Abstract
Patients are different regarding their health conditions, illnesses and ailments, and mobility. These and other factors could affect their specific feelings about the thermal environment. Current methods of predicting thermal sensations were developed based on research on a group of healthy people. Therefore, the use of these methods with patients should be verified. This paper aimed to verify selected thermal comfort models in terms of their reliability to predict the average assessment of thermal conditions in the patient rooms and the percentage of dissatisfied patients. Thermal condition analyses were based on microclimate parameter measurements and extensive questionnaires among patients, done in parallel in the hospital’s patient rooms. The research was carried out in 23 hospitals located in the following provinces in Poland: (Warmińsko-Mazurskie, Kujawsko-Pomorskie, Mazowieckie, Wielkopolskie, Łódzkie, Świętokrzyskie, Lubelskie and Dolnośląskie). Overall, 890 patients from 14 different specialities participated in the research. Actual thermal sensations of patients differed from predictions obtained from selected thermal comfort models. A comparison of the actual thermal sensations with the PMV model indicates the shift of the comfort curve towards cooler rather than neutral conditions. A comparison of the same to the adaptive model predictions indicates that patients had a higher dissatisfaction rate and preferred cooler thermal conditions than predicted. Research findings show that normative models are not fully reliable in predicting patients’ thermal sensations.
1. Introduction
The thermal environment is one of the internal environment elements that significantly affects the health, productivity, and efficiency of employees, which has been proven in many studies involving students or office workers [1,2,3,4,5,6]. Therefore, it can be assumed that in the case of sick rooms, it is crucial that the thermal environment conditions ensure the comfort of their users; however, all medical, technological, and sanitary-hygienic requirements must be met at the same time. In the literature, the human perception of the thermal environment is determined by three different methods, which can be described as physical, psychological, and physiological. The first is based on models of physical phenomena occurring at the boundary between humans and the external environment; the second uses the actual, subjective perception of the thermal environment by humans expressed, for example, in the so-called survey research; the third is based on measurements of physiological parameters such as body temperature. Normative models of thermal comfort [7,8] use a physical model that assumes that comfortable conditions in terms of thermal sensations are neutral and are equivalent to the state of thermal comfort, which occurs if the body exchanges a balance of heat with the external environment. The model [7] was developed based on PMV (Predictive Mean Vote) and PPD (Predicted Percent of Dissatisfied) indices, the determination of which requires registration of personal parameters (thermal insulation of clothing, metabolic output) and thermal environment parameters (air temperature, radiation temperature, relative humidity, and air velocity).
According to [7] the PMV is an index that predicts the mean value of the votes of a large group of persons on the seven-point thermal sensation scale (i.e., −3 cold, −2 cool, −1 slightly cool, 0 neutral, +1 slightly warm, +2 warm, and +3 hot), based on the heat balance of the human body. The PPD is an index that establishes a quantitative prediction of the percentage of thermally dissatisfied people who feel too cool or too warm. For the standard in Ref. [7], thermally dissatisfied people are those who will vote hot, warm, cool, or cold on the seven-point thermal sensation scale.
Over time, other determinants of individual thermal sensation have also been recognised, i.e., gender, acclimatisation, climate zone, and adaptability of clothing. A modification of the PMV model developed by de Dear et al. [8] was the basis for the adaptation model [9], which considers the adaptation phenomenon’s influence and is dedicated to rooms without mechanical cooling systems. This model is also included in Ref. [10]. Unfortunately, there are no models available to predict the thermal sensation directed at or positively verified on a group of patients in hospital patient rooms. Apart from the factors mentioned above, which influence the perception of the thermal environment by healthy persons, the thermal sensation of patients in hospital rooms may additionally be conditioned, among others, by sanitary and hygienic requirements, medical recommendations, technological requirements, and economic criteria. Patients constitute a heterogeneous user group in terms of their level of mobility, state of health, medical conditions, period of hospitalisation, etc. The division of the hospital that most clearly accounts for these differences is wards, which house patients with similar conditions and complaints, as well as the categorisation of patient rooms according to their rank, e.g., into recovery rooms, intensive care unit patient rooms, or standard patient rooms, as well as septic and aseptic isolation rooms within the wards. The multitude and complexity of factors that distinguish patients in hospital rooms from healthy people, on whose responses the thermal comfort models were based, justified the thesis that the thermal sensations of patients in hospitals differ from thermal sensations indicated by normative models. The prediction of thermal sensations of patients, therefore, requires modification of the currently used thermal comfort indices. For this reason, the present study aimed to analyse the thermal sensations of patients in Polish hospitals in selected wards to verify the validity of the currently used methods for forecasting the thermal comfort conditions of room users.
Research in this area has already been carried out randomly; e.g., the influence of the gender of the room occupants on their thermal sensations was studied, among others, by Breslin et al. [11]. In the range from slightly cool to warm conditions, the influence of gender was insignificant, while in cool conditions, women perceived the thermal environment as cooler than men. Furthermore, studies to determine the effect of acclimatisation on thermal sensation found that although the acclimatisation process alters human physiological responses to heat stress, these changes are so small that the resulting change in thermal sensation appears to be insignificant. Research by Costa et al. [12] found that climatic conditions can affect emergency hospitalisations for heart diseases. A study by Webb et al. [13] to determine whether non-disability affects thermal sensation was conducted on a group of 16 non-disabled and 16 disabled people. They found no significant differences between the mean thermal sensations of non-disabled and disabled people. The disabled people in the study had been diagnosed with diseases such as cerebral palsy, spina bifida, stroke, Friedreich’s disease, blindness, paralysis, encephalitis, Guillain-Barré Syndrome, amputated limbs, and leg implants. Hwang et al. [14] conducted a study of the thermal environment in patient rooms, involving 927 patients residing in a medical centre located in Taiwan. The patient rooms in the hospital studied were unheated, and the indoor temperature, even during the lowest outdoor temperatures, was resultant (uncontrolled) and due to local weather conditions, i.e., a mild winter season with the lowest average monthly temperature of about 16 °C. The results indicate that weakened patients in the winter season prefer warmer than the forecast conditions, while in the summer season, the actual neutral temperature practically coincides with the forecast neutral temperature. Patients who are at full strength in the summer season prefer cooler thermal conditions than forecast, while in the winter season, they prefer warmer than forecast. In addition, it was noted that during the first days in the hospital, patients often felt discomfort due to their failure to adapt to the hospital’s thermal conditions; however, they compensated for this by, among other things, adjusting their clothing. However, there is still a lack of studies in the literature indicating directions for modifying the PMV model.
2. Materials and Methods
The study to assess differences between predicted and actual thermal sensations of patients was carried out in hospitals located in various regions of Poland (climatic zone Dfb according to [15] therefore, continental climate with warm summers. The average temperature of the coldest month is −3 °C or less, and the average temperature of the hottest month is above 10 °C; there is no month with an average temperature above 22 °C. Precipitation is evenly distributed throughout the year). The request for consent to conduct the study was sent to about 310 Polish hospitals; 192 hospitals (62%) replied positively, 20 hospitals (6%) replied negatively, and 98 hospitals (32%) did not respond. From among the hospitals that expressed their willingness to participate in the survey, as a result of analyses conducted with representatives of health care services, 23 hospitals were selected based on aspects of diversity and representativeness, e.g., in terms of the category (voivodship hospitals, county hospitals, city hospitals, etc.), location, size, standard and age of hospitals, medical specialisation of hospital wards, availability, and technical and technological equipment. When selecting the specialisation of the wards in which the study was conducted, special attention was paid to the wards where the specificity of the patients’ conditions could affect their thermal preferences. A total of 890 patients were surveyed inwards of 14 different medical specialities. The number of patients participating in the study exceeded the 423-person minimum non-returnable sample size for 50% fractions. Because the order of magnitude of the fraction of items having the trait was unknown, a fraction of 50% was assumed, and an acceptable estimation error of 4% and a significance level of 10% were assumed in the estimates. The sample size was determined based on the entire population of patients treated in the country’s general hospitals on an inpatient basis, which for the most recent years was 8.4 million patients. The patients proved to be a population so complex and unrecognised in terms of thermal expectations that in the statistical analyses for the total patients, it proved necessary to take a sample for the whole country and the most unfavourable fraction value, thus resulting in high minimum population size. Moreover, taking into account that in the studies on individual hospital wards, the provisions of the standard [10] regarding the minimum sample size for questionnaire studies were fulfilled, as well as taking into account the number of patients in general studies and in analyses of components of thermal comfort in other research (Table 1), for the purposes of further analyses, the minimum sample size of 16 patients was assumed for basic studies, and the minimum sample size of 99 patients for detailed studies. The basic study includes, among other things, a comparison of the results of the mean thermal condition score obtained from the questionnaire surveys with the predictions. In contrast, the detailed study uses a full range of analyses, in addition to a comparison of the actual and predicted percentage of patients dissatisfied with the different ranges of the mean thermal condition score based on the patients’ actual thermal sensations, thermal comfort sensations, and thermal preferences.

Table 1.
Patients population in general research and detailed research studies.
The measurements of microclimate parameters were performed according to the recommendations of standards [7,10,24,25], in the locations where the users usually or presumably stay, and the minimum total duration of the tests within one ward met the requirement of 2 h. The surveys in each patient room were carried out according to the steps outlined below:
- Immediately upon entering the patients’ room, an on-site visit was made, followed by an initial interview with the patients. Patients’ clothing, activity, mobility, and type of bedding and covering were determined, among other things.
- Acclimatisation of the meter and measurement of thermal environment parameters. Recording of thermal environment parameters required to calculate PMV, i.e., air temperature, air velocity, and relative humidity, as well as the temperature of the black ball (the microclimate meter recorded values of the temperature of the black ball, which was then converted in the meter to the corresponding value of the radiation temperature) was carried out using microclimate meters (Ekohigiena, model EHA MM101, and Sensor-Electronic, model SensoData 5500 MK; Figure 1). This was carried out in parallel with the questionnaire study to maintain the correspondence between the conditions recorded by the meter and the conditions felt by the patients (measurements were carried out under the provisions of EN ISO 28802 [24]). Measurement and acclimatisation of the meter at the first measurement point in a given patient room took about 30 min, and at subsequent measurement points, about 15 min.
 Figure 1. The photo of microclimate meter [26].
Figure 1. The photo of microclimate meter [26]. - Collection of patients’ subjective assessments. During the measurement of the thermal environment parameters, patients present in the room were asked to answer questions in a questionnaire, the content of which was under the guidelines presented in EN ISO 7730 [7] and ISO 10551 [25].
Based on the conducted measurements, the PMV index values were calculated, and their results were compared with the actual feelings of patients. In further analyses included in this paper, the following scale of thermal environment ratings was used:
- average rating based on the analysis of thermal sensations (AMVoc): −3—cold, −2—cool, −1—slightly cool, 0—neutral, 1—slightly warm, 2—warm, 3—hot;
- actual average rating based on the analysis of feelings of thermal comfort (AMVkc): 0—comfortable, 1—slightly uncomfortable, 2—uncomfortable, 3—very uncomfortable;
- real average rating based on thermal preference analysis (AMVpc): −3—much warmer, −2—warmer, −1—slightly warmer, 0—no change, 1—slightly cooler, 2—cooler, 3—much cooler;
- prediction by the PMV model of mean evaluation (PMV) and prediction by the adaptive model of mean evaluation (PMV*): −3—cold, −2—cool, −1—slightly cool, 0—neutral, 1—slightly warm, 2—warm, 3—hot.
The calculation of PMV was carried out following the methodology set out in [7], i.e., temperature velocity and air humidity, as well as metabolic rate and thermal insulation of clothing, were substituted for the formula contained in the standard.
3. Results
3.1. PMV Model
The patient-averaged actual mean rating of thermal conditions obtained from the survey of patients’ thermal sensations, thermal comfort sensations, and thermal preferences (AMV) was compared with the patient-averaged predicted mean rating (PMV). The results are shown in Figure 2.
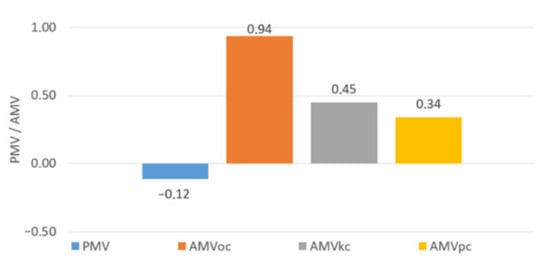
Figure 2.
The predicted mean value of thermal conditions according to PMV vs. actual mean value of thermal conditions according to patients’ thermal sensations (AMVoc), thermal comfort feelings (AMVkc), and thermal preferences (AMVpc).
The predicted mean score deviated to the greatest extent from the actual mean score obtained from the analysis of thermal sensations (the difference between PMV and AMVoc was 1.06), to a significantly lesser extent from the actual mean score obtained from the analysis of thermal comfort sensations (the difference between PMV and AMVkc was 0.57), and to the least extent from the actual mean score obtained from the analysis of thermal preferences (the difference between PMV and AMVpc was 0.48). Regardless of the adopted method of surveying thermal sensations, patients expected cooler thermal conditions than the PMV model predictions indicated. Furthermore, the results showed that the greater intuitiveness of the patient survey with questions about thermal comfort sensations and thermal preferences translated into higher reliability of this form of the patient survey than was the case with questions about thermal sensations. The higher value of the minimum percentage of dissatisfaction obtained in actual surveys than its value predicted by the PMV model may be due to a greater variation in patients’ assessment of the thermal environment than is the case in the group of healthy subjects on which the standard is based [7].
Reference [7] does not provide the calculation methodology for supine patients; therefore, the non-normative methodology of PMV determination [27,28] was used for this group of users, which was also used and positively evaluated in the study [21]. The following analyses attempt to confirm that the computational methodology [27,28] provides similar accuracy in PMV prediction as the normative method [7] applied to sedentary patients. A comparison of the prediction results conducted using the PMV-PPD model with survey results for sitting and recumbent patients is provided in Figure 3.

Figure 3.
Predicted mean value of thermal conditions vs. actual mean value of thermal conditions for different patient activities.
Regardless of the activity of the patients, the discrepancy between the actual and predicted mean rating of the thermal environment is similar, which may provide further justification that computational methodologies [7,27,28] with similar predictive performance were applied to both groups of patients.
The significant difference between the actual and the predicted minimum percentage of dissatisfied patients may also be due to the medical condition of the patients; however, an individual assessment of each patient’s medical condition was not possible. Patients with similar conditions are located within wards of a specific specialisation. Therefore, the analysis of the influence of medical conditions on patients’ perception of the thermal environment was conducted by dividing patients into wards of similar specialisation. Primary analyses comparing the predicted and actual assessment of the thermal environment were carried out for wards with at least 16 patients and are shown in Figure 4.
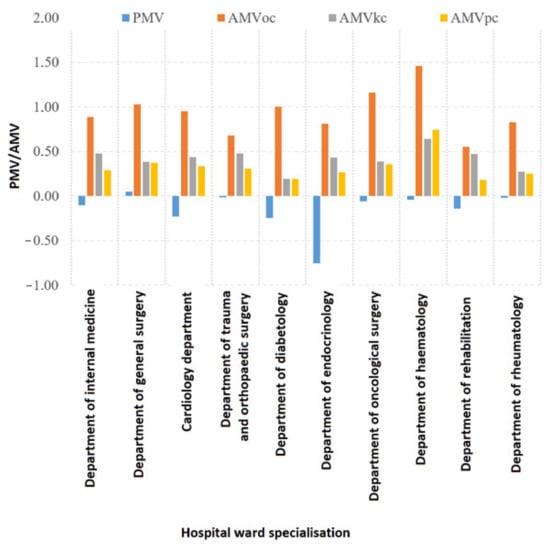
Figure 4.
Predicted mean value of thermal conditions vs. actual mean value of thermal conditions, depending on different specialities of wards [7].
In each speciality, the patients’ mean assessment of the thermal environment indicated that it was too warm. At the same time, the predicted mean assessment of the thermal environment stated that the patient rooms were too cool (except for the General Surgery departments). In addition, there was a discrepancy between the predicted and actual mean rating in each ward, the greatest difference being in the patients’ assessment of thermal sensation, while the smallest difference was usually in the patients’ assessment of thermal preference (except in the haematology wards). The difference between the actual and predicted mean assessment of the thermal environment at each ward varied. In the case of the analysis of thermal sensations, it ranged from 0.69 (Trauma and Orthopaedic Surgery wards) to 1.56 (Endocrinology wards), with a mean for all wards of 1.06. For the analysis of thermal comfort sensations, it ranged from 0.29 (Rheumatology departments) to 1.18 (Endocrinology departments), with an average for all patients of 0.57. The assessment of thermal preference ranged from 0.27 (Rheumatology departments) to 1.02 (Endocrinology departments), with an average for all patients of 0.46. The spectrum of differences between the actual and predicted mean scores in the different wards indicates the influence of the specialisation of the hospital ward and thus also of the patient’s medical condition on their perception of the thermal environment.
3.2. Adaptive Model
De Dear et al. [29] developed a model taking into account the adaptation phenomenon to thermal conditions. One of the manifestations of adaptation is a change in the range of comfortable thermal conditions depending on the external temperature. The existence of this phenomenon in hospital patients’ rooms was verified by comparing the differences between the predicted and actual mean ratings of thermal conditions, which were obtained for different outdoor temperature values. Irrespective of the outdoor temperature, patients expected cooler thermal conditions than forecast; however, the magnitude of this difference varied with outdoor temperature; the lower the outdoor temperature, the larger the group of patients who accepted cooler indoor thermal conditions. This trend ceases below 10 °C, when, regardless of the outside temperature, the difference remains the same and generally coincides with the assumptions of the adaptive model [9]. As assumed by Ref. [9], the adaptation model was not verified for subjects with a metabolic expenditure of less than 1 met. Hence, as shown in Figure 5, this was verified, and it was confirmed that the phenomenon of adaptation occurred regardless of the activity of the patients.
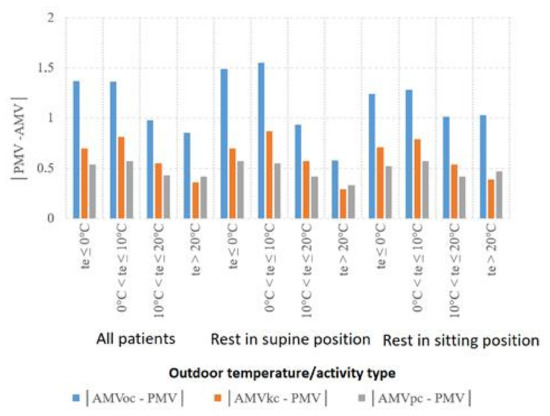
Figure 5.
Difference between actual and predicted mean value of thermal conditions in different climate conditions.
Therefore, the analysis of the adaptive model’s reliability for patients is justified because the phenomena of adaptation to thermal conditions have been confirmed. However, the adaptation model does not provide for the determination of thermal comfort indices as in the case of the PMV model but is based on a graph of the dependence of the permissible values for the individual categories of thermal comfort and operative temperatures on the external temperature. To carry out further analyses in a form similar to the PMV model, it is necessary to make some determinations. The adaptive model is based on the PMV model and, according to Ref. [9], in addition to the thermal comfort condition, it has been assigned the same categories as the PMV model. Since in Ref. [9], concerning the adaptive model, nowhere is it indicated that the categories of thermal comfort should correspond to different values of PMV (predicted mean rating) than for the model specified in [7], for individual categories of thermal comfort, the exact values of the indices mentioned above were assumed as for the PMV model, designating them as PMV* and PPD*. As in the case of the PMV model analysis and in the case of the adaptive model, for all patients, the dependence of the actual and predicted percentage of dissatisfaction on the PMV* index determined by the adaptive model was verified; this was done based on three methods of surveying the conditions of the thermal environment, using questions about thermal sensations, perceived thermal comfort, and thermal preferences (Figure 6).
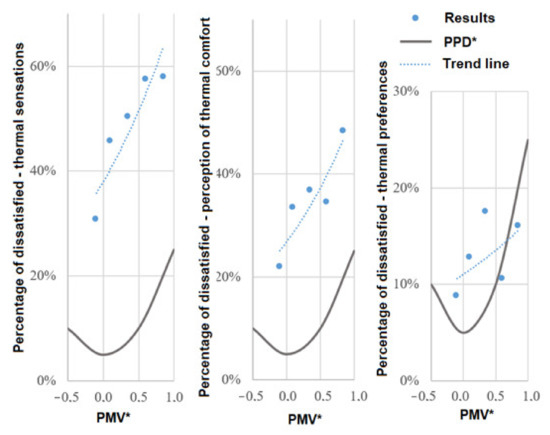
Figure 6.
Actual vs. predicted percentage of dissatisfied patients—a comparative analysis of actual and predicted percentage with the adaptive model percentage of dissatisfied patients in different thermal conditions according to patients’ thermal sensations, thermal comfort feelings, and thermal preferences [9].
Due to the small number of patients residing in conditions predicted by the adaptation model to be cool and slightly cool, the same course and inflexion point of the trend line is not known, so it is also unknown whether the proportion of dissatisfied patients in cooler thermal conditions would be even lower, and whether optimal thermal conditions would occur at lower PMV*. In addition, the shape of the trend line is less smooth than the normative reference curve, indicating a higher rate of dissatisfaction as one moves away from the thermal comfort state. The point of minimum percentage of dissatisfaction could therefore not be determined from the trend line. Instead, the location of the survey point with the lowest percentage of dissatisfaction was determined. The results of the survey of thermal sensations, thermal comfort sensations, and thermal preferences among all patients indicate that the point of the minimum percentage of dissatisfaction is shifted towards slightly cool conditions and occurs in the range of PMV* values from −0.2 to 0; it is 31% for the survey of thermal sensations, 22% for the survey of thermal comfort sensations, and 9% for the survey of thermal preferences.
4. Directions for Modifying Thermal Comfort Models
The analyses showed that the thermal comfort model [7] did not achieve satisfactory performance in predicting the mean rating of thermal conditions in patients’ rooms. The results obtained for the patients showed that they are a far more diverse group in terms of their perception of the thermal environment than the office workers or students whose responses formed the basis for the PMV model. Given this observation, the analyses were directed at identifying the factors causing this diversity and indicating directions for further research. The analyses conducted, regardless of the thermal comfort model used, encountered a higher actual percentage of dissatisfaction than predicted, a different distribution of actual thermal sensations relative to the reference according to [7], a shift in patients’ thermal expectations relative to predicted ones, and a different shape of the trend line than the reference PPD or PPD* curve. At the same time, the critical issue that needs to be clarified first is the significantly higher actual percentage of dissatisfaction obtained from the survey of thermal sensations, and in particular its minimum value, than the percentage of dissatisfied patients predicted by any of the thermal comfort models, and consequently also the different distribution of thermal sensations. The high value of the minimum percentage of dissatisfaction and the different shape of the trend line indicates the differentiation of the surveyed group in terms of thermal sensations, which may result from higher and more differentiated expectations of thermal comfort. The high value of the minimum percentage of dissatisfied patients and the different shapes of the trend line indicate the diversity of the study group in terms of thermal sensations, which may be due to, among others, higher and more varied thermal expectations among patients, diversity of medical conditions, the incomprehensibility of terms used to describe thermal sensations, the issue of taking adaptation into account, inaccuracy in determining the metabolic expenditure of patients and the thermal insulation of clothing, and a large percentage of patients with advanced age. At the same time, it should also be borne in mind that some inaccuracies may result from the fact that the study was conducted in actual facilities and not in laboratory conditions.
Studies conducted in actual facilities are often characterised by users who have no experience in surveying the thermal environment conditions; the patients studied were one such group. The primary normative form of assessing thermal conditions is the survey of thermal sensations; however, in studies with an untrained panel, questions about the level of thermal comfort and thermal preferences are often used. However, as noted by various authors [14,18,21], the scales of thermal preferences and sensations are not equivalent, and the scale of thermal comfort is most similar to the scale of thermal comfort. The values of the percentage of dissatisfaction obtained in the study in the case of the evaluation of actual thermal sensations were the highest; in the case of thermal comfort, they were significantly lower but still above the forecast values, while in the case of actual thermal preferences, they were the lowest and were close to the forecast values. The results closer to the prognosis obtained when surveying feelings of thermal comfort or thermal preference indicate that the form used to define the different states of thermal preference and thermal comfort was more intuitive than in the case of the question about thermal sensations. In particular, patients overused the terms slightly warm and warm in the winter season and the terms cool and slightly cool in the summer season. This may have been since patients did indeed feel comfortable or even more comfortable in non-neutral conditions. However, a summary of the heat sensation questionnaire results shows that this was most often due to a different understanding of the terms used to define heat sensations. The above observations suggest that modifications to thermal comfort models are best made based on the survey of thermal comfort sensations. In subsequent studies conducted under actual conditions, it is recommended to maintain the comprehensive survey of thermal sensations and use the three forms of questions mentioned above. In addition, given the smaller discrepancies between thermal sensations and thermal preferences in other studies [14,18] conducted in hospital settings, verifying the normative terms used for thermal sensations is recommended, including ensuring the quality of the translation from English and searching for synonyms that will allow the introduction of more intuitive terms, although this is not the case in Ref. [7].
The adaptation model included in Ref. [9] is a modification of the PMV model aimed, among others, at taking into account the adaptation phenomenon depending on external thermal conditions. Based on the comparison of the mean assessment predicted by the PMV-PPD model with the actual mean assessment of the thermal environment for individual ranges of external temperature, it was proven that the actual thermal expectations of the tested patients depended on the weather conditions. The difference between the actual and predicted mean assessment of the thermal environment changed with outdoor temperature changes. In contrast, according to the assumptions of the adaptive model [9], in the heating period, the influence of outdoor temperature ceased. In addition, the use of the adaptive model following Ref. [9] is conditional on many assumptions, referred to in the standard as required or recommended. The normative adaptation model was developed based on studies among users whose metabolic expenditure ranges from 1 met to 1.3 met. Although the patients in the patient rooms showed activities with lower metabolic expenditure, it was confirmed that adaptation occurred in the present study. In addition, consideration of the adaptation phenomenon is contingent on ensuring that the clothing set can be adjusted (at least between 0.5 clo and 1.0 clo). Access to adjust the degree of window opening should also be provided. In the vast majority of patient rooms, the possibility to open or tilt the windows was provided, and there were no rules that would limit the possibility of adjusting clothing within the range given in the standard. This range was even wider, as patients were also provided with bedding. However, patients were characterised by different mobility, which for some resulted in the fact that access to windows and modification of clothing or bedding was possible only with the help of a few medical personnel. Additionally, in multi-bed rooms, the access to adjust the degree of window opening was sometimes limited due to the different thermal expectations of patients.
Moreover, the standard recommendations [9] were different depending on the ward, i.e., different technical solutions limited the negative effects of the thermal environment (e.g., roller blinds, shutters, room ventilators). In contrast, others depended on the patient’s condition, i.e., changes in body posture and physical activity modifications [9]. Therefore, adaptation to thermal conditions for patients in hospital rooms is a more complex process than is the case for healthy individuals, on whom the adaptation model is based [9]. Notwithstanding the above, the adaptive model [9] has achieved greater reliability in predicting the mean rating of thermal conditions in patients’ rooms and has been found to better represent the perception of the thermal environment by the patients studied. Its potential for development is also higher; although, in many aspects, it should be modified to take proper account of the possibilities of patients’ adaptation to thermal conditions. Further studies should also include facilities with cooler thermal conditions, which unfortunately may be challenging to achieve in actual facilities. The influence on the perception of the thermal environment of individual adaptation components should be thoroughly assessed by classifying patients according to the available forms of adaptation and the period of adaptation to thermal conditions in the patient’s room (patient hospitalisation time).
The PMV model, in contrast to the adaptive model, requires the determination of individual parameters, i.e., the type of activity and the set of clothing and bedding used. The metabolic expenditure of the patients was determined according to the second level of precision and taken from tables formulated for healthy subjects, as metabolic expenditure values for sick subjects are not currently available and need to be supplemented. In addition, the metabolic expenditure in elderly people performing the same type of activity as younger people is usually lower; Ref. [30], however, allows the adoption of standard values of the percentage of dissatisfaction for larger groups of people when elderly people are among them. On the other hand, the percentage of elderly people in patients’ rooms is much higher than in standard rooms. The basic or total insulation of clothing, bed, and bedding was determined based on observation and interviews and based on the values of total insulation of bedding (It,bedding) and basic insulation of clothing layers (Iclu) taken from Refs. [31,32]. In this method, measurement inaccuracies cannot be excluded. At the same time, the clothing and garments used by the patients were highly variable. The predictions of the PMV model are highly sensitive to any inaccuracies in this respect [33]. Therefore, when conducting analyses with models requiring the determination of activity and thermal insulation of clothing, it is recommended to use a methodology that provides greater accuracy in determining individual parameters, specifically by determining metabolic expenditure with a higher level of precision (verifying beforehand that its values for the tested patients are the same as for healthy persons). Additionally, it is important to maintain the highest accuracy and meticulousness in determining the clothing sets, type of bedding, and to what extent the body is covered by these, as well as, if possible, perform laboratory verification of thermal insulation of clothing sets and bedding used by the patients. Hospital patients are heterogeneous in terms of their medical condition, whereas the healthy subjects on whom the thermal comfort models are based are significantly less heterogeneous. The above-described fact and the high heterogeneity of patients’ thermal expectations suggest that the reasons for this heterogeneity should be sought in the medical condition of the subjects. Patients’ medical status was differentiated by, among others, the phase of the treatment process, invasiveness of medical procedures, the current and planned duration of hospitalisation, well-being, and health status. The general well-being of patients participating in the study was good (about 65%) or indifferent (about 35%), with patients feeling normal (about 60%) or lethargic (about 30%). Still, more than half of the patients refused to participate in the study, which was often dictated by, among other things, poor well-being or health status. Detailed analyses of the influence of patients’ health status and well-being on the assessment of the thermal environment were omitted, as it was considered that the factors mentioned above could significantly affect the results of the analyses.
5. Discussion
A problematic issue related to the determination of thermal parameters for patient rooms is the fact that the standards require the use of a thermal comfort model that converts the recommended values for the maximum percentage of users’ dissatisfaction. However, the available normative thermal comfort models [7,9] have not yet been verified on a statistically reliable sample of patients. The vast majority of studies with topics similar to those addressed in this paper have been conducted on a population not exceeding 100 patients, which was significantly smaller than the population in the present study (890 patients), by Skoog et al. [34], Giuli et al. [16], Hashiguchi et al. [22,23], Khodakarmi et al. [17], Pourshaghaghy et al. [20], and Verheyen et al. [21]. Other studies were conducted in hospitals located in climatic zones other than Poland and on a sample close to or larger than the minimum population size of 423 patients, such as those by Nematchoua et al. [18,19] in Madagascar in a group of 198 patients, Sattayakorn et al. [35] in Thailand in a group of 451 patients, and Hwang et al. [14] in Taiwan in a group of 927 patients. All the studies mentioned above took place in hospital patient rooms, except for Ref. [35], which was conducted with patients in waiting rooms (temporary stay of people, averaging about 2 h). In the present study, selected thermal comfort models were analysed and verified in the context of the accuracy of predicting the thermal sensations of patients in hospital patient rooms, based on parallel questionnaire studies, measurements of the thermal environment, and visual assessment of individual parameters, i.e., the type of clothing and bedding used, as well as the type of activity. The methodology of the study, which is of key importance for obtaining reliable results, was based on expert consultations, analysis of the current state of knowledge [36], pilot studies carried out, and results and conclusions from previous studies conducted on hospital patients’ rooms [13,14,17,18,19,22]. The PMV [7] and adaptive [9] models were included in the scope of analysis. They were chosen because they predicted thermal sensations based on environmental conditions and visual assessment of the user’s thermal characteristics without requiring measurements of parameters in the patient’s body area and were based on the normative [7] scale for assessing thermal sensations. An additional advantage was that the aforementioned thermal comfort models were also used in other studies conducted in hospital patient rooms. In the case of the PMV model, it was used in Ref. [36], while the adaptive model was used only in Ref. [19], where it was not verified. The application of the adaptive model to the patients is justified because, as proven in the present study, the actual thermal expectations of the tested patients depended on the weather conditions and were subject to the phenomenon of adaptation. Nevertheless, the use of the PMV model was justified only in publications [17,34,35], where patient rooms were equipped with a cooling system [17,34] or patients were temporarily staying in the ward [35]. In studies [14,16,20,21], it was not justified why the phenomenon of users’ adaptation to thermal conditions was not considered in the analyses of results, and the PMV model was chosen instead of the adaptation model for the analysis of results. In publications [22,23], radiation temperature, air velocity, and individual parameters were not recorded, making it impossible to verify the PMV model for patients. The analysis of PMV and adaptive models conducted in the present study, concerning all patients, showed inaccuracies in predicting the mean thermal environment rating and the predicted percentage of dissatisfied patients using normative thermal comfort models, which was also confirmed in publications [34,35]. The patients studied preferred cooler thermal conditions than the predictions of the PMV and adaptive models, but the results obtained in the analyses conducted for the adaptive model were closer to the predicted ones, and this thermal comfort model should be considered as better at accounting for thermal expectations. On the other hand, Ref. [20] confirmed the effectiveness of the PMV model in predicting the mean rating of the thermal environment and the percentage of dissatisfaction and noted that the respondents showed greater sensitivity to thermal conditions than predicted by the PMV model. However, the results of this study [20] should be taken with caution, as the methodology of the study was burdened with the following simplifications: results were compiled for medical staff and patients together, the same value of thermal resistance of a set of clothes was assumed for all users, the same values of metabolic expenditure were assumed for all patients and medical staff, and thermal conditions were recorded using a measuring grid and not necessarily near to the patient’s bed. Reference [14] also assumed the same activity and thermal insulation of clothing for all patients, and the study confirmed the reliability of the PMV model for the winter season. In the summer season, the studied patients expected cooler conditions than predicted and, regardless of the season, showed less sensitivity to adverse thermal conditions than predicted by the PMV model. In contrast, studies [21,34,35] also reported a shift in patients’ thermal expectations towards cooler conditions than predicted by the PMV model, and studies [21,35] additionally observed a decrease in the accuracy of the PMV model’s prediction of thermal sensation as it moved away from neutral temperature. Although the research methodologies included assumptions that could have affected the results obtained, Ref. [35] was conducted in a hospital waiting room instead of patient rooms, and radiation temperature and air velocity were not measured. In Ref. [34], activity was not determined for each patient, and in the methodology of Ref. [21], no such criteria were noticed. In addition, the present study also showed that patients are a group of users with strongly different thermal expectations, which is due to, among other things, the diversity of medical conditions, the incomprehensibility of the terms used to describe thermal sensations, the issue of taking adaptation into account, higher and more varied thermal expectations among patients, inaccuracies in determining the metabolic expenditure of patients, the thermal insulation of clothing, and the high proportion of patients of advanced age. Studies conducted in real facilities are often characterised by users who have no experience in surveying the thermal environment conditions; the patients studied were one such group. The basic, normative form of assessing thermal conditions is the survey of thermal sensations; however, in studies with an untrained panel, questions about the level of thermal comfort and thermal preferences are often used. However, as noted by the authors in Refs. [14,21], the scales of thermal preferences and thermal sensations are not equivalent, and the scale of thermal sensations is most similar to the scale of thermal comfort. The values obtained in the study of the lowest percentage of dissatisfaction in the case of evaluation of thermal sensations were the highest, in the case of thermal comfort significantly lower but still above the predicted values, and in the case of thermal preferences, the lowest and close to the predicted values. Stronger differentiation of thermal expectations in patients of the analysed patient rooms was also due to different medical conditions of the patients; individual assessment of each patient’s medical condition was not possible, but patients with similar specificity of diseases were located within wards of equal specialisation. Basic analyses of the thermal environment were carried out for 10 of the 14 specialisations of hospital wards, following the established criterion of the minimum number of patients. The difference between the actual and predicted mean assessment of the thermal environment in each ward varied, with the spectrum of differences indicating that the assessment of thermal conditions depended on the specialisation of the hospital ward. In addition, detailed analyses were also conducted for selected hospital ward specialisations (Internal Medicine, General Surgery, and Cardiology wards). The adaptive model proved to be more reliable in predicting the assessment of the thermal environment for patients residing in individual wards. In each ward, the distribution of test points enabled a trend line to be drawn, although the adaptive model was not verified over the full range of thermal conditions due to the small number of patient rooms with thermal conditions with a PMV* of less than −0.2. The obtained values of the percentage of dissatisfaction were similar to those recorded for the total number of patients. However, the course of the trend line for the general surgery and internal medicine wards clearly indicated that they would obtain lower values of the percentage of dissatisfaction at a PMV* less than −0.2. The point of optimal thermal conditions was shifted towards cooler conditions than those predicted by the adaptation model, and in the case of the cardiology speciality wards, towards warmer conditions. In summary, the analysis of thermal conditions in individual wards showed that they varied according to the specialisation of the ward. However, it also showed that factors still significantly differentiate patients’ perceptions of the thermal environment. Different conclusions were formulated in Ref. [35]. However, it is worth mentioning that the study discussed therein was conducted in a hospital waiting room instead of patient rooms, and radiation temperature and air velocity were not measured. It was found that while the psychological well-being of patients and the duration of stay in the ward were factors affecting the actual mean assessment of thermal conditions, health status was not (except for patients from cardiology, gynaecology and urology wards). On the other hand, results similar to those obtained in the present study were presented in Ref. [14], where it was found that thermal sensations of the studied group of patients did not depend, to a great extent, on gender and age. At the same time, medical condition and hospitalisation time differentiated patients’ actual perception of the thermal environment. Acclimatisation of patients to thermal conditions in the patient rooms lasted up to a week; during this period, their length of stay in the hospital affected their perception of the thermal environment. Patients usually compensated for unfavourable thermal sensations by adjusting their clothing [14], followed by full acclimatisation to thermal conditions. In addition, in a study [16], thermal conditions were recorded in wards with different specialisations, with patients in internal medicine wards expecting cooler conditions, and patients in orthopaedic wards expecting warmer conditions. However, it should be borne in mind that the following assumptions may have influenced the results obtained in the publication [16]: surveys and measurements were not conducted in parallel, the activity and type of clothing were not determined individually for each patient, and measurements were taken in the middle of the room and thus not always close to the patients. The thermal expectations of the patients proved to be different and more diverse than those of the office workers or students from whom the PMV and adaptive models were developed. In addition, analysis of ratings of thermal conditions across wards showed that these varied by ward specialisation, although it also showed that there were still factors that significantly differentiated patients’ perceptions of the thermal environment. Among the factors that may cause different perceptions of the thermal environment, medical issues such as the phase of the treatment process, the well-being of patients, their health status, or details of ailments and conditions should be the subject of further research work in this direction.
6. Conclusions
Based on the analyses carried out, the following conclusions were drawn:
- The analyses showed that the thermal comfort model [7] did not achieve satisfactory performance in predicting the mean rating of thermal conditions in patients’ rooms. We can see the reasons for this in the following issues: patients are a far more diverse group in terms of their perception of the thermal environment than the office workers or students whose responses formed the basis for the PMV model; moreover, patients seemed to answer the questionnaire by marking ‘warm’ with the feeling characterised as ‘neutral’. In addition, the PMV value is strongly influenced by the accurate determination of individual parameters, i.e., the type of activity and the set of clothing and bedding used. Although we determined the metabolic rate and the thermal clothing insulation using the best knowledge, normative data, and recent publications, we believe that for people who are ill, elderly, or have impaired mobility, the metabolic rate is not yet determined accurately enough, as well as the thermal insulation of clothing sets and bedding is not sufficiently recognised in the literature.
- The adaptive model provides higher forecasting reliability for thermal environment assessment than the PMV model. However, the results of the analyses indicate that patients are more diverse in terms of thermal expectations than students and office workers, on whom the normative models are based, and expect slightly cooler conditions than predicted.
- The study patients adapted to the thermal conditions. At the same time, the distribution of results was different from that predicted by the adaptation model, indicating that the patients may have shown lower acceptability of adverse thermal conditions or the adaptation process itself may have occurred differently, i.e., the study patients may have adapted to the thermal conditions to a different extent than predicted by the adaptation model, or this may have been due to an unwarranted or overly strong consideration of adaptation for some patients.
- The specialisation of the hospital wards in which patients were housed differentiated in their thermal expectations, with the adaptive model proving more reliable in predicting thermal environment ratings for patients housed on individual wards. The results of the individual ward studies showed that there are still factors that differentiate patients’ perceptions of the thermal environment, including medical issues that have not yet been identified as having an impact on perceptions of the thermal environment, such as the phase of the treatment process, patients’ well-being, health status, or details of ailments and conditions.
- The results of the study were the furthest from the predicted ones in the case of the survey of thermal sensations, closer to the predicted ones in the case of the survey of thermal comfort sensations, and in the case of the survey of thermal preferences, they were the closest to the predicted ones; however, Refs. [14,21,28] have shown that the scales of thermal preferences and thermal sensations are not equivalent, and the scale of thermal sensations is most similar to the scale of thermal comfort. On this basis, it was concluded that the surveyed patients most reliably assessed thermal conditions in patients’ rooms by determining the degree of thermal comfort.
Author Contributions
Conceptualization, P.U. and A.B.; methodology, P.U. and A.B.; investigation, P.U.; writing—original draft preparation, A.B.; writing—review and editing, A.B.; supervision, A.B.; project administration, A.B.; funding acquisition, A.B. All authors have read and agreed to the published version of the manuscript.
Funding
Research was funded by Halton Foundation Inc. grant and Warsaw University of Technology within the Excellence Initiative: Research University (IDUB) programme.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Wargocki, P. Indoor Climate and Productivity in Offices: How to Integrate Productivity in Life-Cycle Cost Analysis of Building Services; REHVA Guidebook No. 6; REHVA: Ixelles, Belgium, 2006. [Google Scholar]
- Mujan, I.; Anđelković, A.S.; Munćan, V.; Kljajić, M.; Ružić, D. Influence of indoor environmental quality on human health and productivity—A review. J. Clean. Prod. 2019, 217, 646–657. [Google Scholar] [CrossRef]
- Roelofsen, P. The impact of office environments on employee performance: The design of the workplace as a strategy for productivity enhancement. J. Facil. Manag. 2002, 1, 247–264. [Google Scholar] [CrossRef]
- Akimoto, T.; Tanabe, S.; Yanai, T.; Sasaki, M. Thermal comfort and productivity—Evaluation of workplace environment in a task conditioned office. Build. Environ. 2010, 45, 45–50. [Google Scholar] [CrossRef]
- Kim, J.; Bauman, F.; Raftery, P.; Arens, E.; Zhang, H.; Fierro, G.; Andersen, M.; Culler, D. Occupant comfort and behavior: High-resolution data from a 6-month field study of personal comfort systems with 37 real office workers. Build. Environ. 2019, 148, 348–360. [Google Scholar] [CrossRef]
- Kwon, M.; Remøy, H.; van den Dobbelsteen, A.A.J.F.; Knaack, U. Personal control and environmental user satisfaction in office buildings: Results of case studies in the Netherlands. Build. Environ. 2019, 149, 428–435. [Google Scholar] [CrossRef]
- ISO 7730:2005; Ergonomics of the Thermal Environment—Analytical Determination and Interpretation of Thermal Comfort Using Calculation of the PMV and PPD Indices and Local Thermal Comfort Criteria. ISO: Geneva, Switzerland, 2005.
- de Dear, R.; Brager, G.S. Developing an adaptive model of thermal comfort and preference. ASHRAE Trans. 1998, 104 Pt 1, 1–18. [Google Scholar]
- EN 16798-1:2019; Energy Performance of Buildings—Ventilation for Buildings—Part 1: Indoor Environmental Input Parameters for Design and Assessment of Energy Performance of Buildings Addressing Indoor Air Quality, Thermal Environment, Lighting and Acoustics—Module M1-6. European Committee for Standardization: Brussels, Belgium, 2019.
- ASHRAE 55-2013: ANSI/ASHRAE 55:2013; Thermal Environmental Conditions for Human Occupancy. ASHRAE: Atlanta, GA, USA, 2013; p. 30.
- Breslin, R. Gender Differences and Thermal Comfort Requirements; Final Year Undergrade Report; Department of Human Science, Loughborough University: Loughborough, UK, 1995. [Google Scholar]
- Costa, I.T.; Wollmann, C.A.; Gobo, J.P.A.; Ikefuti, P.V.; Shooshtarian, S.; Matzarakis, A. Extreme Weather Conditions and Cardiovascular Hospitalizations in Southern Brazil. Sustainability 2021, 13, 12194. [Google Scholar] [CrossRef]
- Webb, L.; Parsons, K. Thermal comfort requirements for people with physical disabilities. Proc. Hum. Factors Ergon. Soc. Annu. Meet. 2000, 44, 114–121. [Google Scholar]
- Hwang, R.-L.; Lin, T.-P.; Cheng, M.-J.; Chien, J.-H. Patient thermal comfort requirement for hospital environments in Taiwan. Build. Environ. 2007, 42, 2980–2987. [Google Scholar] [CrossRef]
- Peel, M.C.; Finlayson, B.L.; McMahon, T.A. Updated world map of the Köppen-Geiger climate classification. Hydrol. Earth Syst. Sci. 2007, 11, 1633–1644. [Google Scholar] [CrossRef] [Green Version]
- de Giuli, V.; Zecchin, R.; Salmaso, L.; Corain, L.; De Carlia, M. Measured and perceived indoor environmental quality: Padua Hospital case study. Build. Environ. 2013, 59, 211–226. [Google Scholar] [CrossRef]
- Khodakarami, J.; Knight, I. Required and current thermal conditions for occupants in iranian hospitals. HVAC&R Res. 2008, 14, 175–193. [Google Scholar]
- Nematchoua, M.K.; Ricciardi, P.; Reiter, S.; Asadi, S.; Demers, C.M.H. Thermal comfort and comparison of some parameters coming from hospitals and shopping centers under natural ventilation: The case of Madagascar Island. J. Build. Eng. 2017, 13, 196–206. [Google Scholar] [CrossRef] [Green Version]
- Nematchoua, M.K.; Ricciardia, P.; Burattic, C. Statistical analysis of indoor parameters an subjective responses of building occupants in a hot region of Indian ocean; a case of Madagascar island. Appl. Energy 2017, 208, 1562–1575. [Google Scholar] [CrossRef] [Green Version]
- Pourshaghaghy, A.; Omidvari, M. Examination of thermal comfort in a hospital using PMV-PPD model. Appl. Ergon. 2012, 43, 1089–1095. [Google Scholar] [CrossRef] [PubMed]
- Verheyen, J.; Theys, N.; Allonsius, L.; Descamps, F. Thermal comfort of patients: Objective and subjective measurements in patient rooms of a Belgian healthcare facility. Build. Environ. 2011, 46, 1195–1204. [Google Scholar] [CrossRef]
- Hashiguchi, N.; Hirakawa, M.; Tochihara, Y.; Kaji, Y.; Karaki, C. Effects of setting up of humidifiers on thermal conditions and subjective responses of patients and staff in a hospital during winter. Appl. Ergon. 2008, 39, 158–165. [Google Scholar] [CrossRef]
- Hashiguchi, N.; Hirakawa, M.; Tochihara, Y.; Kaji, Y.; Karaki, C. Thermal Environment and Subjective Responses of Patients and Staff in a Hospital during Winter. J. Physiol. Anthr. Appl. Hum. Sci. 2005, 24, 111–115. [Google Scholar] [CrossRef] [Green Version]
- ISO 28802:2012; Ergonomics of the Physical Environment—Assessment of Environments by Means of An Environmental Survey Involving Physical Measurements of the Environment and Subjective Responses of People. ISO: Geneva, Switzerland, 2012.
- ISO 10551:2019; Ergonomics of the Physical Environment—Subjective Judgement Scales for Assessing Physical Environments. ISO: Geneva, Switzerland, 2019.
- Available online: https://www.ekohigiena.com.pl/miernik-mikroklimatu-eha-mm-101 (accessed on 16 March 2022).
- Lin, Z.; Deng, S. A study on the thermal comfort in sleeping environments in the subtropics—Developing a thermal comfort model for sleeping environments. Build. Environ. 2008, 43, 70–81. [Google Scholar] [CrossRef]
- Gagge, A.P.; Fobelets, A.P.; Berglund, L.G. A standard predictive index of human response to the thermal environment. ASHRAE Trans. 1986, 92, 709–731. [Google Scholar]
- de Dear, R.; Brager, G.S. Developing an Adaptive Model of Thermal Comfort and Preference-Final Report (ASHRAE RP-884); ASHRAE: Atlanta, GA, USA, 1997. [Google Scholar]
- ISO 28803:2012; Ergonomics of the Physical Environment—Application of International Standards to People with Special Requirements. International Organization for Standardization: Geneva, Switzerland, 2012.
- Lin, Z.; Deng, S. A study on the thermal comfort in sleeping environments in the subtropics—Measuring the total insulation values for the bedding systems commonly used in the. Build. Environ. 2008, 43, 905–916. [Google Scholar] [CrossRef]
- ISO 9920:2007; Ergonomics of the Thermal Environment—Estimation of Thermal Insulation and Water Vapour Resistance of a Clothing Ensemble. ISO: Geneva, Switzerland, 2007.
- Hasan, M.H.; Alsaleem, F.; Rafaie, M. Sensitivity study for the PMV thermal comfort model and the use of wearable devices biometric data for metabolic rate estimation. Build. Environ. 2016, 110, 173–183. [Google Scholar] [CrossRef]
- Skoog, J.; Fransson, N.; Jagemar, L. Thermal environment in Swedish hospitals: Summer and winter measurements. Energy Build. 2005, 37, 872–877. [Google Scholar] [CrossRef]
- Sattayakorn, S.; Ichinose, M.; Sasaki, R. Clarifying thermal comfort of healthcare occupants in tropical region: A case of indoor environment in Thai hospitals. Energy Build. 2017, 149, 45–57. [Google Scholar] [CrossRef]
- Uścinowicz, P.; Chludzinska, M.; Bogdan, A. Thermal environment conditions in Polish operating rooms. Build. Environ. 2015, 94, 296–304. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).