Are Metal-Free Monolithic Crowns the Present of Prosthesis? Study of Mechanical Behaviour
Abstract
1. Introduction
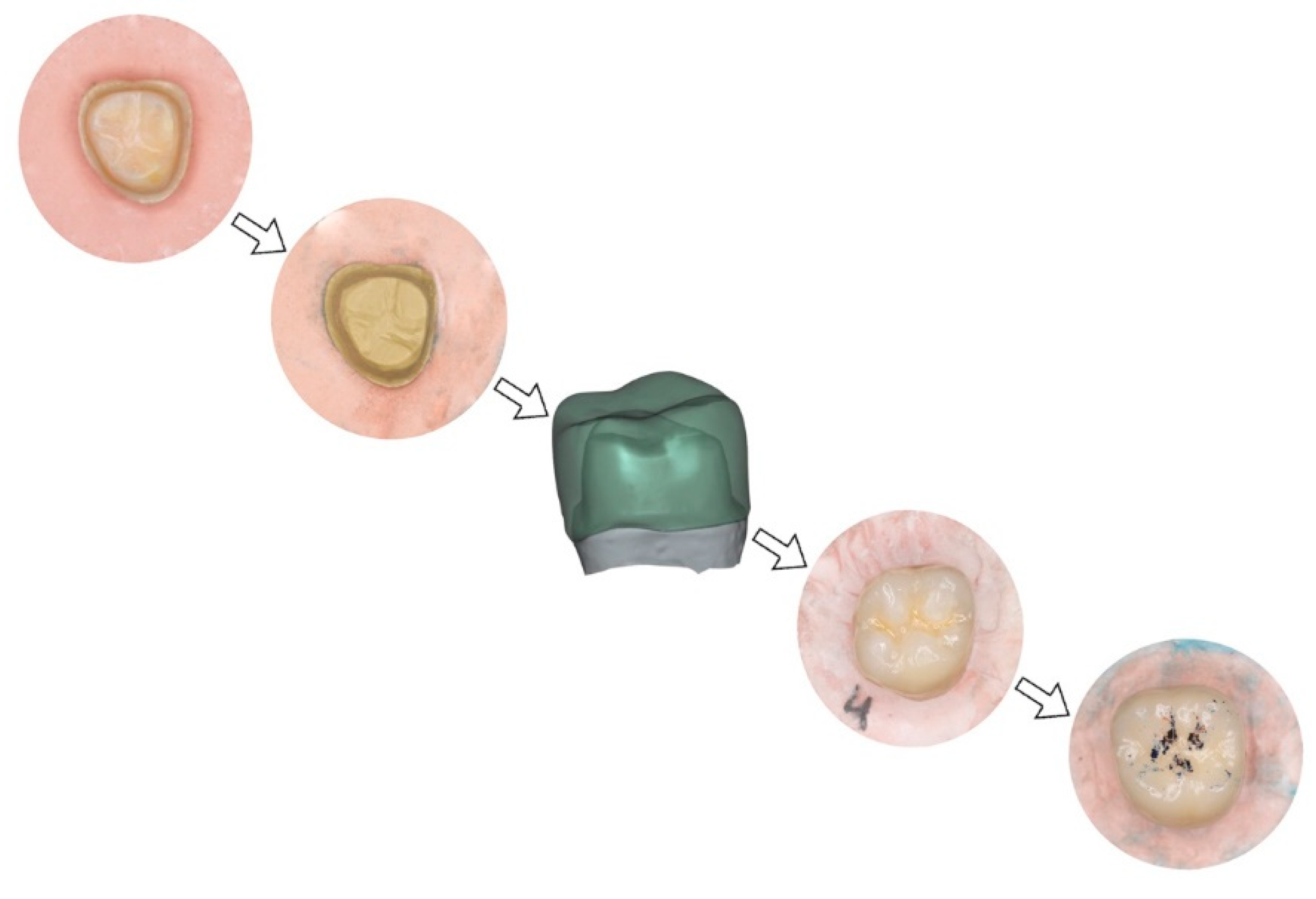
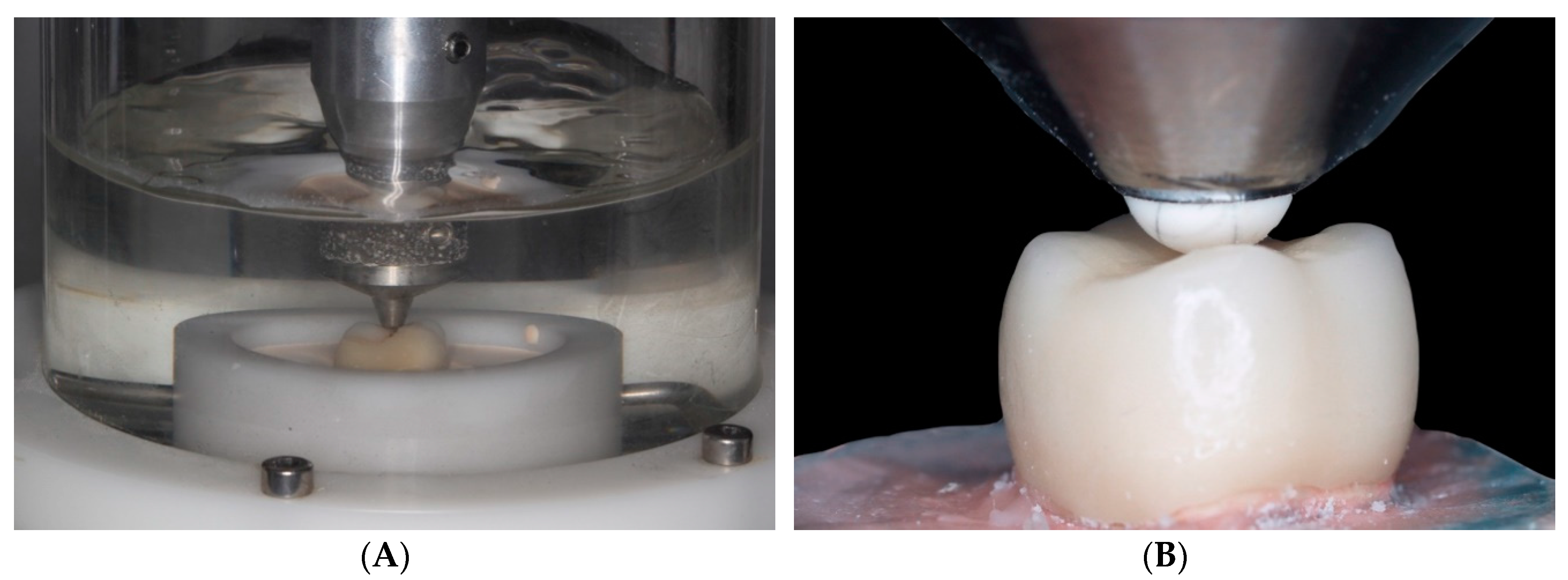
2. Material and Methods
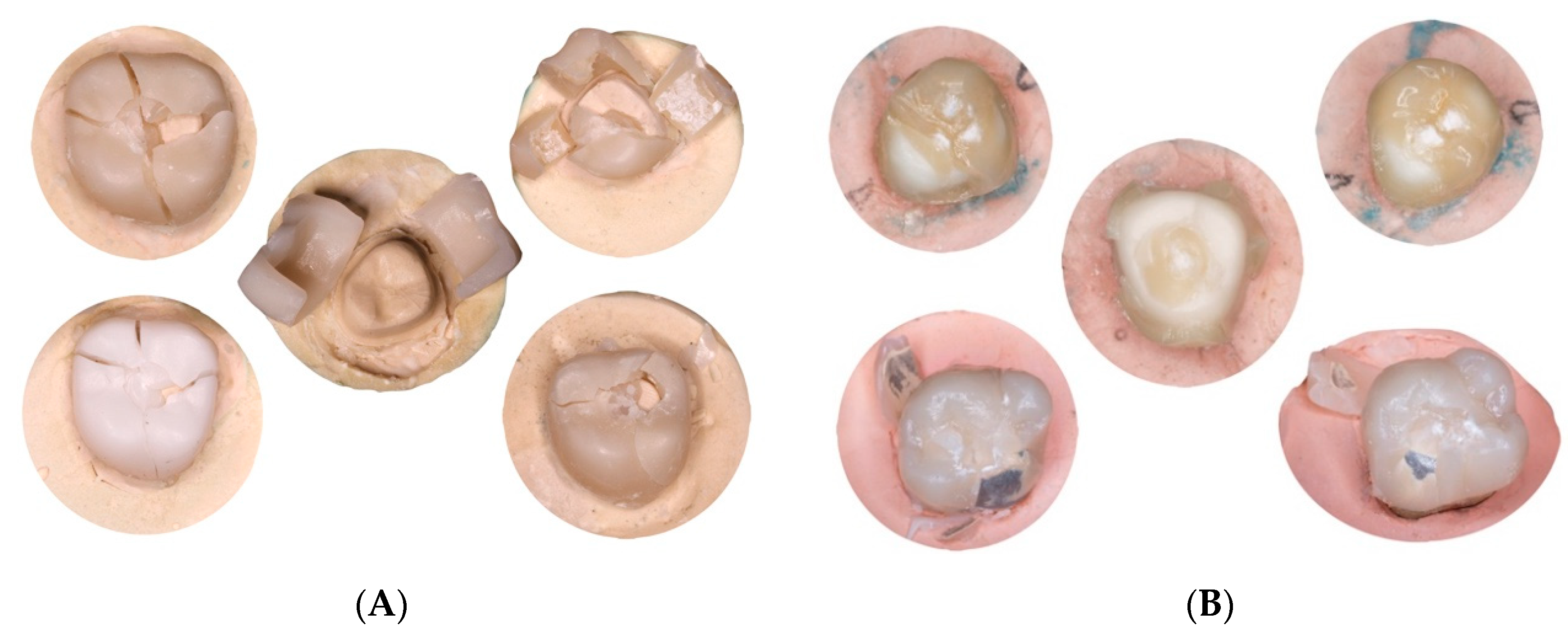
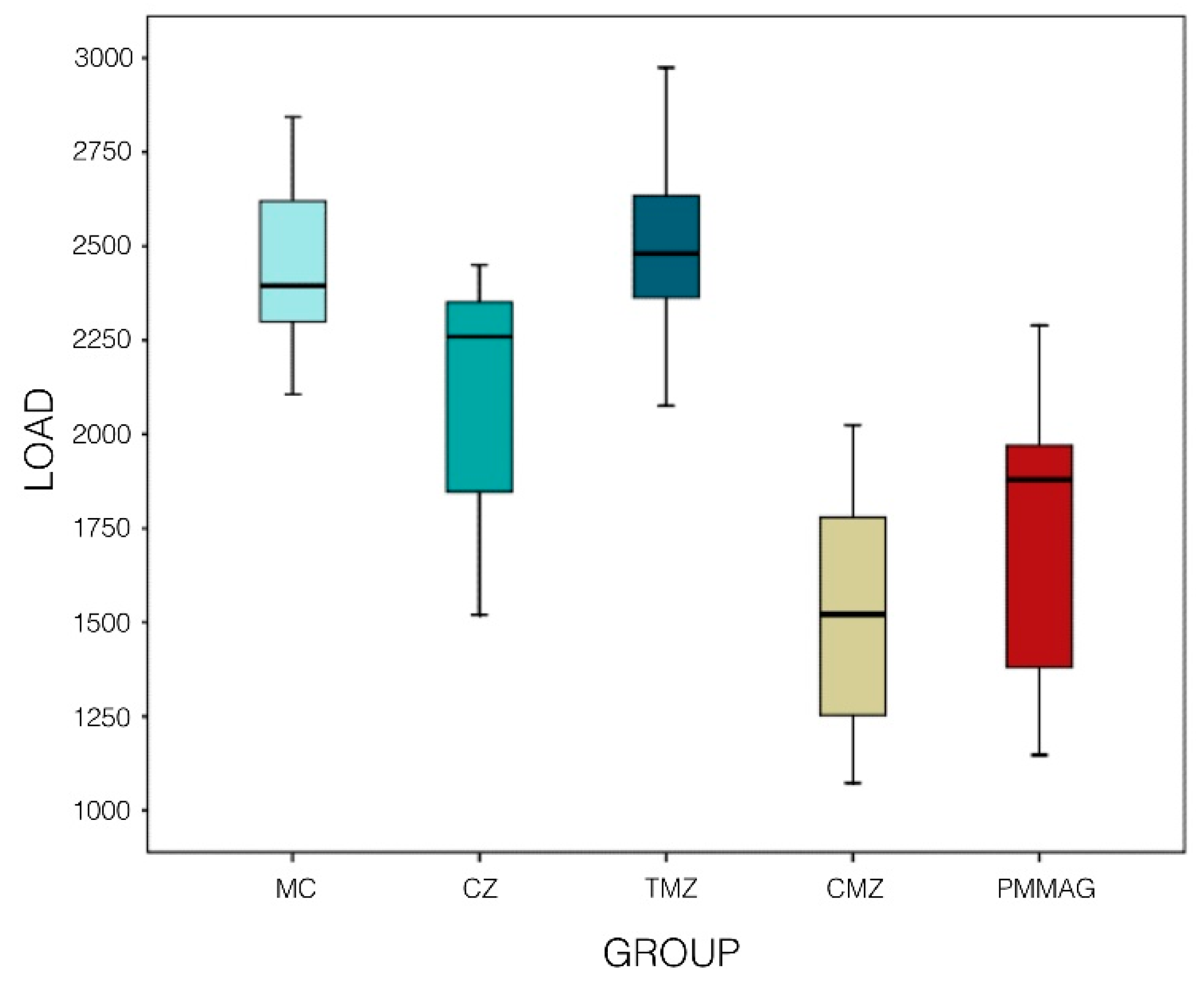
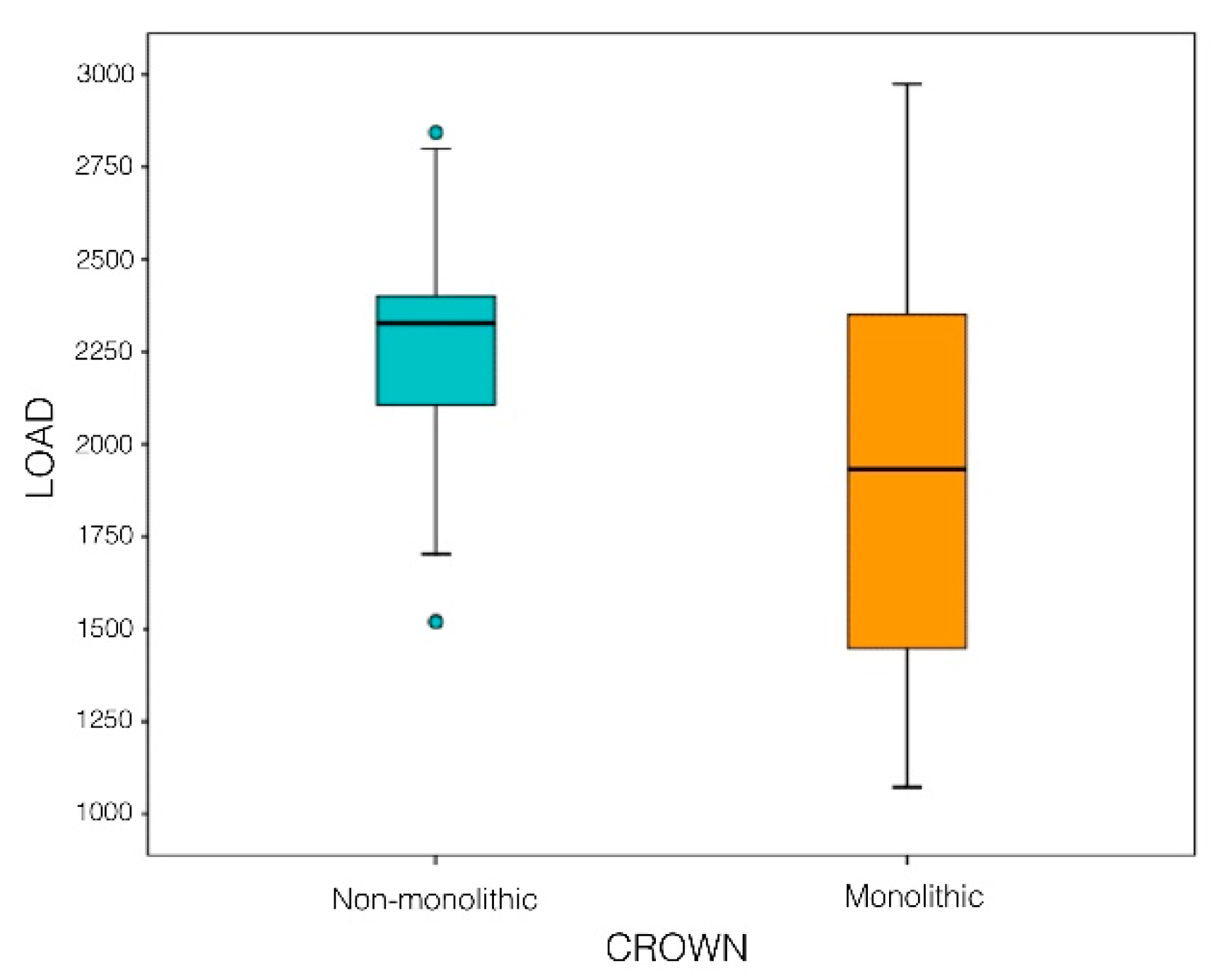
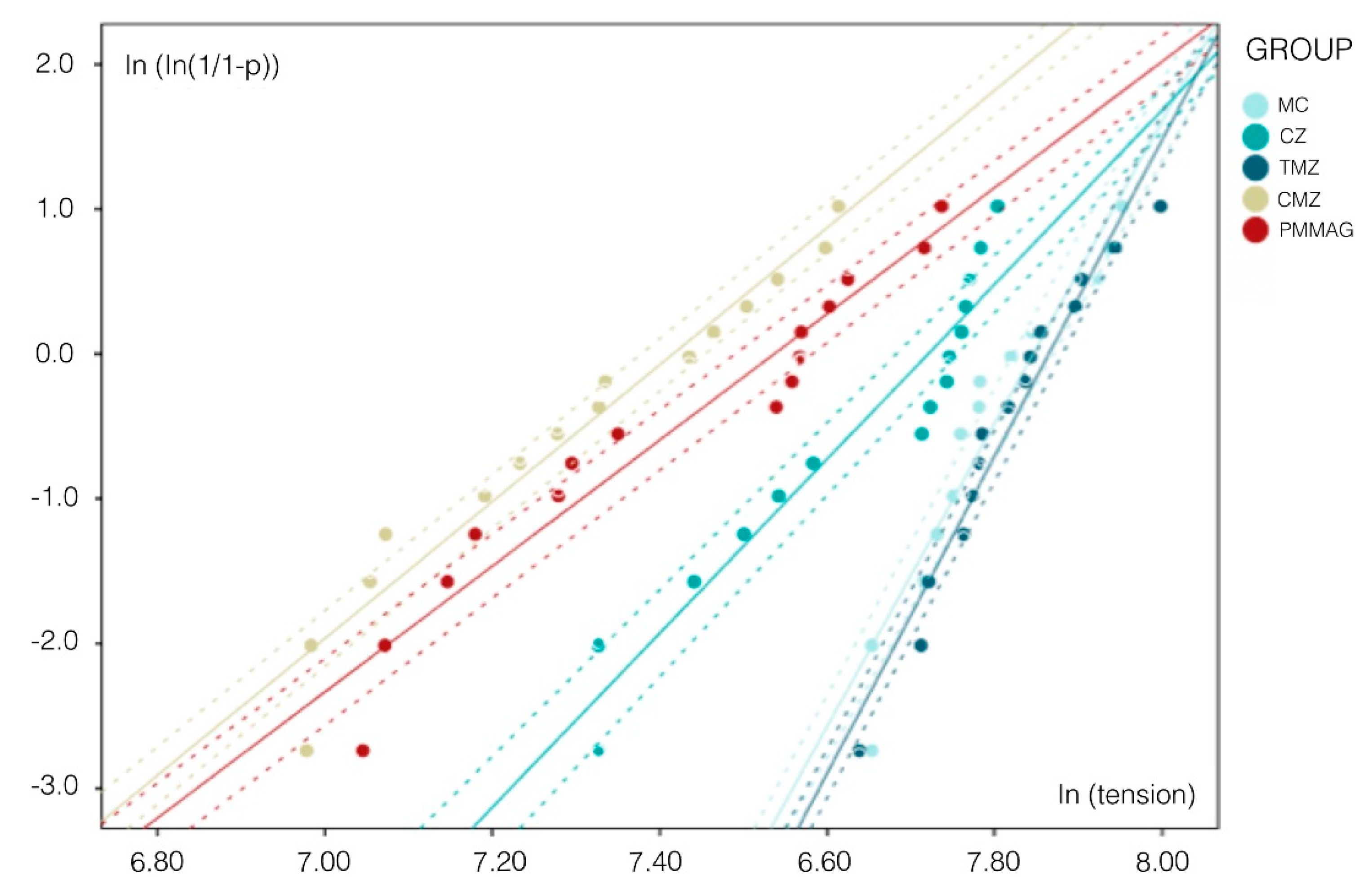
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Sailer, I.; Pjetursson, B.E.; Zwahlen, M.; Hämmerle, C.H. A systematic review of the survival and complication rates of all-ceramic and metal-ceramic reconstructions after an observation period of at least 3 years. Part II: Fixed dental prostheses. Clin. Oral Implant. Res. 2007, 18, 86–96. [Google Scholar] [CrossRef] [PubMed]
- López-Suárez, C.; Castillo-Oyagüe, R.; Rodriguez-Alonso, V.; Lynch, C.D.; Súarez-García, M.J. Fracture load of metal-ceramic, monolithic, and bi-layered zirconia-based posterior fixed dental prostheses after thermo-mechanical cycling. J. Dent. 2018, 73, 97–104. [Google Scholar] [CrossRef] [PubMed]
- Agustín-Panadero, R.; Fons-Font, A.; Román-Rodriguez, J.L.; Granell-Ruiz, M.; Rio-Highsmith, J.; Solá-Ruiz, M.F. Zirconia Versus Metal: A Preliminary Comparative Analysis of Ceramic Veneer Behavior. Int. J. Prosthodont. 2012, 25, 294–300. [Google Scholar]
- Sun, T.; Zhou, S.; Lai, R.; Liu, R.; Ma, S.; Zhou, Z.; Longquan, S. Load-bearing capacity and the recommended thickness of dental monolithic zirconia single crowns. J. Mech. Behav. Biomed. Mater. 2014, 35, 93–101. [Google Scholar] [CrossRef]
- Sailer, I.; Balmer, M.; Hüsler, J.; Hämmerle, C.H.F.; Känel, S.; Thoma, D.S. 10-year randomized trial (RCT) of zirconia ceramic and metal-ceramic fixed dental prostheses. J. Dent. 2018, 76, 32–39. [Google Scholar] [CrossRef]
- Edelhoff, D.; Florian, B.; Florian, W.; Johnen, C. HIP-zirconia fixed partial denture. Clinical results after 3 years of clinical service. Quintessence Int. 2008, 39, 459–471. [Google Scholar]
- Tsalouchou, E.; Cattell, M.; Knowles, J.; Pittayachawan, P.; McDonald, A. Fatigue and fracture properties of yttria partially stabilized zirconia crown systems. Dent. Mater. 2008, 24, 308–318. [Google Scholar] [CrossRef]
- López-Suarez, C.; Rodriguez, V.; Pelaez, J.; Agustin-Panadero, R.; Suarez, M.J. Comparative fracture behavior of monolithic and veneered zirconia posterior fixed dental prostheses. Dent. Mater. 2017, 36, 816–821. [Google Scholar] [CrossRef]
- Rinke, S.; Fischer, C. Range of indications for translucent zirconia modifications: Clinical and technical aspects. Quintessence Int. 2013, 44, 557–566. [Google Scholar]
- Mori, K. Influence of the design of zirconia framework on the fracture strength of veneering porcelain. Kokubyo Gakkai Zasshi 2010, 77, 67–70. [Google Scholar]
- López-Suarez, C.; Tobar, C.; Sola-Ruiz, M.F.; Pelaez, J.; Suarez, M.J. Effect of thermomechanical and static loading on the load to fracture of metal-ceramic, monolithic, and veneered zirconia posterior fixed partial dentures. J. Prosthodont. 2019, 28, 171–178. [Google Scholar] [CrossRef] [PubMed]
- Lawson, N.; Jurado, C.; Huang, C.; Morris, G.; Burgess, J.; Liu, P. Effect of surface treatment and cement on fracture load of traditional zirconia (3Y), translucent zirconia (5Y) and lithium disilicate crowns. J. Prosthodont. 2019, 28, 659–665. [Google Scholar] [CrossRef] [PubMed]
- Camposilvan, E.; Leonec, R.; Gremillarda, L.; Sorrentinoc, R.; Zaronec, F.; Ferrarid, M.; Chevaliera, J. Aging resistance, mechanical properties and translucency of different yttria stabilized zirconia ceramics for monolithic dental crown applications. Dent. Mater. 2018, 34, 879–890. [Google Scholar] [CrossRef] [PubMed]
- Bindl, A.; Lüthy, H.; Mörmann, H. Thin-wall ceramic CAD/CAM crown copings: Strength hand fracture pattern. J. Oral Rehabil. 2006, 33, 520–528. [Google Scholar] [CrossRef] [PubMed]
- Avezedo, L.; Antonaya, J.L.; Molinero, P.; Rio-Highsmith, J. Improving PMMA resin using graphene oxide for a definitive prosthodontic rehabilitation—A clinical report. J. Clin. Exp. Dent. 2019, 11, 70–74. [Google Scholar]
- Habib, S.R.; Otaibi, A.K.A.; Anazi, T.A.A.; Anazi, S.M.A. Evaluation of thickness of CAD/CAM fabricated zirconia cores by digital microscope. Technol. Health Care 2018, 26, 181–185. [Google Scholar] [CrossRef]
- Rodrigues, S.B.; Franken, P.; Celeste, R.K.; Leitune, V.C.B.; Collares, F.M. CAD/CAM or conventional ceramic materials restorations longevity: A systematic review and meta-analysis. J. Prosthodont. Res. 2019, 63, 389–395. [Google Scholar] [CrossRef]
- Sulaiman, T.A.; Abdulmajeed, A.; Donovan, T.E.; Ritter, A.V.; Vallittu, P.K.; Närhi, T.O. Optical properties and light irradiance of monolithic zirconia at variable thicknesses. Dent. Mater. 2015, 31, 1180–1187. [Google Scholar] [CrossRef]
- Shillingburg, H.T.; Hobo, S.; Fisher, D.W. Preparation design and margin distortion in porcelain-fused-to-metal restorations. J. Prosthet. Dent. 1973, 89, 527–532. [Google Scholar] [CrossRef]
- Quinn, J.; Quinn, G. A practical and systematic review of Weibull statistics for reporting strengths of dental materials. Dent. Mater. 2010, 26, 135–147. [Google Scholar] [CrossRef]
- Yin, R.; Kim, Y.K.; Jang, Y.S.; Lee, J.J.; Lee, M.H.; Bae, T.S. Comparative evaluation of the mechanical properties of CAD/CAM dental blocks. Odontology 2019, 107, 360–367. [Google Scholar] [CrossRef] [PubMed]
- De Boever, J.A.; McCall, W.D.; Holden, S. Functional occlusal forces: An investigation by telemetry. J. Prosthet. Dent. 1978, 40, 326–333. [Google Scholar] [CrossRef]
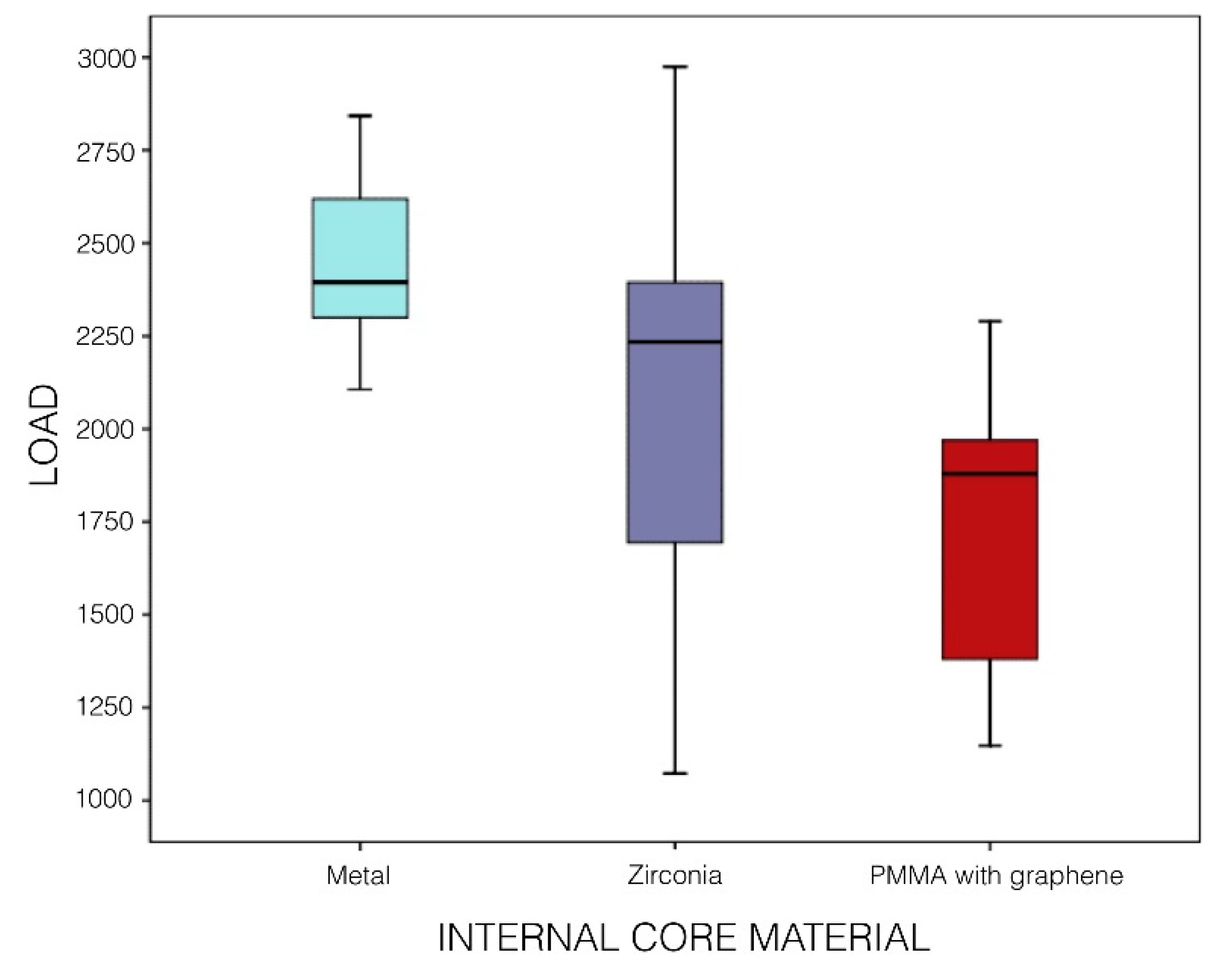
| Specimens | Metal-Ceramic | Zirconia-Ceramic | Tetragonal Monolithic Zirconia | Cubic Monolithic Zirconia | Polymethyl Methacrylate (PMMA) Doped with Graphene Nanoparticles |
|---|---|---|---|---|---|
| 1 | 2685.87 N | 2236.254 N | 2394.835 N | 1384.274 N | 1449.108 N |
| 2 | 2488.602 N | 2399.993 N | 2688.01 N | 1882.76 N | 1312.192 N |
| 3 | 2842.947 N | 2345.123 N | 2376.143 N | 1532.125 N | 2289.915 N |
| 4 | 2395.1 N | 1808.736 N | 2532.037 N | 1179.266 N | 1937.071 N |
| 5 | 2553.012 N | 2259.367 N | 2234.173 N | 1072.836 N | 1555.745 N |
| 6 | 2106.848 N | 1964.957 N | 2547.455 N | 1520.888 N | 1147.493 N |
| 7 | 2332.87 N | 2310.984 N | 2255.185 N | 1157.506 N | 2002.78 N |
| 8 | 2277.845 N | 1885.435 N | 2579.959 N | 1744.477 N | 1472.441 N |
| 9 | 2761.99 N | 1520.135 N | 2075.45 N | 1447.455 N | 2242.947 N |
| 10 | 2397.889 N | 2365.786 N | 2480.427 N | 1993.116 N | 1177.994 N |
| 11 | 2106.443 N | 2304.045 N | 2404.181 N | 1694.028 N | 1933.257 N |
| 12 | 2798.884 N | 2449.68 N | 2974.749 N | 1327.419 N | 1879.851 N |
| 13 | 2240.876 N | 1704.029 N | 2818.966 N | 1078.637 N | 1915.503 N |
| 14 | 2342.765 N | 1520.135 N | 2350.442 N | 1814.381 N | 2047.491 N |
| 15 | 2321.767 N | 2356.276 N | 2707.736 N | 2024.667 N | 1269.293 N |
| Mean | 2443.58 N | 2095.39 N | 2494.64 N | 1523.58 N | 1708.87 N |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Agustín-Panadero, R.; León Martínez, R.; Solá-Ruíz, M.F.; Fons-Font, A.; García Engra, G.; Fernández-Estevan, L. Are Metal-Free Monolithic Crowns the Present of Prosthesis? Study of Mechanical Behaviour. Materials 2019, 12, 3663. https://doi.org/10.3390/ma12223663
Agustín-Panadero R, León Martínez R, Solá-Ruíz MF, Fons-Font A, García Engra G, Fernández-Estevan L. Are Metal-Free Monolithic Crowns the Present of Prosthesis? Study of Mechanical Behaviour. Materials. 2019; 12(22):3663. https://doi.org/10.3390/ma12223663
Chicago/Turabian StyleAgustín-Panadero, Rubén, Raquel León Martínez, María Fernanda Solá-Ruíz, Antonio Fons-Font, Georgina García Engra, and Lucía Fernández-Estevan. 2019. "Are Metal-Free Monolithic Crowns the Present of Prosthesis? Study of Mechanical Behaviour" Materials 12, no. 22: 3663. https://doi.org/10.3390/ma12223663
APA StyleAgustín-Panadero, R., León Martínez, R., Solá-Ruíz, M. F., Fons-Font, A., García Engra, G., & Fernández-Estevan, L. (2019). Are Metal-Free Monolithic Crowns the Present of Prosthesis? Study of Mechanical Behaviour. Materials, 12(22), 3663. https://doi.org/10.3390/ma12223663







