Comparative Evaluation of Mechanical Properties and Wear Ability of Five CAD/CAM Dental Blocks
Abstract
1. Introduction
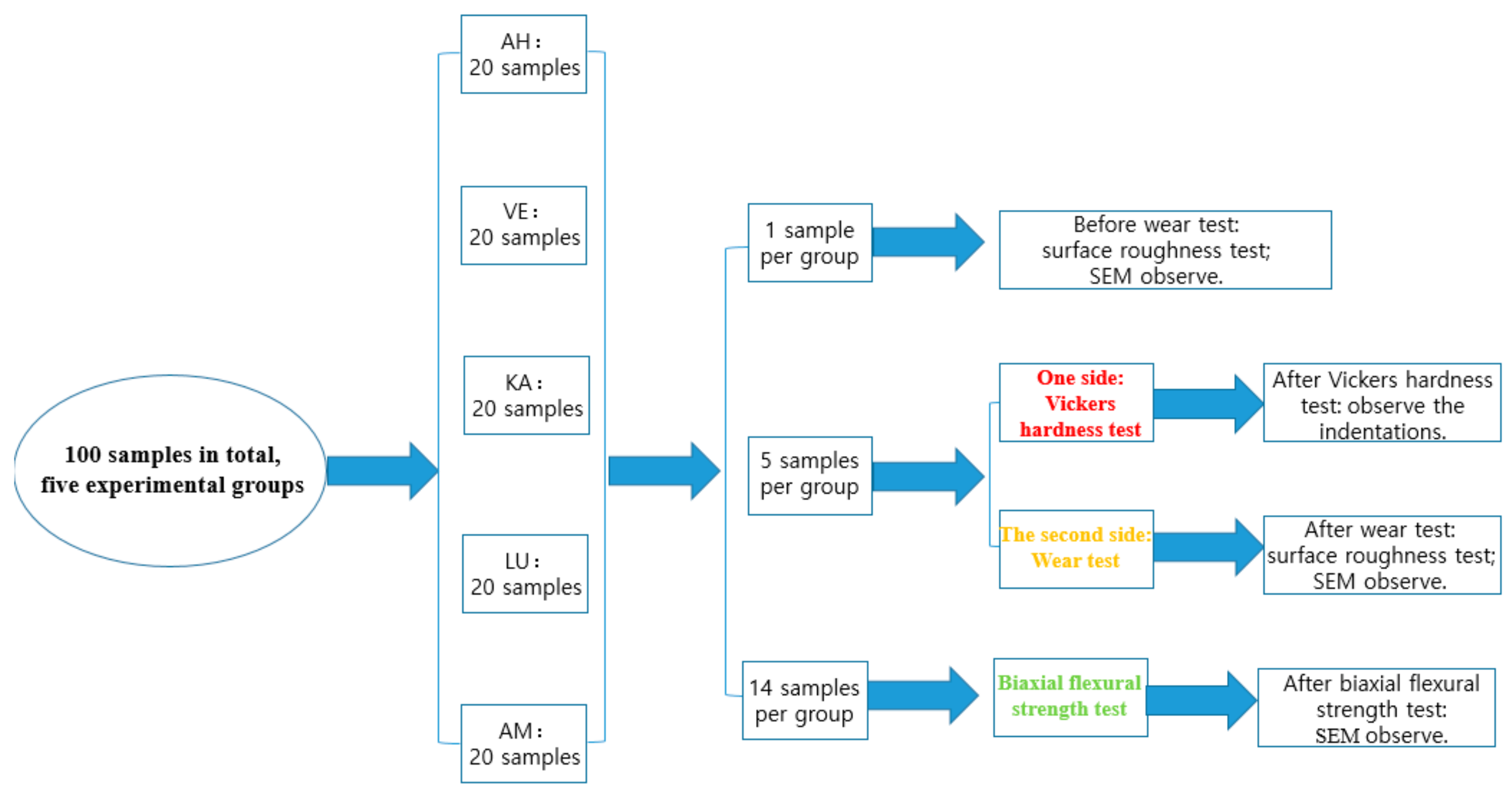
2. Materials and Methods
2.1. Specimen Preparation
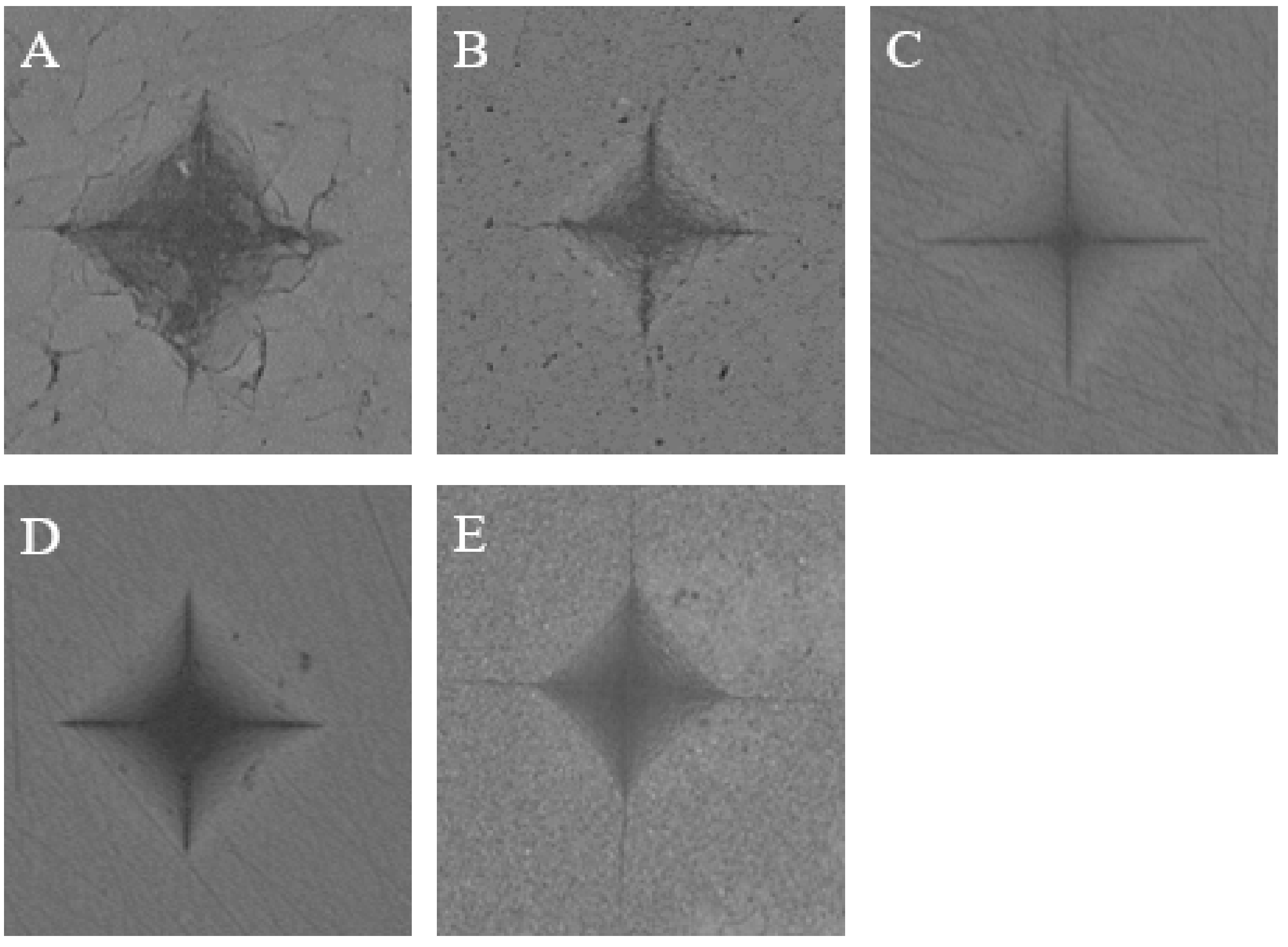
2.2. Vickers Hardness Test
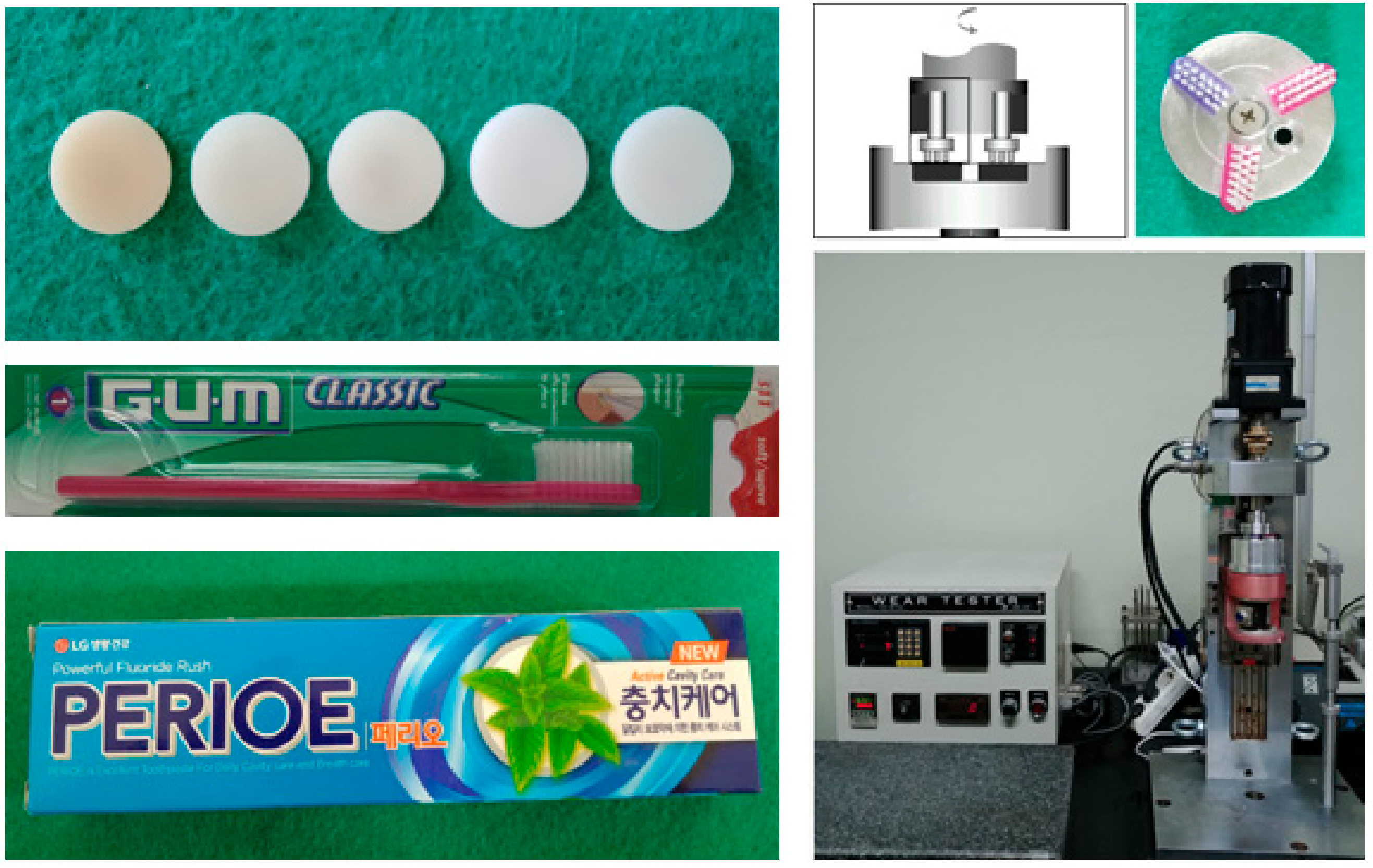
2.3. Wear Test
2.4. Surface Roughness Test
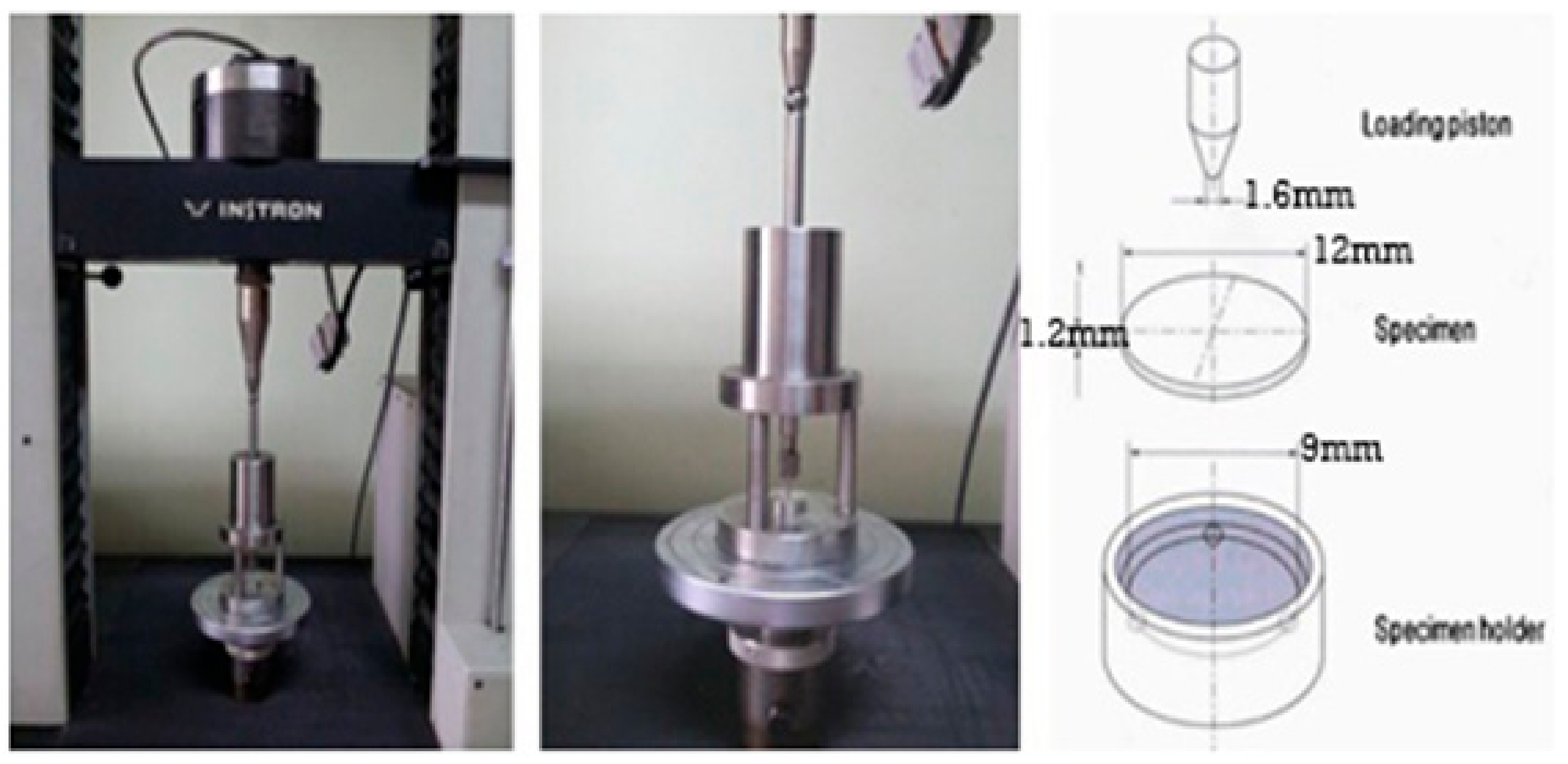
2.5. Biaxial Flexural Strength Test
2.6. Statistical Analysis
3. Results
3.1. Vickers Hardness
3.2. Wear Test
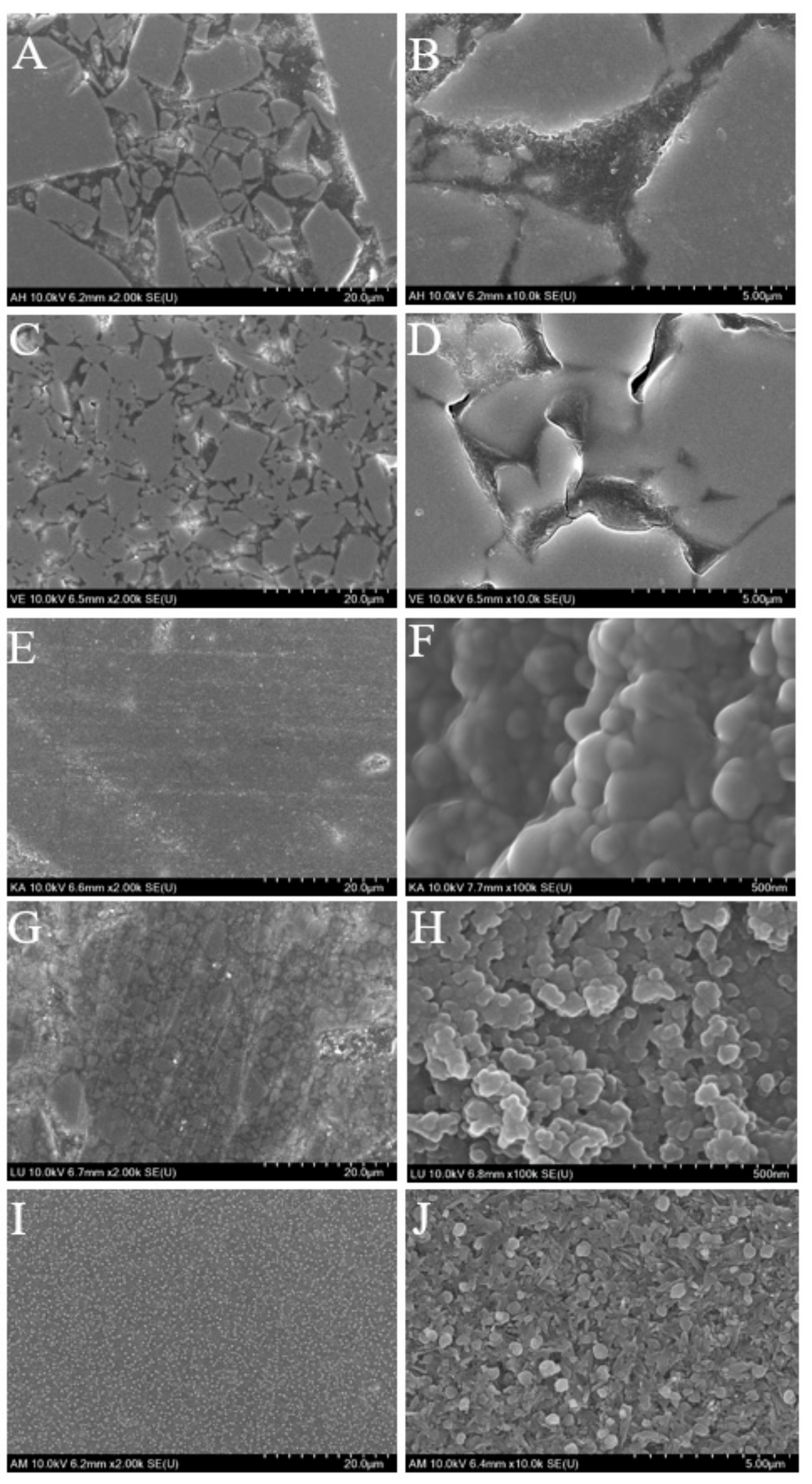
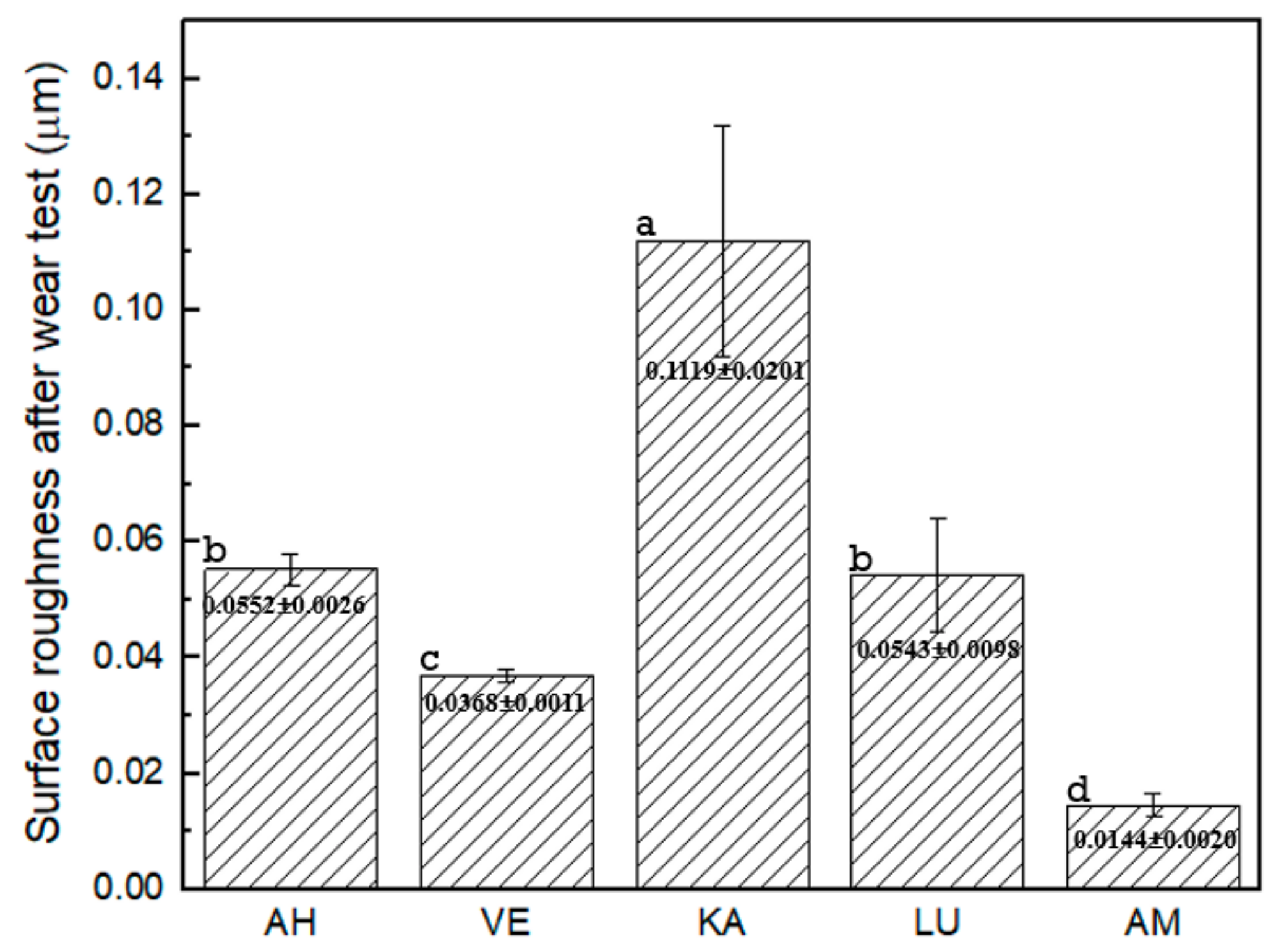
3.3. Surface Roughness after Toothbrushing
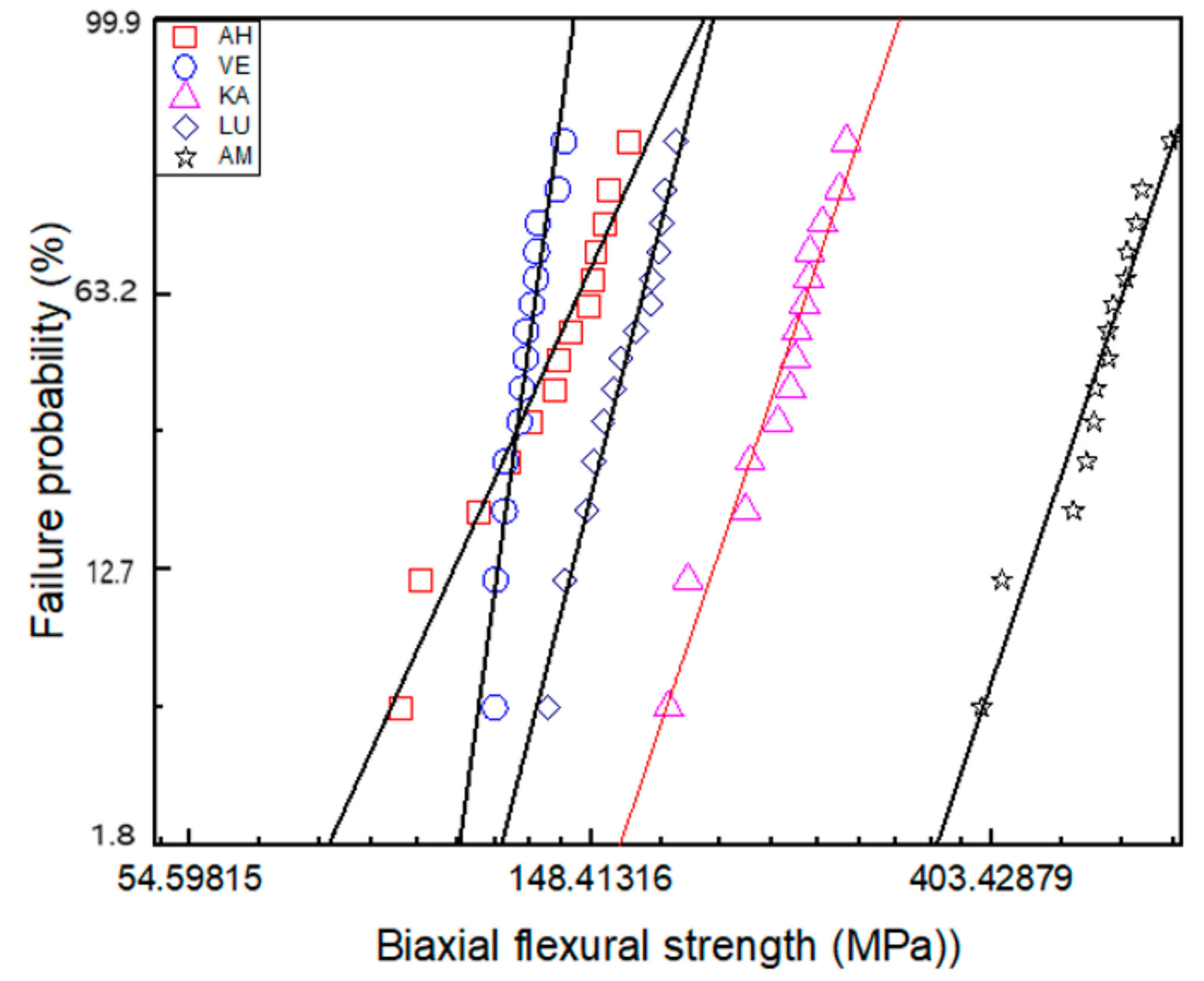
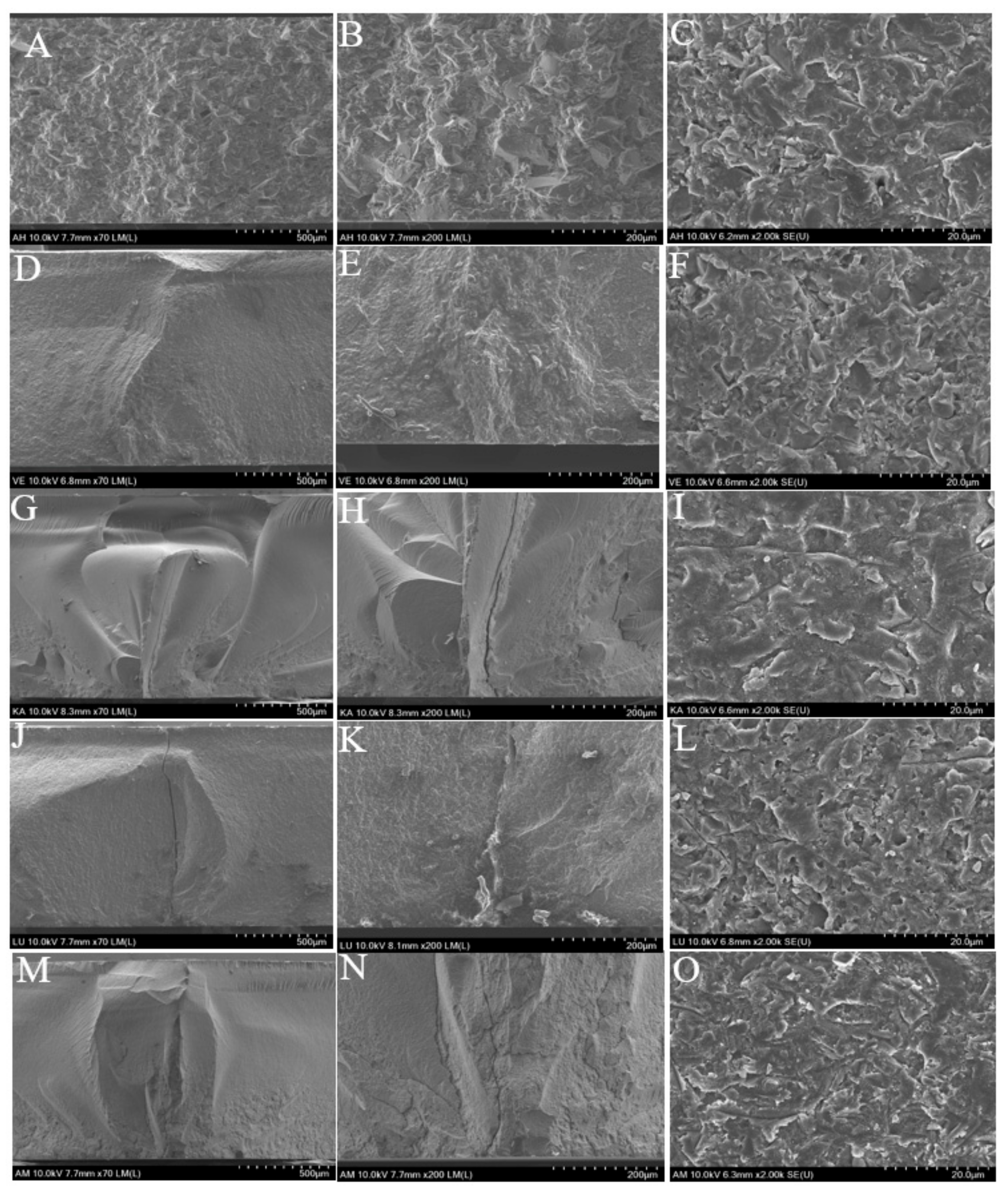
3.4. Biaxial Flexural Strength
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Giordano, R. Materials for chairside CAD/CAM–produced restorations. J. Am. Dent. Assoc. 2006, 137, 14S–21S. [Google Scholar] [CrossRef] [PubMed]
- Beuer, F.; Schweiger, J.; Edelhoff, D. Digital dentistry: An overview of recent developments for CAD/CAM generated restorations. Br. Dent. J. 2008, 204, 505–511. [Google Scholar] [CrossRef] [PubMed]
- Poticny, D.J.; Klim, J. CAD/CAM In-office Technology. J. Am. Dent. Assoc. 2010, 141, 5S–9S. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.Y.; Hickel, R.; Setcos, J.C.; Kunzelmann, K.H. Effects of surface finish and fatigue testing on the fracture strength of CAD-CAM and pressed-ceramic crowns. J. Prosthet. Dent. 1999, 82, 468–475. [Google Scholar] [CrossRef]
- Kois, D.E.; Isvilanonda, V.; Chaiyabutr, Y.; Kois, J.C. Evaluation of fracture resistance and failure risks of posterior partial coverage restorations. J. Esthet. Restor. Dent. 2013, 25, 110–122. [Google Scholar] [CrossRef] [PubMed]
- Zahran, M.; El-Mowafy, O.; Tam, L.; Watson, P.A.; Finer, Y. Fracture Strength and Fatigue Resistance of All-Ceramic Molar Crowns Manufactured with CAD/CAM Technology. J. Prosthodont. 2008, 17, 370–377. [Google Scholar] [CrossRef] [PubMed]
- Sripetchdanond, J.; Leevailoj, C. Wear of human enamel opposing monolithic zirconia, glass ceramic, and composite resin: An in vitro study. J. Prosthet. Dent. 2014, 112, 1141–1150. [Google Scholar] [CrossRef]
- Quinn, G.D.; Giuseppetti, A.A.; Hoffman, K.H. Chipping fracture resistance of dental CAD/CAM restorative materials: Part I—Procedures and results. Dent. Mater. 2014, 30, e99–e111. [Google Scholar] [CrossRef]
- Attia, A.; Abdelaziz, K.M.; Freitag, S.; Kern, M. Fracture load of composite resin and feldspathic all-ceramic CAD/CAM crowns. J. Prosthet. Dent. 2006, 95, 117–123. [Google Scholar] [CrossRef]
- Attia, A.; Kern, M. Influence of cyclic loading and luting agents on the fracture load of two all-ceramic crown systems. J. Prosthet. Dent. 2004, 92, 551–556. [Google Scholar] [CrossRef]
- Douglas, R.D. Color stability of new-generation indirect resins for prosthodontic application. J. Prosthet. Dent. 2000, 83, 166–170. [Google Scholar] [CrossRef]
- Dhawan, P.; Prakash, H.; Shah, N. Clinical and scanning electron microscopic assessments of porcelain and ceromer resin veneers. Indian J. Dent. Res. 2003, 14, 264–278. [Google Scholar] [PubMed]
- Behr, M.; Rosentritt, M.; Handel, G. Fiber-reinforced composite crowns and FPDs: A clinical report. Int. J. Prosthodont. 2003, 16, 239–243. [Google Scholar] [PubMed]
- Coldea, A.; Swain, M.V.; Thiel, N. Mechanical properties of polymer-infiltrated-ceramic-network materials. Dent. Mater. 2013, 29, 419–426. [Google Scholar] [CrossRef] [PubMed]
- Schlichting, L.H.; Maia, H.P.; Baratieri, L.N.; Magne, P. Novel-design ultra-thin CAD/CAM composite resin and ceramic occlusal veneers for the treatment of severe dental erosion. J. Prosthet. Dent. 2011, 105, 217–226. [Google Scholar] [CrossRef]
- Charlton, D.G.; Roberts, H.W.; Tiba, A. Measurement of select physical and mechanical properties of 3 machinable ceramic materials. Quintessence Int. 2008, 39, 573–579. [Google Scholar] [PubMed]
- Plotino, G.; Grande, N.M.; Bedini, R.; Pameijer, C.H.; Somma, F. Flexural properties of endodontic posts and human root dentin. Dent. Mater. 2007, 23, 1129–1135. [Google Scholar] [CrossRef]
- Hayashi, M.; Koychev, E.V.; Okamura, K.; Sugeta, A.; Hongo, C.; Okuyama, K.; Ebisu, S. Heat treatment strengthens human dentin. J. Dent. Res. 2008, 87, 762–766. [Google Scholar] [CrossRef]
- Ryou, H.; Amin, N.; Ross, A.; Eidelman, N.; Wang, D.H.; Romberg, E.; Arola, D. Contributions of microstructure and chemical composition to the mechanical properties of dentin. J. Mater. Sci. Mater. Med. 2011, 22, 1127–1135. [Google Scholar] [CrossRef]
- Dirxen, C.; Blunck, U.; Preissner, S. Clinical Performance of a New Biomimetic Double Network Material. Open Dent. J. 2013, 7, 118–122. [Google Scholar] [CrossRef]
- Turssi, C.P.; De Moraes Purquerio, B.; Serra, M.C. Wear of Dental Resin Composites: Insights into Underlying Processes and Assessment Methods—A Review. J. Biomed. Mater. Res. B Appl. Biomater. 2003, 15, 280–285. [Google Scholar] [CrossRef] [PubMed]
- Heintze, S.D.; Cavalleri, A.; Forjanic, M.; Zellweger, G.; Rousson, V. A comparison of three different methods for the quantification of the in vitro wear of dental materials. Dent. Mater. 2006, 22, 1051–1062. [Google Scholar] [CrossRef] [PubMed]
- Turssi, C.P.; Ferracane, J.L.; Ferracane, L.L. Wear and fatigue behavior of nano-structured dental resin composites. J. Biomed. Mater. Res. B Appl. Biomater. 2006, 78, 196–203. [Google Scholar] [CrossRef] [PubMed]
- Mitra, S.B.; Wu, D.; Holmes, B.N. An application of nanotechnology in advanced dental materials. J. Am. Dent. Assoc. 2003, 134, 1382–1390. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.H.K.; Quinn, J.B.; Giuseppetti, A.A. Wear and mechanical properties of nano-silica-fused whisker composites. J. Dent. Res. 2004, 83, 930–935. [Google Scholar] [CrossRef] [PubMed]
- Costa, A.R.; Correr, A.B.; Puppin-Rontani, R.M.; Vedovello, S.A.; Valdrighi, H.C.; Correr-Sobrinho, L.; Vedovello Filho, M. Effect of bonding material, etching time and silane on the bond strength of metallic orthodontic brackets to ceramic. Braz. Dent. J. 2012, 23, 223–227. [Google Scholar] [CrossRef] [PubMed]
- Yuasa, T.; Iijima, M.; Ito, S.; Muguruma, T.; Saito, T.; Mizoguchi, I. Effects of long-term storage and thermocycling on bond strength of two self-etching primer adhesive systems. Eur. J. Orthod. 2010, 32, 285–290. [Google Scholar] [CrossRef]
- Costa, A.R.; Correr, A.B.; Puppin-Rontani, R.M.; Vedovello, S.A.S.; Valdrighi, H.C.; Correr-Sobrinho, L.; Vedovello Filho, M. Effects of thermocycling and light source on the bond strength of metallic brackets to bovine teeth. Braz. Dent. J. 2011, 22, 486–489. [Google Scholar] [CrossRef]
- Peutzfeldt, A.; Asmussen, E. In vitro wear, hardness, and conversion of diacetyl-containing and propanal-containing resin materials. Dent. Mater. 1996, 12, 103–108. [Google Scholar] [CrossRef]
- Murakami, M. Surface properties of an indirect composite polymerized with five laboratory light polymerization systems. J. Oral Sci. 2009, 51, 215–221. [Google Scholar] [CrossRef][Green Version]
- Mandikos, M.N.; McGivney, G.P.; Davis, E.; Bush, P.J.; Carter, J.M. A comparison of the wear resistance and hardness of indirect composite resins. J. Prosthet. Dent. 2001, 85, 386–395. [Google Scholar] [CrossRef] [PubMed]
- Hahnel, S.; Schultz, S.; Trempler, C.; Ach, B.; Handel, G.; Rosentritt, M. Two-body wear of dental restorative materials. J. Mech. Behav. Biomed. Mater. 2011, 4, 237–244. [Google Scholar] [CrossRef] [PubMed]
- Turssi, C.P.; de Magalhaes, C.S.; Serra, M.C.; Rodrigues Junior, A.L. Surface roughness assessment of resin-based materials during brushing preceded by pH-cycling simulations. Oper. Dent. 2001, 26, 576–584. [Google Scholar] [PubMed]
- Rios, D.; Honório, H.M.; de Araújo, P.A.; de Andrade Moreira Machado, M.A. Wear and superficial roughness of glass ionomer cements used as sealants, after simulated toothbrushing. Pesqui. Odontol. Bras. 2007, 16, 343–348. [Google Scholar] [CrossRef]
- De Gee, A.J.; ten Harkel-Hagenaar, H.C.; Davidson, C.L. Structural and physical factors affecting the brush wear of dental composites. J. Dent. 1985, 13, 60–70. [Google Scholar] [CrossRef]
- Jones, P.A.; Fisher, S.E.; Wilson, H.J. Abrasivity of dentifrices on anterior restorative materials. Br. Dent. J. 1985, 158, 130–133. [Google Scholar] [CrossRef] [PubMed]
- Matinlinna, J.P. Handbook of Oral Biomaterials; CRC Press: Boca Raton, FA, USA, 2014. [Google Scholar]
- McCabe, J.F.; Carrick, T.E. A statistical approach to the mechanical testing of dental materials. Dent. Mater. 1986, 2, 139–142. [Google Scholar] [CrossRef]
- Jin, J.; Takahashi, H.; Iwasaki, N. Effect of Test Method on Flexural Strength of Recent Dental Ceramics. Dent. Mater. J. 2004, 23, 490–496. [Google Scholar] [CrossRef]
- Bakke, M.; Holm, B.; Jensen, B.L.; Michler, L.; Møller, E. Unilateral, isometric bite force in 8-68-year-old women and men related to occlusal factors. Eur. J. Oral Sci. 1990, 98, 149–158. [Google Scholar] [CrossRef]
- Helkimo, E.; Carlsson, G.E.; Helkimo, M. Bite force and state of dentition. Acta Odontol. Scand. 1977, 35, 297–303. [Google Scholar] [CrossRef]
- Suzuki, S.; Leinfelder, K.F.; Kawai, K.; Tsuchitani, Y. Effect of particle variation on wear rates of posterior composites. Am. J. Dent. 1995, 8, 173–178. [Google Scholar] [PubMed]
- Asmussen, E.; Peutzfeldt, A. Influence of UEDMA, BisGMA and TEGDMA on selected mechanical properties of experimental resin composites. Dent. Mater. 1998, 14, 51–56. [Google Scholar] [CrossRef]
- Opdam, N.J.M.; Roeters, J.J.M.; Joosten, M.; Veeke, O. Vd Porosities and voids in Class I restorations placed by six operators using a packable or syringable composite. Dent. Mater. 2002, 18, 58–63. [Google Scholar] [CrossRef]



| Material | Code | Company | Lot No. | Monomer Composition | Filler Composition | Filler Mass (%) |
|---|---|---|---|---|---|---|
| Amber Mill Hybrid | AH | Hass, Kangreung, Korea | Prototype | UDMA, TEGDMA | Crystalline glass | 76 |
| Vita Enamic | VE | Vita Zahnfabrik, Germany | 2M2-T(754101) | UDMA, TEGDMA | Feldspar ceramic enriched with aluminum oxide | 86 |
| Katana Avencia | KA | Kuraray Noritake, Tokyo, Japan | A2-LT(000015) | UDMA, methacrylate monomer | SiO2 (40 nm), Al2O3 (20 nm) | 62 |
| Lava Ultimate | LU | 3M ESPE, Saint Paul, MN, USA | A2-HT(N826384) | Bis-GMA, UDMA, Bis-EMA, TEGDMA | SiO2 (20 nm), ZrO2(4–11 nm), ZrO2/SiO2 clusters | 80 |
| Amber Mill | AM | Hass, Kangreung, Korea | A2(EBE06KJ0202) | - | Crystalline Lithium disilicate ceramic | - |
| Material | Δm (mg) | ρ (g/cm3) | ΔV (mm3) | ΔVrelw (%) |
|---|---|---|---|---|
| AH | 0.067 ± 0.047 | 1.927 ± 0.011 | 0.035 ± 0.025 | 0.92 ± 0.673 |
| VE | 0.1 ± 0.082 | 1.947 ± 0.006 | 0.051 ± 0.042 | 1.29 ± 0.955 |
| KA | 0.267 ± 0.047 | 2.769 ± 0.032 | 0.096 ± 0.018 | 2.977 ± 0.375 |
| LU | 0.133 ± 0.047 | 2.107 ± 0.007 | 0.063 ± 0.022 | 2.023 ± 0.073 |
| AM | 0.1 ± 0.001 | 1.708 ± 0.003 | 0.059 ± 0.0005 | 1.893 ± 0.514 |
| Acrylic (Reference material) | 3.8 ± 1.023 | 1.141 ± 0.002 | 3.332 ± 0.901 | - |
| AH | VE | KA | LU | AM | |
|---|---|---|---|---|---|
| m | 6.40 | 20.94 | 8.58 | 11.33 | 8.63 |
| σmax | 163 | 138.9 | 281 | 183.7 | 631.1 |
| σf ± SD | 134.34 ± 6.40 | 126.34 ± 6.63 | 240.88 ± 29.62 | 161.93 ± 11.33 | 529.46 ± 63.67 |
| BP | 2.14 ± 0.35 | 2.93 ± 0.26 | 5.64 ± 1.23 | 3.29 ± 0.59 | 6.36 ± 1.17 |
| N | 14 | 14 | 14 | 14 | 14 |
| R2 | 0.96 | 0.92 | 0.96 | 0.98 | 0.94 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yin, R.; Jang, Y.-S.; Lee, M.-H.; Bae, T.-S. Comparative Evaluation of Mechanical Properties and Wear Ability of Five CAD/CAM Dental Blocks. Materials 2019, 12, 2252. https://doi.org/10.3390/ma12142252
Yin R, Jang Y-S, Lee M-H, Bae T-S. Comparative Evaluation of Mechanical Properties and Wear Ability of Five CAD/CAM Dental Blocks. Materials. 2019; 12(14):2252. https://doi.org/10.3390/ma12142252
Chicago/Turabian StyleYin, Ruizhi, Yong-Seok Jang, Min-Ho Lee, and Tae-Sung Bae. 2019. "Comparative Evaluation of Mechanical Properties and Wear Ability of Five CAD/CAM Dental Blocks" Materials 12, no. 14: 2252. https://doi.org/10.3390/ma12142252
APA StyleYin, R., Jang, Y.-S., Lee, M.-H., & Bae, T.-S. (2019). Comparative Evaluation of Mechanical Properties and Wear Ability of Five CAD/CAM Dental Blocks. Materials, 12(14), 2252. https://doi.org/10.3390/ma12142252





