Customized 3D-Printed Titanium Mesh Developed to Regenerate a Complex Bone Defect in the Aesthetic Zone: A Case Report Approached with a Fully Digital Workflow
Abstract
1. Introduction
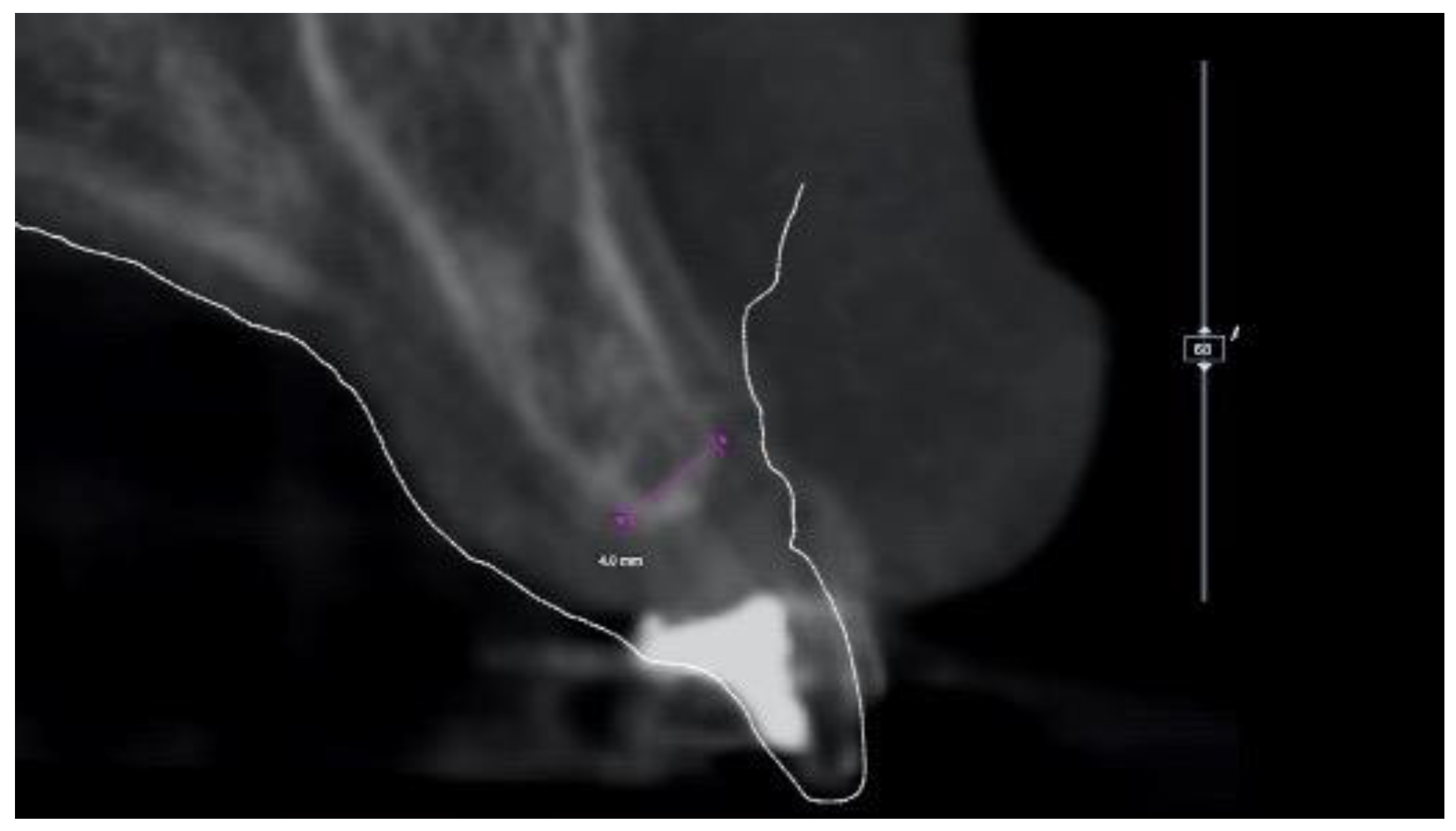
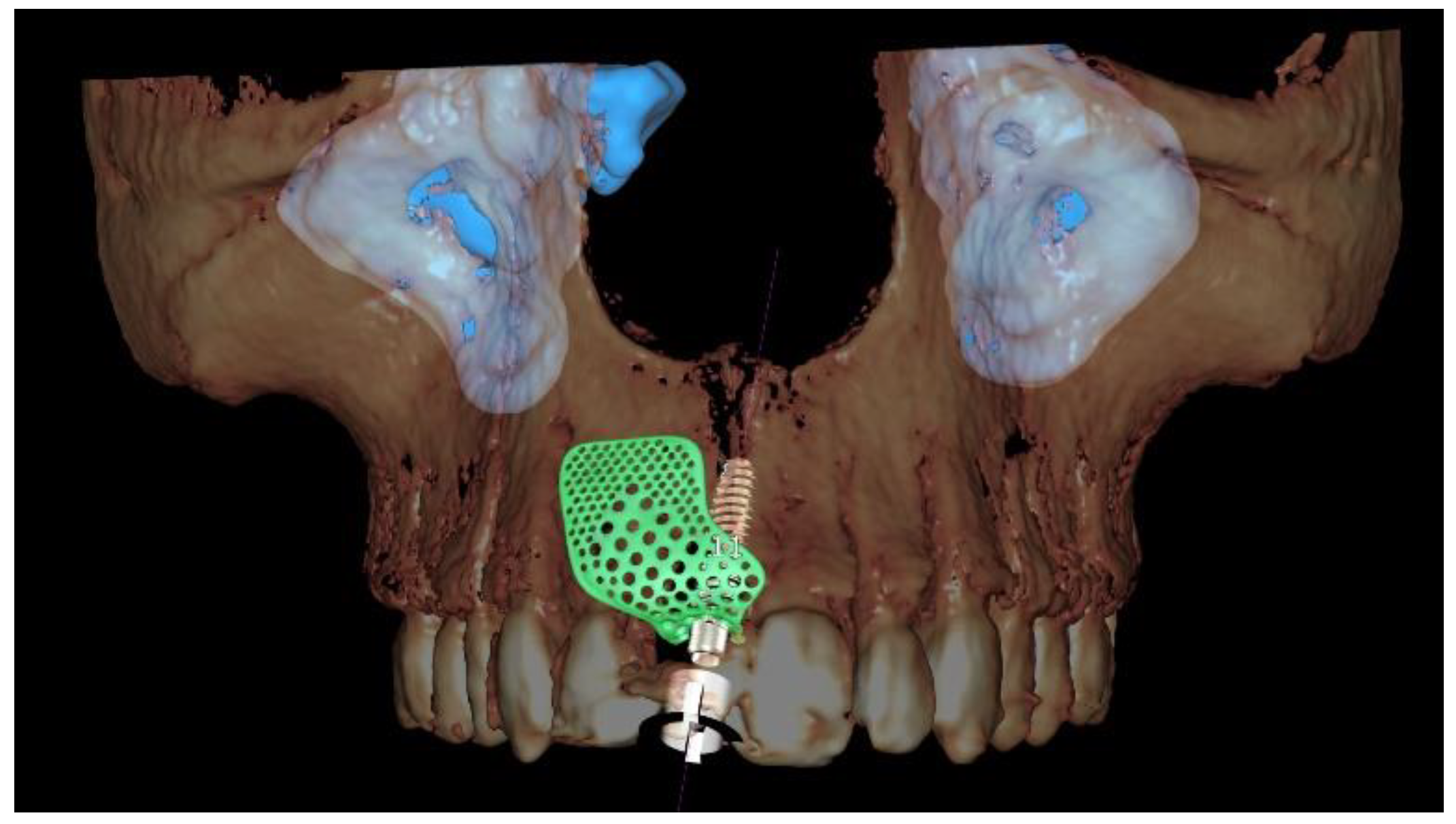
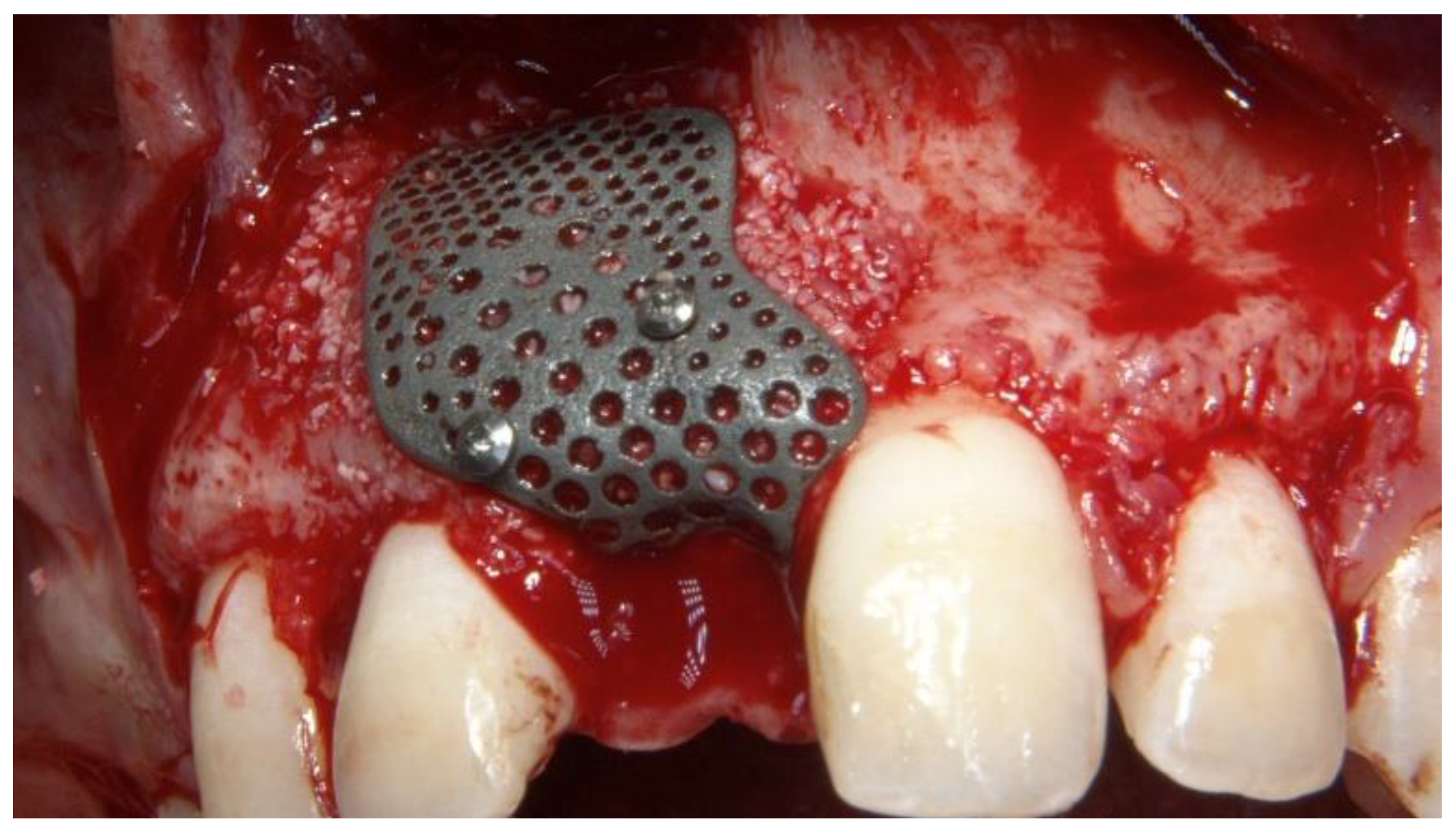
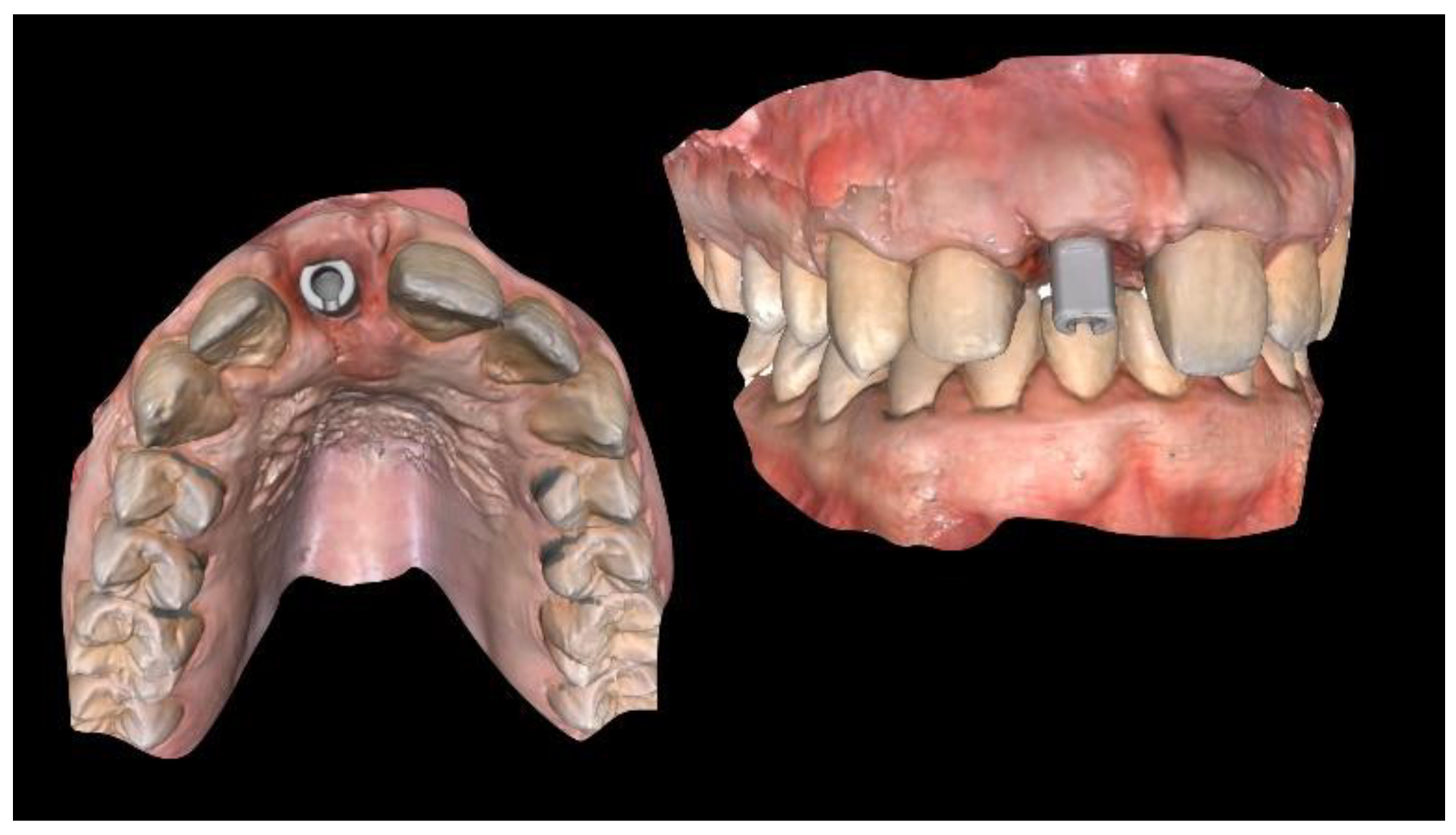
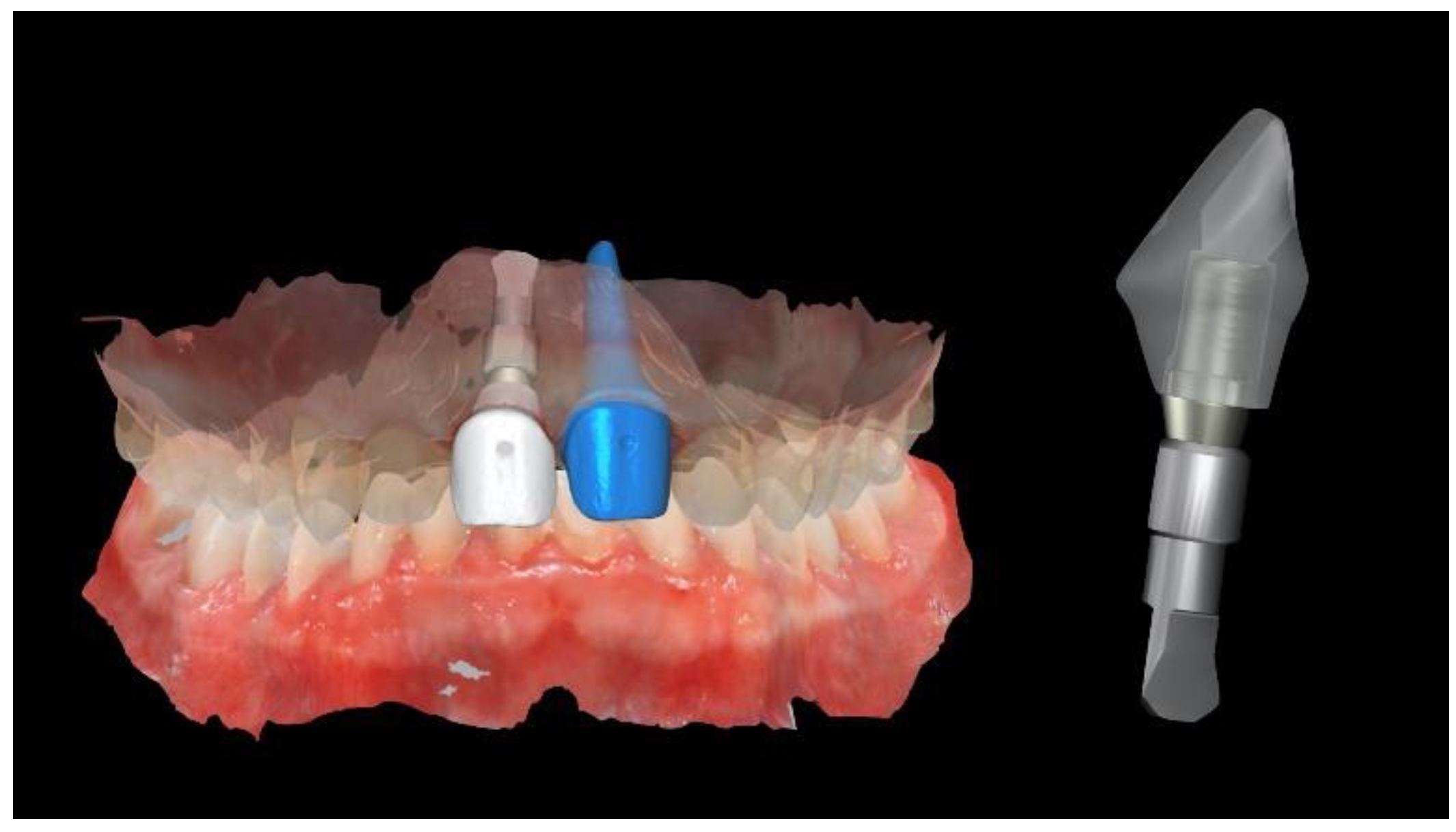
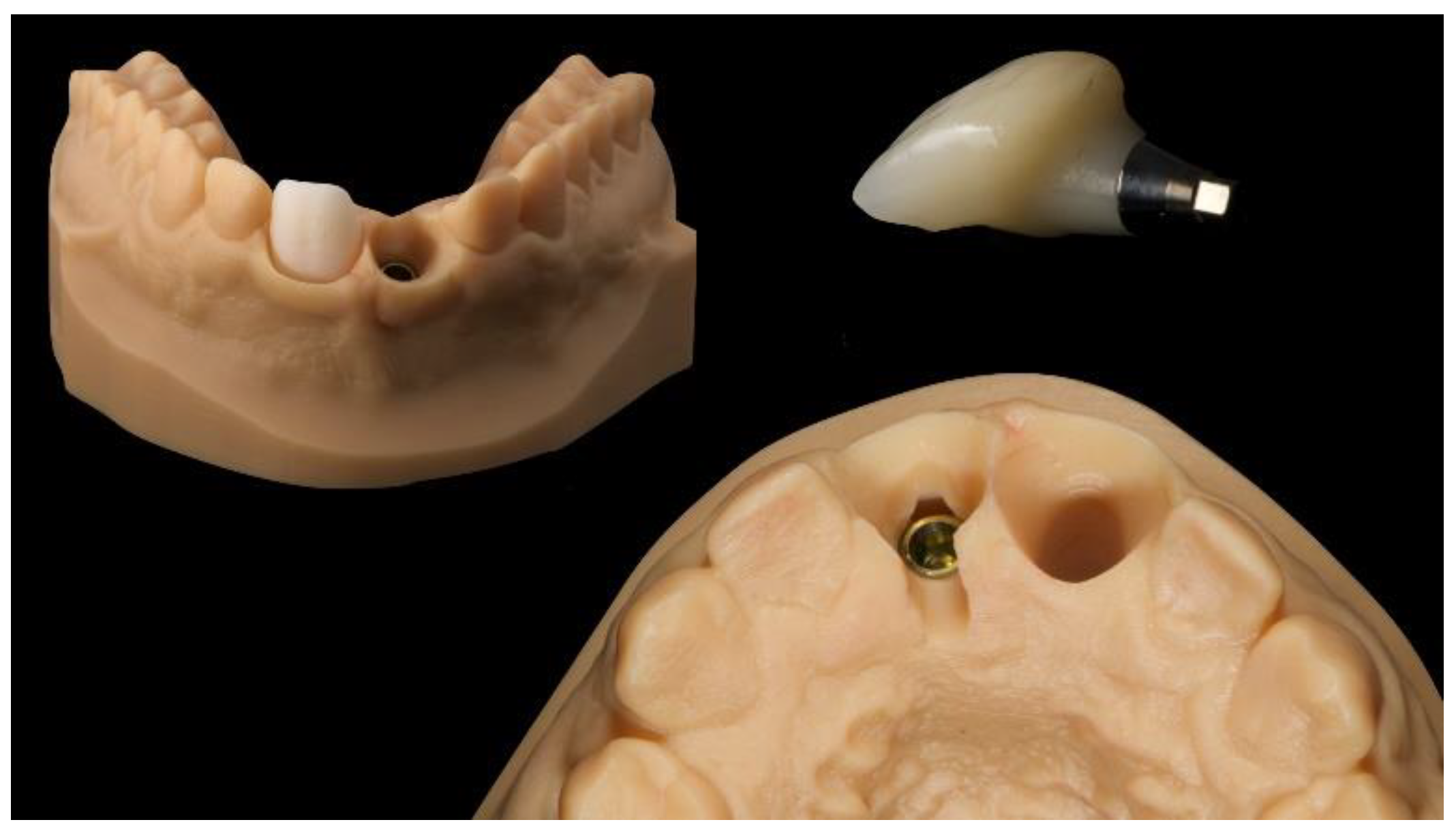
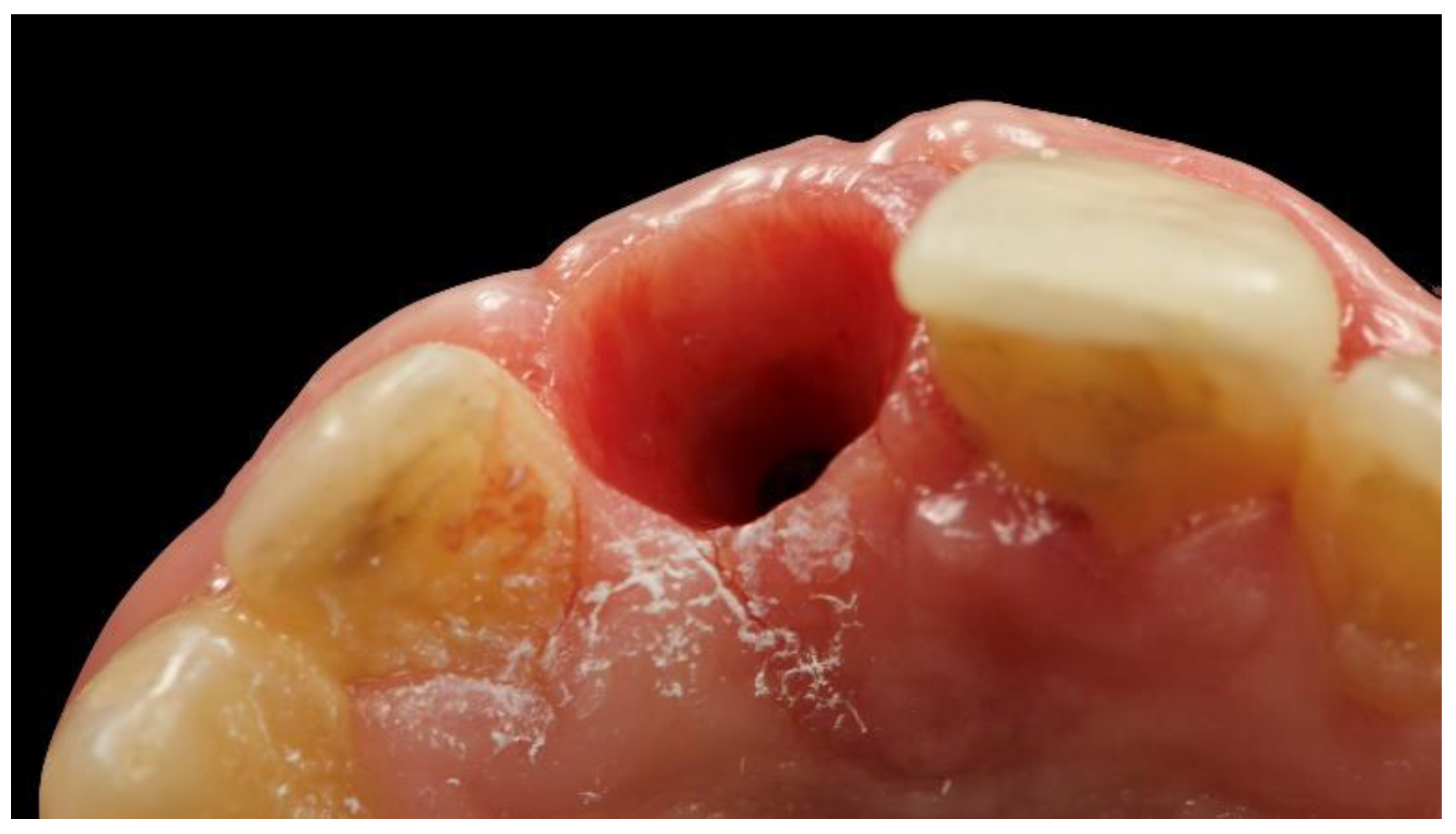
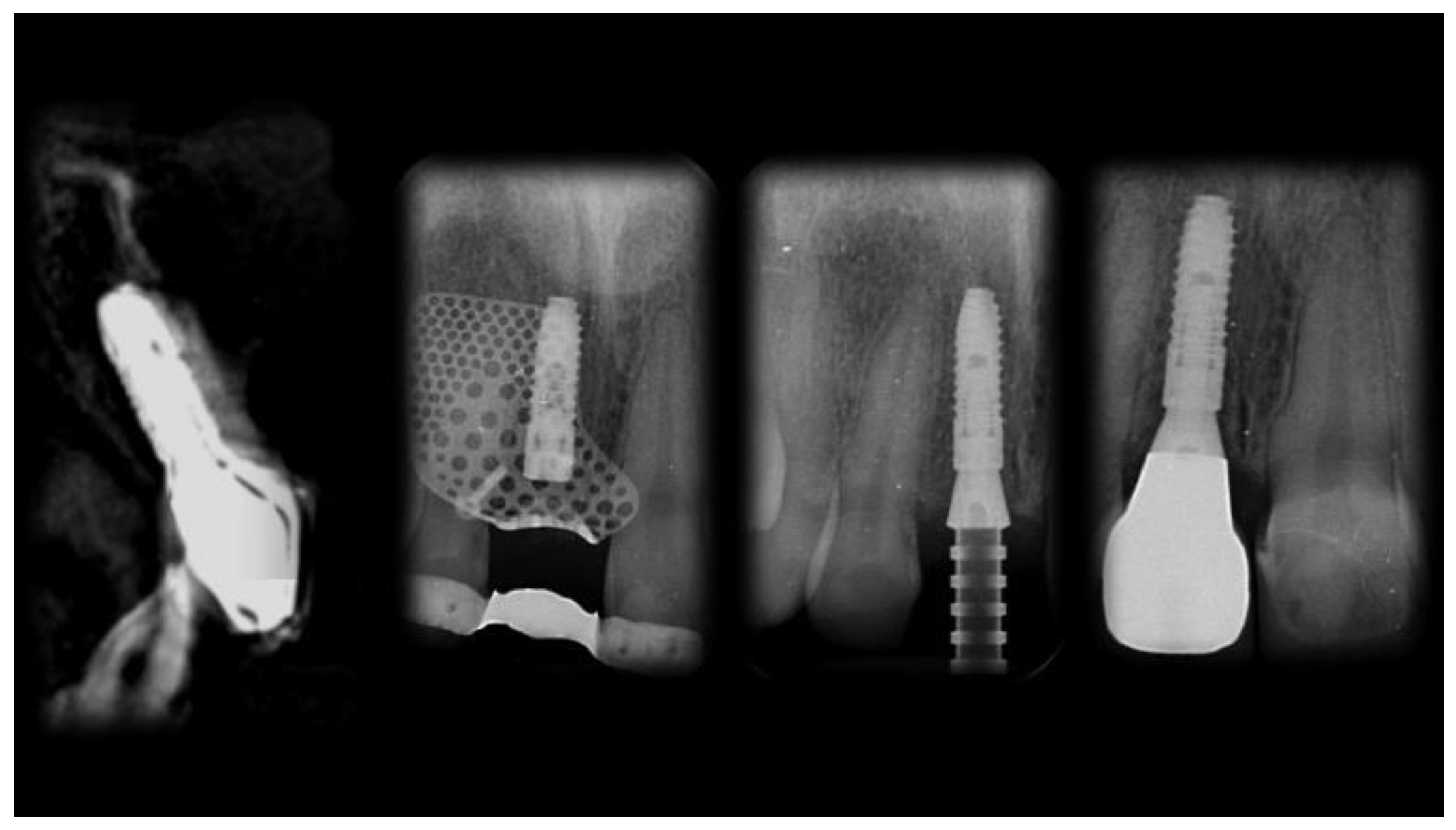
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Esposito, M.; Trullenque-Eriksson, A.; Tallarico, M. Endodontic retreatment versus dental implants of teeth with an uncertain endodontic prognosis: 3-year results from a randomised controlled trial. Eur. J. Oral Implantol. 2018, 11, 423–438. [Google Scholar] [PubMed]
- Meloni, S.M.; Lumbau, A.; Baldoni, E.; Pisano, M.; Spano, G.; Massarelli, O.; Tallarico, M. Platform switching versus regular platform single implants: 5-year post-loading results from a randomised controlled trial. Int. J. Oral Implantol. (New Malden) 2020, 13, 43–52. [Google Scholar]
- Meloni, S.M.; Lumbau, A.; Spano, G.; Baldoni, E.; Pisano, M.; Tullio, A.; Tallarico, M. Sinus augmentation grafting with anorganic bovine bone versus 50% autologous bone mixed with 50% anorganic bovine bone: 5 years after loading results from a randomised controlled trial. Int. J. Oral Implantol. (New Malden) 2019, 12, 483–492. [Google Scholar]
- Meloni, S.M.; Spano, G.; Ceruso, F.M.; Gargari, M.; Lumbau, A.; Baldoni, E.; Massarelli, O.; Pisano, M.; Tallarico, M. Upper jaw implant restoration on six implants with flapless guided template surgery and immediate loading: 5 years results of a prospective case series. Oral Implantol. 2020, 12, 151–160. [Google Scholar] [CrossRef]
- Tallarico, M.; Cervino, G.; Scrascia, R.; Uccioli, U.; Lumbau, A.I.; Meloni, S.M. Minimally invasive treatment of edentulous maxillae with overdenture fully supported by a cad/cam Titanium Bar with a low-profile attachment screwed on four or six implants: A case series. Prosthesis 2020, 2, 53–64. [Google Scholar] [CrossRef]
- Meloni, S.M.; Jovanovic, S.A.; Urban, I.; Baldoni, E.; Pisano, M.; Tallarico, M. Horizontal ridge augmentation using GBR with a native collagen membrane and 1:1 ratio of particulate xenograft and autologous bone: A 3-year after final loading prospective clinical study. Clin. Implant. Dent. Relat. Res. 2019, 12, 22–29. [Google Scholar] [CrossRef]
- Meloni, S.M.; Jovanovic, S.A.; Urban, I.; Canullo, L.; Pisano, M.; Tallarico, M. Horizontal ridge augmentation using GBR with a native collagen membrane and 1:1 ratio of Particulated Xenograft and Autologous Bone: A 1-year prospective clinical study. Clin. Implant. Dent. Relat. Res. 2017, 19, 38–45. [Google Scholar] [CrossRef]
- Meloni, S.M.; Jovanovic, S.A.; Pisano, M.; De Riu, G.; Baldoni, E.; Tallarico, M. One-stage horizontal guided bone regeneration with autologous bone, anorganic bovine bone and collagen membranes: Follow-up of a prospective study 30 months after loading. Eur. J. Oral Implantol. 2018, 15, 1–7. [Google Scholar]
- Testori, T.; Weinstein, T.; Scutellà, F.; Wang, H.L.; Zucchelli, G. Implant placement in the esthetic area: Criteria for positioning single and multiple implants. Periodontology 2000 2018, 77, 176–196. [Google Scholar] [CrossRef]
- Buser, D.; Martin, W.; Belser, U.C. Optimizing esthetics for implant restorations in the anterior maxilla: Anatomic and surgical considerations. Int. J. Oral Maxillofac. Implants 2004, 19, 43–61. [Google Scholar]
- Tallarico, M.; Kim, Y.J.; Cocchi, F.; Martinolli, M.; Meloni, S.M. Accuracy of newly developed sleeve-designed templates for insertion of dental implants: A prospective multicenters clinical trial. Clin. Implant. Dent. Relat. Res. 2018, 11, 203–206. [Google Scholar] [CrossRef] [PubMed]
- Tallarico, M.; Meloni, S.M.; Canullo, L.; Caneva, M.; Polizzi, G. Five-year results of a randomized controlled trial comparing patients rehabilitated with immediately loaded maxillary cross-arch fixed dental prosthesis supported by four or six implants placed using guided surgery. Clin. Implant. Dent. Relat. Res. 2016, 18, 965–972. [Google Scholar] [CrossRef] [PubMed]
- Meloni, S.M.; Tallarico, M.; Pisano, M.; Xhanari, E.; Canullo, L. Immediate loading of fixed complete denture prosthesis supported by 4-8 implants placed using guided surgery: A 5-year prospective study on 66 patients with 356 implants. Clin. Implant. Dent. Relat. Res. 2016, 37, 610–621. [Google Scholar] [CrossRef] [PubMed]
- Tallarico, M.; Meloni, S. Retrospective analysis on survival rate, template-related complications, and prevalence of peri-implantitis of 694 anodized implants placed using computer-guided surgery: Results between 1 and 10 years of follow-up. Int. J. Oral Maxillofac. Implants 2017, 32, 1162–1171. [Google Scholar] [CrossRef]
- Tallarico, M.; Esposito, M.; Xhanari, E.; Caneva, M.; Meloni, S.M. Computer-guided vs freehand placement of immediately loaded dental implants: 5-year post- loading results of a randomised controlled trial. Eur. J. Oral Implantol. 2018, 11, 203–213. [Google Scholar]
- Tallarico, M.; Luzi, C.; Galasso, G.; Lione, R.; Cozza, P. Comprehensive rehabilitation and natural esthetics with implant and orthodontics (CRANIO): An interdisciplinary approach to missingmaxillary lateral incisors. J. Oral Sci. Rehabil. 2017, 3, 8–16. [Google Scholar]
- Tallarico, M.; Ceruso, F.M.; Muzzi, L.; Meloni, S.M.; Kim, Y.J.; Gargari, M.; Martinolli, M. Effect of simultaneous immediate implant placement and guided bone reconstruction with ultra-fine titanium mesh membranes on radiographic and clinical parameters after 18 months of loading. Materials 2019, 12, 1710. [Google Scholar] [CrossRef]
- Trento, G.S.; Carvalho, P.H.A.; Macedo, D.V.; Gabrielli, M.A.C.; Monnazzi, M.S.; Pereira-Filho, V.A. Titanium mesh associated with rhBMP-2 in alveolar ridge reconstruction. Int. J. Oral Maxillofac. Surg. 2019, 48, 546–553. [Google Scholar] [CrossRef]
- Jung, G.U.; Jeon, J.Y.; Hwang, K.G.; Park, C.J. Preliminary evaluation of a three-dimensional, customized, and preformed titanium mesh in peri-implant alveolar bone regeneration. J. Korean Assoc. Oral Maxillofac. Surg. 2014, 40, 181–188. [Google Scholar] [CrossRef]
- Tallarico, M.; Martinolli, M.; Kim, Y.J.; Cocchi, F.; Meloni, S.M.; Alushi, A.; Xhanari, E. Accuracy of computer-assisted template-based implant placement using two different surgical templates designed with or without metallic sleeves: A randomized controlled trial. Dent. J. 2019, 7, 41. [Google Scholar] [CrossRef]
- Tallarico, M.; Erta, X.; Yong, J.K.; Cocchi, F.; Martinolli, M.; Adem, A.; Baldoni, E.; Meloni, S.M. Accuracy of computer-assisted template-based implant placement using conventional impression and scan model or intraoral digital impression: A randomised controlled trial with 1 year of follow-up. Int. J. Oral Implantol. 2019, 12, 197–206. [Google Scholar]
- Mangano, F.; Mangano, C.; Margiani, B.; Admakin, O. Combining intraoral and face scans for the design and fabrication of computer-assisted design/computer-assisted manufacturing (CAD/CAM) polyether-ether-ketone (PEEK) implant-supported bars for maxillary overdentures. Scanning 2019, 2019, 4274715. [Google Scholar] [CrossRef] [PubMed]
- Mangano, F.; Hauschild, U.; Veronesi, G.; Imburgia, M.; Mangano, C.; Admakin, O. Trueness and precision of 5 intraoral scanners in the impressions of single and multiple implants: A comparative in vitro study. BMC Oral Health 2019, 19, 101. [Google Scholar] [CrossRef] [PubMed]









© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tallarico, M.; Park, C.-J.; Lumbau, A.I.; Annucci, M.; Baldoni, E.; Koshovari, A.; Meloni, S.M. Customized 3D-Printed Titanium Mesh Developed to Regenerate a Complex Bone Defect in the Aesthetic Zone: A Case Report Approached with a Fully Digital Workflow. Materials 2020, 13, 3874. https://doi.org/10.3390/ma13173874
Tallarico M, Park C-J, Lumbau AI, Annucci M, Baldoni E, Koshovari A, Meloni SM. Customized 3D-Printed Titanium Mesh Developed to Regenerate a Complex Bone Defect in the Aesthetic Zone: A Case Report Approached with a Fully Digital Workflow. Materials. 2020; 13(17):3874. https://doi.org/10.3390/ma13173874
Chicago/Turabian StyleTallarico, Marco, Chang-Joo Park, Aurea Immacolata Lumbau, Marco Annucci, Edoardo Baldoni, Alba Koshovari, and Silvio Mario Meloni. 2020. "Customized 3D-Printed Titanium Mesh Developed to Regenerate a Complex Bone Defect in the Aesthetic Zone: A Case Report Approached with a Fully Digital Workflow" Materials 13, no. 17: 3874. https://doi.org/10.3390/ma13173874
APA StyleTallarico, M., Park, C.-J., Lumbau, A. I., Annucci, M., Baldoni, E., Koshovari, A., & Meloni, S. M. (2020). Customized 3D-Printed Titanium Mesh Developed to Regenerate a Complex Bone Defect in the Aesthetic Zone: A Case Report Approached with a Fully Digital Workflow. Materials, 13(17), 3874. https://doi.org/10.3390/ma13173874







