar] [CrossRef] [PubMed]
- Hennet, P. Piezoelectric bone surgery: A review of the literature and potential applications in veterinary oromaxillofacial surgery. Front. Vet. Sci. 2015, 2, 8. [Google Scholar] [CrossRef] [Green Version]
- Peker Tekdal, G.; Bostanci, N.; Belibasakis, G.N.; Gürkan, A. The effect of piezoelectric surgery implant osteotomy on radiological and molecular parameters of peri-implant crestal bone loss: A randomized, controlled, split-mouth trial. Clin. Oral Implant. Res. 2016, 27, 535–544. [Google Scholar] [CrossRef] [PubMed]
- Zizzari, V.L.; Berardi, D.; Congedi, F.; Tumedei, M.; Cataldi, A.; Perfetti, G. Morphological aspect and iNOS and bax expression modification in bone tissue around dental implants positioned using piezoelectric bone surgery versus conventional drill Technique. J. Craniofacial Surg. 2015, 26, 741–744. [Google Scholar] [CrossRef]
- Preti, G.; Martinasso, G.; Peirone, B.; Navone, R.; Manzella, C.; Muzio, G.; Russo, C.; Canuto, R.A.; Schierano, G. Cytokines and growth factors involved in the osseointegration of oral titanium implants positioned using piezoelectric bone surgery versus a drill technique: A pilot study in minipigs. J. Periodontol. 2007, 78, 716–722. [Google Scholar] [CrossRef] [Green Version]
- Lajolo, C.; Valente, N.A.; Romandini, W.G.; Petruzzi, M.; Verdugo, F.; D’Addona, A. Bone heat generated using conventional implant drills versus piezosurgery unit during apical cortical plate perforation. J. Periodontol. 2018, 89, 661–668. [Google Scholar] [CrossRef]
- Stelzle, F.; Frenkel, C.; Riemann, M.; Knipfer, C.; Stockmann, P.; Nkenke, E. The effect of load on heat production, thermal effects and expenditure of time during implant site preparation—An experimental ex vivo comparison between piezosurgery and conventional drilling. Clin. Oral Implant. Res. 2014, 25, 140–148. [Google Scholar] [CrossRef]
- Stacchi, C.; Robiony, M.; Motta Jones, J.; Lombardi, T.; Verardi, S. Letter to the editor: RE: Bone heat generated using conventional implant drills versus piezosurgery unit during apical cortical plate perforation. J. Periodontol. 2018, 89, 1161–1162. [Google Scholar] [CrossRef]
- Pavlíková, G.; Foltán, R.; Horká, M.; Hanzelka, T.; Borunská, H.; Sedý, J. Piezosurgery in oral and maxillofacial surgery. Int. J. Oral Maxillofac. Surg. 2011, 40, 451–457. [Google Scholar] [CrossRef]
- Gehrke, S.A.; Loffredo Neto, H.; Mardegan, F.E. Investigation of the effect of movement and irrigation systems on temperature in the conventional drilling of cortical bone. Br. J. Oral Maxillofac. Surg. 2013, 51, 953–957. [Google Scholar] [CrossRef]
- Davidson, S.R.; James, D.F. Measurement of thermal conductivity of bovine cortical bone. Med. Eng. Phys. 2000, 22, 741–747. [Google Scholar] [CrossRef]
- Szalma, J.; Lovász, B.V.; Vajta, L.; Soós, B.; Lempel, E.; Möhlhenrich, S.C. The influence of the chosen in vitro bone simulation model on intraosseous temperatures and drilling times. Sci. Rep. 2019, 9, 11817. [Google Scholar] [CrossRef]
- Sedlin, E.D.; Hirsch, C. Factors affecting the determination of the physical properties of femoral cortical bone. Acta Orthop. Scand. 1966, 37, 29–48. [Google Scholar] [CrossRef]
- Lamazza, L.; Laurito, D.; Lollobrigida, M.; Brugnoletti, O.; Garreffa, G.; De Biase, A. Identification of possible factors influencing temperatures elevation during implant site preparation with piezoelectric technique. Ann. Stomatol. 2015, 5, 115–122. [Google Scholar]
- Laurito, D.; Lamazza, L.; Garreffa, G.; De Biase, A. An alternative method to record rising temperatures during dental implant site preparation: A preliminary study using bovine bone. Ann. Dell’istituto Super. Sanita 2010, 46, 405–410. [Google Scholar]
- García-Moreno, S.; González-Serrano, J.; López-Pintor, R.M.; Pardal-Peláez, B.; Hernández, G.; Martínez-González, J.M. Implant stability using piezoelectric bone surgery compared with conventional drilling: A systematic review and meta-analysis. Int. J. Oral Maxillofac. Surg. 2018, 47, 1453–1464. [Google Scholar] [CrossRef]
- Timon, C.; Keady, C. Thermal osteonecrosis caused by bone drilling in orthopedic surgery: A literature review. Cureus 2019, 11, e5226. [Google Scholar] [CrossRef] [Green Version]
- Dolan, E.B.; Haugh, M.G.; Tallon, D.; Casey, C.; McNamara, L.M. Heat-shock-induced cellular responses to temperature elevations occurring during orthopaedic cutting. J. R. Soc. Interface 2012, 9, 3503–3513. [Google Scholar] [CrossRef] [Green Version]
- Pandey, R.K.; Panda, S.S. Drilling of bone: A comprehensive review. J. Clin. Orthop. Trauma 2013, 4, 15–30. [Google Scholar] [CrossRef] [Green Version]
- Yoshida, K.; Uoshima, K.; Oda, K.; Maeda, T. Influence of heat stress to matrix on bone formation. Clin. Oral Implant. Res. 2009, 20, 782–790. [Google Scholar] [CrossRef]
- Lamazza, L.; Garreffa, G.; Laurito, D.; Lollobrigida, M.; Palmieri, L.; De Biase, A. Temperature values variability in piezoelectric implant site preparation: Differences between cortical and corticocancellous bovine bone. BioMed Res. Int. 2016, 6473680. [Google Scholar] [CrossRef] [Green Version]
- Karaca, F.; Aksakal, B.; Kom, M. Influence of orthopaedic drilling parameters on temperature and histopathology of bovine tibia: An in vitro study. Med. Eng. Phys. 2011, 33, 1221–1227. [Google Scholar] [CrossRef]
- Tang, H.; Deng, W.; Sun, Z.; Wang, Y.; Li, L.; Ding, Y.; Zhou, Y. Optimization of factors influencing temperature rise and thermal necrosis of a robot driven piezoelectric osteotomy in bovine cortical bone: An in vitro study using an orthogonal test design. Clin. Biomech. 2019, 70, 249–256. [Google Scholar] [CrossRef]
- Doblaré, M.; García, J.M.; Gómez, M.J. Modelling bone tissue fracture and healing: A review. Eng. Fract. Mech. 2004, 71, 1809–1840. [Google Scholar] [CrossRef]
- Abdel-Wahab, A.A.; Alam, K.; Silberschmidt, V.V. Analysis of anisotropic viscoelastoplastic properties of cortical bone tissues. J. Mech. Behav. Biomed. Mater. 2011, 4, 807–820. [Google Scholar] [CrossRef] [Green Version]

| 4 s Cycles Group | 6 s Cycles Group | p Value # | |||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Duration (s) | 119.80 | 36.4 | 143.17 | 29.4 | 0.002 |
| Cycles | 29.95 | 9.1 | 23.80 | 4.9 | 0.005 |
| Tmax (°C) | 37.24 | 4.6 | 42.44 | 7.3 | 0.002 |
| T±30 (°C) | 33.30 | 3.3 | 37.01 | 5.2 | 0.003 |
| 4 s Cycles Group | 6 s Cycles Group | p Value # | |
|---|---|---|---|
| Median | Median | ||
| Duration (s) | 108.67 | 142.50 | <0.0001 |
| Cycles | 27.17 | 23.75 | 0.020 |
| Tmax (°C) | 37.82 | 40.71 | 0.020 |
| T±30 (°C) | 32.94 | 36.32 | 0.020 |
| F * | p Value | |
|---|---|---|
| Duration (s) | 0.13 | 0.72 |
| Cycles | 4.35 | 0.04 |
| Tmax (°C) | 2.37 | 0.13 |
| T±30 (°C) | 3.48 | 0.07 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lamazza, L.; Lollobrigida, M.; Vozza, I.; Palmieri, L.; Stacchi, C.; Lombardi, T.; De Biase, A. Piezoelectric Implant Site Preparation: Influence of Handpiece Movements on Temperature Elevation. Materials 2020, 13, 4072. https://doi.org/10.3390/ma13184072
Lamazza L, Lollobrigida M, Vozza I, Palmieri L, Stacchi C, Lombardi T, De Biase A. Piezoelectric Implant Site Preparation: Influence of Handpiece Movements on Temperature Elevation. Materials. 2020; 13(18):4072. https://doi.org/10.3390/ma13184072
Chicago/Turabian StyleLamazza, Luca, Marco Lollobrigida, Iole Vozza, Luigi Palmieri, Claudio Stacchi, Teresa Lombardi, and Alberto De Biase. 2020. "Piezoelectric Implant Site Preparation: Influence of Handpiece Movements on Temperature Elevation" Materials 13, no. 18: 4072. https://doi.org/10.3390/ma13184072







