Effect of Dentin Bonding Agents, Various Resin Composites and Curing Modes on Bond Strength to Human Dentin
Abstract
1. Introduction
- One-step adhesive systems show comparable bond strengths to multi-step adhesive systems.
- Flowable resin composites, universal resin composites and bulk-fill resin composites produce almost equal bond strengths.
- The curing program has no impact on bond strengths.
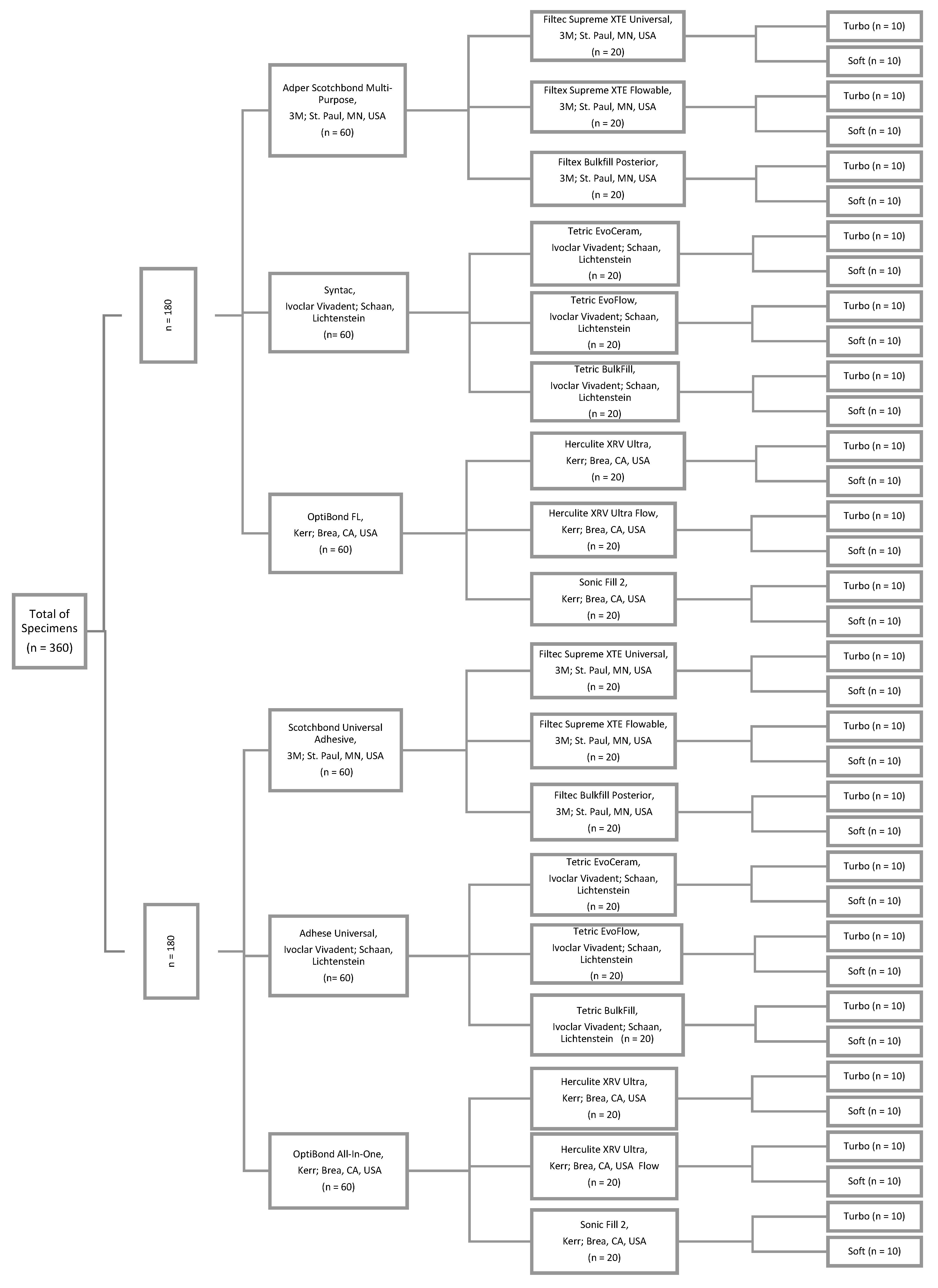
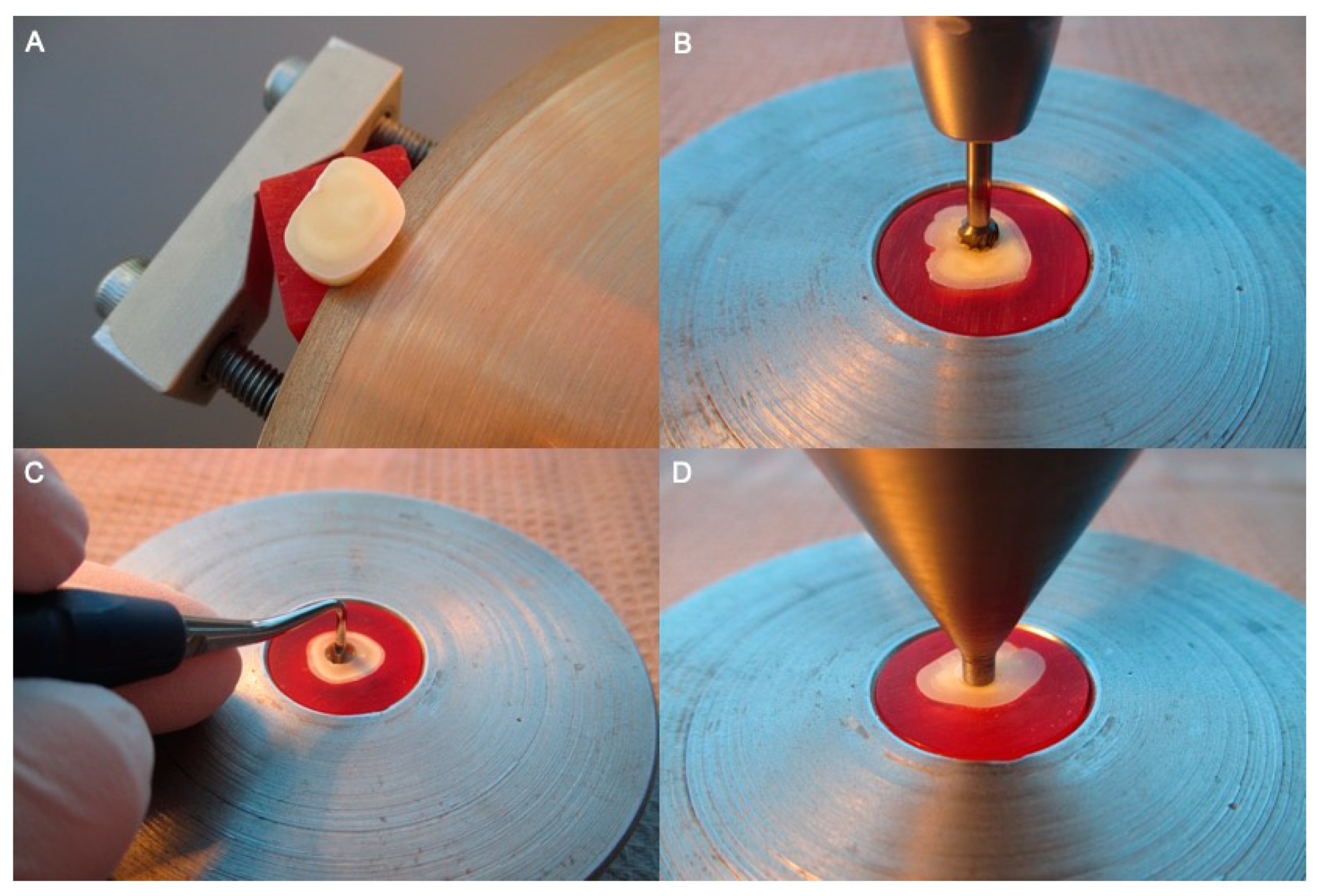
2. Materials and Methods
Statistical Evaluation
3. Results
4. Discussion
5. Conclusions
- Multi-step adhesive systems are preferable to one-step adhesive systems due to their higher bond strength to dentin.
- Flowable resin composites showed the highest bond strength values to dentin and should become more important as restoration material especially in cavity lining.
- The use of a shrinkage-reducing soft-start mode for the polymerization of resin composites does not enhance the bond strength to dentin.
- Acetone-based, HEMA-free and maleic acid-containing adhesives should be avoided due to their lower bond strength with dentin.
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Brunthaler, A.; König, F.; Lucas, T.; Sperr, W.; Schedle, A. Longevity of direct resin composite restorations in posterior teeth. Clin. Oral Investig. 2003, 7, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Van Meerbeek, B.; Kanumilli, P.V.; De Munck, J.; Van Landuyt, K.; Lambrechts, P.; Peumans, M. A randomized, controlled trial evaluating the three-year clinical effectiveness of two etch & rinse adhesives in cervical lesions. Oper. Dent. 2004, 29, 376–385. [Google Scholar] [PubMed]
- Watts, D.C.; Satterthwaite, J.D. Axial shrinkage-stress depends upon both C-factor and composite mass. Dent. Mater. 2008, 24, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Mantri, S.P.; Mantri, S.S. Management of shrinkage stresses in direct restorative light-cured composites: A review. J. Esthet. Restor. Dent. 2013, 25, 305–313. [Google Scholar] [CrossRef]
- Feng, L.; Suh, B.I. A mechanism on why slower polymerization of a dental composite produces lower contraction stress. J. Biomed. Mater. Res. Part B Appl. Biomater. 2006, 78, 63–69. [Google Scholar] [CrossRef]
- Wang, Z.; Chiang, M.Y. System compliance dictates the effect of composite filler content on polymerization shrinkage stress. Dent. Mater. 2016, 32, 551–560. [Google Scholar] [CrossRef]
- Sunbul, H.; Silikas, N.; Watts, D.C. Polymerization shrinkage kinetics and shrinkage-stress in dental resin-composites. Dent. Mater. 2016, 32, 998–1006. [Google Scholar] [CrossRef]
- Benetti, A.R.; Havndrup-Pedersen, C.; Honoré, D.; Pedersen, M.K.; Pallesen, U. Bulk-fill resin composites: Polymerization contraction, depth of cure, and gap formation. Oper. Dent. 2015, 40, 190–200. [Google Scholar] [CrossRef]
- De Munck, J.; Van Landuyt, K.; Peumans, M.; Poitevin, A.; Lambrechts, P.; Braem, M.; Van Meerbeek, B. A critical review of the durability of adhesion to tooth tissue: Methods and results. J. Dent. Res. 2005, 84, 118–132. [Google Scholar] [CrossRef]
- Masarwa, N.; Mohamed, A.; Abou-Rabii, I.; Abu Zaghlan, R.; Steier, L. Longevity of Self-etch Dentin Bonding Adhesives Compared to Etch-and-rinse Dentin Bonding Adhesives: A Systematic Review. J. Evid. Based Dent. Pract. 2016, 16, 96–106. [Google Scholar] [CrossRef]
- Ozer, F.; Blatz, M.B. Self-etch and etch-and-rinse adhesive systems in clinical dentistry. Compend. Contin. Educ. Dent. 2013, 34, 12–14. [Google Scholar] [PubMed]
- Borges, B.C.; Vilela, A.R.; da Silva-Junior, C.A.; Souza-Junior, E.J.; Sinhoreti, M.A.; Pinheiro, F.H.; Braz, R.; Montes, M.A. Dual-cured etch-and-rinse adhesive systems increase the bond durability of direct coronal dentin restorations. Oper. Dent. 2013, 38, 512–518. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Omran, T.A.; Garoushi, S.; Abdulmajeed, A.A.; Lassila, L.V.; Vallittu, P.K. Influence of increment thickness on dentin bond strength and light transmission of composite base materials. Clin. Oral Investig. 2017, 21, 1717–1724. [Google Scholar] [CrossRef]
- Flury, S.; Peutzfeldt, A.; Lussi, A. Influence of increment thickness on microhardness and dentin bond strength of bulk fill resin composites. Dent. Mater. 2014, 30, 1104–1112. [Google Scholar] [CrossRef] [PubMed]
- Garoushi, S.; Vallittu, P.; Shinya, A.; Lassila, L. Influence of increment thickness on light transmission, degree of conversion and micro hardness of bulk fill composites. Odontology 2016, 104, 291–297. [Google Scholar] [CrossRef] [PubMed]
- Haenel, T.; Hausnerová, B.; Steinhaus, J.; Price, R.B.; Sullivan, B.; Moeginger, B. Effect of the irradiance distribution from light curing units on the local micro-hardness of the surface of dental resins. Dent. Mater. 2015, 31, 93–104. [Google Scholar] [CrossRef] [PubMed]
- Chuang, S.F.; Huang, P.S.; Chen, T.Y.; Huang, L.H.; Su, K.C.; Chang, C.H. Shrinkage behaviors of dental composite restorations-The experimental-numerical hybrid analysis. Dent. Mater. 2016, 32, e362–e373. [Google Scholar] [CrossRef]
- Mouhat, M.; Mercer, J.; Stangvaltaite, L.; Örtengren, U. Light-curing units used in dentistry: Factors associated with heat development-potential risk for patients. Clin. Oral Investig. 2017, 21, 1687–1696. [Google Scholar] [CrossRef]
- Durey, K.; Santini, A.; Miletic, V. Pulp chamber temperature rise during curing of resin-based composites with different light-curing units. Prim. Dent. Care 2008, 15, 33–38. [Google Scholar] [CrossRef]
- Gomes, M.; DeVito-Moraes, A.; Francci, C.; Moraes, R.; Pereira, T.; Froes-Salgado, N.; Yamazaki, L.; Silva, L.; Zezell, D. Temperature increase at the light guide tip of 15 contemporary LED units and thermal variation at the pulpal floor of cavities: An infrared thermographic analysis. Oper. Dent. 2013, 38, 324–333. [Google Scholar] [CrossRef]
- Sirisha, K.; Rambabu, T.; Ravishankar, Y.; Ravikumar, P. Validity of bond strength tests: A critical review-Part II. J. Conserv. Dent. 2014, 17, 420–426. [Google Scholar] [CrossRef] [PubMed]
- Sirisha, K.; Rambabu, T.; Shankar, Y.R.; Ravikumar, P. Validity of bond strength tests: A critical review: Part I. J. Conserv. Dent. 2014, 17, 305–311. [Google Scholar] [CrossRef] [PubMed]
- Braga, R.R.; Meira, J.B.; Boaro, L.C.; Xavier, T.A. Adhesion to tooth structure: A critical review of "macro" test methods. Dent. Mater. 2010, 26, e38–e49. [Google Scholar] [CrossRef] [PubMed]
- Van Meerbeek, B.; Peumans, M.; Poitevin, A.; Mine, A.; Van Ende, A.; Neves, A.; De Munck, J. Relationship between bond-strength tests and clinical outcomes. Dent. Mater. 2010, 26, e100–e121. [Google Scholar] [CrossRef] [PubMed]
- Cekic-Nagas, I.; Ergun, G.; Nagas, E.; Tezvergil, A.; Vallittu, P.K.; Lassila, L.V. Comparison between regional micropush-out and microtensile bond strength of resin composite to dentin. Acta. Odontol. Scand. 2008, 66, 73–81. [Google Scholar] [CrossRef] [PubMed]
- Richardson, J.T. Eta squared and partial eta squared as measures of effect size in educational research. Educ. Res. Rev. 2011, 6, 135–147. [Google Scholar] [CrossRef]
- Sofan, E.; Sofan, A.; Palaia, G.; Tenore, G.; Romeo, U.; Migliau, G. Classification review of dental adhesive systems: From the IV generation to the universal type. Ann. Stomatol. 2017, 8, 1–17. [Google Scholar]
- Tay, F.R.; Pashley, D.H. Have dentin adhesives become too hydrophilic? J. Can. Dent. Assoc. 2003, 69, 726–731. [Google Scholar]
- Tay, F.R.; Pashley, D.H.; Suh, B.I.; Carvalho, R.M.; Itthagarun, A. Single-step adhesives are permeable membranes. J. Dent. 2002, 30, 371–382. [Google Scholar] [CrossRef]
- Hashimoto, M.; Ohno, H.; Sano, H.; Kaga, M.; Oguchi, H. In vitro degradation of resin-dentin bonds analyzed by microtensile bond test, scanning and transmission electron microscopy. Biomaterials 2003, 24, 3795–3803. [Google Scholar] [CrossRef]
- Fu, B.; Yuan, J.; Qian, W.; Shen, Q.; Sun, X.; Hannig, M. Evidence of chemisorption of maleic acid to enamel and hydroxyapatite. Eur. J. Oral Sci. 2004, 112, 362–367. [Google Scholar] [CrossRef] [PubMed]
- Zafar, M.S.; Ahmed, N. The effects of acid etching time on surface mechanical properties of dental hard tissues. Dent. Mater. J. 2005, 34, 315–320. [Google Scholar] [CrossRef] [PubMed]
- Zanchi, C.H.; Münchow, E.A.; Ogliari, F.A.; Chersoni, S.; Prati, C.; Demarco, F.F.; Piva, E. Development of experimental HEMA-free three-step adhesive system. J. Dent. 2010, 38, 503–508. [Google Scholar] [CrossRef] [PubMed]
- Van Landuyt, K.L.; Yoshida, Y.; Hirata, I.; Snauwaert, J.; De Munck, J.; Okazaki, M.; Suzuki, K.; Lambrechts, P.; Van Meerbeek, B. Influence of the chemical structure of functional monomers on their adhesive performance. J. Dent. Res. 2008, 87, 757–761. [Google Scholar] [CrossRef] [PubMed]
- Nakaoki, Y.; Nikaido, T.; Pereira, P.N.; Inokoshi, S.; Tagami, J. Dimensional changes of demineralized dentin treated with HEMA primers. Dent. Mater. 2000, 16, 441–446. [Google Scholar] [CrossRef]
- Zanchi, C.H.; Münchow, E.A.; Ogliari, F.A.; de Carvalho, R.V.; Chersoni, S.; Prati, C.; Demarco, F.F.; Piva, E. Effects of long-term water storage on the microtensile bond strength of five experimental self-etching adhesives based on surfactants rather than HEMA. Clin. Oral Investig. 2013, 17, 833–839. [Google Scholar] [CrossRef]
- Van Meerbeek, B.; Van Landuyt, K.; De Munck, J.; Hashimoto, M.; Peumans, M.; Lambrechts, P.; Yoshida, Y.; Inoue, S.; Suzuki, K. Technique-sensitivity of contemporary adhesives. Dent. Mater. J. 2005, 24, 1–13. [Google Scholar] [CrossRef]
- Rathke, A.; Alt, A.; Gambin, N.; Haller, B. Dentin diffusion of HEMA released from etch-and-rinse and self-etch bonding systems. Eur. J. Oral Sci. 2007, 115, 510–516. [Google Scholar] [CrossRef]
- Paranjpe, A.; Bordador, L.C.; Wang, M.Y.; Hume, W.R.; Jewett, A. Resin monomer 2-hydroxyethyl methacrylate (HEMA) is a potent inducer of apoptotic cell death in human and mouse cells. J. Dent. Res. 2005, 84, 172–177. [Google Scholar] [CrossRef]
- Irmak, Ö.; Baltacıoğlu, İ.H.; Ulusoy, N.; Bağış, Y.H. Solvent type influences bond strength to air or blot-dried dentin. BMC Oral Health 2016, 16, 77. [Google Scholar] [CrossRef]
- Reis, A.; Loguercio, A.D.; Azevedo, C.L.; de Carvalho, R.M.; da Julio, S.M.; Grande, R.H. Moisture spectrum of demineralized dentin for adhesive systems with different solvent bases. J. Adhes. Dent. 2003, 5, 183–192. [Google Scholar] [PubMed]
- Abdalla, A.I. Bond strength of a total-etch and two self-etch adhesives to dentin with and without intermediate flowable liner. Am. J. Dent. 2010, 23, 157–160. [Google Scholar] [PubMed]
- Reddy, S.N.; Jayashankar, D.N.; Nainan, M.; Shivanna, V. The effect of flowable composite lining thickness with various curing techniques on microleakage in class II composite restorations: An in vitro study. J. Contemp. Dent. Pract. 2013, 14, 56–60. [Google Scholar] [CrossRef] [PubMed]
- Anatavara, S.; Sitthiseripratip, K.; Senawongse, P. Stress relieving behaviour of flowable composite liners: A finite element analysis. Dent. Mater. J. 2016, 35, 369–378. [Google Scholar] [CrossRef] [PubMed]
- Mosharrafian, S.; Heidari, A.; Rahbar, P. Microleakage of Two Bulk Fill and One Conventional Composite in Class II Restorations of Primary Posterior Teeth. J. Dent. 2017, 14, 123–131. [Google Scholar]
- Poggio, C.; Chiesa, M.; Scribante, A.; Mekler, J.; Colombo, M. Microleakage in Class II composite restorations with margins below the CEJ: In vitro evaluation of different restorative techniques. Med. Oral Patol. Oral Cir. Bucal. 2013, 18, 793–798. [Google Scholar] [CrossRef]
- Ilie, N.; Kunzelmann, K.H.; Hickel, R. Evaluation of micro-tensile bond strengths of composite materials in comparison to their polymerization shrinkage. Dent. Mater. 2006, 22, 593–601. [Google Scholar] [CrossRef]
| Composite Material | One-Step Self-Etch Adhesive System | Multi-Step Etch-and-Rinse Adhesive System | |
|---|---|---|---|
| Universal | Filtec Supreme XTE Universal | 13.11 ± 5.04 (soft) a,A,I,y 13.04 ± 4.20 (turbo) a,AB,I,y | 18.44 ± 2.00 (soft) a,B,I,z 18.42 ± 2.23 (turbo) a,B,I,z |
| Tetric EvoCeram | 11.90 ± 3.08 (soft) a,A,I,z 10.26 ± 2.91 (turbo) a,A,I,z | 11.23 ± 1.49 (soft) a,A,I,z 10.75 ± 3.12 (turbo) a,A,I,z | |
| Herculite XRV Ultra | 15.77 ± 1.67 (soft) b,A,I,y 15.27 ± 4.34 (turbo) a,B,I,y | 18.64 ± 1.72 (soft) a,B,I,z 18.86 ± 4.50 (turbo) a,B,I,z | |
| Flowable | Filtec Supreme XTE Flowable | 22.91 ± 1.99 (soft) b,B,I,y 21.81 ± 2.16 (turbo) c,B,I,y | 25.54 ± 2.80 (soft) c,B,I,z 25.80 ± 2.81 (turbo)c,B,I,z |
| Tetric EvoFlow | 18.04 ± 2.51 (soft) b,A,I,z 17.51 ± 1.98 (turbo) b,A,I,z | 11.71 ± 1.59 (soft) a,A,I,y 10.90 ± 4.38 (turbo) a,A,I,y | |
| Herculite XRV Ultra Flow | 23.20 ± 2.39 (soft) c,B,I,y 22.69 ± 2.72 (turbo) b,B,I,y | 27.50 ± 2.58 (soft) b,B,I,z 27.18 ± 2.21 (turbo) b,B,I,z | |
| Bulk-Fill | Filtec Bulk-Fill Posterior | 16.69 ± 4.48 (soft) a,B,I,y 17.29 ± 4.78 (turbo) b,B,I,y | 21.76 ± 2.84 (soft) b,C,I,z 22.33 ± 2.57 (turbo) b,C,I,z |
| Tetric Bulk-Fill | 12.84 ± 2.43 (soft) a,A,I,z 12.07 ± 2.23 (turbo)a,A,I,z | 12.23 ± 3.51 (soft) a,A,I,z 11.63 ± 1.71 (turbo) a,A,I,z | |
| Sonic Fill 2 | 11.81 ± 4.09 (soft) a,A,I,y 12.73 ± 2.01 (turbo) a,A,I,y | 18.31 ± 3.08 (soft) a,B,I,z 18.92 ± 2.39 (turbo) a,B,I,z | |
| Composite Material | One-Step Self-Etch Adhesive System | Multi-Step Etch-and-Rinse Adhesive System | |
|---|---|---|---|
| Universal | Filtec Supreme XTE Universal | 80 (43;98) (soft) 70 (33;94) (turbo) | 60 (25;88) (soft) 70 (33;94) (turbo) |
| Tetric EvoCeram | 70 (33;94) (soft) 80 (43;98) (turbo) | 100 (68;100) (soft) 100 (68;100) (turbo) | |
| Herculite XRV Ultra | 70 (33;94) (soft) 60 (25;88) (turbo) | 70 (33;94) (soft) 50 (17;82) (turbo) | |
| Flowable | Filtec Supreme XTE Flowable | 30 (5;66) (soft) 40 (11;74) (turbo) | 20 (1;56) (soft) 20 (1;56) (turbo) |
| Tetric EvoFlow | 30 (5;66) (soft) 40 (11;74) (turbo) | 80 (43;98) (soft) 70 (33;94) (turbo) | |
| Herculite XRV Ultra Flow | 20 (1;56) (soft) 30 (5;66) (turbo) | 10 (0;45) (soft) 20 (1;56) (turbo) | |
| Bulk-Fill | Filtec Bulk-Fill Posterior | 50 (17;82) (soft) 40 (11;74) (turbo) | 40 (11;74) (soft) 30 (5;66) (turbo) |
| Tetric Bulk-Fill | 40 (11;74) (soft) 50 (17;82) (turbo) | 90 (54;100) (soft) 100 (68;100) (turbo) | |
| Sonic Fill 2 | 80 (43;98) (soft) 90 (54;100) (turbo) | 70 (33;94) (soft) 80 (43;98) (turbo) | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Steiner, R.; Edelhoff, D.; Stawarczyk, B.; Dumfahrt, H.; Lente, I. Effect of Dentin Bonding Agents, Various Resin Composites and Curing Modes on Bond Strength to Human Dentin. Materials 2019, 12, 3395. https://doi.org/10.3390/ma12203395
Steiner R, Edelhoff D, Stawarczyk B, Dumfahrt H, Lente I. Effect of Dentin Bonding Agents, Various Resin Composites and Curing Modes on Bond Strength to Human Dentin. Materials. 2019; 12(20):3395. https://doi.org/10.3390/ma12203395
Chicago/Turabian StyleSteiner, Rene, Daniel Edelhoff, Bogna Stawarczyk, Herbert Dumfahrt, and Isabel Lente. 2019. "Effect of Dentin Bonding Agents, Various Resin Composites and Curing Modes on Bond Strength to Human Dentin" Materials 12, no. 20: 3395. https://doi.org/10.3390/ma12203395
APA StyleSteiner, R., Edelhoff, D., Stawarczyk, B., Dumfahrt, H., & Lente, I. (2019). Effect of Dentin Bonding Agents, Various Resin Composites and Curing Modes on Bond Strength to Human Dentin. Materials, 12(20), 3395. https://doi.org/10.3390/ma12203395






