Effects of Printing Parameters on the Fit of Implant-Supported 3D Printing Resin Prosthetics
Abstract
1. Introduction
2. Materials and Methods
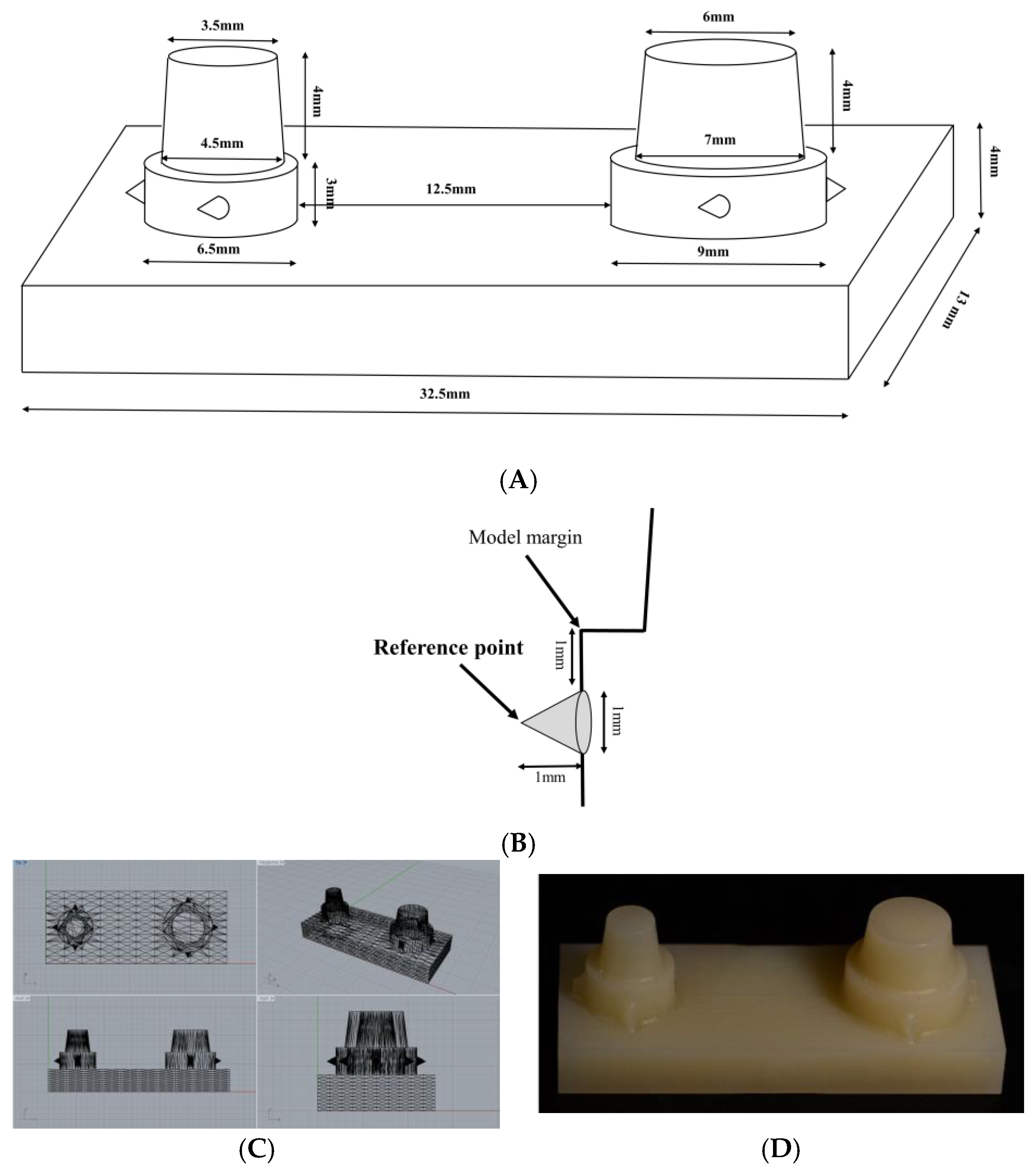
2.1. Model Design and Fabrication
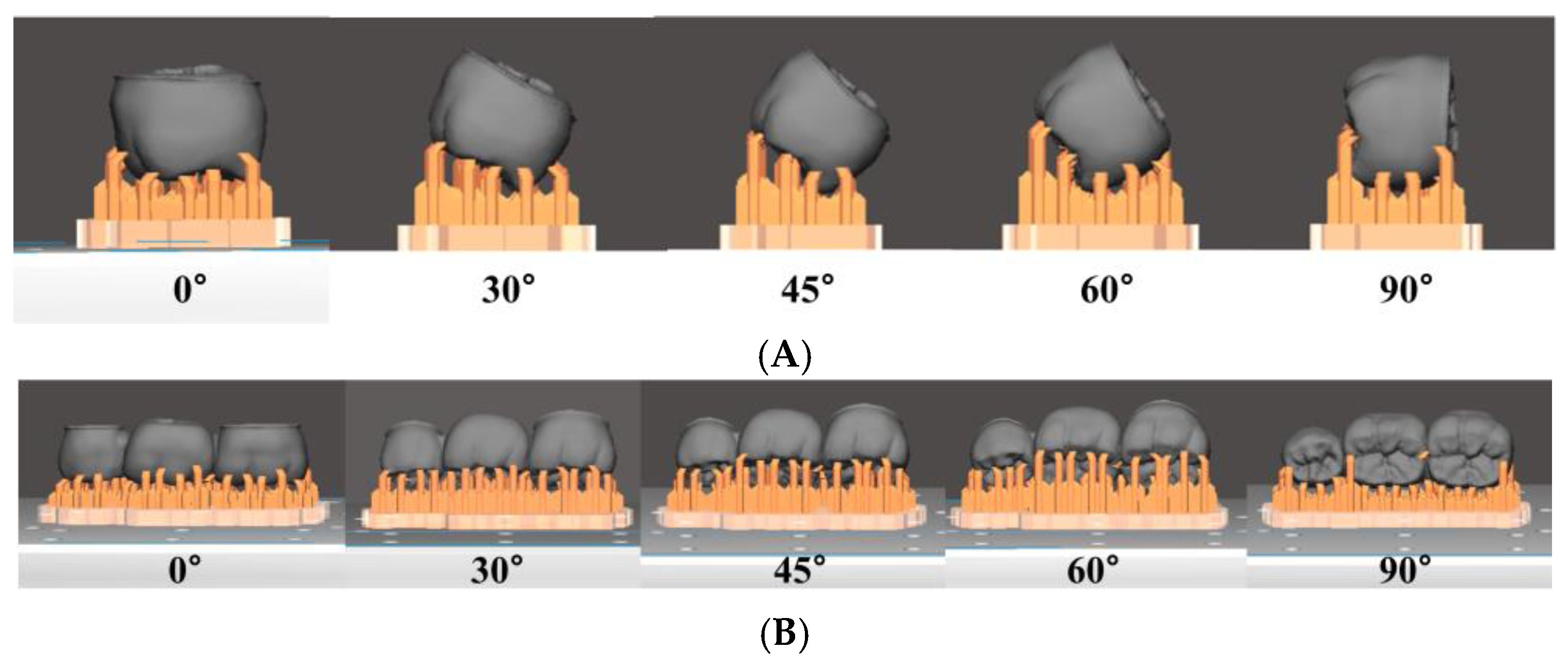
2.2. Prosthesis Design and Fabrication
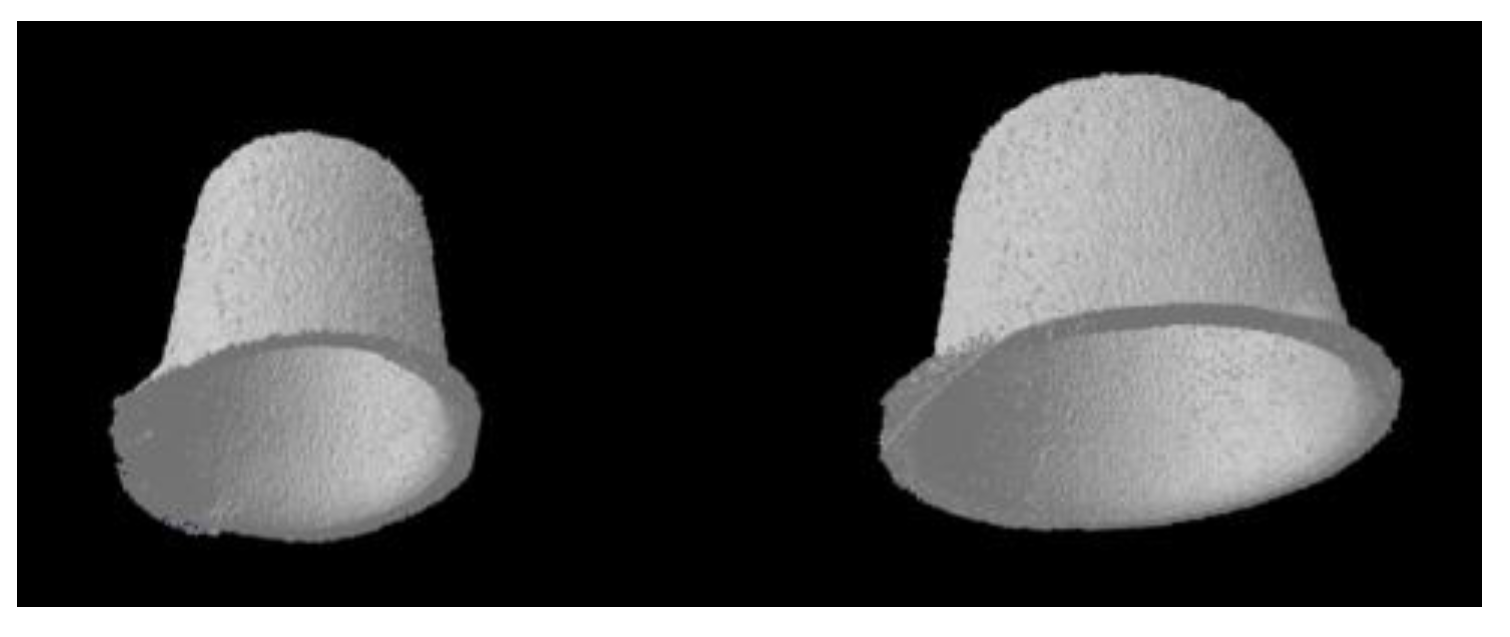
2.3. Micro-CT Scanning
2.4. Internal Gap Volume Analysis
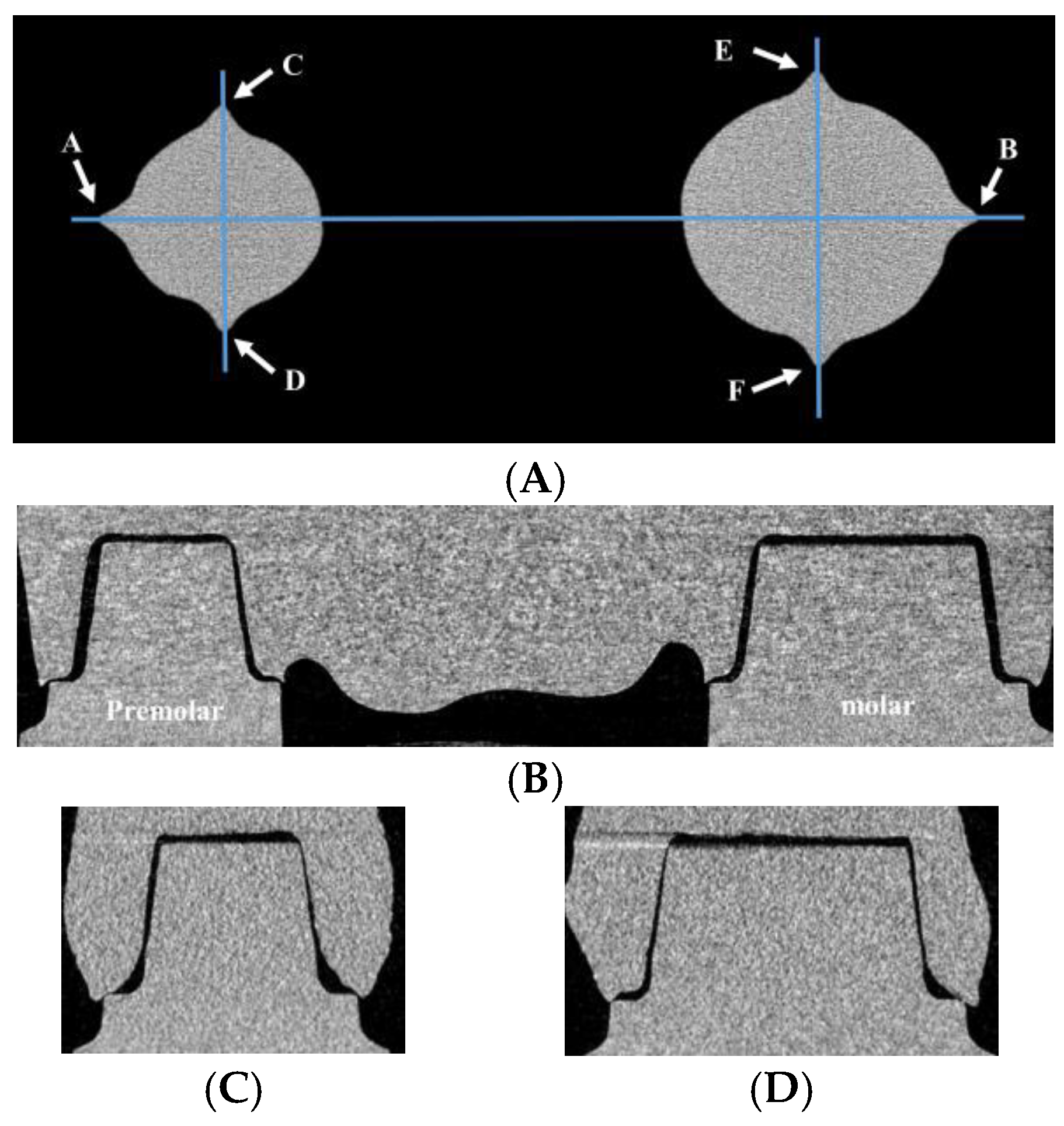
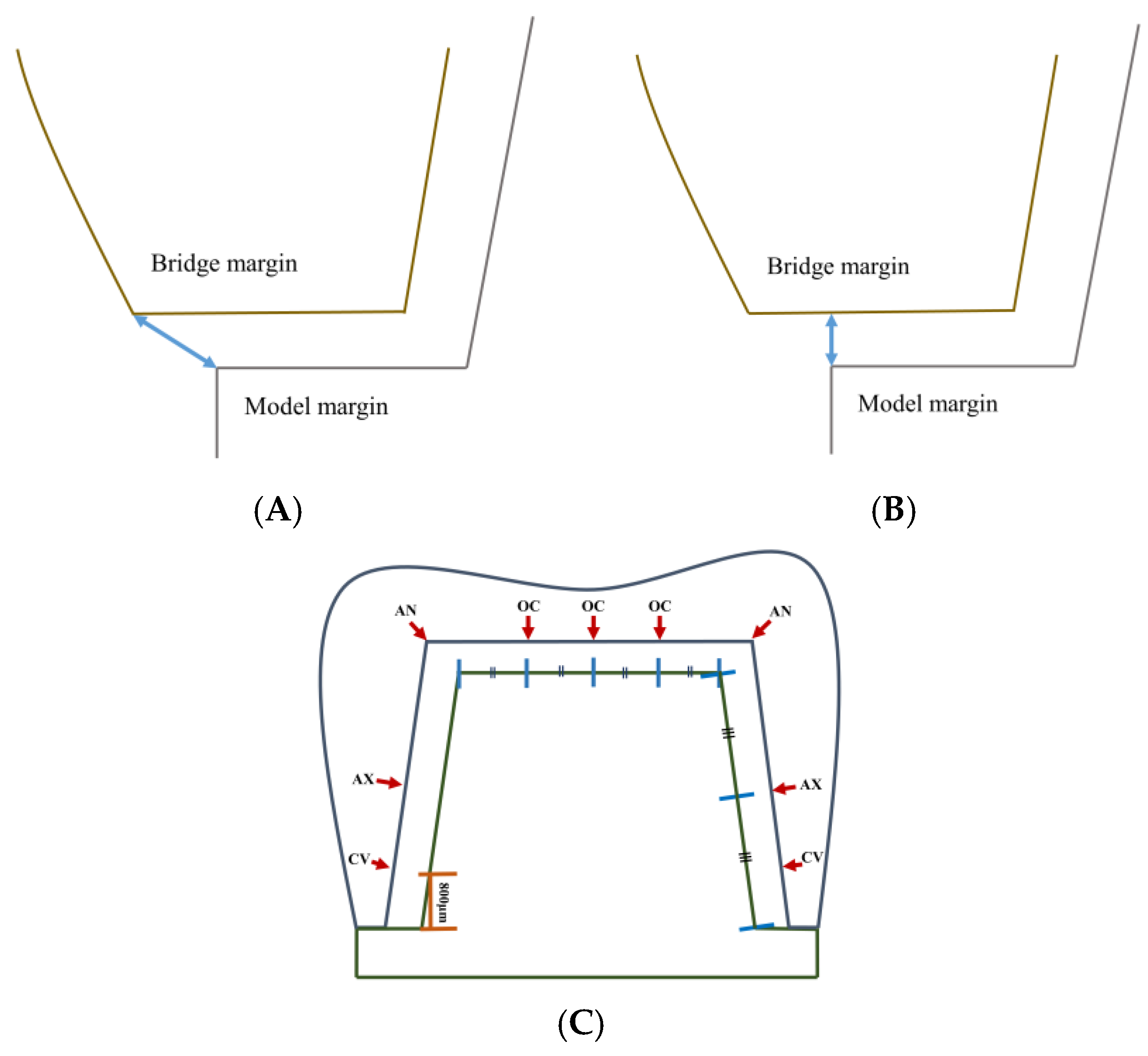
2.5. Marginal Fit and Internal Gap Length Analysis
2.6. Statistical Analysis
3. Results
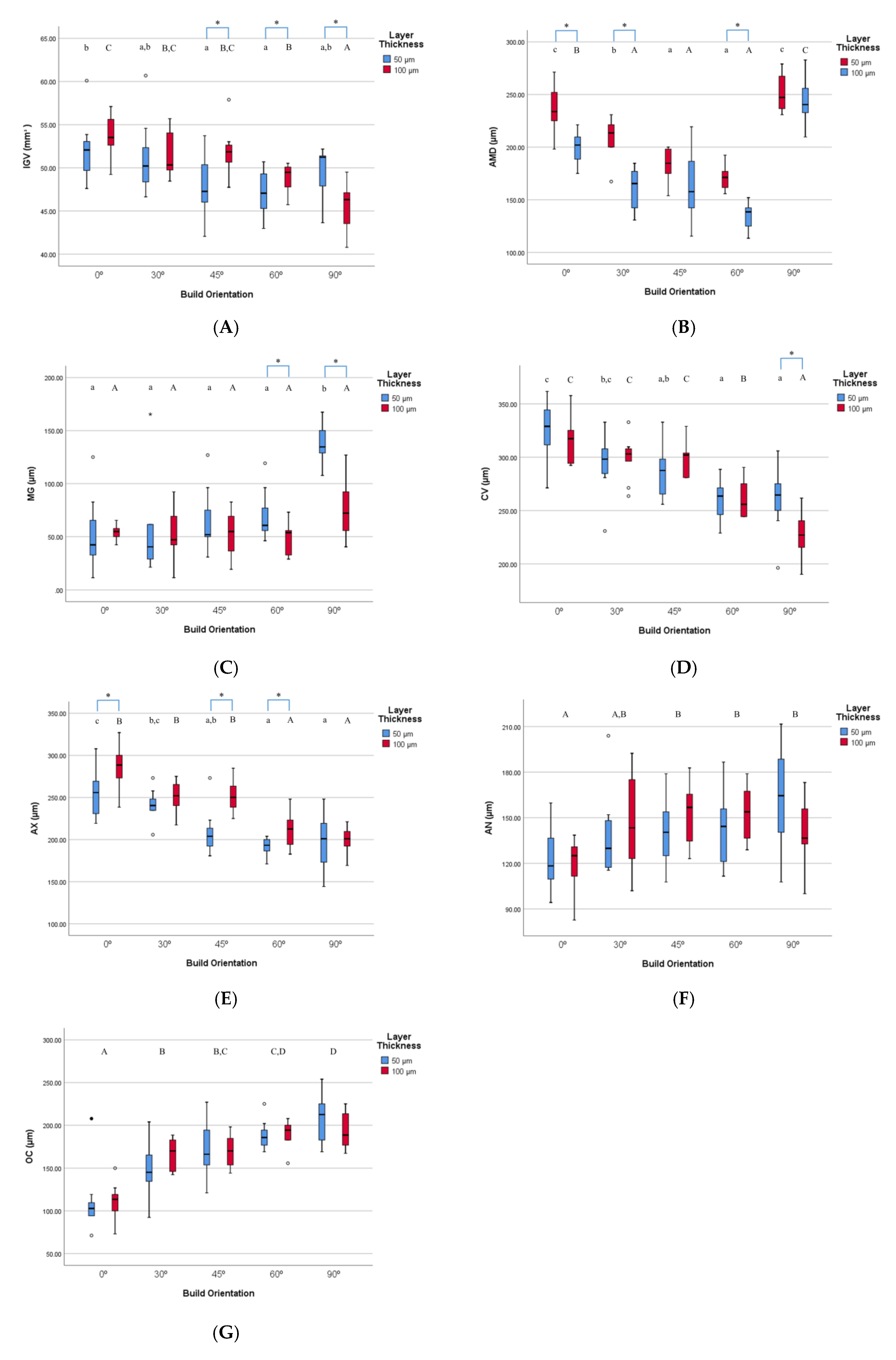
3.1. Internal Gap Volume Analysis for 3D Printing
3.2. Marginal Fit and Internal Gap Length Analysis for 3D Printing
3.3. Comparison of 3D Printing and Milling
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Bayne, S.; Heymann, H. CAD/CAM in dentistry: Present and future applications. Quintessence Int. 1996, 27, 431–433. [Google Scholar]
- Miyazaki, T.; Hotta, Y.; Kunii, J.; Kuriyama, S.; Tamaki, Y. A review of dental CAD/CAM: Current status and future perspectives from 20 years of experience. Dent. Mater. J. 2009, 28, 44–56. [Google Scholar] [CrossRef] [PubMed]
- Pettenò, D.; Schierano, G.; Bassi, F.; Bresciano, M.E.; Carossa, S. Comparison of marginal fit of 3 different metal-ceramic systems: An in vitro study. Int. J. Prosthodont. 2000, 13, 405–408. [Google Scholar] [PubMed]
- Beuer, F.; Schweiger, J.; Edelhoff, D. Digital dentistry: An overview of recent developments for CAD/CAM generated restorations. Br. Dent. J. 2008, 204, 505–511. [Google Scholar] [CrossRef] [PubMed]
- Atzeni, E.; Salmi, A. Economics of additive manufacturing for end-usable metal parts. Int. J. Adv. Manuf. Technol. 2012, 62, 1147–1155. [Google Scholar] [CrossRef]
- van Noort, R. The future of dental devices is digital. Dent. Mater. 2012, 28, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Stansbury, J.W.; Idacavage, M.J. 3D printing with polymers: Challenges among expanding options and opportunities. Dent. Mater. 2016, 32, 54–64. [Google Scholar] [CrossRef] [PubMed]
- Osman, R.B.; Alharbi, N.; Wismeijer, D. Build angle: Does it influence the accuracy of 3D-printed dental restorations using digital light-processing technology? Int. J. Prosthodont. 2017, 30, 182–188. [Google Scholar] [CrossRef]
- Wu, G.; Hsu, S. Review: Polymeric-based 3D printing for tissue engineering. J. Med. Biol. Eng. 2015, 35, 285–292. [Google Scholar] [CrossRef]
- Mai, H.; Lee, K.; Lee, D. Fit of interim crowns fabricated using photopolymer-jetting 3D printing. J. Prosthet. Dent. 2017, 118, 208–215. [Google Scholar] [CrossRef]
- Burns, D.R.; Beck, D.A.; Nelson, S.K. A review of selected dental literature on contemporary provisional fixed prosthodontic treatment: Report of the committee on research in fixed prosthodontics of the academy of fixed prosthodontics. J. Prosthet. Dent. 2003, 90, 474–497. [Google Scholar] [CrossRef]
- Patras, M.; Naka, O.; Doukoudakis, S.; Pissiotis, A. Management of provisional restorations’ deficiencies: A literature review. J. Esthet. Restor. Dent. 2012, 24, 26–38. [Google Scholar] [CrossRef] [PubMed]
- Raigrodski, A.J. Soft Tissue Management: The Restorative Perspective: Putting Concepts into Practice; International Quintessence Publishing Group: Chicago, IL, USA, 2015; p. 209. [Google Scholar]
- Gratton, D.G.; Aquilino, S.A. Interim restorations. Dent. Clin. N. Am. 2004, 48, 487–497. [Google Scholar] [CrossRef] [PubMed]
- Alharbi, N.; Alharbi, S.; Cuijpers, V.M.J.I.; Osman, R.B.; Wismeijer, D. Three-dimensional evaluation of marginal and internal fit of 3D-printed interim restorations fabricated on different finish line designs. J. Prosthodont. Res. 2018, 62, 218–226. [Google Scholar] [CrossRef] [PubMed]
- Tahayeri, A.; Morgan, M.; Fugolin, A.P.; Bompolaki, D.; Athirasala, A.; Pfeifer, C.S.; Ferracane, J.L.; Bertassoni, L.E. 3D printed versus conventionally cured provisional crown and bridge dental materials. Dent. Mater. 2018, 34, 192–200. [Google Scholar] [CrossRef] [PubMed]
- Unkovskiy, A.; Bui, P.H.; Schille, C.; Geis-Gerstorfer, J.; Huettig, F.; Spintzyk, S. Objects build orientation, positioning, and curing influence dimensional accuracy and flexural properties of stereolithographically printed resin. Dent. Mater. 2018, 34, 324–333. [Google Scholar] [CrossRef] [PubMed]
- Alharbi, N.; Osman, R.B.; Wismeijer, D. Factors influencing the dimensional accuracy of 3D-printed full-coverage dental restorations using stereolithography technology. Int. J. Prosthodont. 2016, 29, 503–510. [Google Scholar] [CrossRef]
- Giannetopoulos, S.; van Noort, R.; Tsitrou, E. Evaluation of the marginal integrity of ceramic copings with different marginal angles using two different CAD/CAM systems. J. Dent. 2010, 38, 980–986. [Google Scholar] [CrossRef] [PubMed]
- Nawafleh, N.A.; Mack, F.; Evans, J.; Mackay, J.; Hatamleh, M.M. Accuracy and reliability of methods to measure marginal adaptation of crowns and FDPs: A literature review. J. Prosthodont. 2013, 22, 419–428. [Google Scholar] [CrossRef] [PubMed]
- Beuer, F.; Naumann, M.; Gernet, W.; Sorensen, J.A. Precision of fit: Zirconia three-unit fixed dental prostheses. Clin. Oral Investig. 2008, 13, 343–349. [Google Scholar] [CrossRef]
- Kohorst, P.; Brinkmann, H.; Dittmer, M.P.; Borchers, L.; Stiesch, M. Influence of the veneering process on the marginal fit of zirconia fixed dental prostheses. J. Oral Rehabil. 2010, 37, 283–291. [Google Scholar] [CrossRef] [PubMed]
- Otis, L.L.; Everett, M.J.; Sathyam, U.S. Optical coherence tomography: A new imaging technology for dentistry. J. Am. Dent. Assoc. 2000, 131, 511–514. [Google Scholar] [CrossRef] [PubMed]
- Borba, M.; Cesar, P.F.; Griggs, J.A.; Della Bona, Á. Adaptation of all-ceramic fixed partial dentures. Dent. Mater. 2011, 27, 1119–1126. [Google Scholar] [CrossRef] [PubMed]
- Contrepois, M.; Soenen, A.; Bartala, M.; Laviole, O. Marginal adaptation of ceramic crowns: A systematic review. J. Prosthet. Dent. 2013, 110, 447–454. [Google Scholar] [CrossRef] [PubMed]
- Brand, R.W.; Satin, E.; Isselhard, D.E. Anatomy of Orofacial Structures: A Comprehensive Approach; Mosby: St. Louis, MO, USA, 2014. [Google Scholar]
- Goodacre, C.J.; Campagni, W.V.; Aquilino, S.A. Tooth preparations for complete crowns: An art form based on scientific principles. J. Prosthet. Dent. 2001, 85, 363–376. [Google Scholar] [CrossRef] [PubMed]
- Holmes, J.R.; Bayne, S.C.; Holland, G.A.; Sulik, W.D. Considerations in measurement of marginal fit. J. Prosthet. Dent. 1989, 62, 405–408. [Google Scholar] [CrossRef]
- Yildirim, G.; Uzun, I.H.; Keles, A. Evaluation of marginal and internal adaptation of hybrid and nanoceramic systems with microcomputed tomography: An in vitro study. J. Prosthet. Dent. 2017, 118, 200–207. [Google Scholar] [CrossRef]
- Kim, J.; Jeong, J.; Lee, J.; Cho, H. Fit of lithium disilicate crowns fabricated from conventional and digital impressions assessed with micro-CT. J. Prosthet. Dent. 2016, 116, 551–557. [Google Scholar] [CrossRef]
- Boitelle, P.; Mawussi, B.; Tapie, L.; Fromentin, O. A systematic review of CAD/CAM fit restoration evaluations. J. Oral Rehabil. 2014, 41, 853–874. [Google Scholar] [CrossRef]
- Tuntiprawon, M.; Wilson, P.R. The effect of cement thickness on the fracture strength of all-ceramic crowns. Aust. Dent. J. 1995, 40, 17–21. [Google Scholar] [CrossRef]
- Beschnidt, S.M.; Strub, J.R. Evaluation of the marginal accuracy of different all-ceramic crown systems after simulation in the artificial mouth. J. Oral Rehabil. 1999, 26, 582–593. [Google Scholar] [CrossRef] [PubMed]
- Groten, M.; Axmann, D.; Pröbster, L.; Weber, H. Determination of the minimum number of marginal gap measurements required for practical in vitro testing. J. Prosthet. Dent. 2000, 83, 40–49. [Google Scholar] [CrossRef]
- Mitchell, C.A.; Pintado, M.R.; Douglas, W.H. Nondestructive, in vitro quantification of crown margins. J. Prosthet. Dent. 2001, 85, 575–584. [Google Scholar] [CrossRef] [PubMed]
- Wolfart, S.; Wegner, S.M.; Al-Halabi, A.; Kern, M. Clinical evaluation of marginal fit of a new experimental all-ceramic system before and after cementation. Int. J. Prosthodont. 2003, 16, 587–592. [Google Scholar] [PubMed]
- Seo, D.; Yi, Y.; Roh, B. The effect of preparation designs on the marginal and internal gaps in Cerec3 partial ceramic crowns. J. Dent. 2009, 37, 374–382. [Google Scholar] [CrossRef] [PubMed]
- Persson, A.; Andersson, M.; Oden, A.; Sandborgh-Englund, G. A three-dimensional evaluation of a laser scanner and a touch- probe scanner. J. Prosthet. Dent. 2006, 95, 194–200. [Google Scholar] [CrossRef] [PubMed]
- Mehl, A.; Gloger, W.; Kunzelmann, K.; Hickel, R. A new optical 3-D device for the detection of wear. J. Dent. Res. 1997, 76, 1799–1807. [Google Scholar] [CrossRef] [PubMed]
- Gu, X.; Kern, M. Marginal discrepancies and leakage of all-ceramic crowns: Influence of luting agents and aging conditions. Int. J. Prosthodont. 2003, 16, 109–116. [Google Scholar] [PubMed]
- Stappert, C.; Dai, M.; Chitmongkolsuk, S.; Gerds, T.; Strub, JR. Marginal adaptation of three-unit fixed partial dentures constructed from pressed ceramic systems. Br. Dent. J. 2004, 196, 766–770. [Google Scholar] [CrossRef] [PubMed]
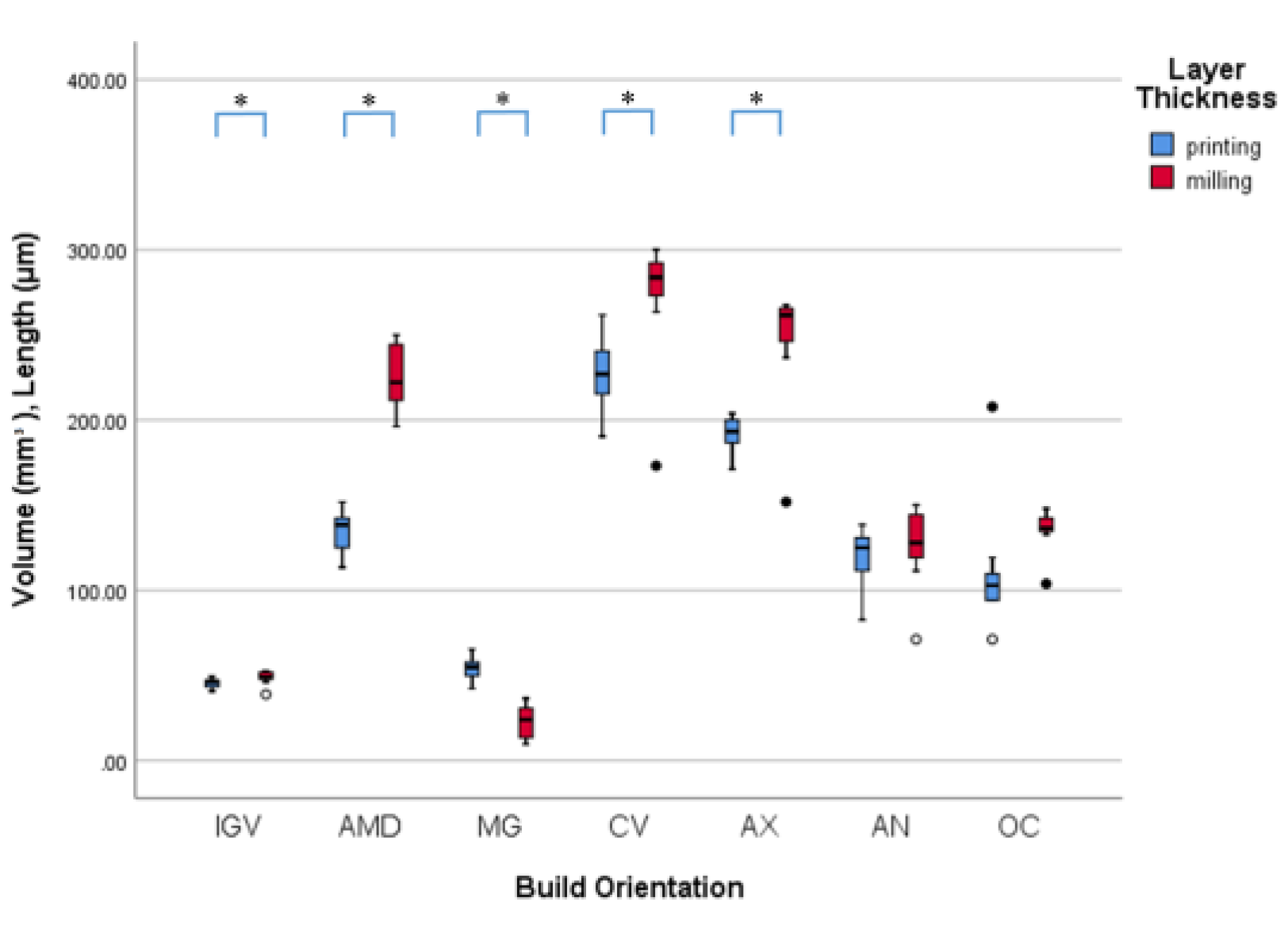
| Area | Selected 3D Printing Group | 3D Printing | Milling | p-Value |
|---|---|---|---|---|
| IGV | 100 µm, 90° | 45.5 ± 2.5 | 48.7 ± 4.0 | * p = 0.048 |
| AMD | 100 µm, 60° | 136.2 ± 11.8 | 225.1 ± 18.9 | * p = 0.000 |
| MG | 100 µm, 0° | 50.0 ± 14.7 | 23.1 ± 9.3 | * p = 0.000 |
| CV | 100 µm, 90° | 227.6 ± 20.7 | 273.4 ± 37.0 | * p = 0.003 |
| AX | 50 µm, 60° | 190.3 ± 11.3 | 247.2 ± 35.0 | * p = 0.000 |
| AN | 100 µm, 0° | 118.9 ± 17.5 | 125.4 ± 22.7 | p = 0.480 |
| OC | 50 µm, 0° | 111.2 ± 36.3 | 135.4 ± 12.2 | p = 0.06 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, G.-S.; Kim, S.-K.; Heo, S.-J.; Koak, J.-Y.; Seo, D.-G. Effects of Printing Parameters on the Fit of Implant-Supported 3D Printing Resin Prosthetics. Materials 2019, 12, 2533. https://doi.org/10.3390/ma12162533
Park G-S, Kim S-K, Heo S-J, Koak J-Y, Seo D-G. Effects of Printing Parameters on the Fit of Implant-Supported 3D Printing Resin Prosthetics. Materials. 2019; 12(16):2533. https://doi.org/10.3390/ma12162533
Chicago/Turabian StylePark, Gang-Seok, Seong-Kyun Kim, Seong-Joo Heo, Jai-Young Koak, and Deog-Gyu Seo. 2019. "Effects of Printing Parameters on the Fit of Implant-Supported 3D Printing Resin Prosthetics" Materials 12, no. 16: 2533. https://doi.org/10.3390/ma12162533
APA StylePark, G.-S., Kim, S.-K., Heo, S.-J., Koak, J.-Y., & Seo, D.-G. (2019). Effects of Printing Parameters on the Fit of Implant-Supported 3D Printing Resin Prosthetics. Materials, 12(16), 2533. https://doi.org/10.3390/ma12162533




