Copper Alloy Touch Surfaces in Healthcare Facilities: An Effective Solution to Prevent Bacterial Spreading
Abstract
:1. Introduction
2. Materials and Methods
2.1. In Situ Approach: Environmental Contaminations of Frequently Touch Surfaces
2.1.1. Long-Term Care Facilities Environment and Study Design
2.1.2. Sampling Protocol
2.1.3. Bacteria Recovery and Culture
2.2. In Vitro Approach: Anti MRSA Standardized Activity of “in Use” Copper Door Handles
2.2.1. Door Handle Collection
2.2.2. Preparation of the Handles
2.2.3. Methicillin-Resistant Staphylococcus aureus Strain Preparation
2.2.4. Bacterial Viability on Door Handles
2.3. Statistical Analysis
3. Results
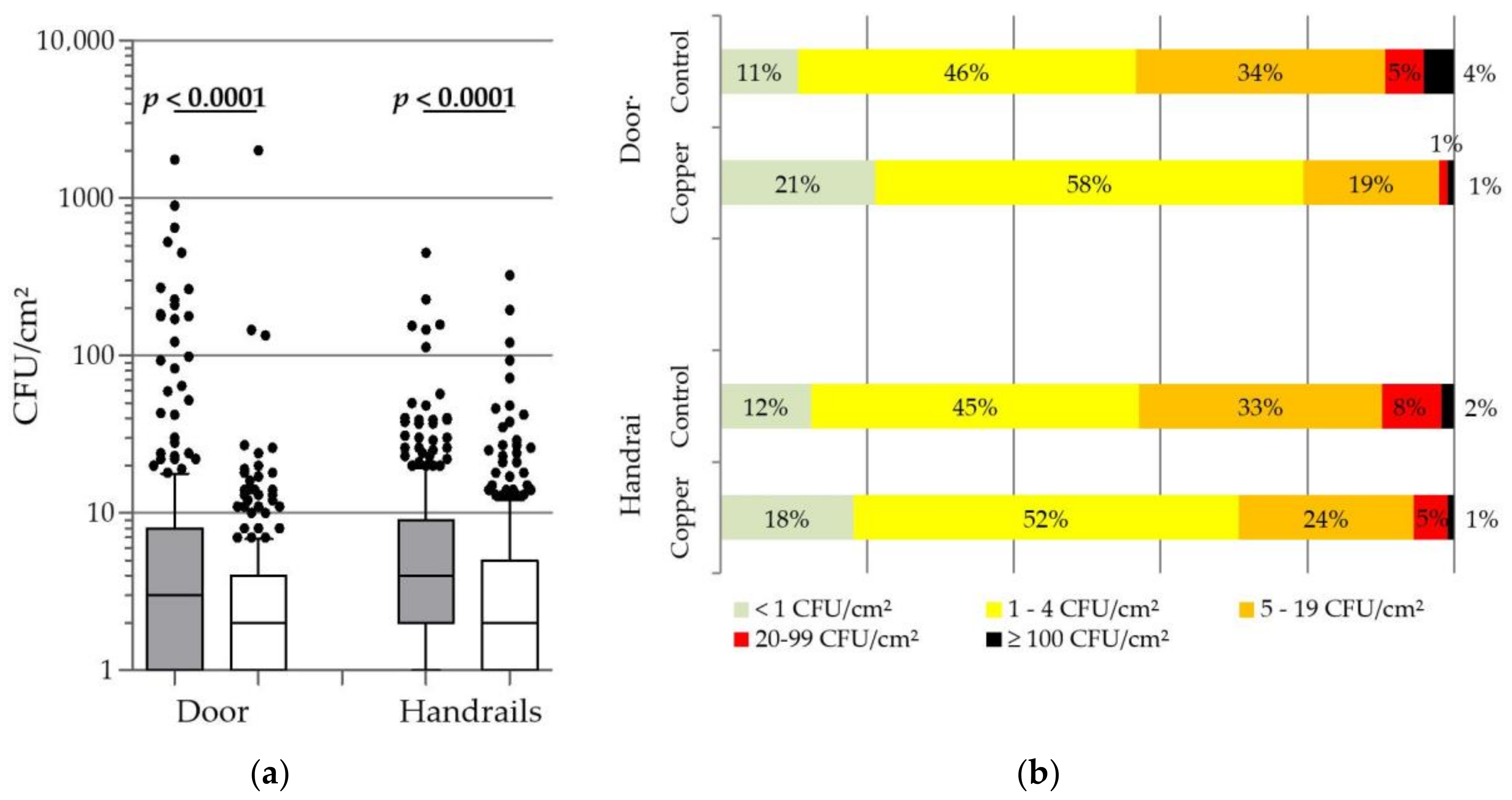
3.1. Global Dispersion of the Bacterial Contamination
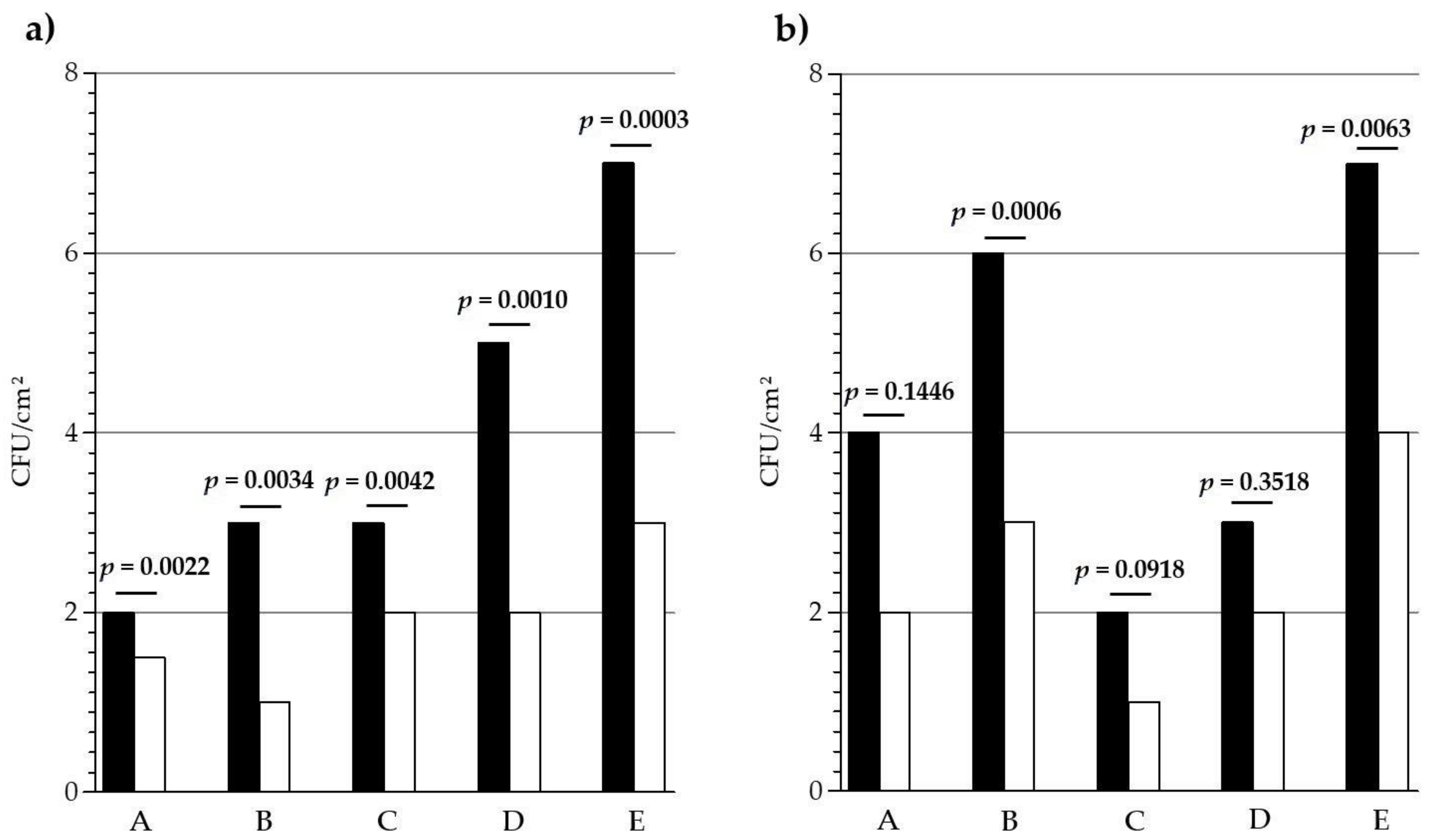
3.2. Bacterial Contamination by Long-Term Care Facility
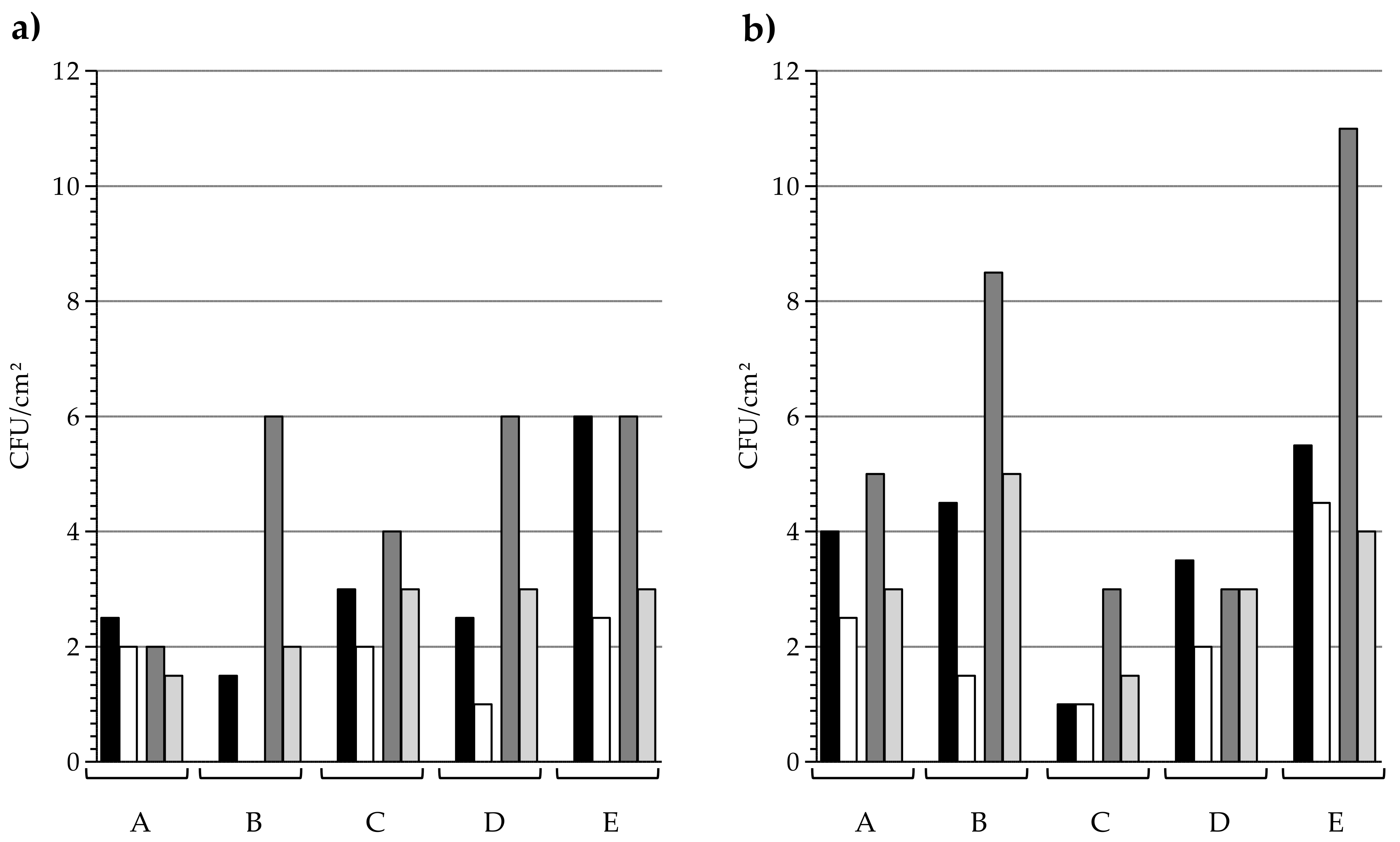
3.3. In Situ Persistence of the Copper Antibacterial Activity
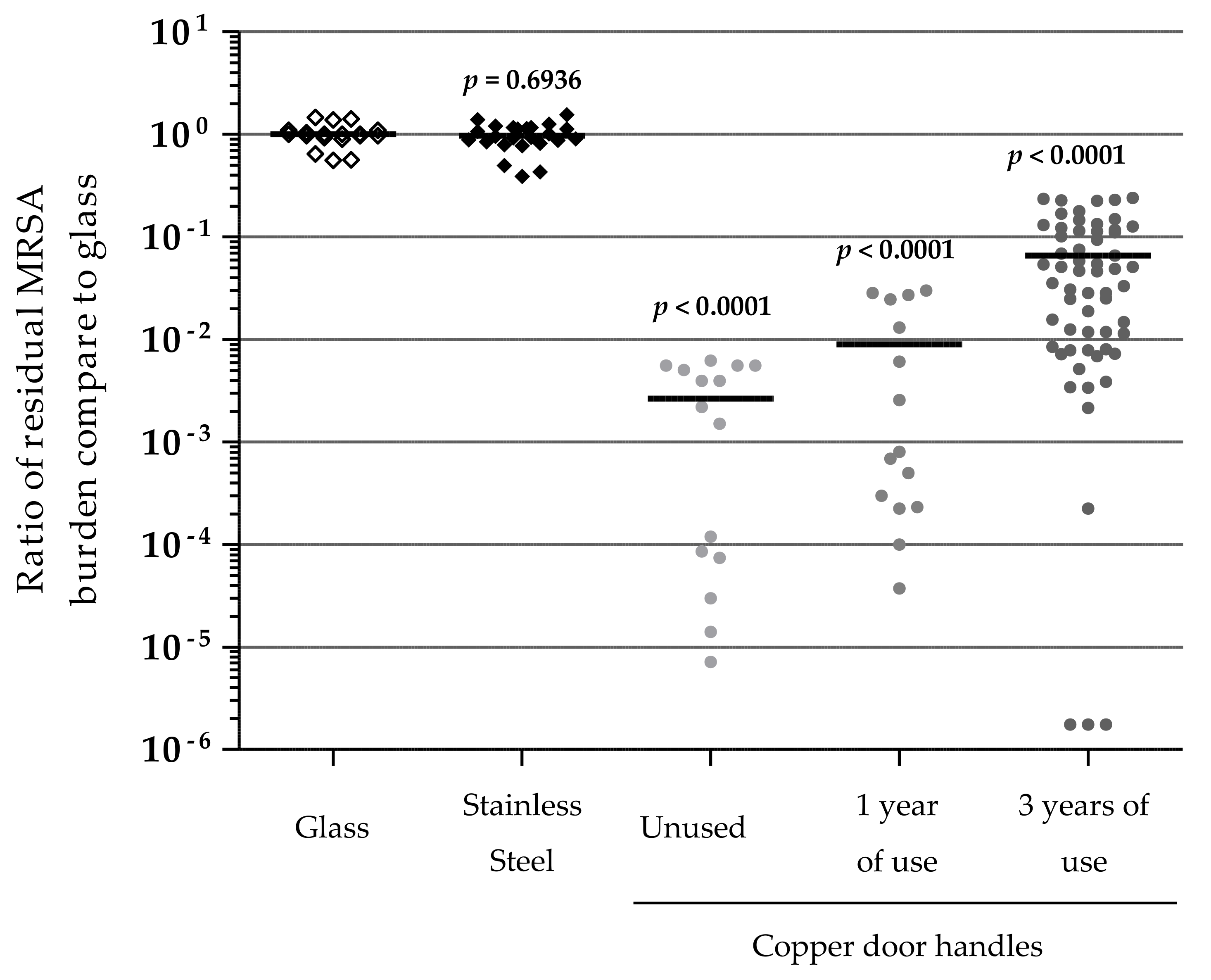
3.4. In Vitro Evaluation of Door Handles Activity against MRSA
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Magill, S.S.; Edwards, J.R.; Bamberg, W.; Beldavs, Z.G.; Dumyati, G.; Kainer, M.A.; Lynfield, R.; Maloney, M.; McAllister-Hollod, L.; Nadle, J.; et al. Multistate point-prevalence survey of health care–associated infections. N. Engl. J. Med. 2014, 370, 1198–1208. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control. Point Prevalence Survey of Healthcare-Associated Infections and Antimicrobial Use in European Acute Care Hospitals; ECDC: Stockholm, Sweden, 2013. [Google Scholar]
- Harris, A.D.; Perencevich, E.N.; Johnson, J.K.; Paterson, D.L.; Morris, J.G.; Strauss, S.M.; Johnson, J.A. Patient-to-patient transmission is important in extended-spectrum β-lactamase–producing Klebsiella pneumoniae acquisition. Clin. Infect. Dis. 2007, 45, 1347–1350. [Google Scholar] [CrossRef] [PubMed]
- Weber, D.J.; Anderson, D.; Rutala, W.A. The role of the surface environment in healthcare-associated infections. Curr. Opin. Infect. Dis. 2013, 26, 338–344. [Google Scholar] [CrossRef] [PubMed]
- Hayden, M.K.; Blom, D.W.; Lyle, E.A.; Moore, C.G.; Weinstein, R.A. Risk of hand or glove contamination after contact with patients colonized with vancomycin-resistant enterococcus or the colonized patients’ environment. Infect. Control Hosp. Epidemiol. 2008, 29, 149–154. [Google Scholar] [CrossRef] [PubMed]
- McBryde, E.S.; Bradley, L.C.; Whitby, M.; McElwain, D.L.S. An investigation of contact transmission of methicillin-resistant Staphylococcus aureus. J. Hosp. Infect. 2004, 58, 104–108. [Google Scholar] [CrossRef] [PubMed]
- De la Rosa-Zamboni, D.; Ochoa, S.A.; Laris-González, A.; Cruz-Córdova, A.; Escalona-Venegas, G.; Pérez-Avendaño, G.; Torres-García, M.; Suaréz-Mora, R.; Castellanos-Cruz, C.; Sánchrez-Flores, Y.V.; et al. Everybody hands-on to avoid ESKAPE: Effect of sustained hand hygiene compliance on healthcare-associated infections and multidrug resistance in a paediatric hospital. J. Med. Microbiol. 2018, 67, 1761–1771. [Google Scholar] [CrossRef] [PubMed]
- Otter, J.A.; Yezli, S.; Salkeld, J.A.; French, G.L. Evidence that contaminated surfaces contribute to the transmission of hospital pathogens and an overview of strategies to address contaminated surfaces in hospital settings. Am. J. Infect. Control 2013, 41, S6–S11. [Google Scholar] [CrossRef] [PubMed]
- Sexton, T.; Clarke, P.; O’Neill, E.; Dillane, T.; Humphreys, H. Environmental reservoirs of methicillin-resistant Staphylococcus aureus in isolation rooms: Correlation with patient isolates and implications for hospital hygiene. J. Hosp. Infect. 2006, 62, 187–194. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, B.G.; Dancer, S.J.; Anderson, M.; Dehn, E. Risk of organism acquisition from prior room occupants: A systematic review and meta-analysis. J. Hosp. Infect. 2015, 91, 211–217. [Google Scholar] [CrossRef]
- Attaway, H.H.; Fairey, S.; Steed, L.L.; Salgado, C.S.; Michels, H.T.; Schmidt, M.G. Intrinsic bacterial burden associated with intensive care unit hospital beds: Effects of disinfection on population recovery and mitigation of potential infection risk. Am. J. Infect. Control 2012, 40, 907–912. [Google Scholar] [CrossRef] [PubMed]
- Kramer, A.; Schwebke, I.; Kampf, G. How long do nosocomial pathogens persist on inanimate surfaces? A systematic review. BMC Infect. Dis. 2006, 6, 130. [Google Scholar] [CrossRef] [PubMed]
- Hardy, K.J.; Gossain, S.; Henderson, N.; Drugan, C.; Oppenheim, B.A.; Gao, F.; Hawkey, P.M. Rapid recontamination with MRSA of the environment of an intensive care unit after decontamination with hydrogen peroxide vapour. J. Hosp. Infect. 2007, 66, 360–368. [Google Scholar] [CrossRef] [PubMed]
- Clement, J.L.; Jarrett, P.S. Antimicrobial silver. Met. Based Drugs 1994, 1, 467–482. [Google Scholar] [CrossRef] [PubMed]
- Cho, M.; Chung, H.; Choi, W.; Yoon, J. Linear correlation between inactivation of E. coli and OH radical concentration in TiO2 photocatalytic disinfection. Water Res. 2004, 38, 1069–1077. [Google Scholar] [CrossRef]
- Cho, M.; Chung, H.; Choi, W.; Yoon, J. Different inactivation behaviors of MS-2 phage and Escherichia coli in TiO2 photocatalytic disinfection. Appl. Environ. Microb. 2005, 71, 270–275. [Google Scholar] [CrossRef]
- Kikuchi, Y.; Sunada, K.; Iyoda, T.; Hashimoto, K.; Fujishima, A. Photocatalytic bactericidal effect of TiO2 thin films: Dynamic view of the active oxygen species responsible for the effect. J. Photochem. Photobiol. Chem. 1997, 106, 51–56. [Google Scholar] [CrossRef]
- Oh, Y.J.; Hubauer-Brenner, M.; Hinetrdorfer, P. Influence of surface morphology on the antimicrobial effect of transistion metal oxides in polymer surface. J. Nanosci. Nanotechnol. 2015, 15, 7853–7859. [Google Scholar] [CrossRef]
- Sunada, K.; Minoshima, M.; Hashimoto, K. Highly efficient antiviral and antibacterial activities of solid-state cuprous compounds. J. Hazard. Mater. 2012, 235, 265–270. [Google Scholar] [CrossRef]
- Mehtar, S.; Wiid, I.; Todorov, S.D. The antimicrobial activity of copper and copper alloys against nosocomial pathogens and Mycobacterium tuberculosis isolated from healthcare facilities in the Western Cape: An in-vitro study. J. Hosp. Infect. 2008, 68, 45–51. [Google Scholar] [CrossRef]
- Quaranta, D.; Krans, T.; Santo, C.E.; Elowsky, C.G.; Domaille, D.W.; Chang, C.J.; Grass, G. Mechanisms of contact-mediated killing of yeast cells on dry metallic copper surfaces. Appl. Environ. Microb. 2011, 77, 416–426. [Google Scholar] [CrossRef] [PubMed]
- Santo, C.E.; Lam, E.W.; Elowsky, C.G.; Quaranta, D.; Domaille, D.W.; Chang, C.J.; Grass, G. Bacterial killing by dry metallic copper surfaces. Appl. Environ. Microb. 2011, 77, 794–802. [Google Scholar] [CrossRef] [PubMed]
- Warnes, S.L.; Summersgill, E.N.; Keevil, C.W. Inactivation of murine norovirus on a range of copper alloy surfaces is accompanied by loss of capsid integrity. Appl. Environ. Microb. 2015, 81, 1085–1091. [Google Scholar] [CrossRef]
- Warnes, S.L.; Little, Z.R.; Keevil, C.W. Human coronavirus 229E remains infectious on common touch surface materials. MBio 2015, 6, e01697-15. [Google Scholar] [CrossRef] [PubMed]
- Warnes, S.L.; Keevil, C.W. Inactivation of norovirus on dry copper alloy surfaces. PLoS ONE 2013, 8, e75017. [Google Scholar] [CrossRef] [PubMed]
- Weaver, L.; Noyce, J.O.; Michels, H.T.; Keevil, C.W. Potential action of copper surfaces on meticillin-resistant Staphylococcus aureus. J. Appl. Microbiol. 2010, 109, 2200–2205. [Google Scholar] [CrossRef] [PubMed]
- Weaver, L.; Michels, H.T.; Keevil, C.W. Survival of Clostridium difficile on copper and steel: Futuristic options for hospital hygiene. J. Hosp. Infect. 2008, 68, 145–151. [Google Scholar] [CrossRef] [PubMed]
- Wheeldon, L.J.; Worthington, T.; Lambert, P.A.; Hilton, A.C.; Lowden, C.J.; Elliott, T.S. Antimicrobial efficacy of copper surfaces against spores and vegetative cells of Clostridium difficile: The germination theory. J. Antimicrob. Chemother. 2008, 62, 522–525. [Google Scholar] [CrossRef] [PubMed]
- Grass, G.; Rensing, C.; Solioz, M. Metallic copper as an antimicrobial surface. Appl. Environ. Microb. 2011, 77, 1541–1547. [Google Scholar] [CrossRef]
- Liu, S.; Zhang, X.X. Small colony variants are more susceptible to copper-mediated contact killing for Pseudomonas aeruginosa and Staphylococcus aureus. J. Med. Microbiol. 2016, 65, 1143–1151. [Google Scholar] [CrossRef]
- Mathews, S.; Hans, M.; Mücklich, F.; Solioz, M. Contact killing of bacteria on copper is suppressed if bacteria-metal contact is prevented and is induced on iron by copper ions. Appl. Environ. Microb. 2013, AEM-03608. [Google Scholar] [CrossRef]
- Société Française de Microbiologie. Staphylococcus spp.; CASFM/EUCAST; Société Française de Microbiologie: Paris, France, 2017; pp. 52–60. [Google Scholar]
- Neely, A.N. A survey of gram-negative bacteria survival on hospital fabrics and plastics. J. Burn Care Rehabil. 2000, 21, 523–527. [Google Scholar] [CrossRef] [PubMed]
- Casey, A.L.; Adams, D.; Karpanen, T.J.; Lambert, P.A.; Cookson, B.D.; Nightingale, P.; Miruszebko, L.; Shillam, R.; Christian, P.; Elliot, T.S.J. Role of copper in reducing hospital environment contamination. J. Hosp. Infect. 2010, 74, 72–77. [Google Scholar] [CrossRef] [PubMed]
- Hinsa-Leasure, S.M.; Nartey, Q.; Vaverka, J.; Schmidt, M.G. Copper alloy surfaces sustain terminal cleaning levels in a rural hospital. Am. J. Infect. Control 2016, 44, e195–e203. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, Z.; Petrusan, A.J.; Hooke, P.; Hinsa-Leasure, S.M. Reduction of bacterial burden by copper alloys on high-touch athletic center surfaces. Am. J. Infect. Control 2018, 46, 197–201. [Google Scholar] [CrossRef] [PubMed]
- Inkinen, J.; Mäkinen, R.; Keinänen-Toivola, M.M.; Nordström, K.; Ahonen, M. Copper as an antibacterial material in different facilities. Lett. Appl. Microbiol. 2017, 64, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Karpanen, T.J.; Casey, A.L.; Lambert, P.A.; Cookson, B.D.; Nightingale, P.; Miruszenko, L.; Elliott, T.S. The antimicrobial efficacy of copper alloy furnishing in the clinical environment: A crossover study. Infect. Control Hosp. Epidemiol. 2012, 33, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Mikolay, A.; Huggett, S.; Tikana, L.; Grass, G.; Braun, J.; Nies, D.H. Survival of bacteria on metallic copper surfaces in a hospital trial. Appl. Microbiol. Biotechnol. 2010, 87, 1875–1879. [Google Scholar] [CrossRef] [PubMed]
- Rai, S.; Hirsch, B.E.; Attaway, H.H.; Nadan, R.; Fairey, S.; Hardy, J.; Miller, G.; Armellino, D.; Moran, W.R.; Sharpe, P.; et al. Evaluation of the antimicrobial properties of copper surfaces in an outpatient infectious disease practice. Infect. Control Hosp. Epidemiol. 2012, 33, 200–201. [Google Scholar] [CrossRef]
- Schmidt, M.G.; von Dessauer, B.; Benavente, C.; Benavente, C.; Benadof, D.; Cifuentes, P.; Elgueta, A.; Duran, C.; Navarrete, M.S. Copper surfaces are associated with significantly lower concentrations of bacteria on selected surfaces within a pediatric intensive care unit. Am. J. Infect. Control 2016, 44, 203–209. [Google Scholar] [CrossRef]
- Schmidt, M.G.; Attaway, H.H.; Sharpe, P.A.; John, J., Jr.; Sepkowitz, K.A.; Morgan, A.; Fairey, S.E.; Singh, S.; Steed, L.L.; Cantey, J.R.; et al. Sustained reduction of microbial burden on common hospital surfaces through introduction of copper. J. Clin. Microbiol. 2012, 50, 2217–2223. [Google Scholar] [CrossRef] [PubMed]
- Souli, M.; Antoniadou, A.; Katsarolis, I.; Mavrou, I.; Paramythiotou, E.; Papadomichelakis, E.; Drogari-Apiranthitou, M.; Panagea, T.; Giamarellou, H.; Petrikkos, G.; et al. Reduction of environmental contamination with multidrug-resistant bacteria by copper-alloy coating of surfaces in a highly endemic setting. Infect. Control Hosp. Epidemiol. 2017, 38, 765–771. [Google Scholar] [CrossRef] [PubMed]
- Airey, P.; Verran, J. Potential use of copper as a hygienic surface; problems associated with cumulative soiling and cleaning. J. Hosp. Infect. 2007, 67, 271–277. [Google Scholar] [CrossRef] [PubMed]
- Savey, A.; Machut, A.; Barreto, C. Enquête Nationale de Prévalence des infections associées aux soins et des traitements antibiotiques en Établissements d’hébergement pour personnes âgées dépendantes (Ehpad); Résultats nationaux 2016; Santé publique France: Saint-Maurice, France, 2017; p. 67. [Google Scholar]
- Rampling, A.; Wiseman, S.; Davis, L.; Hyett, A.P.; Walbridge, A.N.; Payne, G.C.; Cornaby, A.J. Evidence that hospital hygiene is important in the control of methicillin-resistant Staphylococcus aureus. J. Hosp. Infect. 2001, 49, 109–116. [Google Scholar] [CrossRef] [PubMed]
| Long-Term Care Facilities | A | B | C | D | E |
|---|---|---|---|---|---|
| Total Number of rooms | 82 | 117 | 24 | 56 | 347 |
| Copper outfitted rooms | 43 | 54 | 12 | 30 | 158 |
| Number of employees (Full-time equivalent) | 55 | 71 | 6 | 33 | 193 |
| Control handles | PVC | PVC | Stainless steel | Aluminium or PVC | PVC |
| Control handrails | Wood | PVC | PVC | Aluminium or Wood | Wood |
| Surface cleaning solution used | Diesin HG a | APESIN Clean Bacto b | D10.1 c | Helispray A d or water on copper surfaces | Aniosurf e |
| Surface disinfection frequency | 1/day | 1/day | 1/day | 1/day | 1/day |
| Copper installation date | 07/2014 | 07/2014 | 10/2014 | 06/2014 | 06/2014 |
| Seq 1 dates | 06 June 2016 13 June 2016 20 June 2016 | 07 June 2016 14 June2016 21 June 2016 | 28 June 2016 04 July 2016 18 July 2016 | 27 March 2017 03 March 2017 10 April 2017 | 03 October 2016 10 October 2016 17 October 2016 |
| Seq 2 date | 06 February 2017 | 13 February 2017 | 13 February 2017 | 06 June 2017 | 16 June 2017 |
| Seq 3 dates | 11 September 2017 18 September 2017 25 September 2017 | 26 September 2017 03 October 2017 10 October 2017 | 02 October 2017 09 October 2017 14 November 2017 | 16 October 2017 06 November 2017 13 November 2017 | 20 November 2017 27 November 2017 04 December 2017 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Colin, M.; Klingelschmitt, F.; Charpentier, E.; Josse, J.; Kanagaratnam, L.; De Champs, C.; Gangloff, S.C. Copper Alloy Touch Surfaces in Healthcare Facilities: An Effective Solution to Prevent Bacterial Spreading. Materials 2018, 11, 2479. https://doi.org/10.3390/ma11122479
Colin M, Klingelschmitt F, Charpentier E, Josse J, Kanagaratnam L, De Champs C, Gangloff SC. Copper Alloy Touch Surfaces in Healthcare Facilities: An Effective Solution to Prevent Bacterial Spreading. Materials. 2018; 11(12):2479. https://doi.org/10.3390/ma11122479
Chicago/Turabian StyleColin, Marius, Flora Klingelschmitt, Emilie Charpentier, Jérôme Josse, Lukshe Kanagaratnam, Christophe De Champs, and Sophie C. Gangloff. 2018. "Copper Alloy Touch Surfaces in Healthcare Facilities: An Effective Solution to Prevent Bacterial Spreading" Materials 11, no. 12: 2479. https://doi.org/10.3390/ma11122479
APA StyleColin, M., Klingelschmitt, F., Charpentier, E., Josse, J., Kanagaratnam, L., De Champs, C., & Gangloff, S. C. (2018). Copper Alloy Touch Surfaces in Healthcare Facilities: An Effective Solution to Prevent Bacterial Spreading. Materials, 11(12), 2479. https://doi.org/10.3390/ma11122479





