Models and Indicators to Assess Thermal Sensation Under Steady-State and Transient Conditions
Abstract
:1. Introduction
2. Steady-state Conditions
2.1. Heat Balance Equation of the Human Body
| metabolic rate, the sum between the metabolic rate required for the person’s activity and the metabolic rate required for shivering : ; | |
| effective mechanical power, “the energy spent in overcoming external mechanical forces on the body”; | |
| total rate of heat loss from skin; | |
| total rate of heat loss through respiration; | |
| sensible heat loss from skin; | |
| convective heat flow, “the heat exchange by convection between the boundary surface (clothing or skin) and environment”; | |
| radiative heat flow, “the heat exchange by radiation between the boundary surface (clothing or skin) and environment”; | |
| the evaporative heat flow at the skin, “the rate at which heat energy is transferred by evaporation from or condensation on the skin”; | |
| respiratory convective heat flow, “the heat exchanges by convection in the respiratory tract”; | |
| respiratory evaporative heat flow, “the heat exchanges by evaporation in the respiratory tract”; | |
| body heat storage rate, “the rate of increase (+) or decrease (−) in the heat content of the body caused by an imbalance between heat production and heat loss”; | |
| rate of heat storage in the skin compartment; | |
| rate of heat storage in the core compartment. |
| fraction of the body mass concentrated in the skin compartment, dimensionless; | |
| specific heat capacity of body, with ; | |
| DuBois body surface area, “the total surface area of a nude person”, with , ; | |
| body mass, kg; | |
| body height, m; | |
| core temperature, “the mean temperature of the thermal core of the body”, ; | |
| local skin temperature, “the skin temperature measured at a specific point of the body surface”, ; | |
| time, s. |
Heat Losses from the Body to Outer Surrounding
- The sensible heat loss from the skin can be expressed as:where the terms are defined according to the Standard ISO 13731:2001 [31]:
total heat transfer coefficient, the sum between the convective heat transfer coefficient and radiative heat transfer coefficient , , ; convective heat transfer coefficient, “the net sensible heat transfer per unit area between a surface and a moving fluid medium per unit temperature difference between the surface and the medium”, ; radiative heat transfer coefficient, “the net rate of heat transfer per unit area by radiation between two surfaces, per unit temperature difference between the surfaces”, ; operative temperature, “uniform temperature of an imaginary black enclosure in which an occupant would exchange the same amount of heat by radiation plus convection as in the actual non-uniform environment”, ; air temperature, “the dry-bulb temperature of the air surrounding the occupant, ; mean radiant temperature, “uniform temperature of an imaginary black enclosure in which an occupant would exchange the same amount of radiant heat as in the actual non-uniform enclosure”, ; clothing area factor , “ratio between the surface area of the clothed body, including unclothed parts, and the surface of the nude body”, dimensionless; thermal resistance of clothing, . - The evaporative heat flow at the skin is the sum between evaporative heat loss by regulatory sweating and diffusion evaporative heat loss :where the terms are defined as in the Standard ISO 13731:2001 [31]:
skin wettedness, “the equivalent fraction of the skin surfaces which can be considered as fully wet,” dimensionless; skin wettedness caused by diffusion, represents the zone of the human body which has to be wetted to evaporate the regulatory sweat: maximum possible evaporative heat flow at the skin, “the heat flow due to evaporation that can be achieved in the hypothetical case of the skin completely wetted”; occurs when skin wittedness is : saturated water vapour pressure at skin temperature, ; water vapour partial pressure, “the pressure which the water vapour would exert if it alone occupied the volume occupied by the humid air at the same temperature”, kPa; evaporative resistance of a clothing ensemble, “resistance to vapour transport of a uniform layer of insulation covering the entire body that has the same effect on evaporative heat loss as the actual clothing under (static, wind-still) conditions”, ; evaporative heat transfer coefficient, “net latent-heat per unit vapour-pressure difference caused by the evaporation of water from a unit area of a wet surface or by condensation of water vapour on a unit area of body surface”, . - The respiratory heat flow is the sum between the respiratory convective heat flow and the respiratory evaporative heat flow :
2.2. Approaches for Assessing Indoor and Outdoor Human Thermal Indices
2.3. Fanger One-Dimensional Model
2.4. PMV Index for Thermal Sensation Prediction
- The convective heat transfer coefficient is solved by iterations and is given by:
- The ratio of clothed surface area is expressed by:
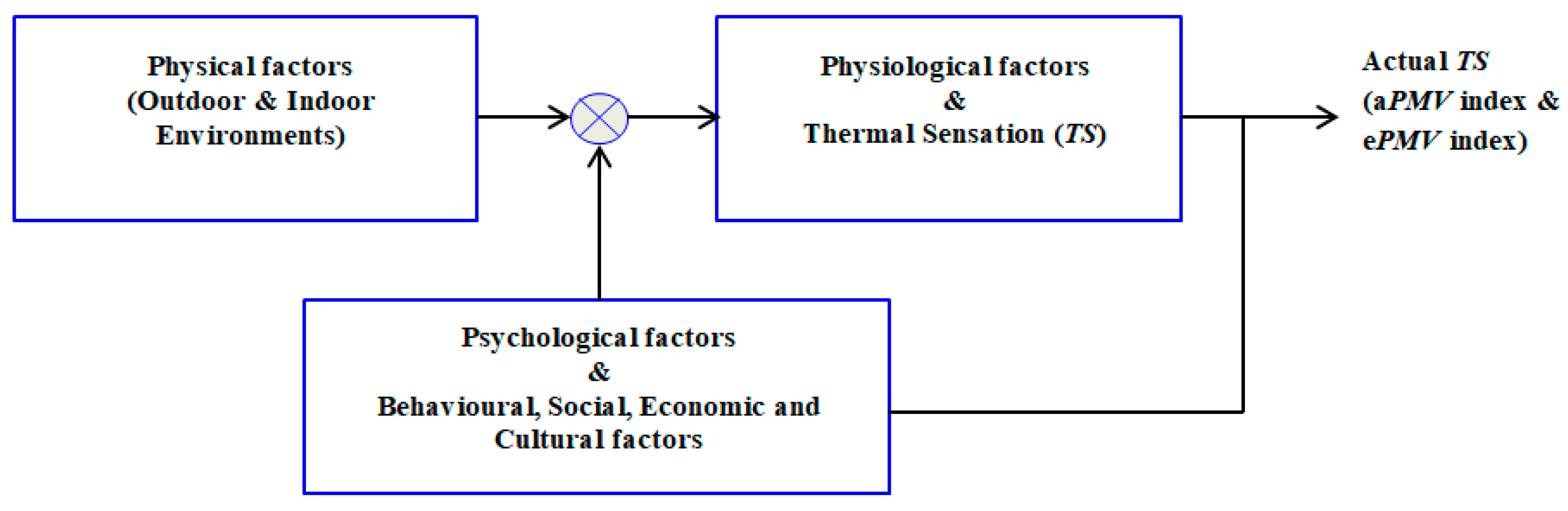
2.5. Psychological Factors, Adaptive PMV Index and Extended PMV Index
2.6. Local Discomfort Assessment Models
3. Transient Conditions
3.1. Non-Uniform Energy Balance Models
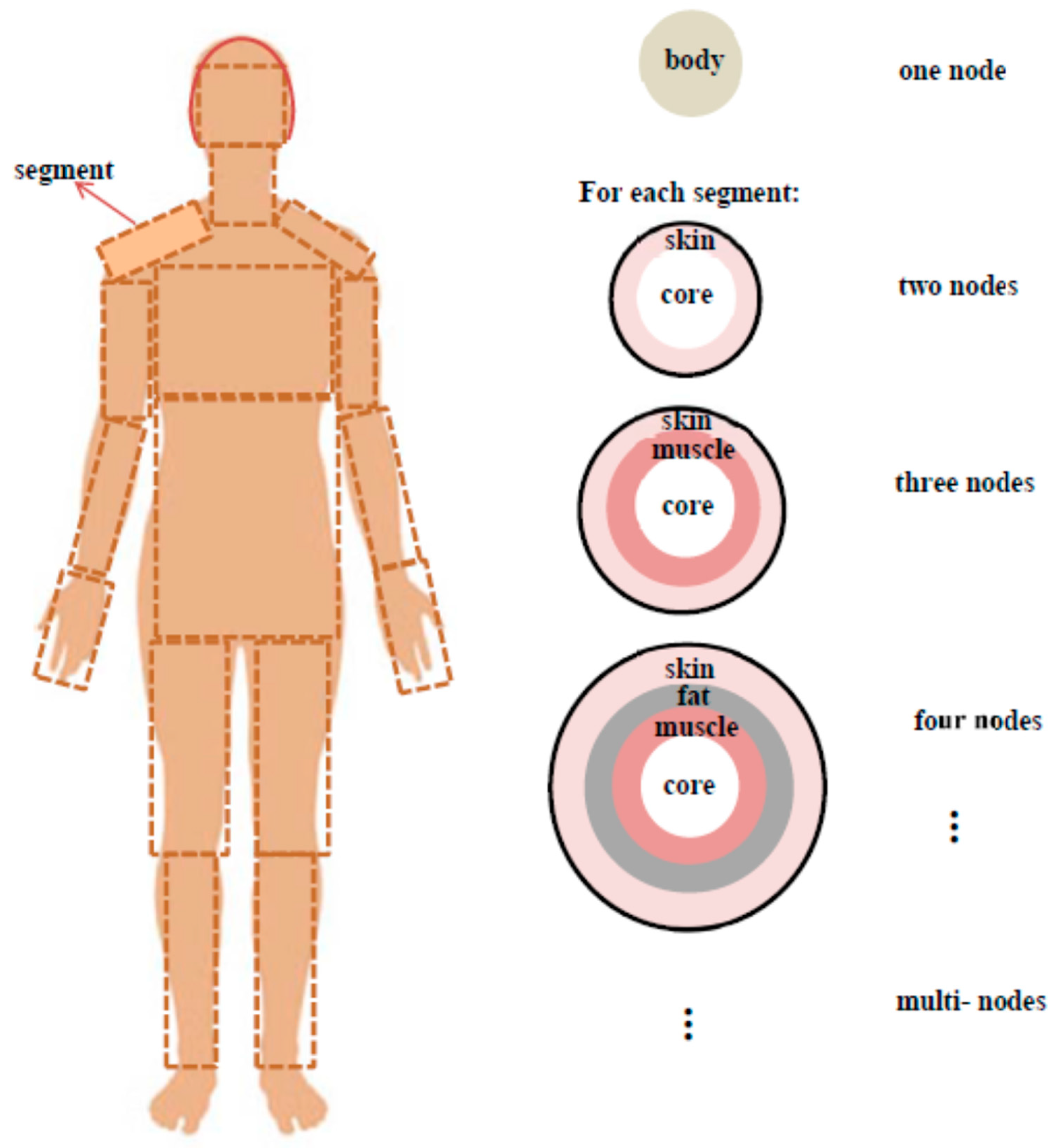
- Body segments: the body can be represented as a single component or as a set of interconnected components called segments (e.g., head, trunk, fore arms, upper arms, fingers, hand, legs, etc.).
- Thermal nodes: each body segment can be represented by using multiple concentric layers or thermal nodes (e.g., two layers with the core part of the body and skin; three layers with core, muscles and skin; four layers with core, muscle, fat and skin). Each layer is interfaced with the adjacent one(s). Each individual thermal node (skin tissue, fat tissue, muscle tissue, bone) has different physical properties (e.g. thermal capacity, thermal conductivity, etc.) [62]. Most of the physical properties are obtained from measurements and physiological studies [63].
- The passive (or controlled) system is affected by the heat transfer phenomena that occur inside the human body, or between the human body and the external ambient. Heat transfer in the core occurs by conduction with the skin and two convection phenomena (one with the skin due to the blood-vessels convection (blood acts as a carrier) and another with the external environment due to the breathing). In the core, the heat is generated by the metabolism and muscle work [67]. At the surface of the body-environment interface the heat exchange occurs by evaporation, convection and radiation [72]. To simulate the heat transfer phenomena, key parameters are the thermal properties of the blood, muscle, fat and bones. In addition, external sources given by electromagnetic (EM) fields are considered (Section 3.3).
- The active (or controlling) system controls the passive system to regulate the temperature of the human body in steady-state and transient environments [75]. The active system considers the human body’s regulatory responses of vasodilatation, vasoconstriction, sweating and shivering. The objective is to provide thermoregulation by maintaining constant body core temperature. For this purpose, feedback signals are used to change the parameters of the passive system. The main feedback signal comes from the skin temperature. Further feedback signals come from the hypothalamic temperature variation, the skin temperature variation, and the basal evaporative heat loss from the skin [76]. Under stress conditions, the core temperature is particularly relevant in the case of hyperthermia, while the core and skin temperatures are relevant in case of hypothermia [77].
3.1.1. Two-Node Thermal Model
- SET predicts TS in conditions with high airflows [136]. According to the ASHRAE Standard 55-2017 [1], SET is defined as the air temperature of a standard environment at 50% relative humidity (RH) for individuals wearing clothing that would be standard for the given activity in the real environment. SET considers standard climate having uniform temperature , relative air velocity , metabolic heat rate , and clothing insulation .
- SET* is a temperature index for uniform thermal environments [137]. SET* is the air temperature of a hypothetical climate at uniform temperature and relative humidity , where the individuals have the same physiological strain (i.e., the same , and heat losses to the environment) as in the real environment [138]. The standard environment has , relative air velocity , metabolic heat rate , and clothing insulation .
3.1.2. Multi-Node and Multi-Segment Thermal Models
Other Multi-Node and Multi-Segment Models
Models for Patients, Children, Adults and the Elderly
3.1.3. Multi-Element and Multi-Segment Thermal Models
3.2. Considerations on the Human Clothing
3.2.1. Thermophysical Properties of Clothing
3.2.2. Human Clothing Models
3.3. Anatomical Models
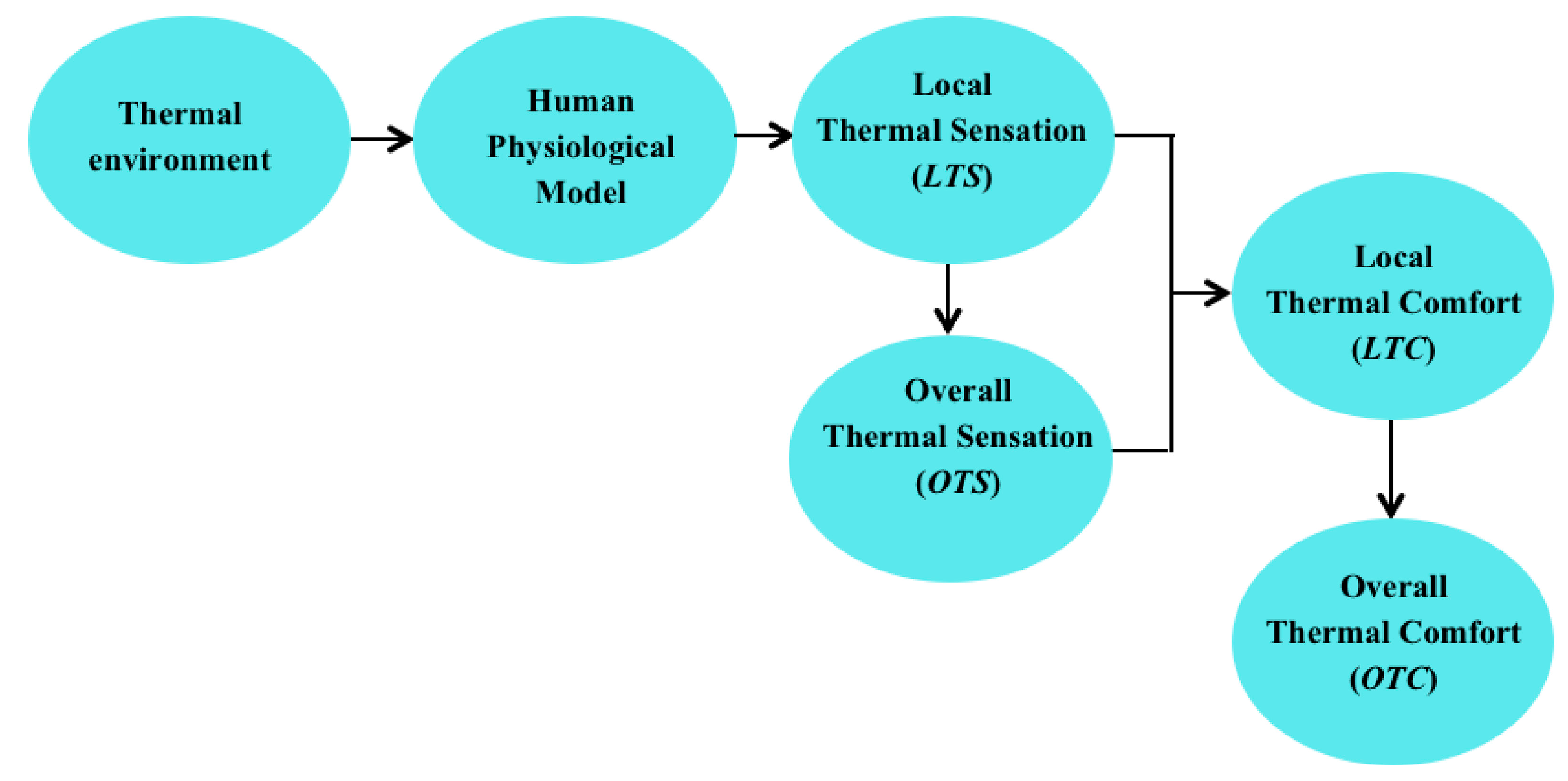
3.4. Models to Predict the Local and Overall Thermal Sensation
4. Conclusions
Funding
Acknowledgments
Conflicts of Interest
References
- Thermal Environmental Conditions for Human Occupancy; ANSI/ASHRAE Standard 55-2017; American Society of Heating, Refrigerating and Air-conditioning Engineering: Atlanta, GA, USA, 2017.
- Parsons, K. Measurement Methods and Assessment Techniques. In Human Thermal Environments—The Effects of Hot, Moderate, and Cold Environments on Human Health, Comfort, and Performance; CRC Press, Taylor & Francis Group: Boca Raton, FL, USA, 2002; Chapter 5; pp. 101–138. [Google Scholar]
- Fanger, P.O. Thermal Comfort: Analysis and Applications in Environmental Engineering; McGraw Hill Book Company: New York, NY, USA, 1970. [Google Scholar]
- IUPS Thermal Commission. Glossary of terms for thermal physiology. Third edition. Jpn. J. Physiol. 2001, 51, 245–280. [Google Scholar]
- Forgiarini Rupp, F.; Giraldo Vásquez, N.; Lamberts, R. A review of human thermal comfort in the built environment. Energy Build. 2015, 105, 178–205. [Google Scholar] [CrossRef]
- Nikolopoulou, M.; Steemers, K. Thermal comfort and psychological adaptation as a guide for designing urban spaces. Energy Build. 2003, 35, 95–101. [Google Scholar] [CrossRef]
- Yao, R.; Li, B.; Liu, J. A theoretical adaptive model of thermal comfort—Adaptive Predicted Mean Vote (aPMV). Build. Environ. 2009, 44, 2089–2096. [Google Scholar] [CrossRef]
- Gagge, A.P.; Stolwijk, J.A.J.; Nishi, Y. An effective temperature scale based on a simple model of human physiological regulatory response. ASHRAE Trans. 1971, 77, 247–262. [Google Scholar]
- D’Ambrosio Alfano, F.R.; Olesen, B.W.; Palella, B.I. Povl Ole Fanger’s Impact Ten Years Later. Energy Build. 2017, 152, 243–249. [Google Scholar] [CrossRef]
- International Organization for Standardization. Moderate Thermal Environments—Determination of the PMV and PPD Indices and Specification of the Conditions for Thermal Comfort, 1st ed.; Standard ISO 7730:1984; International Organization for Standardization: Geneva, Switzerland, 1984. [Google Scholar]
- De Dear, R.J.; Brager, G.S. Developing an adaptive model of thermal comfort and preference. ASHRAE Trans. 1998, 104, 145–167. [Google Scholar]
- American Society of Heating, Refrigerating and Air-conditioning Engineering. Thermal Environmental Conditions for Human Occupancy; ANSI/ASHRAE Standard 55-2004; American Society of Heating, Refrigerating and Air-conditioning Engineering: Atlanta, GA, USA, 2004. [Google Scholar]
- European Committee for Standardization. Indoor Environmental Input Parameters for Design and Assessment of Energy Performance of Buildings Addressing Indoor Air Quality, Thermal Environment, Lighting and Acoustics; Standard EN 15251:2007; European Committee for Standardization: Brussels, Belgium, 2007. [Google Scholar]
- Carlucci, S.; Bai, L.; de Dear, R.; Yang, L. Review of adaptive thermal comfort models in built environmental regulatory documents. Build. Environ. 2018, 137, 73–89. [Google Scholar] [CrossRef]
- Thermal Environmental Conditions for Human Occupancy; ANSI/ASHRAE, Standard 55-2013; American National Standards Institute, American Society of Heating, Refrigerating and Air-Conditioning Engineers: Atlanta, GA, USA, 2013.
- International Standardization Organization. Ergonomics of the Thermal Environment—Assessment of the Influence of the Thermal Environment Using Subjective Judgement Scales, 1st ed.; Standard ISO 10551-1995; International Standardization Organization: Geneva, Switzerland, 1995. [Google Scholar]
- Athienitis, A.K.; Santamouris, M. Thermal Analysis and Design of Passive Solar Buildings; Earthscan Publishing House: New York, NY, USA, 2013. [Google Scholar]
- Koelblen, B.; Psikuta, A.; Bogdan, A.; Annaheim, S.; Rossi, R.M. Thermal sensation models: A systematic comparison. Indoor Air 2017, 27, 680–689. [Google Scholar] [CrossRef] [PubMed]
- Takada, S.; Matsumoto, S.; Matsushita, T. Prediction of whole-body thermal sensation in the non-steady state based on skin temperature. Build. Environ. 2013, 68, 123–133. [Google Scholar] [CrossRef]
- Walgama, C.; Fackrell, S.; Karimi, M.; Fartaj, A.; Rankin, G.W. Passenger thermal comfort in vehicles—A review. Proc. Inst. Mech. Eng. Part D J. Automob. Eng. 2006, 220, 543–562. [Google Scholar] [CrossRef]
- Koelblen, B.; Psikuta, A.; Bogdan, A.; Annaheim, S.; Rossi, R.M. Thermal sensation models: Validation and sensitivity towards thermo-physiological parameters. Build. Environ. 2018, 130, 200–211. [Google Scholar] [CrossRef]
- Schlader, Z.J.; Stannard, S.R.; Mündel, T. Human thermoregulatory behavior during rest and exercise—A prospective review. Physiol. Behav. 2010, 99, 269–275. [Google Scholar] [CrossRef] [PubMed]
- Alahmer, A.; Mayyas, A.; Mayyas, A.A.; Omar, M.A.; Shan, D. Vehicular thermal comfort models; a comprehensive review. Appl. Therm. Eng. 2011, 31, 995–1002. [Google Scholar] [CrossRef]
- Cheng, Y.; Niu, J.; Gao, N. Thermal comfort models: A review and numerical investigation. Build. Environ. 2012, 47, 13–22. [Google Scholar] [CrossRef]
- Khodakarami, J.; Nasrollahi, N. Thermal comfort in hospitals—A literature review. Renew. Sustain. Energy Rev. 2012, 16, 4071–4077. [Google Scholar] [CrossRef]
- Katić, K.; Li, R.; Zeiler, W. Thermophysiological models and their applications: A review. Build. Environ. 2016, 106, 286–300. [Google Scholar] [CrossRef]
- Mishra, A.K.; Loomans, M.G.L.C.; Hensen, J.L.M. Thermal comfort of heterogeneous and dynamic indoor conditions—An overview. Build. Environ. 2016, 109, 82–100. [Google Scholar] [CrossRef]
- Schweiker, M.; Fuchs, X.; Becker, S.; Shukuya, M.; Dovjak, M.; Hawighorst, M.; Kolarik, J. Challenging the assumptions for thermal sensation scales. Build. Res. Inf. 2017, 45, 572–589. [Google Scholar] [CrossRef]
- Psikuta, A.; Allegrini, J.; Koelblen, B.; Bogdan, A.; Annaheim, S.; Martínez, N.; Derome, D.; Carmeliet, J.; Rossi, R.M. Thermal manikins controlled by human thermoregulation models for energy efficiency and thermal comfort research—A review. Renew. Sustain. Energy Rev. 2017, 78, 1315–1330. [Google Scholar] [CrossRef]
- Fang, Z.; Liu, H.; Li, B.; Tand, M.; Olaideea, O.M. Experimental Investigation on Thermal Comfort Model between Local Thermal Sensation and Overall Thermal Sensation. Energy Build. 2018, 158, 1286–1295. [Google Scholar] [CrossRef]
- International Standardization Organization. Ergonomics of the Thermal Environment—Vocabulary and Symbols, 1st ed.; Standard ISO 13731:2001; International Standardization Organization: Geneva, Switzerland, 2001. [Google Scholar]
- International Standardization Organization. Ergonomics of the Thermal Environment—Determination of Metabolic Rate, 2nd ed.; Standard ISO 8996:2004; International Standardization Organization: Geneva, Switzerland, 2004. [Google Scholar]
- Malchaire, J.; d’Ambrosio Alfano, F.R.; Palella, B.I. Evaluation of the metabolic rate based on the recording of the heart rate. Ind. Health 2017, 55, 219–232. [Google Scholar] [CrossRef] [PubMed]
- Hensen, J.L.M. Literature review on thermal comfort in transient conditions. Build. Environ. 1990, 25, 309–316. [Google Scholar] [CrossRef]
- ASHRAE. Thermal comfort. In ASHRAE Handbook Fundamentals; ASHRAE: Atlanta, GA, USA, 2017; Chapter 9. [Google Scholar]
- Gagge, A.P.; Stolwijk, J.A.J.; Hardy, J.D. Comfort and thermal sensations and associated physiological responses at various ambient temperatures. Environ. Res. 1967, 1, 1–20. [Google Scholar] [CrossRef]
- Gagge, A.P. A two node model of human temperature regulation in FORTRAN. In Bioastronautics Data, 2nd ed.; Parker, J.F., Jr., West, V.R., Eds.; NASA Special Publication: Washington, DC, USA, 1973; pp. 142–148. [Google Scholar]
- Rohles, F.H., Jr.; Nevins, R.G. The nature of thermal comfort for sedentary man. ASHRAE Trans. 1971, 77, 239. [Google Scholar]
- D’Ambrosio Alfano, F.R.; Palella, B.I.; Riccio, G. Thermal Environment Assessment Reliability Using Temperature-Humidity Indices. Ind. Health 2011, 49, 95–106. [Google Scholar] [CrossRef] [PubMed]
- De Freitas, C.R.; Grigorieva, E.A. A comprehensive catalogue and classification of human thermal climate indices. Int. J. Biometeorol. 2015, 59, 109–120. [Google Scholar] [CrossRef] [PubMed]
- Blazejczyk, K.; Epstein, Y.; Jendritzky, G.; Staiger, H.; Tinz, B. Comparison of UTCI to selected thermal indices. Int. J. Biometeorol. 2012, 56, 515–535. [Google Scholar] [CrossRef] [PubMed]
- International Standardization Organization. Ergonomics of the Thermal Environment—Analytical Determination and Interpretation of Heat Stress Using Calculation of the Predicted Heat Strain, 2nd ed.; Standard ISO 7933:2004; International Standardization Organization: Geneva, Switzerland, 2004. [Google Scholar]
- International Standardization Organization. Ergonomics of the Thermal Environment—Determination and Interpretation of Cold Stress When Using Required Clothing Insulation (IREQ) and Local Cooling Effects, 1st ed.; Standard ISO 11079:2007; International Standardization Organization: Geneva, Switzerland, 2007. [Google Scholar]
- International Organization for Standardization. Moderate Thermal Environments—Determination of the PMV and PPD Indices and Specification of the Conditions for Thermal Comfort, 3rd ed.; Standard ISO 7730:2005; International Organization for Standardization: Geneva, Switzerland, 2005. [Google Scholar]
- International Standardization Organization. Ergonomics of the Thermal Environment—Assessment of Heat Stress Using the WBGT (Wet Bulb Globe Temperature) Index, 3rd ed.; Standard ISO 7243:2017; International Standardization Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Höppe, P. Different aspects of assessing indoor and outdoor thermal comfort. Energy Build. 2002, 34, 661–665. [Google Scholar] [CrossRef]
- Thorsson, S.; Lindqvist, M.; Lindqvist, S. Thermal bioclimatic conditions and patterns of behaviour in an urban park in Göteborg, Sweden. Int. J. Biometeorol. 2004, 48, 149–156. [Google Scholar] [CrossRef] [PubMed]
- Macpherson, R.K. The assessment of the thermal environment—A review. Br. J. Ind. Med. 1962, 19, 151–164. [Google Scholar] [CrossRef] [PubMed]
- Zolfaghari, A.; Maerefat, M. A new simplified model for evaluating non-uniform thermal sensation caused by wearing clothing. Build. Environ. 2010, 45, 776–783. [Google Scholar] [CrossRef]
- Chen, K.; Jiao, Y.; Lee, E.S. Fuzzy adaptive networks in thermal comfort. Appl. Math. Lett. 2006, 19, 420–426. [Google Scholar] [CrossRef]
- Fanger, P.O. Calculation of thermal comfort: Introduction of a basic comfort equation. Build. Eng. 1967, 73, III.4.1–III.4.20. [Google Scholar]
- Prek, M. Thermodynamical analysis of human thermal comfort. Energy 2006, 31, 732–743. [Google Scholar] [CrossRef]
- Broday, E.E.; de Paula Xavier, A.A.; de Oliveira, R. Comparative analysis of methods for determining the clothing surface temperature (tcl) in order to provide a balance between man and the Environment. Int. J. Ind. Ergon. 2017, 57, 80–87. [Google Scholar] [CrossRef]
- Marn, J.; Chung, M.; Iljaž, J. Relationship between metabolic rate and blood perfusion under Fanger thermal comfort conditions. J. Therm. Biol. 2019, 80, 94–105. [Google Scholar] [CrossRef] [PubMed]
- International Standardization Organization. Energy Performance of Buildings—Indoor Environmental Quality—Part 1: Indoor Environmental Input Parameters for the Design and Assessment of Energy Performance of Building, 1st ed.; Standard ISO 17772-1; International Standardization Organization: Geneva, Switzerland, 2017. [Google Scholar]
- D’Ambrosio Alfano, F.R.; Palella, B.I.; Riccio, G.; Toftum, J. Fifty years of Fanger’s equation: Is there anything to discover yet? Int. J. Ind. Ergon. 2018, 66, 157–160. [Google Scholar] [CrossRef]
- Candas, V.; Dufour, A. Thermal comfort: Multisensory interactions? J. Appl. Hum. Sci. 2005, 24, 33–36. [Google Scholar] [CrossRef]
- Humphreys, M. Outdoor temperatures and comfort indoors. Batim. Int. Build. Res. Pract. 1978, 6, 92–105. [Google Scholar] [CrossRef]
- Van Marken Lichtenbelt, W.D.; Kingma, B.R. Building and occupant energetics: A physiological hypothesis. Archit. Sci. Rev. 2013, 56, 48–53. [Google Scholar] [CrossRef]
- Fanger, P.O. Thermal environment—Human requirements. Environ. Syst. Decis. 1986, 6, 275–278. [Google Scholar] [CrossRef]
- Fanger, P.O.; Toftum, J. Extension of the PMV model to non-air-conditioned buildings in warm climates. Energy Build. 2002, 34, 533–536. [Google Scholar] [CrossRef]
- De Dear, R.J.; Akimoto, T.; Arens, E.A.; Brager, G.; Candido, C.; Cheong, K.W.D.; Li, B.; Nishihara, N.; Sekhar, S.C.; Tanabe, S.; et al. Progress in thermal comfort research over the last twenty years. Indoor Air 2013, 23, 442–461. [Google Scholar] [CrossRef] [PubMed]
- Stolwijk, J.A.J. Mathematical Model of Thermoregulation, Physiological and Behavioural Temperature Regulation; C.C Thomas Publishers: Springfield, IL, USA, 1970; pp. 703–721. [Google Scholar]
- Arens, E.; Zhang, H. The skin’s role in human thermoregulation and comfort. In Thermal and Moisture Transport in Fibrous Materials; Woodhead Publ.: Cambridge, UK, 2006; Chapter 16; pp. 560–602. [Google Scholar]
- Schellen, L.; Loomans, M.G.L.C.; Kingma, B.R.M.; de Wit, M.H.; Frijns, A.J.H.; van Marken Lichtenbelt, W.D. The use of a thermophysiological model in the built environment to predict thermal sensation, coupling with the indoor environment and thermal sensation. Build. Environ. 2013, 59, 10–22. [Google Scholar] [CrossRef]
- Katić, K.; Zeiler, W.; Boxem, G. Thermophysiological models: A first comparison. In Proceedings of the 5th German-Austrian IBPSA Conference RWTH Aachen University, Aachen, Germany, 22–24 September 2014; pp. 525–602. [Google Scholar]
- Palella, B.I.; d’Ambrosio Alfano, F.R.; Riccio, G. On the Evolution of Thermoregulation Models. Ergon. Int. J. 2017, 1, 000118. [Google Scholar] [CrossRef]
- Yang, Y.; Yao, R.; Li, B.; Liu, H.; Jiang, L. A method of evaluating the accuracy of human body thermoregulation models. Build. Environ. 2015, 87, 1–9. [Google Scholar] [CrossRef]
- Hong, S.H.; Lee, J.M.; Moon, J.W.; Lee, K.H. Thermal Comfort, Energy and Cost Impacts of PMV Control Considering Individual Metabolic Rate Variations in Residential Building. Energies 2018, 11, 1767. [Google Scholar] [CrossRef]
- Stolwijk, J.A.J. A Mathematical Model of Physiological Temperature Regulation in Man; NASA Contractor Report, NASA CR-1855; NASA: Washington, DC, USA, August 1971.
- Fiala, D.; Lomas, K.J.; Stohrer, M. A computer model of human thermoregulation for a wide range of environmental conditions: The passive system. J. Appl. Physiol. 1999, 87, 1957–1972. [Google Scholar] [CrossRef] [PubMed]
- Candas, V.; d’Ambrosio, F.R.; Herrmann, C. A mathematical model of thermoregulation to evaluate thermal comfort. In Proceedings of the 2nd International Conference on Energy and Environment towards the Year 2000, Capri, Italy, 3–5 June 1993; pp. 1031–1043. [Google Scholar]
- Tanabe, S.; Kobayashi, K.; Nakano, J.; Ozeki, Y.; Konishi, M. Evaluation of thermal comfort using combined multi-node thermoregulation (65MN) and radiation models and computational fluid dynamics (CFD). Energy Build. 2002, 34, 637–646. [Google Scholar] [CrossRef]
- Kobayashi, Y.; Tanabe, S. Development of JOS-2 human thermoregulation model with detailed vascular system. Build. Environ. 2013, 66, 1–10. [Google Scholar] [CrossRef]
- Stolwijk, J.A.J.; Hardy, J.D. Temperature Regulation in Man—A Theoretical Study. Pflügers Archiv Die Gesamte Physiologie Des Menschen Und Der Tiere. 1966, 291, 129–162. [Google Scholar] [CrossRef]
- Bernardi, P.; Cavagnaro, M.; Pisa, S.; Piuzzi, E. Specific absorption rate and temperature elevation in a subject exposed in the far-field of radio-frequency sources operating in the 10-900-MHz range. Ieee Trans. Biomed. Eng. 2003, 50, 295–304. [Google Scholar] [CrossRef] [PubMed]
- Jendritzky, G.; de Dear, R. Adaptation and Thermal Environment. In Biometeorology for Adaptation to Climate Variability and Change; Ebi, K.L., Burton, I., McGregor, G., Eds.; Springer Science + Business Media B.V.: Berlin/Heidelberg, Germany, 2009; ISBN 978-1-4020-8920-6. [Google Scholar]
- Fu, G. A Transient 3-D Mathematical Thermal Model for the Clothed Human. Ph.D. Thesis, Kansas State University, Manhattan, KS, USA, 1995. [Google Scholar]
- Kuznetz, L.H. A two-dimensional transient mathematical model of human thermoregulation. Am. J. Physiol. 1979, 237, 266–277. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Li, F.; Liu, Y.; Luo, Z. An integrated model for simulating interactive thermal processes in the humane clothing system. J. Therm. Biol. 2004, 29, 567–575. [Google Scholar]
- Givoni, B.; Goldman, R. Predicting metabolic energy cost. J. Appl. Physiol. 1971, 30, 429–433. [Google Scholar] [CrossRef] [PubMed]
- Wyndham, C.H.; Atkins, A.R. A physiological scheme and mathematical model of temperature regulation in man. Pfulgers Arch. 1968, 303, 14–30. [Google Scholar] [CrossRef]
- Gagge, A.P. Rational temperature indices of man’s thermal environment and their use with a 2-node model of his temperature regulation. Federation Proc. 1973, 32, 1572–1582. [Google Scholar]
- Foda, E.; Sirén, K. A new approach using the Pierce two-node model for different body parts. Int. J. Biometeorol. 2011, 55, 519–532. [Google Scholar] [CrossRef] [PubMed]
- Salloum, M.; Ghaddar, N.; Ghali, K. A new transient bioheat model of the human body and its integration to clothing models. Int. J. Therm. Sci. 2007, 46, 371–384. [Google Scholar] [CrossRef]
- Höppe, P. The physiological equivalent temperature—A universal index for the biometeorogical assessment of the thermal environment. Int. J. Biometeorol. 1999, 43, 71–75. [Google Scholar] [PubMed]
- Azer, N.Z.; Hsu, S. The prediction of thermal sensation from a simple thermoregulatory model. ASHRAE Trans. 1977, 83, 88–102. [Google Scholar]
- Smith, C.E. A Transient Three-Dimensional Model of the Human Thermal System. Ph.D. Thesis, Kansas State University, Manhattan, KS, USA, 1991. [Google Scholar]
- Jones, B.W.; Ogawa, Y. Transient interaction between the human and the thermal environment. ASHRAE Trans. 1992, 98, 189–195. [Google Scholar]
- Crosbie, R.J.; Hardy, J.D.; Fessender, E. Electrical analog simulation of temperature regulation in man. Temp. Meas. Control Sci. Ind. 1963, 3, 627–635. [Google Scholar] [CrossRef]
- Munir, A.; Takada, S.; Matsushita, T. Re-evaluation of Stolwijk’s 25-node human thermal model under thermal-transient conditions: Prediction of skin temperature in low-activity conditions. Build. Environ. 2009, 44, 1777–1787. [Google Scholar] [CrossRef]
- Fiala, D.; Lomas, K.J.; Stohrer, M. Computer predictions of human thermoregulatory and temperature responses to a wide range of environment conditions. Int. J. Biometeorol. 2001, 45, 143–159. [Google Scholar] [CrossRef] [PubMed]
- Lai, D.; Chen, Q. A two-dimensional model for calculating heat transfer in the human body in a transient and non-uniform thermal environment. Energy Build. 2016, 118, 114–122. [Google Scholar] [CrossRef]
- Fiala, D.; Havenith, G.; Bröde, P.; Kampmann, B.; Jendritzky, G. UTCI–Fiala multi-node model of human heat transfer and temperature regulation. Int. J. Biometeorol. 2012, 56, 429–441. [Google Scholar] [CrossRef] [PubMed]
- Blazejczyk, K.; Bröde, P.; Fiala, D.; Havenith, G.; Holmér, I.; Jendritzky, G.; Kampmann, B.; Kunert, A. Principles of the new universal thermal climate index (UTCI) and its application to bioclimatic research in European scale. Misc. Geogr. 2010, 14, 91–102. [Google Scholar]
- Fiala, D.; Psikuta, A.; Jendritzky, G.; Paulke, S.; Nelson, D.A.; van Marken Lichtenbelt, W.D.; Frijns, A.J. Physiological modeling for technical, clinical and research applications. Front. Biosci. 2010, 2, 939–968. [Google Scholar] [CrossRef]
- Kingma, B.R.M. Human thermoregulation: A synergy between physiology and mathematical modelling. Ph.D. Thesis, Maastricht University, Maastricht, The Netherlands, 2012. [Google Scholar]
- Van Marken Lichtenbelt, W.D.; Frijns, A.J.H.; Fiala, D.; Janssen, F.E.M.; van Ooijen, A.M.J.; Van Steenhoven, A.A. Effect of individual characteristics on a mathematical model of human thermoregulation. J. Therm. Biol. 2004, 29, 577–581. [Google Scholar] [CrossRef]
- Van Marken Lichtenbelt, W.D.; Frijns, A.J.H.; van Ooijen, M.J.; Fiala, D.; Kester, A.M.; van Steenhoven, A.A. Validation of an individualised model of human thermoregulation for predicting responses to cold air. Int. J. Biometeorol. 2007, 51, 169–179. [Google Scholar] [CrossRef] [PubMed]
- Huizenga, C.; Zhang, H.; Arens, E. A model of human physiology and comfort for assessing complex thermal environments. Build. Environ. 2001, 36, 691–699. [Google Scholar] [CrossRef]
- Zhang, H.; Huizenga, C.; Arens, E.; Yu, T. Considering individual physiological differences in a human thermal model. J. Therm. Biol. 2001, 26, 401–408. [Google Scholar] [CrossRef]
- D’Ambrosio Alfano, F.R.; Palella, B.I.; Riccio, G. Thermode 193: An enhanced Stolwijk thermoregulation model of the human body. In Proceedings of the 7th International Thermal Manikin and Modelling Meeting, University of Coimbra, Coimbra, Portugal, 3–5 September 2008; pp. 1–8. [Google Scholar]
- Holopainen, R.A. Human Thermal Model for Improved Thermal Comfort. Ph.D. Thesis, Aalto University, Aalto, Findland, 2012. [Google Scholar]
- Holopainen, R.; Tuomaala, P. New human thermal model integrated in a building simulation environment for a more accurate estimation of thermal comfort in transient conditions. Chest 2010, 14, 29.7. [Google Scholar]
- Gardner, G.G.; Martin, C.J. The mathematical modelling of thermal responses of normal subjects and burned patients. Physiol. Meas. 1994, 15, 381–400. [Google Scholar] [CrossRef] [PubMed]
- Severens, N.M.W.; van Marken Lichtenbelt, W.D.; Frijns, A.J.H.; Van Steenhoven, A.A.; De Mol, B.A.J.M.; Sessler, D.I. A model to predict patient temperature during cardiac surgery. Phys. Med. Biol. 2007, 52, 5131–5145. [Google Scholar] [CrossRef] [PubMed]
- Pan, D.; Chan, M.; Deng, S.; Qu, M. A four-node thermoregulation model for predicting the thermal physiological responses of a sleeping person. Build. Environ. 2012, 52, 88–97. [Google Scholar]
- Xu, X.; Werner, J. A dynamic model of the human/clothing/environment-system. Appl. Hum. Sci. J. Physiol. Anthropol. 1997, 16, 61–75. [Google Scholar] [CrossRef]
- Ying, B.; Kwok, Y.; Li, Y.; Yeung, C.Y.; Li, F.Z.; Li, S. Mathematical modeling of thermal physiological responses of clothed infants. J. Therm. Biol. 2004, 29, 559–565. [Google Scholar] [CrossRef]
- Ying, B.; Kwok, Y.; Li, Y.; Li, F.; Yick, K.; Wong, K. An Improved Mathematical Model of Thermal Physiological Response of Naked Infants. J. Fiber Bioeng. Inform. 2009, 2, 90–100. [Google Scholar]
- Pereira, C.B.; Heimann, K.; Czaplik, M.; Blazek, V.; Venema, B.; Leonhardt, S. Thermoregulation in premature infants: A mathematical model. J. Therm. Biol. 2016, 62, 159–169. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.; Lian, Z.; Lan, L. An individualized human thermoregulation model for Chinese adults. Build. Environ. 2013, 70, 257–265. [Google Scholar] [CrossRef]
- Ma, T.; Xiong, J.; Lian, Z. A human thermoregulation model for the Chinese elderly. J. Therm. Biol. 2017, 70, 2–14. [Google Scholar] [CrossRef] [PubMed]
- Novieto, D.T. Adapting a Human Thermoregulation Model for Predicting the Thermal Response of Older Persons. Ph.D. Thesis, De Montfort University, Leicester, UK, 2013. [Google Scholar]
- Wissler, E.H. Steady-state temperature distribution in man. J. Appl. Physiol. 1961, 16, 734–740. [Google Scholar] [CrossRef] [PubMed]
- Wissler, E.H. Mathematical Simulation of Human Thermal Behaviour Using Whole-Body Models; Plenum Press: New York, NY, USA, 1985. [Google Scholar]
- Ferreira, M.S.; Yanagihara, J.I. A transient three-dimensional heat transfer model of the human body. Int. Commun. Heat Mass Transf. 2009, 36, 718–724. [Google Scholar] [CrossRef]
- Fanger, P.O. Thermal Comfort: Analysis and Applications in Engineering; McGraw-Hill: New York, NY, USA, 1982. [Google Scholar]
- Takada, S.; Kobayashi, H.; Matsushita, T. Thermal model of human body fitted with individual characteristics of body temperature regulation. Build. Environ. 2009, 44, 463–470. [Google Scholar] [CrossRef]
- Kingma, B.R.; Frijns, A.J.H.; Schellen, L.; van Marken Lichtenbelt, W.D. Beyond the classic thermoneutral zone, including thermal comfort. Temperature 2014, 1, 142–149. [Google Scholar] [CrossRef] [PubMed]
- Gagge, A.P.; Burton, A.C.; Bazeti, H.C. A practical system of units for the description of heat exchange in man with his thermal environment. Science 1941, 94, 428–430. [Google Scholar] [CrossRef] [PubMed]
- International Standardization Organization. Ergonomics of the Thermal Environment—Estimation of the Thermal Insulation and Evaporative Resistance of a Clothing Ensemble, Standard ISO 9920:2009 (ISO 9920:2007, corrected version 2008-11-01); International Standardization Organization: Geneva, Switzerland, 2009. [Google Scholar]
- Havenith, G.; Heus, R.; Lotens, W.A. Resultant clothing insulation: A function of body movement, posture, wind, clothing and ensemble thickness. Ergonomics 1990, 33, 67–84. [Google Scholar] [CrossRef]
- Havenith, G.; Heus, R.; Lotens, W.A. Clothing ventilation, vapour resistance and permeability index: Changes due to posture, movement and wind. Ergonomics 1990, 33, 989–1005. [Google Scholar] [CrossRef]
- Havenith, G.; Holmér, I.; den Hartog, E.A.; Parsons, K.C. Clothing evaporative heat resistance—Proposal for improved representation in standards and models. Ann. Occup. Hyg. 1999, 43, 339–346. [Google Scholar] [CrossRef]
- Havenith, G.; Nilsson, H.O. Correction of clothing insulation for movement and wind effects, a meta-analysis. Eur. J. Appl. Physiol. 2004, 92, 636–640. [Google Scholar] [CrossRef] [PubMed]
- Havenith, G.; Nilsson, H. Correction of clothing insulation for movement and wind effects, a meta-analysis (erratum). Eur. J. Appl. Physiol. 2005, 93, 506. [Google Scholar] [CrossRef]
- Lu, Y.; Wang, F.; Wan, X.; Song, G.; Shi, W.; Zhang, C. Clothing resultant thermal insulation determined on a movable thermal manikin. Part I: Effects of wind and body movement on total insulation. Int. J. Biometeorol. 2015, 59, 1475–1486. [Google Scholar] [CrossRef] [PubMed]
- D’Ambrosio Alfano, F.R.; Palella, B.I.; Riccio, G.; Malchaire, J. On the effect of thermophysical properties of clothing on the heat strain predicted by PHS model. Ann. Occup. Hyg. 2016, 60, 231–251. [Google Scholar] [CrossRef] [PubMed]
- Kaynakli, O.; Unver, U.; Kilic, M. Evaluating thermal environments for sitting and standing posture. Int. Commun. Heat. Mass Transf. 2003, 30, 1179–1188. [Google Scholar] [CrossRef]
- Kaynakli, O.; Kilic, M. Investigation of indoor thermal comfort under transient conditions. Build. Environ. 2005, 40, 9165–9174. [Google Scholar] [CrossRef]
- Kaynakli, O.; Pulat, E.; Kilic, M. Thermal comfort during heating and cooling in an automobile. Heat Mass Transf. 2005, 41, 449–458. [Google Scholar] [CrossRef]
- Kohri, I.; Mochida, T. Evaluation Method of Thermal Comfort in a vehicle with a Dispersed Two-Node Model, Part 1—Development of a Dispersed Two-Node Model. J. Hum. Environ. Syst. 2002, 6, 19–29. [Google Scholar] [CrossRef]
- Atmaca, I.; Kaynakli, O.; Yigit, A. Effects of radiant temperature on thermal comfort. Build. Environ. 2007, 42, 3210–3220. [Google Scholar] [CrossRef]
- ASHRAE. Thermal Environmental Conditions for Human Occupancy; ANSI/ASHRAE Standard 55-2010; American Society of Heating, Refrigerating and Air-Conditioning Engineers, Inc.: Atlanta, GA, USA, 2010. [Google Scholar]
- Zhu, Y.; Luo, M.; Ouyang, Q.; Huang, L.; Cao, B. Dynamic characteristics and comfort assessment of airflows in indoor environments: A review. Build. Environ. 2015, 91, 5–14. [Google Scholar] [CrossRef]
- Enescu, D. A review of thermal comfort models and indicators for indoor environments. Renew. Sustain. Energy Rev. 2017, 79, 1353–1379. [Google Scholar] [CrossRef]
- Monteiro, L.M. Review of numerical modelling of outdoor thermal comfort. In Proceedings of the World Sustainable Building Conference, Tokyo, Japan, 27–29 September 2005. [Google Scholar]
- Jones, B.W. Transient Model of the Human Body and Clothing Systems; Technical Report 91-01; Institute for Environmental Research, Kansas State University: Manhattan, KS, USA, 1991. [Google Scholar]
- Stolwijk, J.A.J.; Hardy, J.D. Partitional calorimetric studies of responses of man to thermal transients. J. Appl. Physiol. 1966, 21, 967–977. [Google Scholar] [CrossRef] [PubMed]
- Stolwijk, J.A.J.; Hardy, J.D. Control of body temperature. In Handbook of Physiology. Reactions to Environmental Agents; Lee, D.H.K., Falk, H.L., Murphy, S.D., Geiger, S.R., Eds.; Williams and Wilkins: Baltimore, MD, USA, 1977; Section 9; pp. 45–68. [Google Scholar]
- Li, F.; Li, Y. Effect of clothing material on thermal response of the human body. Model. Simul. Mater. Sci. Eng. 2005, 13, 809–827. [Google Scholar]
- Li, B.; Yang, Y.; Yao, R.; Liu, H.; Li, Y. A simplified thermoregulation model of the human body in warm conditions. Appl. Ergon. 2017, 59, 387–400. [Google Scholar] [CrossRef] [PubMed]
- Gordon, R.G.; Roemer, R.B.; Horvath, S.M. A mathematical model of the human temperature regulatory system-transient cold exposure response. IEEE Trans. Biomed. Eng. 1976, 23, 434–444. [Google Scholar] [CrossRef] [PubMed]
- Fiala, D. Dynamic Simulation of Human Heat Transfer and Thermal Comfort. Ph.D. Thesis, De Montfort University, Leicester, UK, 1998. [Google Scholar]
- Fiala, D.; Lomas, K.J.; Stohrer, M. First Principles Modelling of Thermal Sensation Responses in Steady State and Transient Conditions. ASHRAE Trans. 2003, 109, 179–186. [Google Scholar]
- Fiala, D.; Lomas, K.J. The dynamic effect of adaptive human responses in the sensation of thermal comfort. In Proceedings of the Moving Thermal Comfort Standards into the 21st Century, International Conference, Windsor, UK, 5–8 April 2001; pp. 147–157. [Google Scholar]
- Omori, T.; Yang, J.H.; Kato, K.; Murakami, S. Coupled Simulation of Convection and Radiation on Thermal Environment around an Accurately Shaped Human Body. In Proceedings of the 9th International Conference-RoomVent, Coimbra, Portugal, 5–8 September 2004; Volume 7. [Google Scholar]
- Yang, T.; Cropper, P.C.; Cook, M.J.; Yousaf, R.; Fiala, D. A new simulation system to predict human–environment thermal interactions in naturally ventilated buildings. In Proceedings of the 10th International Building Performance Simulation Association Conference and Exhibition (BS2007), Beijing, China, 3–6 September 2007; pp. 751–756. [Google Scholar]
- Van Treek, C.; Pfaffinger, C.M.; Wenisch, P.; Frisch, J.; Yue, Z.; Egger, M.; Rank, E. Towards computational steering of thermal comfort assessment. In Proceedings of the 11th International Conference on Indoor Air Quality and Climate, Copenhagen, Denmark, 17–22 August 2008; Volume 5. [Google Scholar]
- Van Treeck, C.; Frisch, J.; Pfaffinger, M.; Rank, E.; Paulke, S.; Schweinfurth, I.; Schwab, R.; Hellwig, R.; Holm, A. Integrated thermal comfort analysis using a parametric manikin model for interactive real-time simulation. J. Build. Perform. Simul. 2009, 2, 233–250. [Google Scholar] [CrossRef]
- Zare, S.; Hasheminejad, N.; Shirvan, H.E.; Hemmatjo, R.; Sarebanzadeh, K.; Saeid Ahmadi, S. Comparing Universal Thermal Climate Index (UTCI) with selected thermal indices/environmental parameters during 12 months of the year. Weather Clim. Extrem. 2018, 19, 49–57. [Google Scholar] [CrossRef]
- Kingma, B.; Schellen, L.; Frijns, A.; van Marken Lichtenbelt, W. Thermal sensation: A mathematical model based on neurophysiology. Indoor Air 2011, 22, 253–262. [Google Scholar] [CrossRef] [PubMed]
- Huizenga, C.; Zhang, H.; Arens, E.; Wang, D. Skin and core temperature response to partial and whole—Body heating and cooling. J. Therm. Biol. 2004, 29, 549–558. [Google Scholar] [CrossRef]
- Wyon, D.P.; Larsson, S.; Forsgren, B.; Lundgren, I. Standard Procedures for Assessing Vehicle Climate with a Thermal Manikin; SAE Paper 890049; SAE International: Warrendale, PA, USA, 1989. [Google Scholar]
- Tanabe, S.; Arens, E.; Bauman, F.; Zhang, H.; Madsen, T. Evaluating thermal environments by using a thermal manikin with controlled skin surface temperature. ASHRAE Trans. 1994, 100, 39–48. [Google Scholar]
- Nilsson, H.O. Thermal comfort evaluation with virtual thermal manikin methods. Build. Environ. 2007, 42, 4000–4005. [Google Scholar] [CrossRef]
- Foda, E.; Almesri, I.; Awbi, H.B.; Sirén, K. Models of human thermoregulation and the prediction of local and overall thermal sensations. Build. Environ. 2011, 46, 2023–2032. [Google Scholar] [CrossRef]
- Zhu, S.; Kato, S.; Ooka, R.; Sakoi, T. Development of a computational thermal manikin applicable in a nonuniform thermal environment—Part 1: Coupled Simulation of Convection, Radiation, and Smith’s Human Thermal Physiological Model for Sensible Heat Transfer from a Seated Human Body in Radiant Environment. HVAC R Res. 2007, 13, 661–679. [Google Scholar]
- Al-Othmani, M.; Ghaddar, N.; Ghali, K. A multi-segmented human bioheat model for transient and asymmetric radiative environments. Int. J. Heat Mass Transf. 2008, 51, 5522–5533. [Google Scholar] [CrossRef]
- Ozaki, H.; Enomoto-Kushimizu, H.; Tochihara, Y.; Nakamura, K. Thermal responses from repeated exposures to severe cold with intermittent warmer temperatures. Appl. Hum. Sci. 1998, 17, 195–205. [Google Scholar] [CrossRef]
- Kakitsuba, N. Dynamic changes in sweat rates and evaporation rates through clothing during hot exposure. J. Therm. Biol. 2004, 29, 739–742. [Google Scholar] [CrossRef]
- Bach, V.; Telliez, F.; Libert, J.P. The interaction between sleep and thermoregulation in adults and neonates. Physiol. Rev. 2002, 6, 481–492. [Google Scholar] [CrossRef]
- Dijk, D.J.; Duffy, J.F.; Czeisler, C.A. Contribution of circadian physiology and sleep homeostasis to age-related changes in human sleep. Chronobiol. Int. 2000, 17, 285–311. [Google Scholar] [CrossRef] [PubMed]
- Rida, M.; Ghaddar, N.; Ghali, K.; Hoballah, J. Elderly bioheat modeling: Changes in physiology, thermoregulation, and blood flow circulation. Int. J. Biometeorol. 2014, 58, 1825–1843. [Google Scholar] [CrossRef] [PubMed]
- Schellen, L.; van Marken Lichtenbelt, W.D.; Loomans, M.G.L.C.; Toftum, J.; De Wit, M.H. Differences between young adults and elderly in thermal comfort, productivity, and thermal physiology in response to a moderate temperature drift and a steady-state condition. Indoor Air 2010, 20, 273–283. [Google Scholar] [CrossRef] [PubMed]
- Havenith, G. Temperature regulation and technology. Gerontechnology 2001, 1, 41–49. [Google Scholar] [CrossRef]
- Van Hoof, J.; Hensen, J. Thermal comfort and older adults. Gerontechnology 2006, 4, 223–228. [Google Scholar]
- Van Hoof, J. Forty years of Fanger’s model of thermal comfort: Comfort for all? Indoor Air 2008, 18, 182–201. [Google Scholar] [CrossRef] [PubMed]
- Tsuzuki, K.; Ohfuku, T. Thermal sensation and thermoregulation in elderly compared to young people in Japanese winter season. In Proceedings of the 9th International Conference on Indoor Air Quality and Climate, Monterey, CA, USA, 30 June–5 July 2002; pp. 659–664. [Google Scholar]
- Tsuzuki, K.; Iwata, T. Thermal comfort and thermoregulation for elderly people taking light exercise. In Proceedings of the 9th International Conference on Indoor Air Quality and Climate, Monterey, CA, USA, 30 June–5 July 2002; pp. 647–652. [Google Scholar]
- Bussmann, O.; Nahm, W.; Konecny, E. A model for simulating heat transfer and thermoregulation of premature infants. Biomed. Tech. 1998, 43 (Suppl. S1), S300–S301. [Google Scholar]
- Werner, J.; Buse, M. Temperature profiles with respect to inhomogeneity and geometry of the human body. J. Appl. Physiol. 1988, 65, 1110–1118. [Google Scholar] [CrossRef] [PubMed]
- Karaki, W.; Ghaddar, N.; Ghali, K.; Kalev, K.; Holmer, I.; Vanggaard, L.L. Human thermal response with improved AVA modeling of the digits. Int. J. Therm. Sci. 2013, 67, 41–52. [Google Scholar] [CrossRef]
- Tang, Y.L.; He, Y.; Shao, H.W.; Ji, C.J. Assessment of comfortable clothing thermal resistance using a multi-scale human thermoregulatory model. Int. J. Heat Mass Transf. 2016, 98, 568–583. [Google Scholar] [CrossRef]
- Afzali, A.; Maghsoodlou, S. Heat and Moisture Transfer in Clothing System. In Nanostructured Polymer Blends and Composites in Textiles; Apple Academic Press: Oakville, ON, Canada, 2015; Chapter 5; pp. 187–215. [Google Scholar]
- Li, F.; Wang, Y.; Li, Y. A transient 3D thermal model for clothed human body considering more real geometry. J. Comput. 2013, 8, 676–684. [Google Scholar]
- Wissler, E.H. An analysis of factors affecting temperature levels in the nude human. Temp. Meas. Control Sci. Ind. 1963, 3, 603–612. [Google Scholar]
- Jones, B.W.; Ogawa, Y. Transient response of the human-clothing system. J. Therm. Biol. 1993, 18, 413–416. [Google Scholar] [CrossRef]
- Sun, X.Y.; Eckels, S.; Charlie Zheng, Z.Q. An improved thermal model of the human body. HVAC R Res. 2012, 18, 323–338. [Google Scholar]
- Zhang, H. Human Thermal Sensation and Comfort in Transient and Non-Uniform Thermal Environment. Ph.D. Thesis, University of California, Berkeley, CA, USA, 2003. [Google Scholar]
- Neves, S.F.; Campos, J.B.; Mayor, T.S. On the determination of parameters required for numerical studies of heat and mass transfer through textiles methodologies and experimental procedures. Int. J. Heat Mass Transf. 2015, 81, 272–282. [Google Scholar] [CrossRef]
- Woodcock, A.H. Moisture transfer in textile systems, Part 1. Text. Res. J. 1962, 32, 628–633. [Google Scholar] [CrossRef]
- Nilsson, H.O.; Anttonen, H.; Holmér, I. New algorithms for prediction of wind effects on cold protective clothing. In Proceedings of the Nokobetef 6 and 1st European Conference on Protective Clothing, Stockholm, Sweden, 7–10 May 2000; pp. 17–20. [Google Scholar]
- D’Ambrosio Alfano, F.R.; Palella, B.I.; Riccio, G. Notes on the Implementation of the IREQ Model for the Assessment of Extreme Cold Environments. Ergonomics 2013, 56, 707–724. [Google Scholar] [CrossRef] [PubMed]
- Havenith, G.; Holmer, I.; Parsons, K. Personal factors in thermal comfort assessment: Clothing properties and metabolic heat production. Energy Build. 2002, 34, 581–591. [Google Scholar] [CrossRef]
- Holmér, I.; Nilsson, H.; Havenith, G.; Parsons, K.C. Clothing Convective Heat Exchange—Proposal for improved Prediction in Standards and Models. Ann. Occup. Hyg. 1999, 43, 329–337. [Google Scholar] [CrossRef]
- Parsons, K.; Havenith, G.; Holmér, I.; Nilsson, H.; Malchaire, J.B. The Effects of Wind and Human Movement on the Heat and Vapour Transfer Properties of Clothing. Ann. Occup. Hyg. 1999, 43, 347–352. [Google Scholar] [CrossRef]
- Wang, F.; del Ferraro, S.; Lin, L.; Sotto Mayor, T.; Molinaro, V.; Ribeiro, M.; Gao, C.; Kuklane, K.; Holmér, I. Localised boundary air layer and clothing evaporative resistances for individual body segments. Ergonomics 2012, 55, 799–812. [Google Scholar] [CrossRef] [PubMed]
- Qian, X.; Fan, J. Prediction of Clothing Thermal Insulation and Moisture Vapour Resistance of the Clothed Body Walking in Wind. Ann. Occup. Hyg. 2006, 50, 833–842. [Google Scholar] [PubMed]
- Havenith, G.; Kuklane, K.; Fan, J.; Hodder, S.; Ouzzahra, Y.; Lundgren, K.; Au, Y.; Loveday, D. A database of static clothing thermal insulation and vapor permeability values of non-Western ensembles for use in ASHRAE Standard 55, ISO 7730, and ISO 9920. ASHRAE Trans. 2015, 121, 197–215. [Google Scholar]
- Lu, Y.; Wang, F.; Wan, X.; Song, G.; Zhang, C.; Shi, W. Clothing resultant thermal insulation determined on a movable thermal manikin. Part II: Effects of wind and body movement on local insulation. Int. J. Biometeorol. 2015, 59, 1487–1498. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Weng, W.; Wang, F.; Song, G. Integrating a human thermoregulatory model with a clothing model to predict core and skin temperatures. Appl. Ergon. 2017, 61, 168–177. [Google Scholar] [CrossRef] [PubMed]
- Fan, J.T.; Luo, Z.X.; Li, Y. Heat and moisture transfer with sorption and condensation in porous clothing assemblies and numerical simulation. Int. J. Heat Mass Transf. 2000, 43, 2989–3000. [Google Scholar] [CrossRef]
- Khatoon, S.; Kim, M.H. Human Thermal Comfort and Heat Removal Efficiency for Ventilation Variants in Passenger Cars. Energies 2017, 10, 1710. [Google Scholar] [CrossRef]
- Fan, J.T.; Cheng, X.; Wen, X.; Sun, W.W. An improved model of heat and moisture transfer with phase change and mobile condensates in fibrous insulation and comparison with experimental results. Int. J. Heat Mass Transf. 2004, 47, 2343–2352. [Google Scholar] [CrossRef]
- Zhu, Q.Y.; Xie, M.H.; Yang, J.; Li, Y. A fractal model for the coupled heat and mass transfer in porous fibrous media. Int. J. Heat Mass Transf. 2015, 54, 1400–1409. [Google Scholar] [CrossRef]
- Fan, J.; Wen, X. Modeling heat and moisture transfer through fibrous insulation with phase change and mobile condensates. Int. J. Heat Mass Transf. 2002, 45, 4045–4055. [Google Scholar] [CrossRef]
- Ghali, K.; Ghaddar, N.; Jones, B. Modeling of heat and moisture transport by periodic ventilation of thin cotton fibrous media. Int. J. Heat Mass Transf. 2002, 45, 3703–3714. [Google Scholar] [CrossRef]
- Lotens, W.A. Heat Transfer from Humans Wearing Clothing. Ph.D. Thesis, TU Delft, Delft University of Technology, Delft, The Netherlands, 1993. [Google Scholar]
- Lee, K.H.; Schiavon, S. Influence of Three Dynamic Predictive Clothing Insulation Models on Building Energy Use, HVAC Sizing and Thermal Comfort. Energies 2014, 7, 1917–1934. [Google Scholar] [CrossRef]
- Moore, S.M.; McIntosh, R.L.; Iskra, S.; Wood, A.W. Modeling the effect of adverse environmental conditions and clothing on temperature rise in a human body exposed to radio frequency electromagnetic fields. IEEE Trans. Biomed. Eng. 2015, 62, 627–637. [Google Scholar] [CrossRef] [PubMed]
- Wissler, E.H.; Havenith, G. A simple theoretical model of heat and moisture transport in multi-layer garments in cool ambient air. Eur. J. Appl. Physiol. 2009, 105, 797–808. [Google Scholar] [CrossRef] [PubMed]
- Wan, X.; Fan, J. A transient thermal model of the human body-clothing-environment system. J. Therm. Biol. 2008, 33, 87–97. [Google Scholar] [CrossRef]
- Hamdan, H.; Ghaddar, N.; Ouahrani, D.; Ghali, K.; Itani, M. PCM cooling vest for improving thermal comfort in a hot environment. Int. J. Therm. Sci. 2016, 102, 154–167. [Google Scholar] [CrossRef]
- Vecchia, P.; Matthes, R.; Ziegelberger, G.; Lin, J.; Saunders, R.; Swerdlow, A. Exposure to High Frequency Electromagnetic Fields, Biological Effects and Health Consequences (100 kHz-300 GHz); International Commission on Non-Ionizing Radiation Protection: Oberschleissheim, Germany, 2009. [Google Scholar]
- Gosselin, M.; Neufeld, E.; Moser, H.; Huber, E.; Farcito, S.; Gerber, L.; Jedensjö, M.; Hilber, I.; Di Gennaro, F.; Lloyd, B.; et al. Development of a new generation of high-resolution anatomical models for medical device evaluation: The Virtual Population 3.0. Phys. Med. Biol. 2014, 5287–5303. [Google Scholar] [CrossRef] [PubMed]
- Pisa, S.; Cavagnaro, M.; Piuzzi, E.; Bernardi, P.; Lin, J.C. Power density and temperature distributions produced by interstitial arrays of sleeved-slot antennas for hyperthermic cancer therapy. IEEE Trans. Microw. Theory Tech. 2003, 51, 2418–2426. [Google Scholar] [CrossRef]
- Ibrahiem, A.; Dale, C.; Tabbara, W.; Wiart, J. Analysis of the temperature increase linked to the power induced by RF source. Prog. Electromagn. Res. 2005, 52, 23–46. [Google Scholar] [CrossRef]
- Zhang, Y. Generalized dual-phase lag bioheat equations based on nonequilibrium heat transfer in living biological tissues. Int. J. Heat Mass Transf. 2009, 52, 4829–4834. [Google Scholar] [CrossRef]
- Liu, K.C.; Chen, T.M. Analysis of the thermal response and requirement for power dissipation in magnetic hyperthermia with the effect of blood temperature. Int. J. Heat Mass Transf. 2018, 126, 1048–1056. [Google Scholar] [CrossRef]
- Goyal, R.; Bhargava, R. FEM simulation of EM field effect on body tissues with bio-nanofluid (blood with nanoparticles) for nanoparticle mediated hyperthermia. Math. Biosci. 2018, 300, 76–86. [Google Scholar] [CrossRef] [PubMed]
- Nelson, D.A.; Curran, A.R.; Nyberg, H.A.; Marttila, E.A.; Mason, P.A.; Ziriax, J.M. High-resolution simulations of the thermophysiological effects of human exposure to 100 MHz RF energy. Phys. Med. Biol. 2013, 58, 1947–1968. [Google Scholar] [CrossRef] [PubMed]
- Hagino, M.; Hara, J. Development of a Method for Predicting Comfortable Airflow in the Passenger Compartment; Society of Automotive Engineers (SAE) Technical Paper Series; SAE: Warrendale, PA, USA, 1992; Volume 922131. [Google Scholar]
- Cheong, K.W.D.; Yu, W.J.; Sekhar, S.C.; Tham, K.W.; Kosonen, R. Local thermal sensation and comfort study in a field environment chamber served by displacement ventilation system in the tropics. Build. Environ. 2007, 42, 525–533. [Google Scholar] [CrossRef]
- Jin, Q.; Li, X.; Duanmu, L.; Shu, H.; Sun, Y.; Ding, Q. Predictive model of local and overall thermal sensations for non-uniform environments. Build. Environ. 2012, 51, 330–344. [Google Scholar] [CrossRef]
- He, Y.; Li, N.; Zhang, W.; Peng, J. Overall and local thermal sensation & comfort in air-conditioned dormitory with hot-humid climate. Build. Environ. 2016, 101, 102–109. [Google Scholar]
- Zhao, R.Y. Investigation of transient thermal environments. Build. Environ. 2007, 42, 3926–3932. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhao, R. Effect of local exposure on human responses. Build. Environ. 2007, 42, 2737–2745. [Google Scholar] [CrossRef]
- Cui, W.L.; Ouyang, Q.; Zhu, Y.X. Field study of thermal environment spatial distribution and passenger local thermal comfort in aircraft cabin. Build. Environ. 2014, 80, 213–220. [Google Scholar] [CrossRef]
- Duanmu, M.L. The Study on Thermal Environment and Comfort for Desktop Based Task—Ambient Air Conditioning. Ph.D. Thesis, Dalian University of Technology, Dalian, China, 2007. [Google Scholar]
- Zhang, H.; Arens, E.; Kim, D.; Buchberger, E.; Bauman, F.; Huizenga, C. Comfort, perceived air quality, and work performance in a low-power task-ambient conditioning system. Build. Environ. 2010, 45, 29–39. [Google Scholar] [CrossRef]
- Zhang, H.; Arens, E.; Huizenga, C.; Han, T. Thermal sensation and comfort models for non-uniform and transient environments: Part I: Local sensation of individual body parts. Build. Environ. 2010, 45, 380–388. [Google Scholar] [CrossRef]
- Zhang, H.; Arens, E.; Huizenga, C.; Han, T. Thermal sensation and comfort models for non-uniform and transient environments, part II: Local comfort of individual body parts. Build. Environ. 2010, 45, 389–398. [Google Scholar] [CrossRef]
- Zhang, H.; Arens, E.; Huizenga, C.; Han, T. Thermal sensation and comfort models for non-uniform and transient environments, part III: Whole-body sensation and comfort. Build. Environ. 2010, 45, 399–410. [Google Scholar] [CrossRef]
- Pokorny, J.; Jicha, M. Coupling of the Models of Human Physiology and Thermal Comfort. EPJ Web Conf. 2013, 45, 01077. [Google Scholar] [CrossRef]
- Streblow, R.; Müller, D.; Gores, I.; Bendfeldt, P. A Coupled Simulation of the Thermal Environment and Thermal Comfort with an Adapted Tanabe Comfort Model. In Proceedings of the 7th International Thermal Manikin and Modelling Meeting, University of Coimbra, Coimbra, Portugal, 3–5 September 2008. [Google Scholar]
- Schellen, L.; Loomans, M.G.L.C.; de Wit, M.H.; Olesen, B.W.; Lichtenbelt, W.D. The influence of local effects on thermal sensation under non-uniform environmental conditions—Gender differences in thermophysiology, thermal comfort and productivity during convective and radiant cooling. Physiol. Behav. J. 2012, 107, 252–261. [Google Scholar] [CrossRef] [PubMed]
- Arens, E.; Zhang, H.; Huizenga, C. Partial-and whole-body thermal sensation and comfort—Part I: Uniform environmental conditions. J. Therm. Biol. 2006, 31, 53–59. [Google Scholar] [CrossRef]
- Arens, E.; Zhang, H.; Huizenga, C. Partial-and whole-body thermal sensation and comfort—Part II: Non-uniform environmental conditions. J. Therm. Biol. 2006, 31, 60–66. [Google Scholar] [CrossRef]
- He, Y.; Li, N.; Huang, Q. A field study on thermal environment and occupant local thermal sensation in offices with cooling ceiling in Zhuhai China. Energy Build. 2015, 102, 277–283. [Google Scholar] [CrossRef]
- Choi, J.H.; Yeom, D. Investigation of the relationships between thermal sensations of local body areas and the whole body in an indoor built environment. Energy Build. 2017, 149, 204–215. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhao, R. Overall thermal sensation, acceptability and comfort. Build. Environ. 2008, 43, 44–50. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhao, R. Relationship between thermal sensation and comfort in nonuniform and dynamic environments. Build. Environ. 2009, 44, 1386–1391. [Google Scholar] [CrossRef]

| Indicator | TC | TS | TS | TS | TD |
|---|---|---|---|---|---|
| Scale | ISO 4-point * | ASHRAE 7-point | 9-point | 11-point | 11-point |
| +5 | -- | -- | -- | intolerably hot | intolerably warm discomfort |
| +4 | -- | -- | very hot | very hot | limited warm discomfort |
| +3 | -- | hot | hot | hot | very uncomfortable warm |
| +2 | comfortable | warm | warm | warm | uncomfortable and unpleasant warm |
| +1 | slightly comfortable | slightly warm | slightly warm | slightly warm | slightly uncomfortable but acceptable warm |
| 0 | -- | neutral | neutral | neutral | neutral |
| −1 | slightly uncomfortable | slightly cool | slightly cool | slightly cool | slightly uncomfortable but acceptable cold |
| −2 | uncomfortable | cool | cool | cool | uncomfortable and unpleasant cold |
| −3 | -- | cold | cold | cold | very uncomfortable cold |
| −4 | -- | -- | very cold | very cold | limited cold discomfort |
| −5 | -- | -- | -- | intolerably cold | intolerably cold discomfort |
| Review Paper Reference | Thermoregulatory Control | Applications | Thermal Manikins Model | Human Thermal Physiological Model | Human Thermal Psychological Model | Numerical Comparison with Different Tools |
|---|---|---|---|---|---|---|
| Walgama et al. [20] | - | vehicles | yes | yes | yes | - |
| Schlader et al. [22] | yes | during rest & exercise | - | - | - | - |
| Alahmer et al. [23] | - | vehicles | yes | yes | yes | - |
| Cheng et al. [24] | - | - | yes | yes | yes | CFD |
| Khodakarami and Nasrollahi [25] | - | hospitals | - | - | - | - |
| Katić et al. [26] | - | vehicles | - | yes | - | THESEUS-FE |
| Mishra et al. [27] | - | building | - | - | - | - |
| Schweiker et al. [28] | - | TS scales | - | - | - | - |
| Psikuta et al. [29] | yes | outdoor and building | controlled by models of human thermo- regulation | yes | - | CFD |
| Fang et al. [30] | - | calculation of LTS (head; upper and lower parts of the body) and OTS | - | - | - | - |
| Model | Number of Segments/Elements | Number of Nodes/Layers | Advantages | Limitations | Applicability Conditions to Predict Human Thermal Responses |
|---|---|---|---|---|---|
| One-node [81] | 1 | 1 | Introduces the equations of the metabolic costs of running, walking, and carrying loads [26] | Empirical model Limited applicability range Thermoregulatory system not considered | Hot environments Considers clothing |
| One-node [82] | 1 | 1/4 | Two controlling centres (for heat loss and energy stored in the body) [67] | Limited applicability range Differences among body parts not considered Effect of blood flow in the heat transfer within the tissue not considered [67] Big variation of the constants in the control equations [67] | Steady-state, uniform Considers clothing |
| Gagge/Pierce [8,36,83] | 1 | 2 | Good mean skin temperature estimation [84] Simple model and fast calculation time [84] Easy implementation [85] Introduces the SET* index [86] | Limited applicability range No local body zone output [24] Limited human exposure times (<1 h) [24] Does not explain spatial non-uniformities [24] No difference between the sensation of bare skin and clothed skin [49] | Transient, uniform Moderate activity Considers clothing |
| KSU [87,88] | 15 | 2 | Determines TS directly from physiological strain [24] | Limited applicability range Not applicable in cold or hot conditions [85] Heavy computational burden Skin and fat layers modelled as one layer Heat transfer of the blood flow in large arteries neglected [85] | Transient, non-uniform, non-symmetric Sedentary activity Considers clothing |
| Jones, Ogawa [89] | 1 | 2 | Wide applicability range The clothing model reflects non-uniformity User-friendly interface Fast determination of the skin moisture accumulation calculations | Constraints to human exposure times | Transient, non-uniform Various environments, activities and clothing types |
| MSP [84] | 24 | 2 | Accurate predictions of local skin temperatures of separate body parts with normal clothing | Limited applicability range Less accurate predictions at the limb in very cold environment | Steady-state, uniform Sedentary activities Considers clothing |
| Crosbie [90] | 1 | 3 | Accurate human temperature regulation predictions Accurate predictions of dynamic responses to unexpected changes | Limited applicability range | Steady-state and transient, uniform Clothing is not considered |
| Stolwijk [70] | 6 | 4 per segment | Accurate local skin temperature predictions [91] Gives the instantaneous temperature for all body segments [67] | Limited applicability range Less accurate predictions of body core temperature in the cold environment [92] No model of the flow in veins and individual arteries [85] Model based on limited data [93] | Transient, uniform Constant environment Clothing is not considered |
| Fiala thermoregulation [71,92] | 15 | 187 | Wide applicability range Accurate predictions of skin temperatures for cold, moderate and hot stress conditions Accurate predictions of body core temperature in the cold environment [92] | Less accurate predictions of skin temperatures during exercise in cold environments The model is implemented by a commercial software blind to users | Steady-state and transient, non-uniform Indoor and outdoor Different activity intensity [67] Considers clothing |
| Fiala UTCI [94] | 12 | 187 | Wide applicability range Accurate predictions of body thermal effects (hyperthermia and hypothermia) and local effects [92] | Time-consuming when real-time execution of the physiological model is needed [95] | Transient, non-uniform Outdoor applications including weather extremes [95,96] All scales from micro to macro, all climates and seasons [95] Whole-body and local skin cooling [77] Considers clothing |
| ThermoSEM [65,97] | 19 | Multi- node | Accurate predictions of metabolic responses to cold and mean skin temperature [98] More physiological background than in the regression model implemented in [92] | Limited applicability range The energy metabolism requires improvement in reply to mild cold [98] | Transient, close to neutral thermal environments [65] Mild cold environment [98,99] Different subpopulations (male, female) and individual characteristics (height, weight, and fat percentage) Considers clothing |
| UCB [100,101] | 16 | 5 | Flexibility of changing input data [20] Improvements over Stolwijk model [20] Fine segmentation for environments with local temperature variations Accurate predictions of OTS and LTS [17,20] | Extremely sensitive to the skin temperature set-point | Transient, non-uniform Considers clothing |
| 65MN [73] | 16 | 65 | Wide applicability range | Extremely sensitive to the skin temperature set-point on each segment | Steady-state and transient, non-uniform Considers clothing |
| JOS-2 [74] | 17 | Multi- node | Considers arterial and venous circulation (improves 65MN) [67] Accurate core and skin temperature predictions | Applicable to women and elderly | Transient, non-uniform Considers clothing |
| AUB [85] | 15 | 4 | Accurate and realistic representation of the arterial system including blood flow pulsation Accurate predictions of heat gains/losses Improved circulatory system model Solves the asymmetry and uses anatomic positions and real dimensions of arteries | Low time step size achieved for transient simulations | Transient, non-uniform Nude and clothed subjects |
| THERMODE 193 [72,102] | 48 | 193 | Good prediction of mean skin temperatures and their trends in comfort and moderated discomfort cases [72,102] Possibility of using different values of clothing insulation for each body segment | Limited prediction of temperature trend in cold conditions; limited predictions for hands and feet [72] (improvements made in [102]) | Steady-state and transient, non-uniform Considers clothing |
| HTM [103,104] | 16 plus head | 3200/4 | Accurate predictions of the effects on the occupants under different conditions More accurate predictions than in the Fanger model [3] | Limited applicability range | Steady-state and transient, non-uniform Indoor Considers clothing |
| 12-segment [93] | 12 | 1 node per layer / 4 or 5 layers per segment | Accurate skin and rectal temperature predictions | Limited applicability range | Transient, non-uniform Indoor Considers clothing |
| Burned Patients [105] | 11 | 4 per segment | Accurate environmental temperature predictions | Limited applicability range | Transient, non-uniform Ambient temperatures from 20 °C to 40 °C for burned patients Considers clothing |
| Patients during cardiac surgery [106] | 19 | Various tissue layers | Accurate core temperature distribution predictions Accurate predictions of heat losses in surgical interventions not experimentally evaluated in humans | Limited applicability range Uncertain initial boundary conditions lead to model sensitivity Less accurate predictions for the mean skin temperature | Transient, non-uniform Cardiac surgery patients Considers clothing |
| Three-Node [49] | 16 | 2 | Easy implementation due to simplifications Accurate predictions of TS of bare skin and clothed skin Introduces TS indices for bare skin, clothed skin and OTS of body | Clothing system simulated as an overall insulation covering the whole body | Transient, non-uniform Considers clothing |
| Sleeping person [107] | 1 | 4 | Acceptable accuracy to predict thermoregulatory responses Good prediction of indoor parameters (e.g., air temperature and humidity) in a sleeping environment | Limited applicability range | Transient, uniform Sleeping environments Young adults only Clothing is not considered |
| Human/clothing/environment [108] | 6 | 101 nodes per half- cylinder/4 layers per segment | Wide range of environmental conditions (heat, cold, and exercise) User-friendly interface Accurate predictions of human thermal response and clothing effects on humans | Time increment restricted by numerical stability | Steady-state and transient, non-uniform Considers clothing |
| Clothed Infants [109] | 4 | 7 | Accurate predictions of infants’ interaction with the thermoregulation system | Limited applicability range Environment temperature set to 35 °C Relative humidity set to 65% | Transient, non-uniform Clothed infants |
| Naked Infants [110] | 4 | 9 | Accurate core and skin temperature distribution predictions | Limited applicability range | Transient, non-uniform Naked infants |
| Premature Infants [111] | 7 | multi- node/ all segments contain multiple homogeneous layers | Accurate predictions of core and skin temperature distribution at thermal neutrality Accurate global and local physiological response predictions Accurate thermoregulatory dynamic response predictions | Limited applicability range | Transient, non-uniform, thermal neutrality Premature infants Clothing is not considered |
| Chinese adults [112] | 14 | Most segments have 4 layers with 3 sectors | Accurate predictions of mean and local skin temperature compared with the Fiala model Reduced standard deviation of predicted local skin temperatures compared to the standard Chinese model | Limited applicability range Skin surface area and body fat distribution different for Chinese adults and western people | Transient, asymmetrical Chinese young adults Considers clothing |
| Chinese elderly [113] | 14 | Most segments have 4 layers with 3 sectors | Accurate predictions of skin temperature due to the introduction of parameters like height, weight, sex and age [112] | Limited applicability range Modifications of passive and active systems Skin temperature differences between foot and thorax | Transient, asymmetrical Chinese elderly Considers clothing |
| Older Persons [114] | 15 | 187 | Accurate core temperature predictions | Limitations for the mean skin temperature | Steady-state and transient, non-uniform Older individuals Considers clothing |
| Wissler [115,116] | 6 elements (15 in the improved version) | About 5300 nodes | Accurate predictions of the human body’s response to the temperature changes [26] | Many equations needed to represent the temperature variation in space and the thermal flux in the boundaries | Steady-state and transient, non-uniform Cold and hot environments Hyperbaric and one-atmosphere environments Clothing is not considered |
| Ferreira and Yanagihara [117] | 15 | Multi-node/ 8 tissues | Satisfactory representation of the behaviour of the passive human thermal system | Require more segments to improve circulatory and thermoregulatory systems | Transient, uniform Clothing is not considered |
| Aspect | Characteristics | Young Adults | Aged Adults | Reference |
|---|---|---|---|---|
| Thermoregulation | Ability of the human body to regulate its own temperature | High | Low | [165] |
| Illnesses and disabilities | Increases with age | Low | High | [165] |
| Thermal environment | Extreme climate | TS depends on air temperature and skin temperature | TS depends on the air temperature | [166] |
| Physical strain low | - Physical strain high - Physiological modifications:
| [167] | ||
| Same climate (same clothing level) | - Low temperature preference due to high metabolism - High activity level | - High temperature preference due to low metabolism - Low activity level | [168] | |
| Neutral climate | TS of young is similar with TS of aged at specific temperature ranges (summer 24–28 °C, winter 22–25 °C) | [169] | ||
| Cold environment | (colder environment) | [170] | ||
| Hot environment | (warmer environment) | [171] | ||
© 2019 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Enescu, D. Models and Indicators to Assess Thermal Sensation Under Steady-State and Transient Conditions. Energies 2019, 12, 841. https://doi.org/10.3390/en12050841
Enescu D. Models and Indicators to Assess Thermal Sensation Under Steady-State and Transient Conditions. Energies. 2019; 12(5):841. https://doi.org/10.3390/en12050841
Chicago/Turabian StyleEnescu, Diana. 2019. "Models and Indicators to Assess Thermal Sensation Under Steady-State and Transient Conditions" Energies 12, no. 5: 841. https://doi.org/10.3390/en12050841
APA StyleEnescu, D. (2019). Models and Indicators to Assess Thermal Sensation Under Steady-State and Transient Conditions. Energies, 12(5), 841. https://doi.org/10.3390/en12050841





