Thermal Comfort of Older People: Validation of the MPMV Model
Abstract
1. Introduction
2. Method
2.1. Description of the MPMV Index for Older People
2.2. Climate Chamber Studies
2.3. Field Studies
2.4. Model Simulation
3. Results
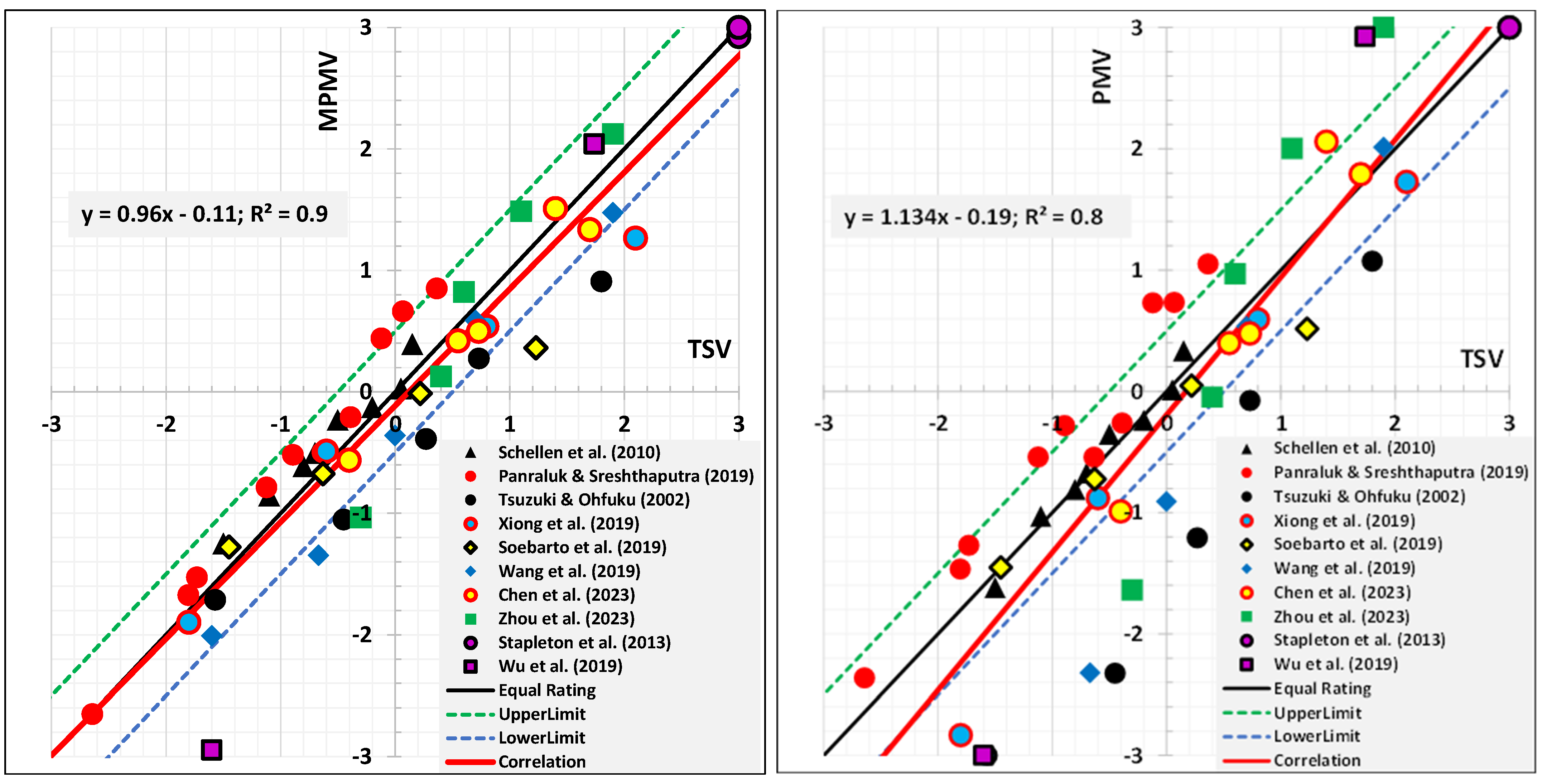
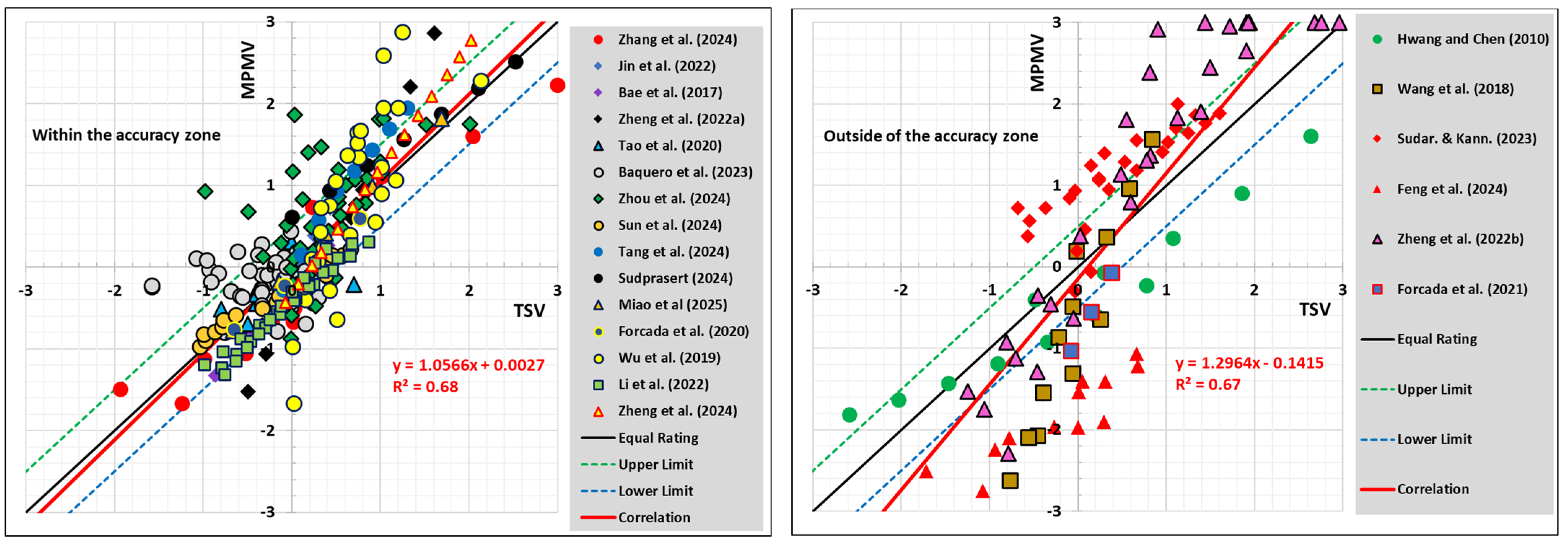
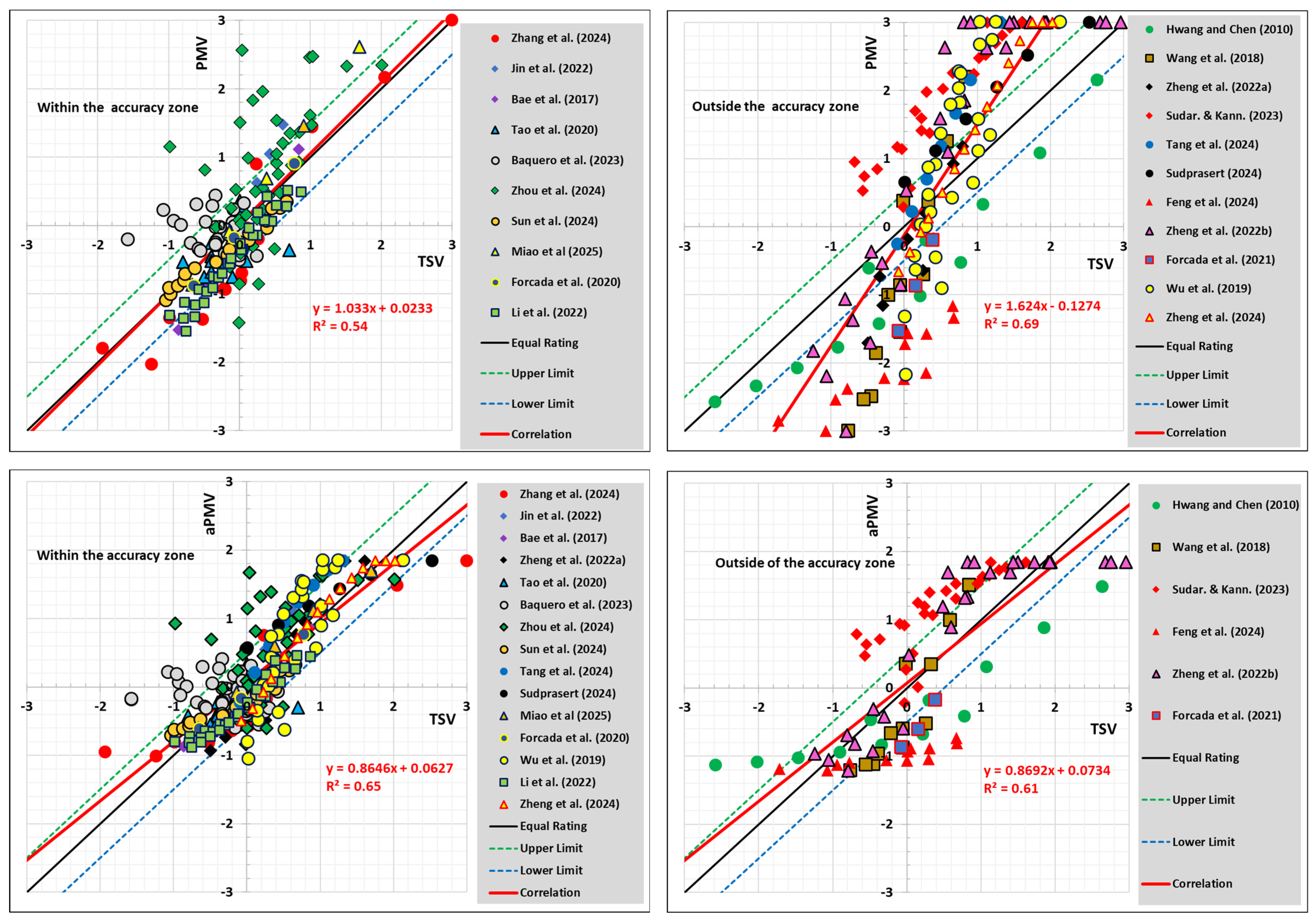
3.1. Climate Chamber Studies
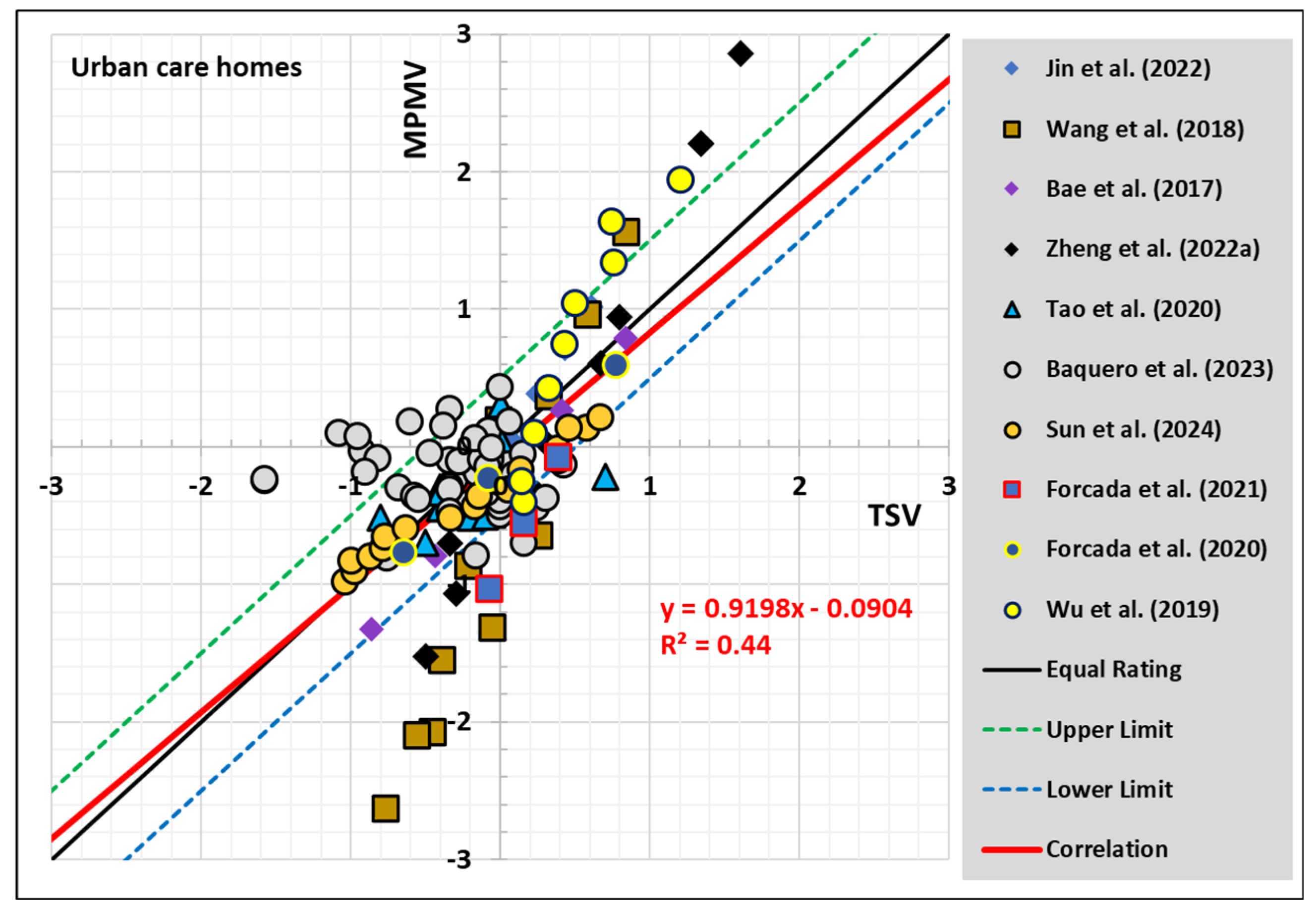
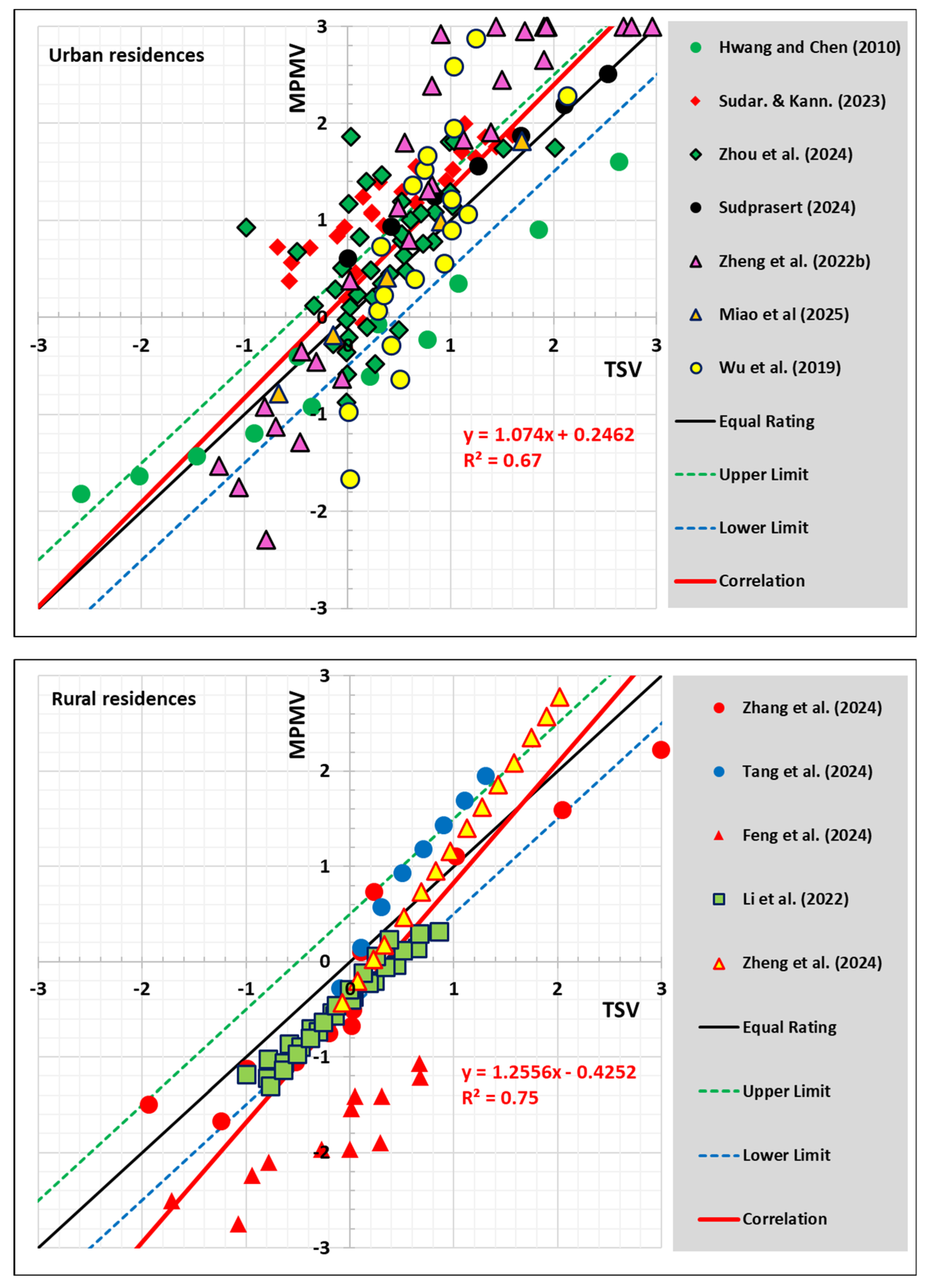
3.2. Field Studies
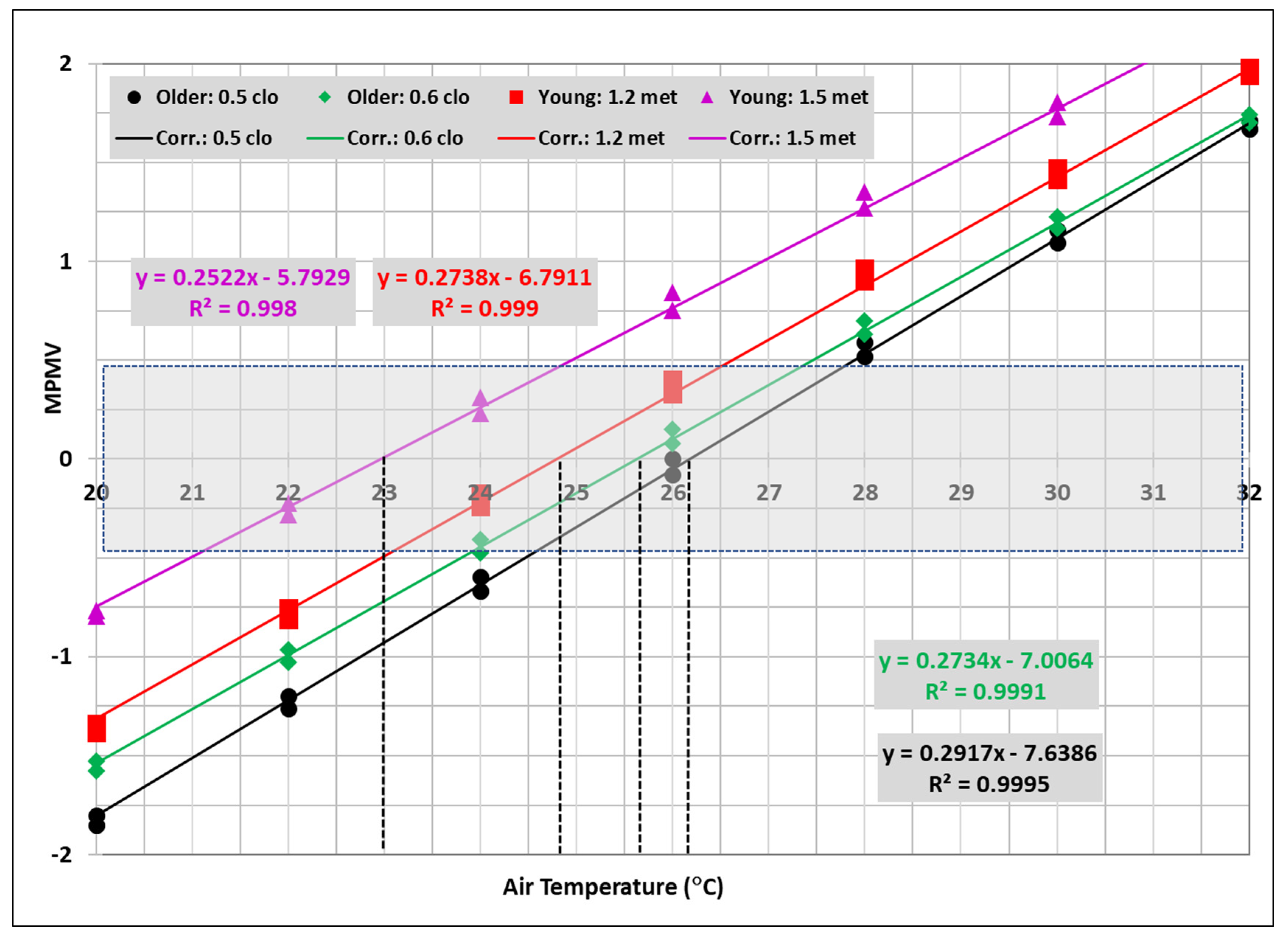
3.3. Comfort Requirements for Older People
4. Discussion
- Transient effects. Field comfort data are reported for average indoor conditions (time or space or both) and activity level of residents during survey periods. However, field environmental conditions are not controlled and may vary throughout the day or across different spaces in a building. Similarly, residents may undertake different activity levels and move between spaces before surveys, depending on building type. Physiological and psychological responses to these transient effects may never reach (or need longer times to reach) the steady state conditions, particularly under cold exposure, thus resulting in body heat storage, which in turn will alter thermal sensation.
- Misestimation of subject data. Subject data include ensemble clothing insulation and metabolic rate of activity. In field studies, clothing information is collected during survey periods, and their overall insulation values are estimated using various existing correlations. For single-layer clothing, such as that used in summers (Icl < 1 clo), insulation value is easier to estimate, but multilayer clothing, such as that used in cold winters (Icl > 1 clo), poses challenges. For example, Wang et al. [62] used a formula that can result in a 25% lower insulation value than the ISO 9920:2007 [75] formula for winter clothing. Recently, Tang et al. (2022) [76] showed that the mean absolute error (MAE) in estimating the ensemble clothing insulation using the ISO 9920:2007 [75] formula may reach 0.31 clo for multilayer clothing with Icl > 1.5 clo.
- Similarly, metabolic rate of subjects during survey periods is challenging to determine due to many uncontrolled factors. First, metabolic rate is affected by prior changes in subject activity levels whose effects would require up to ten minutes to vanish [79]. Second, food intake prior to survey periods can increase metabolic rate (diet-induced thermogenesis) by 10 to 15% [80]). Third, drinking more than 0.5 L of cold water could increase metabolic rate (water-induced thermogenesis) by up to 25 to 30% [81,82].
- Effects of the mean radiant temperature (Tr). Most of the field studies (Table 2) did not provide detailed inputs of Tr in parallel with the air temperature, and therefore, Tr had to be assumed to be equal to the air temperature. This assumption may, however, result in significant differences in the computed thermal sensation votes. For example, increasing or decreasing Tr by more than 3 °C from the air temperature would result in more than ±0.45 units of difference in thermal sensation votes.
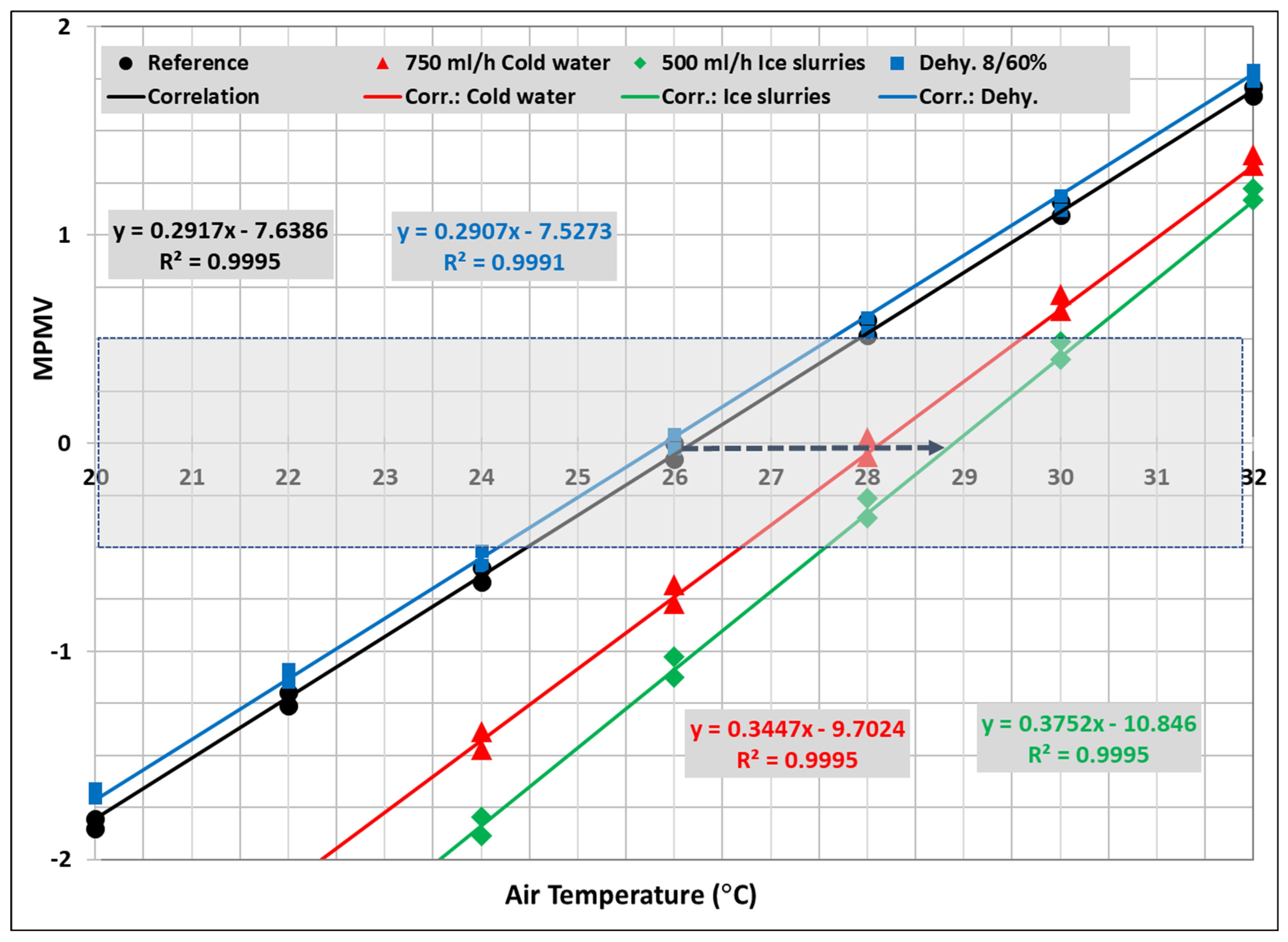
- Effect of Qex. Heat removal from or addition to the body core affects the physiological response and therefore thermal sensation. Heat removal or addition by ingesting cold or hot drinks was reported as one of the effective adaptations means to reduce heat stress and thermal discomfort [22,44,56,83]. Figure 7 shows how thermal sensation of urban older residents is affected by ingesting cold water (750 mL/h at 5 °C, energy equivalent to −15 W/m2) and ice slurries (500 mL/h with ice packing factor of 70%, energy equivalent to −21 W/m2). Drinking cold water or ice slurries may increase the neutral comfort temperature by 2.1 to 2.9 °C and reduce thermal sensation by 0.5 to 1.1 units under indoor temperatures up to 32 °C. Similar results were observed in the experimental study by Wang et al. [84].
- Body dehydration. Body dehydration (or hypohydration) occurs from prolonged exposure to hot conditions with inadequate replacement of body water loss by sweating. Dehydration reduces sweating rate [85] and therefore increases thermal discomfort. Figure 7 shows how body dehydration up to 8% of body weight, combined with a rehydration rate of 60%, reduces the neutral temperature by 0.3 °C but increases thermal sensation by 0.1. Although these changes seem minor, combination of body dehydration with other factors affecting sweating rates can significantly alter psychological responses.
- Seasonal heat and cold acclimatization. Repeated or intermittent exposure to hot (summer) or cold (winter) indoor or outdoor temperatures over several days increases acclimatization, enabling subjects to tolerate warmer or cooler conditions [86,87]. However, it is difficult to report such information for every subject during the survey periods, which extend over a long period of time (weeks or months). Furthermore, it remains unclear whether individuals spending most of their time indoors can fully acclimatize to heat in summer.
- Psychological factors. The design of thermal comfort questionnaires usually does not include factors related to subject psychology, such as mood state, stress, depression, etc., despite their potential impact on thermal perception [88].
Limitations
- The MPMV model was developed using a limited experimental dataset of high quality with known inputs, focusing on older people with average ages from 65 to 72 years (mean value 70 years) [66]. The model requires further improvement to address very old people (age > 70 years), who could have lower thermal sensitivity compared to younger older adults.
- The MPMV model predictions are based on the assumed metabolic rate for a large population of older individuals (FE in Equation (5)), where the effect of age is noticeable. Caution should therefore be exercised in applying the results to individuals or smaller samples of older subjects.
- Most of the collected field studies were carried out in different building types and climate zones in Asia, where comfort scale semantics were translated from English to local languages. Therefore, differences in climate, cultural background, and the interpretations of the translated comfort scale semantics could have affected thermal sensation data [89].
5. Conclusions
Suggested Future Research
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Nomenclature
| Symbol | Meaning |
| aPMV | Adaptive predicted mean vote from [12] |
| CSH | Adjustment constant for non-shivering thermogenesis |
| CSW | Adjustment constant for regulatory sweating |
| FbE | Ratio of basal metabolic rate of older to young adults |
| FE | Ratio of metabolic rate of older to young adults |
| ICl | Intrinsic insulation value of clothing (clo) |
| MPMV | Metabolic-based predicted mean vote from [63] |
| Ma | Metabolic rate of activity of young adult (W/m2 or met) |
| MbE | Basal metabolic rate of an older adult (W/m2 or met) |
| Mb,r | Basal metabolic rate of a reference young adult (W/m2 or met) |
| MC | Metabolic rate required to maintain a neutral comfort state (W/m2 or met) |
| ME | Metabolic rate of an older adult (W/m2 or met) |
| MN | Metabolic rate required to maintain a neutral comfort state at rest with no thermoregulatory controls (W/m2 or met) |
| PMV | Predictive mean vote |
| PTSV | Physiologically based thermal sensation vote |
| Qex | Heat flux extracted from or added to the body core section (W/m2) |
| QexC | Heat flux extracted from or added to the body core section at the neutral comfort state (W/m2) |
| RH | Relative humidity (%) |
| RMSE | Root mean square error |
| TSV | Thermal sensation vote |
| Ta | Air temperature (°C) |
| TcN | Neutral core temperature at rest (°C) |
| Tr | Mean radiant temperature (°C) |
| TskN | Neutral mean skin temperature at rest (°C) |
| Va | Absolute air velocity around body (m/s) |
| WE | Mechanical work performed by older adults (W/m2) |
| ηC | Mechanical work efficiency related to Mc |
| ηN | Mechanical work efficiency related to MN |
| β | Sensitivity factor for MPMV (Equation (2)) |
References
- Xie, J.; Li, H.; Li, C.; Zhang, J.; Luo, M. Review on Occupant-Centric Thermal Comfort Sensing, Predicting, and Controlling. Energy Build. 2020, 226, 110392. [Google Scholar] [CrossRef]
- Zhou, S.; Li, B.; Du, C.; Liu, H.; Wu, Y.; Hodder, S.; Chen, M.; Kosonen, R.; Ming, R.; Ouyang, L.; et al. Opportunities and Challenges of Using Thermal Comfort Models for Building Design and Operation for the Elderly: A Literature Review. Renew. Sustain. Energy Rev. 2023, 183, 113504. [Google Scholar] [CrossRef]
- Jowkar, M.; de Dear, R.; Brusey, J. Influence of Long-Term Thermal History on Thermal Comfort and Preference. Energy Build. 2020, 210, 109685. [Google Scholar] [CrossRef]
- Childs, C.; Elliott, J.; Khatab, K.; Hampshaw, S.; Fowler-Davis, S.; Willmott, J.R.; Ali, A. Thermal Sensation in Older People with and without Dementia Living in Residential Care: New Assessment Approaches to Thermal Comfort Using Infrared Thermography. Int. J. Environ. Res. Public. Health 2020, 17, 6932. [Google Scholar] [CrossRef]
- Brager, G.S.; de Dear, R.J. Historical and Cultural Influences on Comfort Expectations. In Buildings, Culture and Environment; Wiley: Hoboken, NJ, USA, 2003; pp. 177–201. [Google Scholar]
- Sacher, G.A. Energy Metabolism and Thermoregulation in Old Age; No. CONF-790112-2; Argonne National Lab.: Lemont, IL, USA, 1979. [Google Scholar]
- Van Someren, E.J.W. Age-Related Changes in Thermoreception and Thermoregulation. In Handbook of the Biology of Aging; Elsevier: Amsterdam, The Netherlands, 2011; pp. 463–478. [Google Scholar]
- Zhou, H.; Yu, W.; Zhao, K.; Shan, H.; Zhou, S.; Wei, S.; Ouyang, L. Thermal Demand Characteristics of Elderly People with Varying Levels of Frailty in Residential Buildings during the Summer. J. Build. Eng. 2024, 84, 108654. [Google Scholar] [CrossRef]
- Yao, R.; Zhang, S.; Du, C.; Schweiker, M.; Hodder, S.; Olesen, B.W.; Toftum, J.; Romana d’Ambrosio, F.; Gebhardt, H.; Zhou, S.; et al. Evolution and Performance Analysis of Adaptive Thermal Comfort Models—A Comprehensive Literature Review. Build Environ. 2022, 217, 109020. [Google Scholar] [CrossRef]
- Tyler, C.J.; Reeve, T.; Sieh, N.; Cheung, S.S. Effects of Heat Adaptation on Physiology, Perception, and Exercise Performance in the Heat: An Updated Meta-Analysis. J. Sci. Sport Exerc. 2024, 6, 195–217. [Google Scholar] [CrossRef]
- Fanger, P.O. Thermal Comfort: Analysis and Applications in Environmental Engineering; Danish Technical Press: Vanloese, Denmark, 1970. [Google Scholar]
- ANSI/ASHRAE Standard 55-2023; Thermal Environmental Conditions for Human Occupancy. American Society of Heating Refrigerating and Air Conditioning Engineers: Atlanta, GA, USA, 2023.
- ISO 7730:2023; Ergonomics of the Thermal Environment—Analytical Determination and Interpretation of Thermal Comfort Using Calculation of the PMV and PPD Indices and Local Thermal Comfort Criteria. The International Organization for Standardization (ISO): Geneva, Switzerland, 2023.
- Cheung, T.; Schiavon, S.; Parkinson, T.; Li, P.; Brager, G. Analysis of the Accuracy on PMV—PPD Model Using the ASHRAE Global Thermal Comfort Database II. Build Environ. 2019, 153, 205–217. [Google Scholar] [CrossRef]
- Humphreys, M.A.; Fergus Nicol, J. The Validity of ISO-PMV for Predicting Comfort Votes in Every-Day Thermal Environments. Energy Build. 2002, 34, 667–684. [Google Scholar] [CrossRef]
- Bae, C.; Lee, H.; Chun, C. Predicting Indoor Thermal Sensation for the Elderly in Welfare Centres in Korea Using Local Skin Temperatures. Indoor Built Environ. 2017, 26, 1155–1167. [Google Scholar] [CrossRef]
- Tsuzuki, K.; Ohfuku, T. Thermal Sensation and Thermoregulation in Elderly Compared to Young People in Japanese Winter Season. In Proceedings of the Indoor Air Conference, Monterey, CA, USA, 30 June–5 July 2002. [Google Scholar]
- Schellen, L.; van Marken Lichtenbelt, W.; Loomans, M.G.L.C.; Frijns, A.; Toftum, J.; deWit, M. Thermal Comfort, Physiological Responses and Performance of Elderly during Exposure to a Moderate Temperature Drift. In Proceedings of the 9th International Conference and Exhibition on Healthy Buildings, Syracuse, NY, USA, 13–17 September 2009. [Google Scholar]
- Baquero, M.T.; Vergés, R.; Gaspar, K.; Forcada, N. A Field Investigation of the Thermal Comfort of Older Adults in Cold Winter Climates. Indoor Air 2023, 2023, 9185216. [Google Scholar] [CrossRef]
- Wu, Y.; Liu, H.; Li, B.; Kosonen, R.; Kong, D.; Zhou, S.; Yao, R. Thermal Adaptation of the Elderly during Summer in a Hot Humid Area: Psychological, Behavioral, and Physiological Responses. Energy Build. 2019, 203, 109450. [Google Scholar] [CrossRef]
- Tejedor, B.; Casals, M.; Gangolells, M.; Macarulla, M.; Forcada, N. Human Comfort Modelling for Elderly People by Infrared Thermography: Evaluating the Thermoregulation System Responses in an Indoor Environment during Winter. Build Environ. 2020, 186, 107354. [Google Scholar] [CrossRef]
- Shao, T.; Jin, H. A Field Investigation on the Winter Thermal Comfort of Residents in Rural Houses at Different Latitudes of Northeast Severe Cold Regions, China. J. Build. Eng. 2020, 328, 101476. [Google Scholar] [CrossRef]
- Tartarini, F.; Cooper, P.; Fleming, R. Thermal Perceptions, Preferences and Adaptive Behaviours of Occupants of Nursing Homes. Build Environ. 2018, 132, 57–69. [Google Scholar] [CrossRef]
- Li, H.; Hu, H.; Wu, Z.; Kong, X.; Fan, M. Modified Predicted Mean Vote Models for Human Thermal Comfort: An ASHRAE Database-Based Evaluation. Renew. Sustain. Energy Rev. 2025, 209, 115042. [Google Scholar] [CrossRef]
- Fanger, P.O.; Toftum, J. Extension of the PMV Model to Non-Air-Conditioned Buildings in Warm Climates. Energy Build. 2002, 34, 533–536. [Google Scholar] [CrossRef]
- Yao, R.; Li, B.; Liu, J. A Theoretical Adaptive Model of Thermal Comfort—Adaptive Predicted Mean Vote (APMV). Build Environ. 2009, 44, 2089–2096. [Google Scholar] [CrossRef]
- Lamberti, G.; Contrada, F.; Kindinis, A.; Leccese, F.; Salvadori, G. Developing a New Adaptive Heat Balance Model to Enhance Thermal Comfort Predictions and Reduce Energy Consumption. Energy Build. 2024, 321, 114663. [Google Scholar] [CrossRef]
- Schweiker, M.; Wagner, A. A Framework for an Adaptive Thermal Heat Balance Model (ATHB). Build Environ. 2015, 94, 252–262. [Google Scholar] [CrossRef]
- de Dear, R.; Xiong, J.; Kim, J.; Cao, B. A Review of Adaptive Thermal Comfort Research since 1998. Energy Build. 2020, 214, 109893. [Google Scholar] [CrossRef]
- GB/T 50785-2012; Evaluation Standard for Indoor Thermal Environment in Civil Buildings. Ministry of Housing and Urban-Rural Development (MOHURD) and the General Administration of Quality Supervision, Inspection and Quarantine (GAQSIQ) of the People’s Republic of China: Beijing, China, 2012; Chinese Standard.
- Younes, J.; Chen, M.; Ghali, K.; Kosonen, R.; Melikov, A.K.; Ghaddar, N. A Thermal Sensation Model for Elderly under Steady and Transient Uniform Conditions. Build Environ. 2023, 227, 109797. [Google Scholar] [CrossRef]
- Rida, M.; Ghaddar, N.; Ghali, K.; Hoballah, J. Elderly Bioheat Modeling: Changes in Physiology, Thermoregulation, and Blood Flow Circulation. Int. J. Biometeorol. 2014, 58, 1825–1843. [Google Scholar] [CrossRef]
- EN15251:2006; Indoor Environmental Input Parameters for Design and Assessment of Energy Performance of Buildings Addressing Indoor Air Quality, Thermal Environment, Lighting and Acoustics. CEN: Brussels, Belgium, 2006.
- Soebarto, V.; Zhang, H.; Schiavon, S. A Thermal Comfort Environmental Chamber Study of Older and Younger People. Build Environ. 2019, 155, 1–14. [Google Scholar] [CrossRef]
- Zhou, S.; Li, B.; Du, C.; Yao, R.; Ouyang, L.; Zhou, H.; Kosonen, R.; Melikov, A.K.; Shang, L.; Liu, H. Developing Thermal Prediction Models for the Elderly under Temperature Step Changes. Build Environ. 2023, 245, 110902. [Google Scholar] [CrossRef]
- Wang, Z.; Yu, H.; Jiao, Y.; Chu, X.; Luo, M. Chinese Older People’s Subjective and Physiological Responses to Moderate Cold and Warm Temperature Steps. Build Environ. 2019, 149, 526–536. [Google Scholar] [CrossRef]
- Schellen, L.; van Marken Lichtenbelt, W.D.; Loomans, M.G.L.C.; Toftum, J.; de Wit, M.H. Differences between Young Adults and Elderly in Thermal Comfort, Productivity, and Thermal Physiology in Response to a Moderate Temperature Drift and a Steady-State Condition. Indoor Air 2010, 20, 273–283. [Google Scholar] [CrossRef]
- Panraluk, C.; Sreshthaputra, A. Developing Guidelines for Thermal Comfort and Energy Saving during Hot Season of Multipurpose Senior Centers in Thailand. Sustainability 2020, 12, 170. [Google Scholar] [CrossRef]
- Xiong, J.; Ma, T.; Lian, Z.; de Dear, R. Perceptual and Physiological Responses of Elderly Subjects to Moderate Temperatures. Build Environ. 2019, 156, 117–122. [Google Scholar] [CrossRef]
- Stapleton, J.M.; Larose, J.; Simpson, C.; Flouris, A.D.; Sigal, R.J.; Kenny, G.P. Do Older Adults Experience Greater Thermal Strain during Heat Waves? Appl. Physiol. Nutr. Metab. 2014, 39, 292–298. [Google Scholar] [CrossRef]
- Chen, M.; Farahani, A.V.; Kilpeläinen, S.; Kosonen, R.; Younes, J.; Ghaddar, N.; Ghali, K.; Melikov, A.K. Thermal Comfort Chamber Study of Nordic Elderly People with Local Cooling Devices in Warm Conditions. Build Environ. 2023, 235, 110213. [Google Scholar] [CrossRef]
- Fan, G.; Xie, J.; Yoshino, H.; Yanagi, U.; Hasegawa, K.; Wang, C.; Zhang, X.; Liu, J. Investigation of Indoor Thermal Environment in the Homes with Elderly People during Heating Season in Beijing, China. Build Environ. 2017, 126, 288–303. [Google Scholar] [CrossRef]
- Neira-Zambrano, K.; Trebilcock-Kelly, M.; Briede-Westermeyer, J.C. Older Adults’ Thermal Comfort in Nursing Homes: Exploratory Research in Three Case Studies. Sustainability 2023, 15, 3002. [Google Scholar] [CrossRef]
- Sudarsanam, N.; Kannamma, D. Investigation of Summertime Thermal Comfort at the Residences of Elderly People in the Warm and Humid Climate of India. Energy Build. 2023, 291, 113151. [Google Scholar] [CrossRef]
- Hwang, R.L.; Chen, C.P. Field Study on Behaviors and Adaptation of Elderly People and Their Thermal Comfort Requirements in Residential Environments. Indoor Air 2010, 20, 235–245. [Google Scholar] [CrossRef]
- Miao, Y.; Chau, K.W.; Lau, S.S.Y.; Ye, T. A Novel Thermal Comfort Model Modified by Time Scale and Habitual Trajectory. Renew. Sustain. Energy Rev. 2025, 207, 114903. [Google Scholar] [CrossRef]
- Zheng, G.; Wei, C.; Li, K. Determining the Summer Indoor Design Parameters for Pensioners’ Buildings Based on the Thermal Requirements of Elderly People at Different Ages. Energy 2022, 258, 124854. [Google Scholar] [CrossRef]
- Sudprasert, S. Study of Thermal Comfort and the Adaptive Behaviors of the Elderly in Naturally Ventilated Houses. Int. J. Build. Urban Inter. Landsc. Technol. 2020, 16, 73–82. [Google Scholar] [CrossRef]
- Zhang, J.; Lu, J.; Deng, W.; Beccarelli, P.; Lun, I.Y.F. Thermal Comfort Investigation of Rural Houses in China: A Review. Build. Environ. 2023, 235, 110208. [Google Scholar] [CrossRef]
- Ji, T.; Zhang, T.; Fukuda, H. Thermal Comfort Research on the Rural Elderly in the Guanzhong Region: A Comparative Analysis Based on Age Stratification of Residential Environments. Sustainability 2024, 16, 6101. [Google Scholar] [CrossRef]
- Feng, R.; Zheng, W.; Wang, Y.; Shao, T.; Wang, X.; Zhang, J.; Fang, Y.; Dong, C. Thermal Responses of the Elderly in Naturally Ventilated Dwelling Houses during Winter in Rural Xi’an, China. In Proceedings of the E3S Web of Conferences, EDP Sciences, Izmir, Turkey, 9 July 2024; Volume 546. [Google Scholar]
- Zhang, T.; Duan, Y.; Jiao, Z.; Ye, X.; Hu, Q.; Fukuda, H.; Gao, W. Towards Improving Rural Living Environment for Chinese Cold Region Based on Investigation of Thermal Environment and Space Usage Status. Buildings 2022, 12, 2139. [Google Scholar] [CrossRef]
- Li, H.; Xu, G.; Chen, J.; Duan, J. Investigating the Adaptive Thermal Comfort of the Elderly in Rural Mutual Aid Homes in Central Inner Mongolia. Sustainability 2022, 14, 6802. [Google Scholar] [CrossRef]
- Zheng, W.; Feng, R.; Wang, Y.; Shao, T.; Chow, D.; Zhang, L. Fundamental Research on Sustainable Building Design for the Rural Elderly: A Field Study of Various Subjective Responses to Thermal Environments and Comfort Demands during Summer in Xi’an, China. Sustainability 2024, 16, 7778. [Google Scholar] [CrossRef]
- Tang, H.; Gao, Y.; Tan, S.; Guo, Y.; Gao, W. Field Investigation on Adaptive Thermal Comfort in Rural Dwellings: A Case Study in Linyi (China) during Summer. Buildings 2024, 14, 1429. [Google Scholar] [CrossRef]
- Zhang, J.; Lu, J.; Deng, W.; Beccarelli, P.; Lun, I.Y.F. Investigation of Thermal Comfort and Preferred Temperatures among Rural Elderly in Weihai, China: Considering Metabolic Rate Effects. J. Build. Eng. 2024, 97, 110940. [Google Scholar] [CrossRef]
- Tao, Y.; Gou, Z.; Yu, Z.; Fu, J.; Chen, X. The Challenge of Creating Age-Friendly Indoor Environments in a High-Density City: Case Study of Hong Kong’s Care and Attention Homes. J. Build. Eng. 2020, 30, 101280. [Google Scholar] [CrossRef]
- Tartarini, F.; Cooper, P.; Fleming, R. Thermal Environment and Thermal Sensations of Occupants of Nursing Homes: A Field Study. Procedia Eng. 2017, 180, 373–382. [Google Scholar] [CrossRef]
- Baquero, M.T.; Forcada, N. Thermal Comfort of Older People during Summer in the Continental Mediterranean Climate. J. Build. Eng. 2022, 54, 104680. [Google Scholar] [CrossRef]
- Forcada, N.; Gangolells, M.; Casals, M.; Tejedor, B.; Macarulla, M.; Gaspar, K. Summer Thermal Comfort in Nursing Homes in the Mediterranean Climate. Energy Build. 2020, 229, 110442. [Google Scholar] [CrossRef]
- Forcada, N.; Gangolells, M.; Casals, M.; Tejedor, B.; Macarulla, M.; Gaspar, K. Field Study on Thermal Comfort in Nursing Homes in Heated Environments. Energy Build. 2021, 244, 111032. [Google Scholar] [CrossRef]
- Wang, Z.; Yu, H.; Jiao, Y.; Wei, Q.; Chu, X. A Field Study of Thermal Sensation and Neutrality in Free-Running Aged-Care Homes in Shanghai. Energy Build. 2018, 158, 1523–1532. [Google Scholar] [CrossRef]
- Sun, N.; Ding, X.; Bi, J.; Cui, Y. Field Study on Winter Thermal Comfort of Occupants of Nursing Homes in Shandong Province, China. Buildings 2024, 14, 2881. [Google Scholar] [CrossRef]
- Zheng, W.; Shao, T.; Lin, Y.; Wang, Y.; Dong, C.; Liu, J. A Field Study on Seasonal Adaptive Thermal Comfort of the Elderly in Nursing Homes in Xi’an, China. Build Environ. 2022, 208, 108623. [Google Scholar] [CrossRef]
- Laouadi, A. Physiological Indicators of Thermal Comfort: A Comprehensive Approach Using the Metabolic-Based Predicted Mean Vote Index. Buildings 2024, 14, 3861. [Google Scholar] [CrossRef]
- Laouadi, A. A New General Formulation for the PMV Thermal Comfort Index. Buildings 2022, 12, 1572. [Google Scholar] [CrossRef]
- Melzer, K.; Laurie Karsegard, V.; Genton, L.; Kossovsky, M.P.; Kayser, B.; Pichard, C. Comparison of Equations for Estimating Resting Metabolic Rate in Healthy Subjects over 70 Years of Age. Clin. Nutr. 2007, 26, 498–505. [Google Scholar] [CrossRef]
- Aslan, D.H.; Collette, J.M.; Ortega, J.D. Bicycling Exercise Helps Maintain a Youthful Metabolic Cost of Walking in Older Adults. J. Aging Phys. Act. 2021, 29, 36–42. [Google Scholar] [CrossRef]
- Nishimura, T.; Motoi, M.; Egashira, Y.; Choi, D.; Aoyagi, K.; Watanuki, S. Seasonal Variation of Non-Shivering Thermogenesis (NST) during Mild Cold Exposure. J. Physiol. Anthr. 2015, 34, 11. [Google Scholar] [CrossRef]
- Wu, Y.; Liu, H.; Chen, B.; Li, B.; Kosonen, R.; Jokisalo, J.; Chen, T. Effect of Long-Term Thermal History on Physiological Acclimatization and Prediction of Thermal Sensation in Typical Winter Conditions. Build Environ. 2020, 179, 106936. [Google Scholar] [CrossRef]
- Chinevere, T.D.; Kenefick, R.W.; Cheuvront, S.N.; Lukaski, H.C.; Sawka, M.N. Effect of Heat Acclimation on Sweat Minerals. Med. Sci. Sports Exerc. 2008, 40, 886–891. [Google Scholar] [CrossRef]
- Jin, Y.; Wang, F.; Payne, S.R.; Weller, R.B. A Comparison of the Effect of Indoor Thermal and Humidity Condition on Young and Older Adults’ Comfort and Skin Condition in Winter. Indoor Built Environ. 2022, 31, 759–776. [Google Scholar] [CrossRef]
- Zhou, H.; Yu, W.; Zhao, K.; Shan, H.; Zhou, S.; Zhang, Y.; Wang, H.; Wei, S. Adaptative Thermal Comfort Analysis in the Elderly Based on Fried Frailty Classification in Residential Buildings during Summer. Build Environ. 2024, 252, 111262. [Google Scholar] [CrossRef]
- Ji, L.; Laouadi, A.; Wang, L.; Lacasse, M.A. Development of a Bioheat Model for Older People under Hot and Cold Exposures. Build. Simul. 2022, 15, 1815–1829. [Google Scholar] [CrossRef]
- ISO 9920:2007; Ergonomics of the Thermal Environment—Estimation of Thermal Insulation and Water Vapour Resistance of a Clothing Ensemble. The International Organization for Standardization (ISO): Geneva, Switzerland, 2007.
- Tang, Y.; Su, Z.; Yu, H.; Zhang, K.; Li, C.; Ye, H. A Database of Clothing Overall and Local Insulation and Prediction Models for Estimating Ensembles’ Insulation. Build Environ. 2022, 207, 108418. [Google Scholar] [CrossRef]
- Hall, K.S.; Morey, M.C.; Dutta, C.; Manini, T.M.; Weltman, A.L.; Nelson, M.E.; Morgan, A.L.; Senior, J.G.; Seyffarth, C.; Buchner, D.M. Activity-Related Energy Expenditure in Older Adults. Med. Sci. Sports Exerc. 2014, 46, 2335–2340. [Google Scholar] [CrossRef]
- Ainsworth, B.E.; Haskell, W.L.; Whitt, M.C.; Irwin, M.L.; Swartz, A.M.; Strath, S.J.; O’Brien, W.L.; Bassett, D.R., Jr.; Schmitz, K.H.; Emplaincourt, P.O.; et al. Compendium of Physical Activities: An Update of Activity Codes and MET Intensities. Med. Sci. Sports Exerc. 2000, 32, S498–S516. [Google Scholar] [CrossRef]
- Kenny, G.P.; Webb, P.; Ducharme, M.B.; Reardon, F.D.; Jay, O. Calorimetric Measurement of Postexercise Net Heat Loss and Residual Body Heat Storage. Med. Sci. Sports Exerc. 2008, 40, 1629–1636. [Google Scholar] [CrossRef]
- Bo, S.; Fadda, M.; Fedele, D.; Pellegrini, M.; Ghigo, E.; Pellegrini, N. A Critical Review on the Role of Food and Nutrition in the Energy Balance. Nutrients 2020, 12, 1161. [Google Scholar] [CrossRef]
- Boschmann, M.; Steiniger, J.; Hille, U.; Tank, J.; Adams, F.; Sharma, A.M.; Klaus, S.; Luft, F.C.; Jordan, J. Water-Induced Thermogenesis. J. Clin. Endocrinol. Metab. 2003, 88, 6015–6019. [Google Scholar] [CrossRef]
- Dubnov-Raz, G.; Constantini, N.W.; Yariv, H.; Nice, S.; Shapira, N. Influence of Water Drinking on Resting Energy Expenditure in Overweight Children. Int. J. Obes. 2011, 35, 1295–1300. [Google Scholar] [CrossRef]
- Wang, Z.; Cao, B.; Lin, B.; Zhu, Y. Investigation of Thermal Comfort and Behavioral Adjustments of Older People in Residential Environments in Beijing. Energy Build. 2020, 217, 110001. [Google Scholar] [CrossRef]
- Wang, F.; Tang, Y.; Ke, Y.; Zheng, Q.; Lei, T.-H. Ice Slurry Ingestion for Enhanced Occupant Thermal Comfort in Warm/Hot Indoor Environments: A Comparative Study with an Energy-Efficient Desk Fan. Build Environ. 2024, 253, 111350. [Google Scholar] [CrossRef]
- Montain, S.J.; Latzka, W.A.; Sawka, M.N. Control of Thermoregulatory Sweating Is Altered by Hydration Level and Exercise Intensity. J. Appl. Physiol. 1995, 79, 1434–1439. [Google Scholar] [CrossRef]
- Notley, S.R.; Meade, R.D.; Akerman, A.P.; Poirier, M.P.; Boulay, P.; Sigal, R.J.; Flouris, A.D.; Kenny, G.P. Evidence for Age-related Differences in Heat Acclimatisation Responsiveness. Exp. Physiol. 2020, 105, 1491–1499. [Google Scholar] [CrossRef] [PubMed]
- Castellani, J.W.; Young, A.J. Human Physiological Responses to Cold Exposure: Acute Responses and Acclimatization to Prolonged Exposure. Auton. Neurosci. 2016, 196, 63–74. [Google Scholar] [CrossRef]
- Furkan Özbey, M.; Turhan, C. Investigating the Relationship Between Thermal Comfort and Human Psychology: A Review. J. Build. Des. Environ. 2024, 3, 35255. [Google Scholar] [CrossRef]
- Schweiker, M.; André, M.; Al-Atrash, F.; Al-Khatri, H.; Alprianti, R.R.; Alsaad, H.; Amin, R.; Ampatzi, E.; Arsano, A.Y.; Azar, E.; et al. Evaluating Assumptions of Scales for Subjective Assessment of Thermal Environments—Do Laypersons Perceive Them the Way, We Researchers Believe? Energy Build. 2020, 211, 109761. [Google Scholar] [CrossRef]
- Lei, T.-H.; Lan, L.; Wang, F. Indoor Thermal Comfort Research Using Human Participants: Guidelines and a Checklist for Experimental Design. J. Therm. Biol. 2023, 113, 103506. [Google Scholar] [CrossRef]



| Study | Number of Subjects | Mean Age (y) | Ta (°C) | Tr (°C) | RH (%) | Va (m/s) | Icl (clo) | Ma (met) | ME (met) |
|---|---|---|---|---|---|---|---|---|---|
| [17] | 109 | 72.4 | 23–31 | Ta | 60 | 0.2 | 0.63 | 1 | 0.7 |
| [37] | 8 | 70 | 21.5–24 | NA *** | 40 | 0.2 | 1 | 1.2 | NA ** |
| [38] | 33 * | 65.85 | 21–29 | 18.5-31.5 | 45, 60, 74 | 0.1, 0.51, 1.51 | 0.51 | 1.15 | NA |
| [39] | 16 | 70 | 21–31 | Ta | 49–69 | 0.1 | 0.55 | 1 | NA |
| [34] | 22 | 69.74 | 20, 25 | Ta | 40 | 0.1 | 0.72, 1.06 | 1.2 | NA |
| [36] | 18 | 67.4 | 21–32 | NA | 58 | 0.15 | 0.5 | 1 | NA |
| [41] | 26 | 70.8 | 26–33 | NA | 38–62 | 0.1 | 0.5 | 1 | NA |
| [35] | 24 | 66.6 | 25–34 | NA | 50, 60 | 0.1 | 0.34 | 1 | NA |
| [40] | 12 | 65 | 36.5 | NA | 20, 60 | 0.25 | 0.1 | 1 | 0.95 |
| [20] | 8 | 65 | 18, 34 | NA | 50 | 0.1 | 0.5 | 1 | NA |
| Study | Building | Number of Subjects | Season | Age (y) | Ta (°C) | Tr (°C) | RH (%) | Va (m/s) | Icl (clo) | Ma (met) |
|---|---|---|---|---|---|---|---|---|---|---|
| [56] | Rural residences | 11 | Winter, spring, summer, fall | 71 | 6–34 | NA * | 60–71 | 0.2 | 0.23–2.25 | 1.2 |
| [72] | Urban care homes | 11 | Spring | 77 | 20–28 | NA | 31–35 | 0.05 | 0.9, 1.6 | 1.2 |
| [45] | Urban residences | 87 | Winter, summer | 71 | 13.3–32.5 | NA | 67.5 | 0.1 | 0.3–1.4 | 1 |
| [62] | Urban care homes | 342, 330, 368 | Winter, summer, mid-season | 84 | 6–33 | NA | 50–65 | 0–0.2 | 0.42–1.53 | 1.2 |
| [16] | Urban care homes | 294 | Winter, and fall | 75 | 20–28 | NA | 63.3 | 0.1 | 0.7 | 1.2 |
| [64] | Urban care homes | 81, 76, 56 | Winter, summer, and mid-season | 70–74 | 10–36 | NA | 39–56 | 0–0.2 | 0.33–1.56 | 1.2 |
| [57] | Urban care homes | 213, 181 | Winter, summer | 79 | 21–27 | NA | 60, 65 | 0.1–0.4 | 0.7, 1 | 1.2 |
| [19] | Urban care homes | 49 | Winter | 75 | 22–26 | NA | 20–46 | 0.1 | 0.8–1.4 | 1.2 |
| [44] | Urban residences | 740 | Summer * | 69 | 28–34 | NA | 60 | 1.5 | 0.44, 0.82 | 1.1 |
| [73] | Urban residences | 394 | Summer | 73 | 24.7–33.6 | 25-33.7 | 56.6 | 0.1–0.7 | 0.2–0.44 | 1.2 |
| [63] | Urban care homes | 728 | Winter | 78 | 16.6–25 | NA | 28 | 0.1 | 1–1.46 | 1.2 |
| [55] | Rural residences | 97 | Summer ** | 70 *** | 27–34 | NA | 60 | 0.3 | 0.39 | 1.2 |
| [48] | Urban residences | 30 | Summer | 67 | 29–35 | NA | 50 | 0.2 | 0.33 | 1.2 |
| [51] | Rural residences | 161 | Winter | 69 | 5–16 | NA | 53.4 | 0–0.45 | 1.4–1.6 | 1.2 |
| [47] | Urban residences | 29 | Summer | 67, 81, 92 | 21–40 | NA | 62.8 | 0.1 | 0.46 | 1.2 |
| [46] | Urban residences | 15 | Summer | 72 | 23–32 | NA | 74.2 | 0.02 | 0.52 | 1.2 |
| [61] | Urban care homes | 737 | Winter | 87 | 21–25 | NA | 47.2 | 0.22 | 0.92 | 1.15 |
| [60] | Urban care homes | 476 | Summer | 85 | 23–28 | NA | 61.8 | 0.06 | 0.57–0.62 | 1.18 |
| [54] | Rural residences | 230 | Summer | 69 | 23–37 | NA | 27–84 | 0.2 | 0.4–0.54 | 1.29 |
| [20] | Urban care homes and residences | 119, 333 | Summer | 77 | 22–36 | NA | 66.2 | 0.13 | 0.3–0.36 | 1.2 |
| [53] | Rural residences | 187 | Winter | 65, 70, 87 | 15–24 | NA | 39.82 | 0.02 | 1.24–1.5 | 1.2 |
| Building Type → | Urban Care Homes | Urban Residences | Rural Residences | |||
|---|---|---|---|---|---|---|
| Season | Summer | Winter | Summer | Winter | Summer | Winter |
| Tr = Ta RH = 60% Va ≤ 0.2 m/s Icl = 0.6 (0.5) clo Ma = 1.2 (1.5) met | Tr = Ta RH = 40% Va ≤ 0.2 m/s Icl = 1 clo Ma = 1.2 (1.5) met | Tr = Ta RH = 60% Va ≤ 0.2 m/s Icl = 0.5 clo Ma = 1.2 met | Tr = Ta RH = 40% Va ≤ 0.2 m/s Icl = 1 clo Ma = 1.2 met | Tr = Ta RH = 60% Va = 0.3 m/s Icl = 0.4 clo Ma = 1.2 met | Tr = Ta RH = 40% Va = 0.2 m/s Icl = 1.5 clo Ma = 1.2 met | |
| This study (Tn and range) | 25.6 (23) | 24 (19.5) | 26.2 (24.8) | 24 (22) | 27.2 (26) | 21.5 (19) |
| 23.8–27.4 (21–25) | 21.6–26.3 (16.8–22.2) | 24.5–27.9 (23–26.6) | 21.6–26.3 (19.6–24.5) | 25.7–28.7 (24.5–27.6) | 18.6–24.5 (16–22.2) | |
| Field studies | 25.4 [62] 24.1 [64] 25.7 [57] 25.3 (23.9) [60] 25.0 [20] | 16.6 [62] 24.1 [16] 19.3 [64] 23.7 [57] 26.7 [19] 22.0 (20.7) [63] 21.6 (21.9) [61] | 25.2 [45] 26.5 [73] 29.6 [44] 29.0 [48] 26.8 [47] 25.5 [46] 22.2 [20] 25.8, 26.9, 27.9 [8] | 23.2 [45] | 28.1 [56] 27.4 (27.2) [55] 24.0 [54] | 14.8 [56] 11.2 [51] 20.2 [53] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Laouadi, A.; Sirati, M.; Jandaghian, Z. Thermal Comfort of Older People: Validation of the MPMV Model. Energies 2025, 18, 1484. https://doi.org/10.3390/en18061484
Laouadi A, Sirati M, Jandaghian Z. Thermal Comfort of Older People: Validation of the MPMV Model. Energies. 2025; 18(6):1484. https://doi.org/10.3390/en18061484
Chicago/Turabian StyleLaouadi, Abdelaziz, Melina Sirati, and Zahra Jandaghian. 2025. "Thermal Comfort of Older People: Validation of the MPMV Model" Energies 18, no. 6: 1484. https://doi.org/10.3390/en18061484
APA StyleLaouadi, A., Sirati, M., & Jandaghian, Z. (2025). Thermal Comfort of Older People: Validation of the MPMV Model. Energies, 18(6), 1484. https://doi.org/10.3390/en18061484







