Optimal Position of Attachment for Removable Thermoplastic Aligner on the Lower Canine Using Finite Element Analysis
Abstract
1. Introduction
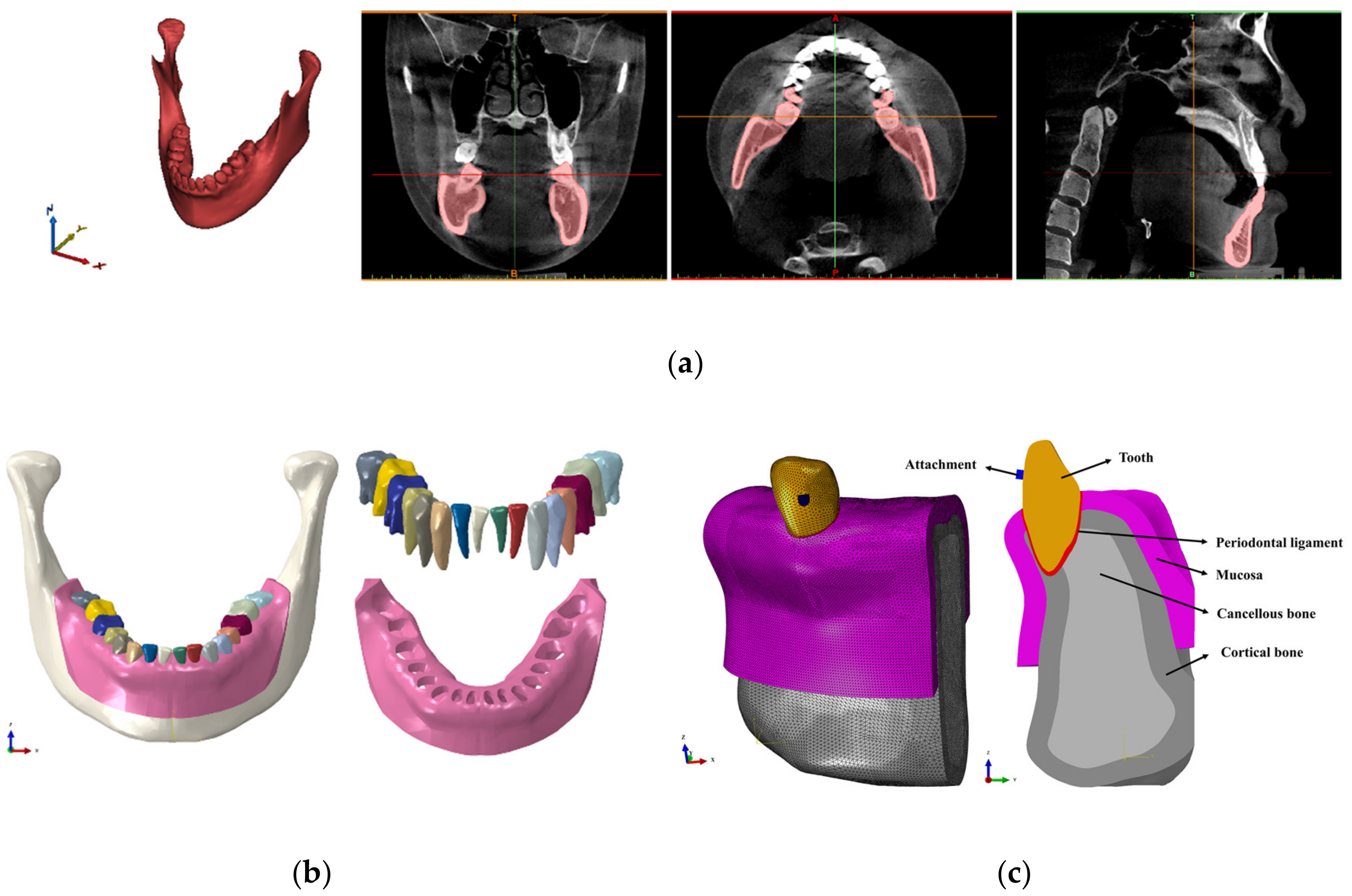
2. Materials and Methods
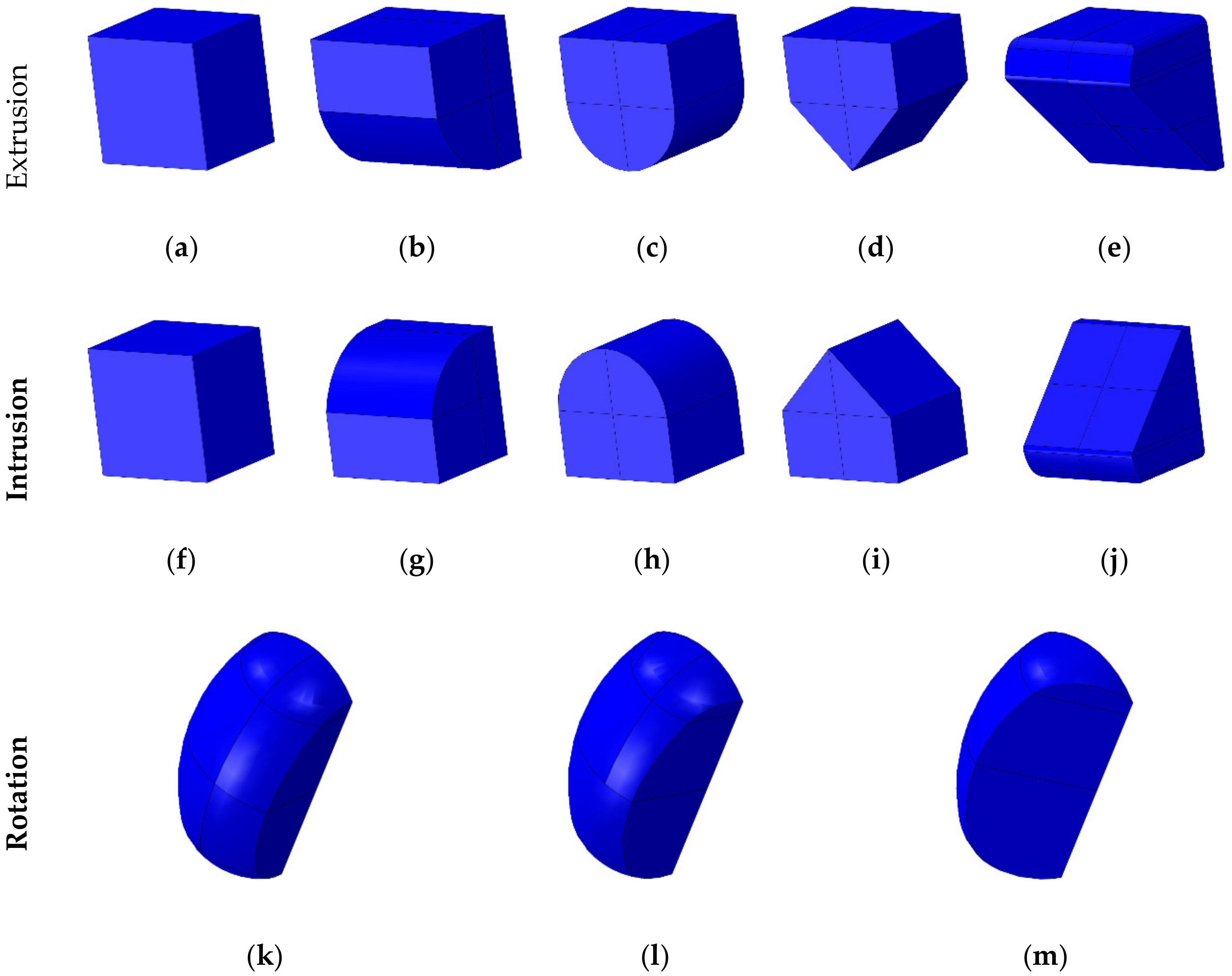
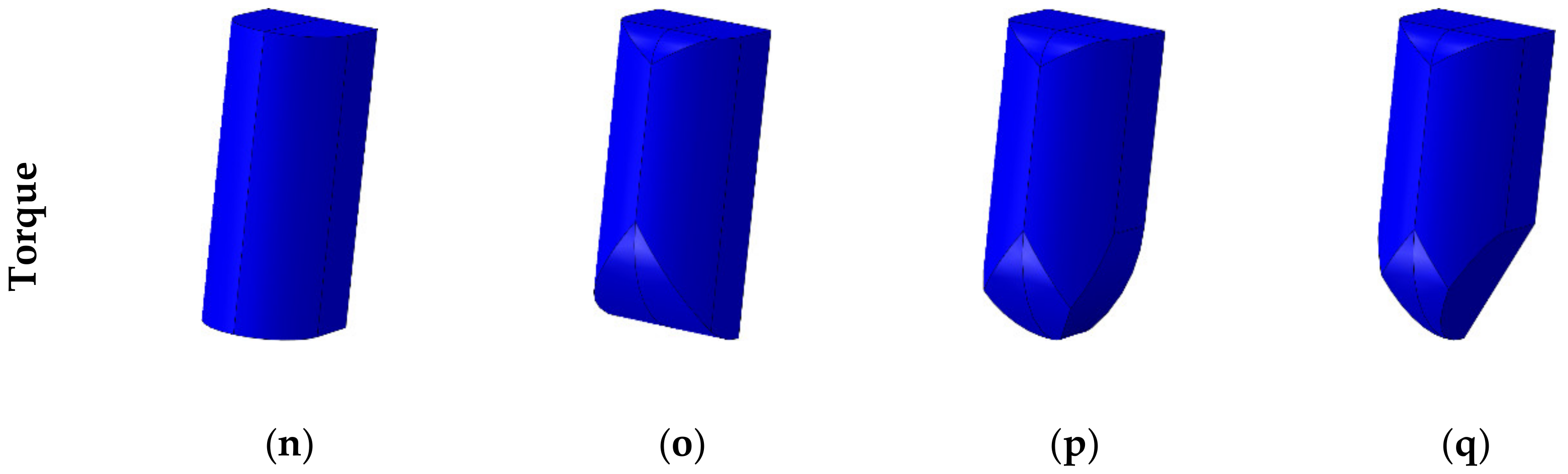
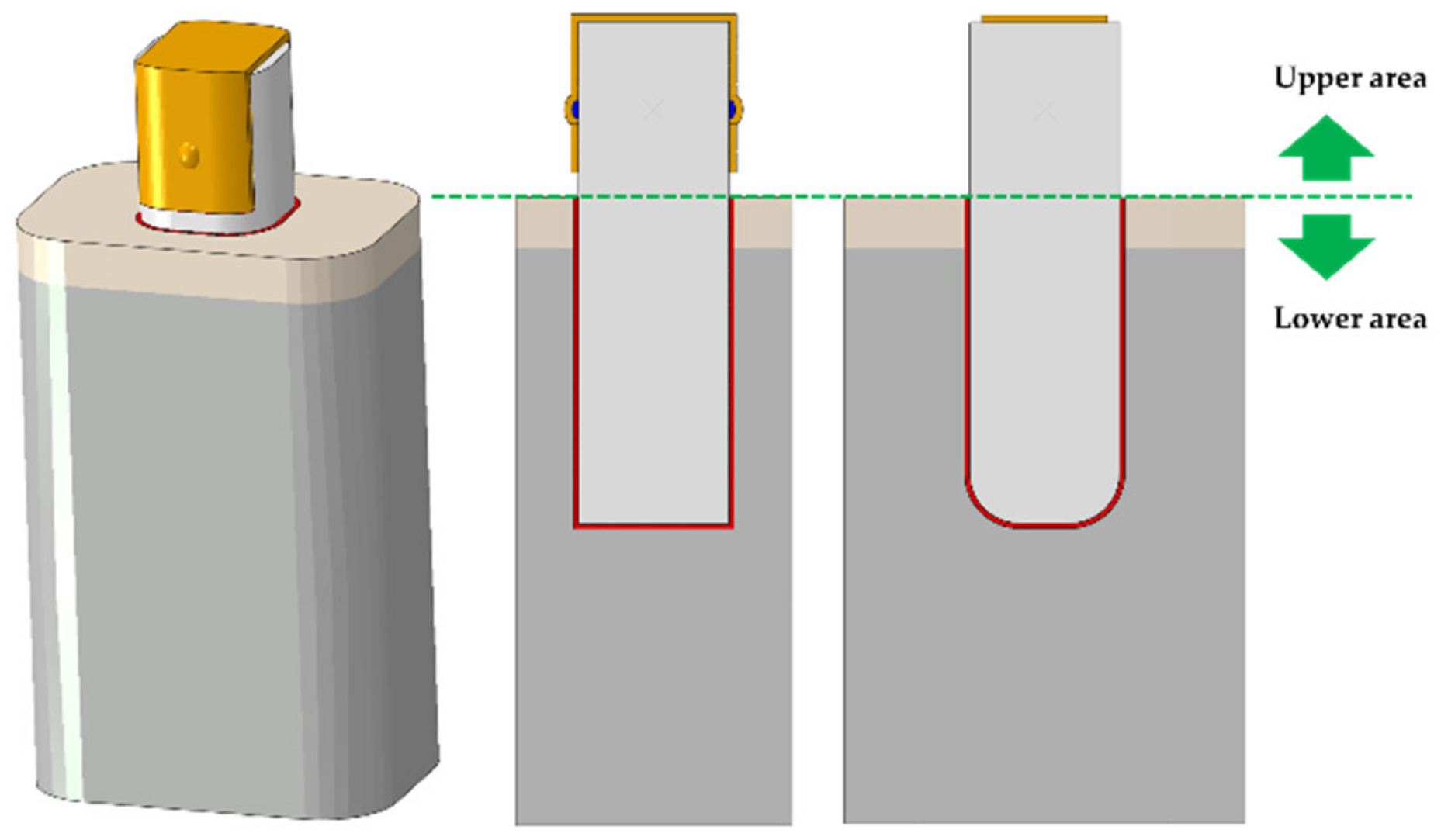
2.1. Designing Attachments for Various Orthodontic Treatment Situations
2.2. Finite Element Analysis for Deriving the Optimum Shape of Attachments for Each Orthodontic Treatment Situations
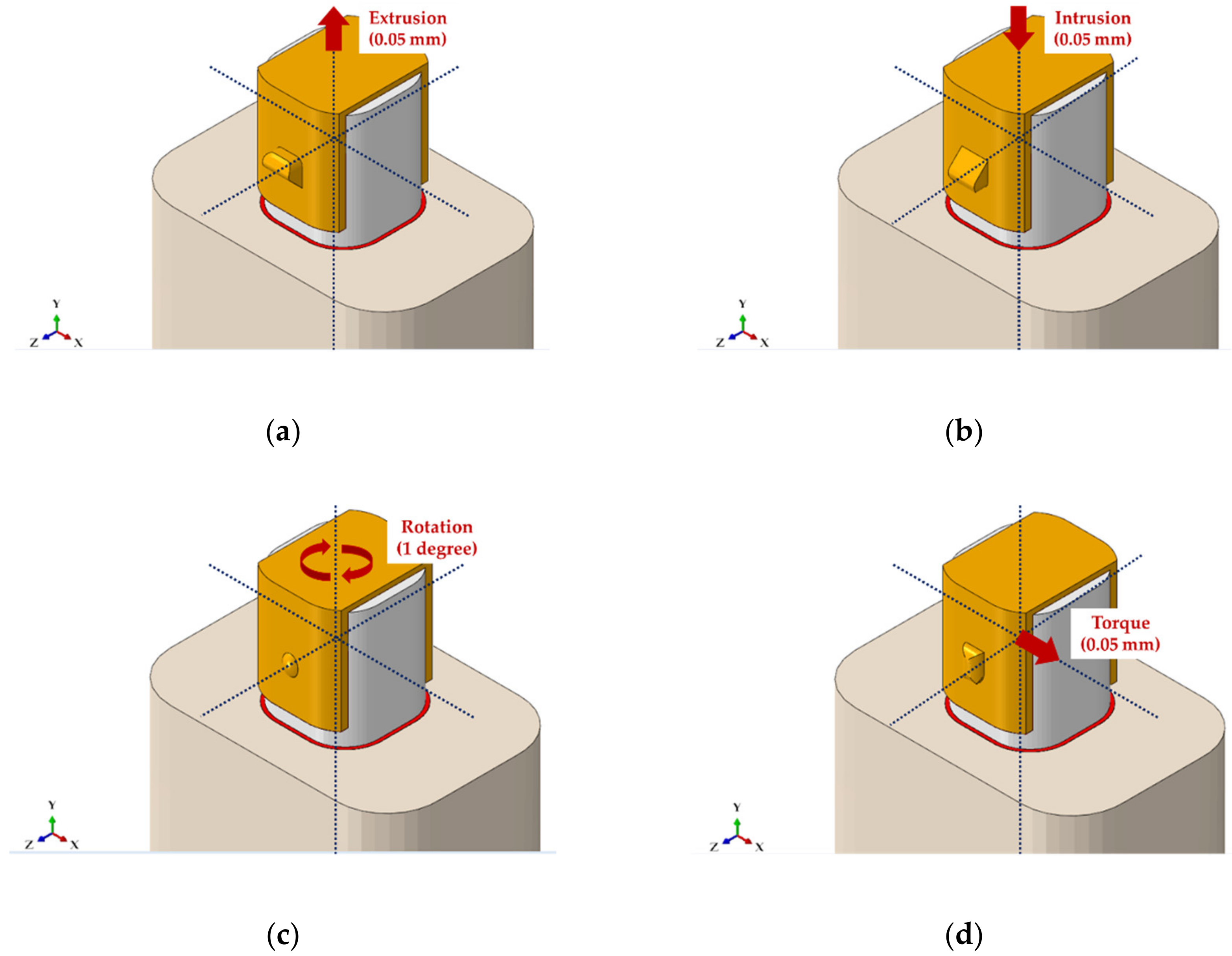
2.3. Constructing a Finite Element Model of the Mandibular Canine Considering Various Attachment Positions for Each Orthodontic Situation
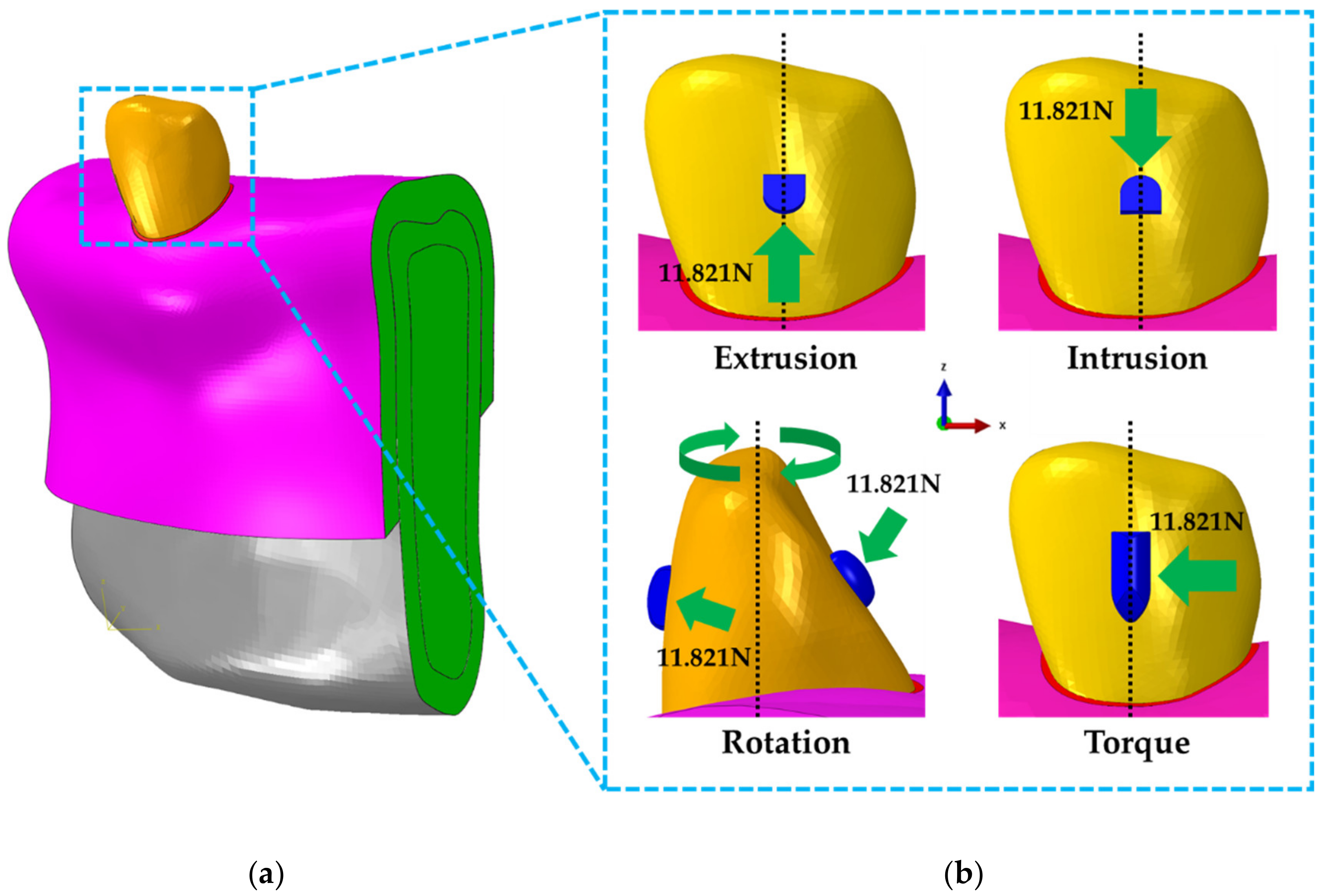
2.4. Contact, Boundary and Loading Conditions of Mandibular Canine Treatment Models
3. Results
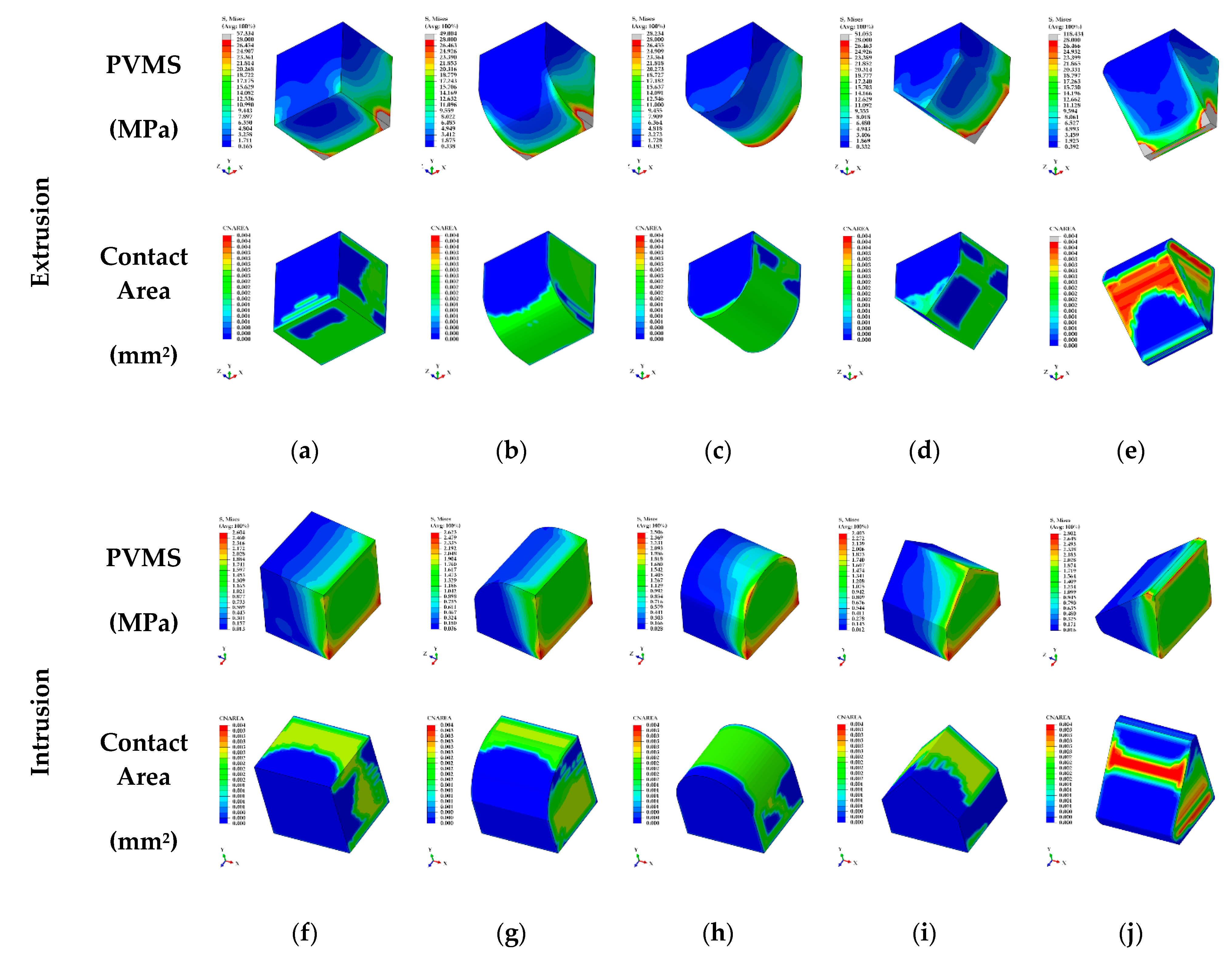
3.1. The Result for Various Shapes of Attachment in Four Orthodontic Treatment Situations
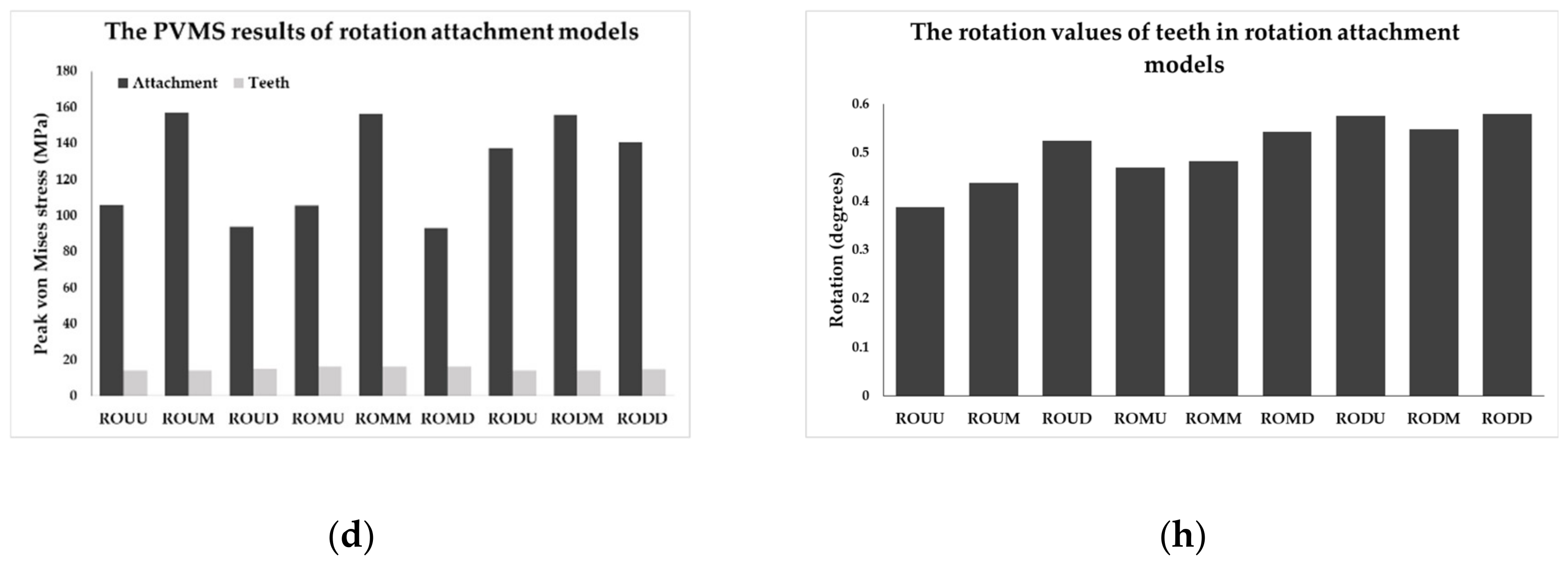
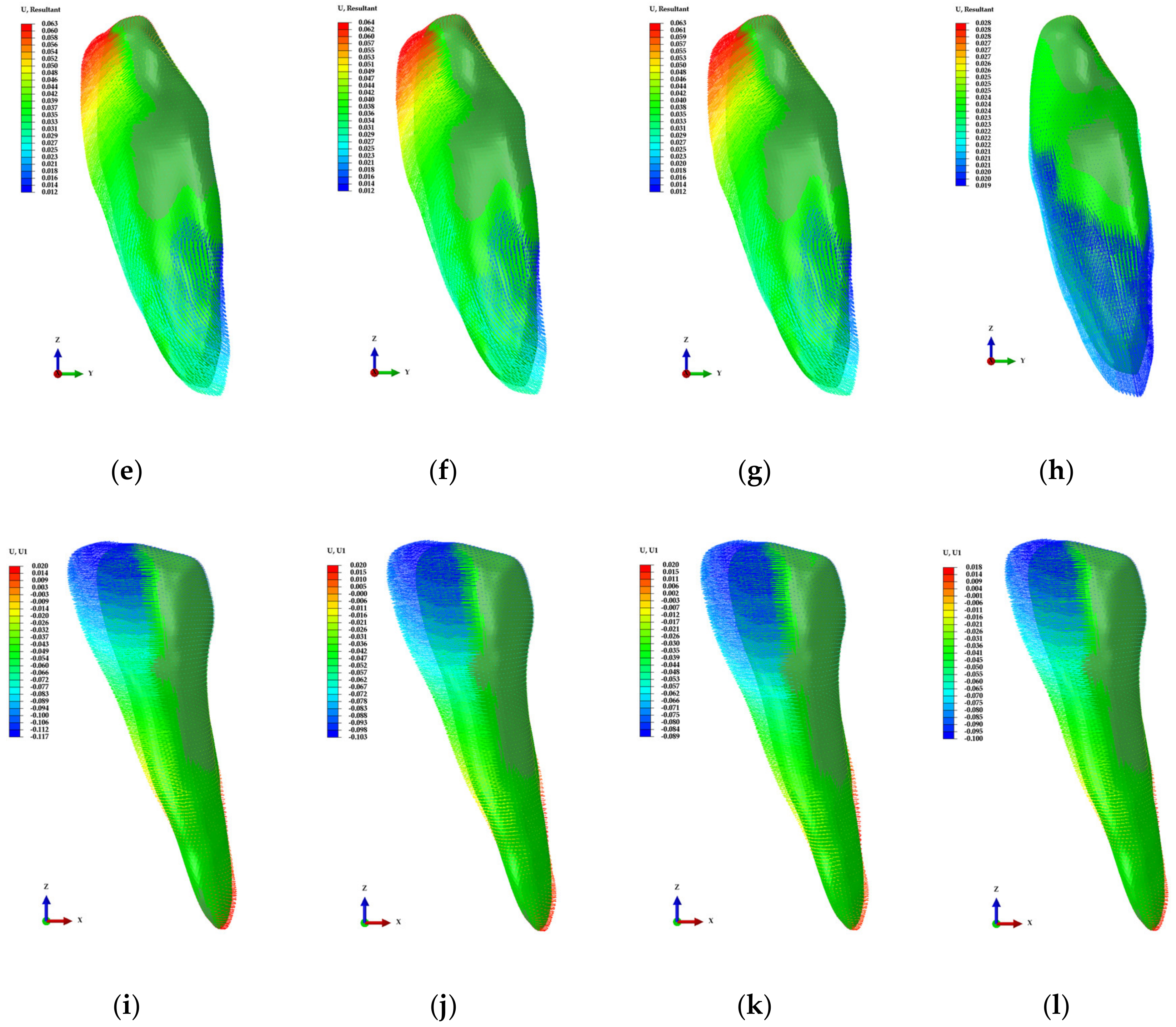
3.2. Results of Finite Element Analysis for Four Teeth Movements to Derive Optimal Attachment Position
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Rapeepattana, S.; Thearmontree, A.; Suntornlohanakul, S. Etiology of Malocclusion and Dominant Orthodontic Problems in Mixed Dentition: A Cross-sectional Study in a Group of Thai Children Aged 8–9 Years. J. Int. Soc. Prev. Community Dent. 2019, 9, 383–389. [Google Scholar] [CrossRef] [PubMed]
- Isola, G.; Anastasi, G.P.; Matarese, G.; Williams, R.C.; Cutroneo, G.; Bracco, P.; Piancino, M.G. Functional and molecular outcomes of the human masticatory muscles. Oral Dis. 2018, 24, 1428–1441. [Google Scholar] [CrossRef] [PubMed]
- Barone, S.; Paoli, A.; Razionale, A.V.; Savignano, R. Computer aided modelling to simulate the biomechanical behaviour of customised orthodontic removable appliances. Int. J. Interact. Des. Manufact. 2016, 10, 387–400. [Google Scholar] [CrossRef]
- Savignano, R.; Barone, S.; Paoli, A.; Razionale, A.V. Advances on Mechanics, Design Engineering and Manufacturing; Springer International Publishing AG: Cham, Switzerland, 2017; pp. 405–414. [Google Scholar] [CrossRef]
- Rosvall, M.D.; Fields, H.W.; Ziuchkovski, J.; Rosenstiel, S.F.; Johnston, W.M. Attractiveness, acceptability, and value of orthodontic appliances. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 276.e1–277. [Google Scholar] [CrossRef] [PubMed]
- Rossini, G.; Parrini, S.; Castroflorio, T.; Deregibus, A.; Debernardi, C.L. Efficacy of clear aligners in controlling orthodontic tooth movement: A systematic review. Angle Orthod. 2015, 85, 881–889. [Google Scholar] [CrossRef]
- Buschang, P.H.; Shaw, S.G.; Ross, M.; Crosby, D.; Campbell, P.M. Comparative time efficiency of aligner therapy and conventional edgewise braces. Angle Orthod. 2014, 84, 391–396. [Google Scholar] [CrossRef]
- Kharbanda, O.P. Orthodontics: Diagnosis of & Management of Malocclusion & Dentofacial Deformities; Elsevier Health Sciences: Amsterdam, The Nederlands, 2019; pp. 405–435. [Google Scholar]
- Eissa, O.; Carlyle, T.; El-Bialy, T. Evaluation of root length following treatment with clear aligners and two different fixed orthodontic appliances. A pilot study. J. Orthod. Sci. 2018, 7, 11–16. [Google Scholar] [CrossRef]
- Cai, Y.; He, B.; Yang, X.; Yao, J. Optimization of configuration of attachment in tooth translation with transparent tooth correction by appropriate moment-to-force ratios: Biomechanical analysis. Biomed. Mater. Eng. 2015, 26, 507–517. [Google Scholar] [CrossRef]
- Joffe, L. Current products and practice invisalign: Early experiences. J. Orthodont. 2003, 30, 348–352. [Google Scholar] [CrossRef]
- Haouili, N.; Kravitz, N.D.; Nikhilesh, R.V.; Ferguson, D.J.; Makki, L. Has Invisalign improved? A prospective follow-up study on the efficancy of tooth movement with invisalign. Am. J. Orthod. Dentofac. Orthop. 2020, in press. [Google Scholar] [CrossRef]
- Boyd, R.L. Surgical-orthodontic treatment of two skeletal Class III patients with Invisalign and fixed appliances. J. Clin. Orthod. 2005, 39, 245–258. [Google Scholar] [PubMed]
- Vlaskalic, V.; Boyd, R. Orthodontic treatment of a mildly crowded malocclusion using the Invisalign System. Aust. Orthod. J. 2001, 17, 41–46. [Google Scholar] [PubMed]
- Graber, L.W.; Vanarsdall, R.L.; Vig, K.W.L. Orthodontics: Current Principles and Techniques; Elsevier/Mosby: St. Louis, MO, USA, 2012; pp. 813–818. [Google Scholar]
- Chang, P.K.; Chen, Y.C.; Huang, C.C.; Lu, W.H.; Chen, Y.C.; Tsai, H.H. Distribution of micromotion in implants and alveolar bone with different thread profiles in immediate loading: A finite element study. Int. J. Oral Maxillofac. Implant. 2012, 27, e96–e101. [Google Scholar]
- Maurer, P.; Holweg, S.; Knoll, W.D.; Schubert, J. Study by finite element method of the mechanical stress of selected biodegradable osteosynthesis screws in sagittal ramus osteotomy. Br. J. Oral Maxillofac. Surg. 2002, 40, 76–83. [Google Scholar] [CrossRef] [PubMed]
- Eraslan, O.; Inan, O. The effect of thread design on stress distribution in a solid screw implant: A 3D finite element analysis. Clin. Oral Investig. 2010, 14, 411–416. [Google Scholar] [CrossRef]
- Gomez, J.P.; Peña, F.M.; Martínez, V.; Giraldo, D.C.; Cardona, C.I. Initial force systems during bodily tooth movement with plastic aligners and composite attachments: A three-dimensional finite element analysis. Angle Orthod. 2015, 85, 454–460. [Google Scholar] [CrossRef]
- Kim, W.H.; Song, E.S.; Ju, K.W.; Lee, J.-H.; Kim, M.Y.; Lim, D.; Kim, B. Finite Element Analysis of Novel Separable Fixture for Easy Retrievement in Case with Peri-Implantitis. Materials 2019, 12, 235. [Google Scholar] [CrossRef]
- Kim, W.H.; Lee, J.-C.; Lim, D.; Heo, Y.-K.; Song, E.-S.; Lim, Y.-J.; Kim, B. Optimized Dental Implant Fixture Design for the Desirable Stress Distribution in the Surrounding Bone Region: A Biomechanical Analysis. Materials 2019, 12, 2749. [Google Scholar] [CrossRef]
- Chen, X.; Mao, B.; Zhu, Z.; Yu, J.; Lu, Y.; Zhang, Q.; Yue, L.; Yu, H. A three-dimensional finite element analysis of mechanical function for 4 removable partial denture designs with 3 framework materials: CoCr, Ti-6Al-4V alloy and PEEK. Sci. Rep. 2019, 9, 13975. [Google Scholar] [CrossRef]
- Savignano, R.; Valentino, R.; Razionale, A.V.; Michelotti, A.; Barone, S.; D’Antò, V. Biomechanical Effects of Different Auxiliary-Aligner Designs for the Extrusion of an Upper Central Incisor: A Finite Element Analysis. J. Healthc. Eng. 2019, 2019, 9687127. [Google Scholar] [CrossRef]
- Wei, Z.; Yu, X.; Xu, X.; Chen, X. Experiment and hydro-mechanical coupling simulation study on the human periodontal ligament. Comput. Methods Programs Biomed. 2014, 113, 749–756. [Google Scholar] [CrossRef] [PubMed]
- Li, W. Biomechanics of infarcted left ventricle: A review of modelling. Biomed. Eng. Lett. 2020. [Google Scholar] [CrossRef]
- Wang, W.; Lynch, J.P. Quantitative assessment of compress-type osseointegrated prosthetic implants in human bone using electromechanical impedance spectroscopic methods. Biomed. Eng. Lett. 2020, 10, 129–147. [Google Scholar] [CrossRef] [PubMed]
- Baek, J.W.; Park, S.J. Finite element analysis of cornea deformation and curvature change during the keratoplasty suturing process. Biomed. Eng. Lett. 2019, 9, 203–209. [Google Scholar] [CrossRef] [PubMed]
- Shash, M.; Nazha, H.; Abbas, W. Influence of different abutment designs on the biomechanical behavior of one-piece zirconia dental implants and their surrounding bone: A 3D-FEA. Innov. Res. Biomed. Eng. 2019, 40, 313–319. [Google Scholar] [CrossRef]
- EI-Anwar, M.I.; El-Zawahry, M.M. A three dimensional finite element study on dental implant design. J. Genet. Eng. Biotechnol. 2011, 9, 77–82. [Google Scholar] [CrossRef]
- Wazeh, A.M.; El-Anwar, M.I.; Atia, R.; Mahjari, R.M.; Linga, S.A.; Al-Pakistani, L.; Yousief, S.A. 3D FEA Study On Implant Threading Role on Selection of Implant and Crown Materials. Open Access Maced. J. Med. Sci. 2018, 6, 1702–1706. [Google Scholar] [CrossRef]
- Sim, B.K.; Kim, B.; Kim, M.J.; Jeong, G.H.; Ju, K.W.; Shin, Y.J.; Kim, M.Y.; Lee, J.H. Hollow Abutment Screw Design for Easy Retrieval in Case of Screw Fracture in Dental Implant System. J. Healthc. Eng. 2017, 2017, 4842072. [Google Scholar] [CrossRef]
- Asiry, M.A.; AlShahrani, I. Prevalence of malocclusion among school children of Southern Saudi Arabia. J. Orthod. Sci. 2019, 8, 2. [Google Scholar] [CrossRef]
- Kravitz, N.D.; Kusnoto, B.; BeGole, E.; Obrez, A.; Agran, B. How well does Invisalign work? A prospective clinical study evaluating the efficacy of tooth movement with Invisalign. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 27–35. [Google Scholar] [CrossRef]
- Li, X.; Ren, C.; Wang, Z.; Zhao, P.; Wang, H.; Bai, Y. Changes in force associated with the amount of aligner activation and lingual bodily movement of the maxillary central incisor. Korean J. Orthod. 2016, 46, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Khosravi, R. Biomechanics in lingual orthodontics: What the future holds. Semin. Orthodont. 2018, 24, 363–371. [Google Scholar] [CrossRef]






| Components | Young’s Modulus (MPa) | Poisson’s Ratio |
|---|---|---|
| Cortical bone [18,22] | 13,700 | 0.3 |
| Cancellous bone [18,22] | 1370 | 0.3 |
| Mucosa [22] | 3.45 | 0.45 |
| Teeth [23] | 20,000 | 0.3 |
| RTA [23] | 2050 | 0.3 |
| Attachment [19] | 12,500 | 0.36 |
| Parameters | a1 | u1 | D1 | a2 | u2 | D2 |
|---|---|---|---|---|---|---|
| Value | 2.5 × 10−1 | 5.5429 × 10−3 | 1.216 × 10−1 | 1.153 × 10−1 | 1.107 × 10−1 | 9.701 × 10−1 |
| Types | Peak von Mises Stress (PVMS) | Contact Pressure | ||||
|---|---|---|---|---|---|---|
| Bone | Teeth | PDL | RTA | Attachment | Attachment | |
| EX1 | 0.186 | 10.416 | 0.017 | 12.586 | 57.334 | 49.906 |
| EX2 | 0.189 | 9.992 | 0.017 | 20.667 | 49.004 | 40.363 |
| EX3 | 0.187 | 9.511 | 0.017 | 10.762 | 28.234 | 12.746 |
| EX4 | 0.188 | 13.705 | 0.017 | 22.272 | 51.053 | 36.582 |
| EX5 | 0.147 | 9.823 | 0.014 | 29.890 | 118.434 | 91.215 |
| IN1 | 3.167 | 3.588 | 0.320 | 2.604 | 2.433 | 1.182 |
| IN2 | 3.167 | 3.488 | 0.320 | 2.623 | 2.661 | 1.327 |
| IN3 | 3.166 | 3.472 | 0.320 | 2.506 | 2.569 | 0.682 |
| IN4 | 3.166 | 3.445 | 0.320 | 2.405 | 2.559 | 1.863 |
| IN5 | 3.167 | 3.445 | 0.320 | 2.802 | 2.562 | 2.546 |
| RO1 | 1.313 | 12.879 | 0.193 | 19.249 | 54.871 | 66.340 |
| RO2 | 1.314 | 10.672 | 0.193 | 18.707 | 49.115 | 50.932 |
| RO3 | 1.310 | 13.059 | 0.193 | 15.017 | 51.801 | 55.853 |
| TO1 | 4.261 | 228.027 | 0.377 | 54.811 | 56.818 | 52.346 |
| TO2 | 4.263 | 231.072 | 0.377 | 78.367 | 66.138 | 32.871 |
| TO3 | 4.705 | 110.484 | 0.403 | 61.892 | 42.228 | 35.769 |
| TO4 | 4.707 | 112.692 | 0.403 | 68.947 | 119.961 | 1515.150 |
| Types | Teeth | Attachment | |||
|---|---|---|---|---|---|
| Upper Region | Lower Region | Total Area | Contact Area | Contact Rate | |
| EX1 | 3.236 µm | 3.068 µm | 2.55 mm2 | 1.57 mm2 | 61.57% |
| EX2 | 3.273 µm | 3.101 µm | 2.63 mm2 | 2.05 mm2 | 77.95% |
| EX3 | 3.271 µm | 3.075 µm | 2.19 mm2 | 1.81 mm2 | 82.65% |
| EX4 | 3.267 µm | 3.079 µm | 2.05 mm2 | 1.15 mm2 | 56.10% |
| EX5 | 2.643 µm | 2.492 µm | 2.21 mm2 | 1.64 mm2 | 74.21% |
| IN1 | 48.887 µm | 47.755 µm | 2.55 mm2 | 1.34 mm2 | 52.55% |
| IN2 | 48.913 µm | 47.750 µm | 2.63 mm2 | 1.52 mm2 | 57.79% |
| IN3 | 48.890 µm | 47.747 µm | 2.19 mm2 | 1.46 mm2 | 66.67% |
| IN4 | 48.868 µm | 47.744 µm | 2.05 mm2 | 0.75 mm2 | 36.59% |
| IN5 | 48.884 µm | 47.747 µm | 2.21 mm2 | 1.15 mm2 | 52.04% |
| RO1 | 0.889 degrees | 0.857 degrees | 0.54 mm2 | 0.22 mm2 | 40.74% |
| RO2 | 0.890 degrees | 0.858 degrees | 0.52 mm2 | 0.21 mm2 | 40.38% |
| RO3 | 0.887 degrees | 0.856 degrees | 0.48 mm2 | 0.19 mm2 | 39.58% |
| TO1 | 59.442 µm | 35.753 µm | 1.83 mm2 | 0.52 mm2 | 28.42% |
| TO2 | 59.463 µm | 35.764 µm | 1.66 mm2 | 0.53 mm2 | 31.93% |
| TO3 | 58.114 µm | 35.115 µm | 1.54 mm2 | 0.72 mm2 | 46.75% |
| TO4 | 58.116 µm | 35.111 µm | 1.51 mm2 | 0.71 mm2 | 47.02% |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, W.-H.; Hong, K.; Lim, D.; Lee, J.-H.; Jung, Y.J.; Kim, B. Optimal Position of Attachment for Removable Thermoplastic Aligner on the Lower Canine Using Finite Element Analysis. Materials 2020, 13, 3369. https://doi.org/10.3390/ma13153369
Kim W-H, Hong K, Lim D, Lee J-H, Jung YJ, Kim B. Optimal Position of Attachment for Removable Thermoplastic Aligner on the Lower Canine Using Finite Element Analysis. Materials. 2020; 13(15):3369. https://doi.org/10.3390/ma13153369
Chicago/Turabian StyleKim, Won-Hyeon, Kyoungjae Hong, Dohyung Lim, Jong-Ho Lee, Yu Jin Jung, and Bongju Kim. 2020. "Optimal Position of Attachment for Removable Thermoplastic Aligner on the Lower Canine Using Finite Element Analysis" Materials 13, no. 15: 3369. https://doi.org/10.3390/ma13153369
APA StyleKim, W.-H., Hong, K., Lim, D., Lee, J.-H., Jung, Y. J., & Kim, B. (2020). Optimal Position of Attachment for Removable Thermoplastic Aligner on the Lower Canine Using Finite Element Analysis. Materials, 13(15), 3369. https://doi.org/10.3390/ma13153369







