Percutaneous Tracheostomy and Percutaneous Angiography: The Diuturnity of Sven-Ivar Seldinger of Mora, Pasquale Ciaglia of Utica
Abstract
:Percutaneous Angiography
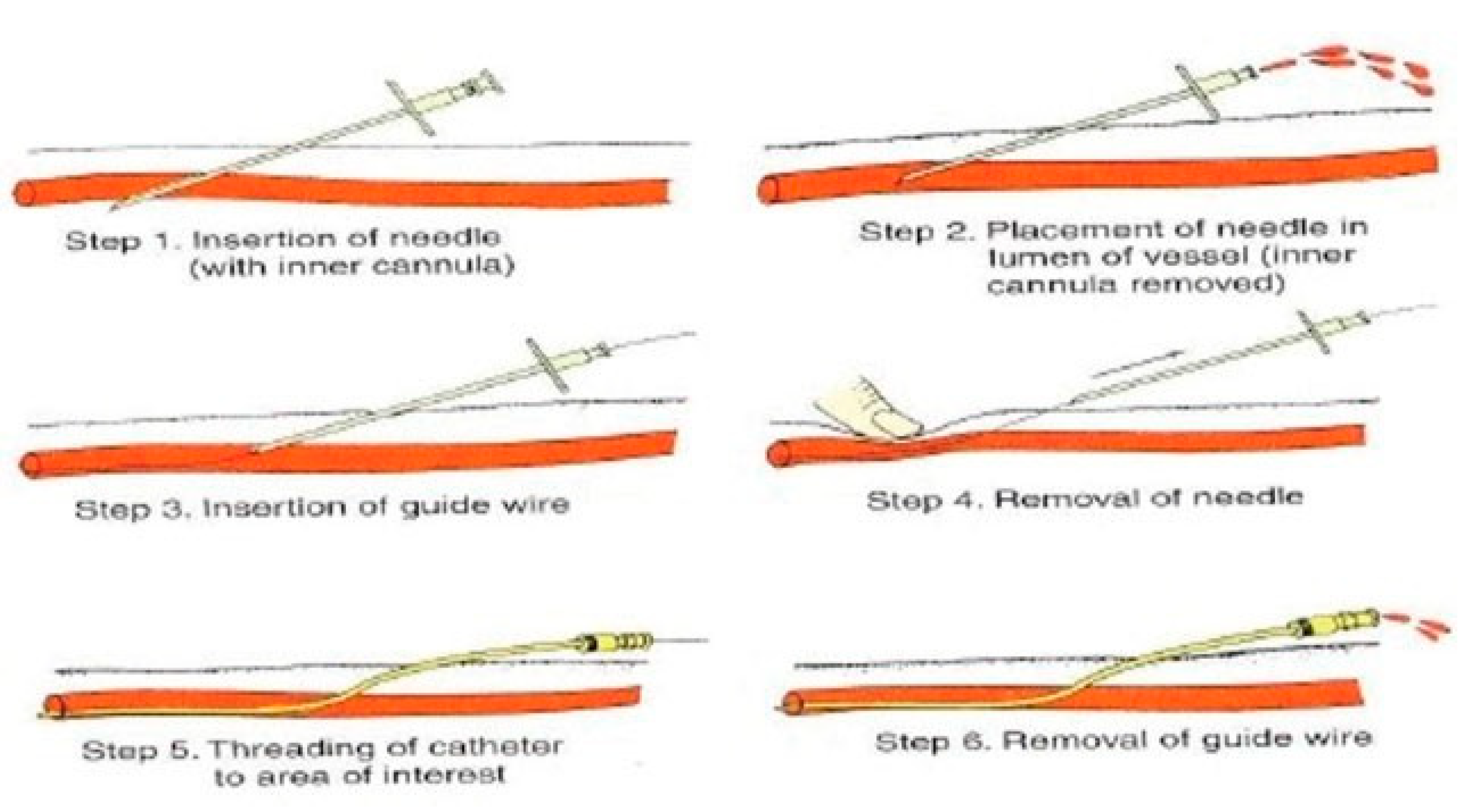
- To visualization of the temporal and aortic vessels, after direct needle stick and an injection of contrast (1931) [4]
- To proposals for catheterization of the right atrium, right ventricle, and pulmonary artery, based on the insights of Nobel Prize winners Werner Forssmann, Andre Cournand, and Dickinson Richards [7]
- To introduction of sheaths into the aorta, using a blunt silver thread as a guide (1949) [10]
- To direct injection of contrast material into the right and the left ventricles by percutaneous puncture (1951) [14]
- To percutaneous insertion of an inherently rigid nonradiopaque, polyethylene tube into the femoral artery, through a hollow needle (1951) [15]
Percutaneous Tracheostomy
Discussion
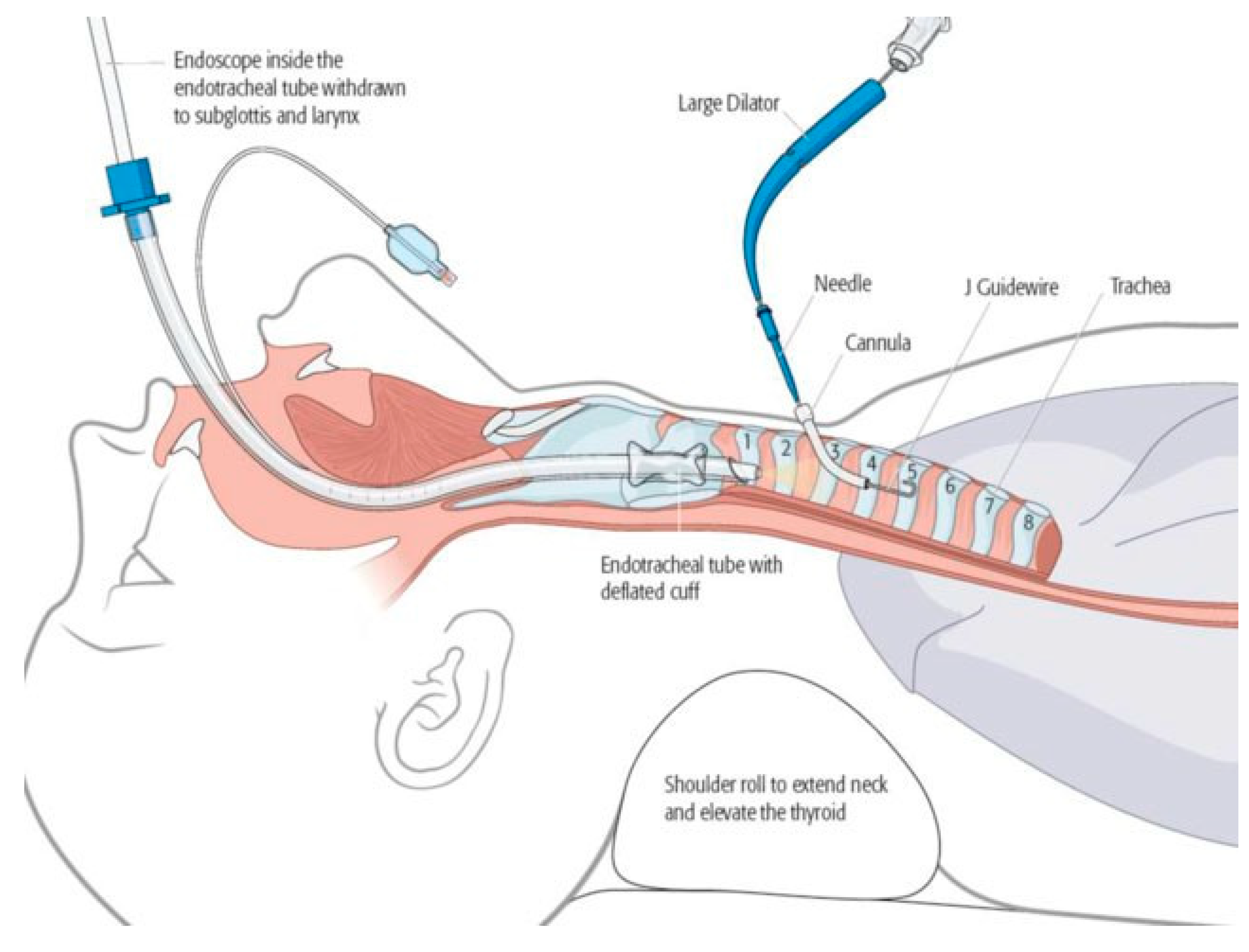
- Thoracic roll to extend the neck and elevate the thyroid gland
- Thorough local anesthetic with epinephrine infiltration of the subcutaneous and pretracheal soft tissue, with a 5- to 10-minute waiting period
- Preparation of skin with chlorhexidine (to avoid tracheal mucosal exposure to povidone)
- Use of a split-thyroid sheet to avoid encumbered access
- Surgical markings (thyroid notch, cricoid, midline, level of horizontal incision, suprasternal notch)
- Horizontal incision, with efficient dissection of the subcutaneous fat and Scarpa fascia
- Vertical dissection between the strap muscles and incision of the pretracheal fascia with needle electrocautery
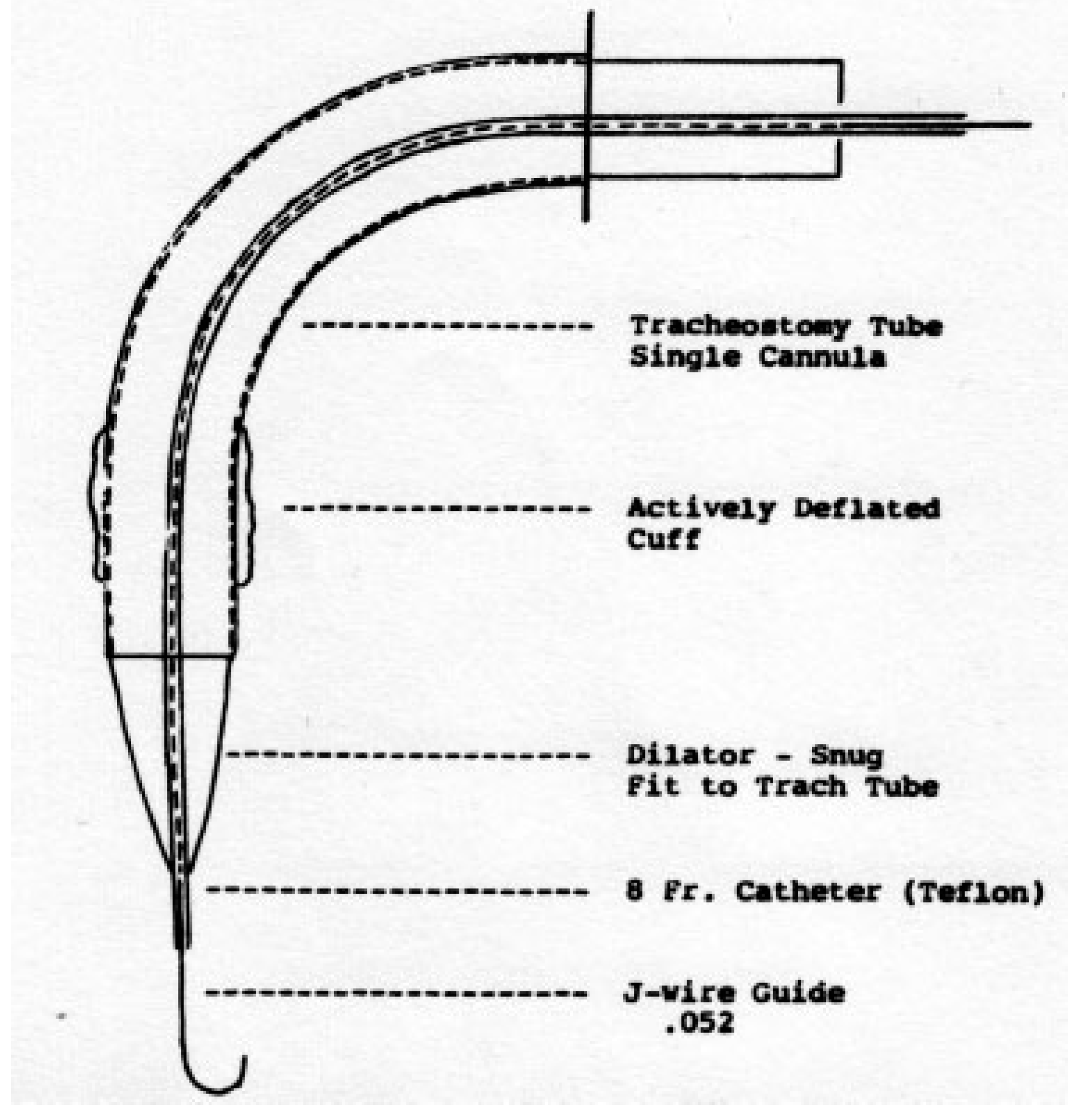
- The needle-and-cannula, after entering the trachea between the second and third “rings” or the third and fourth “rings,” is directed downwardly, toward the carina, to avoid the soft, membranous posterior wall of the trachea and the underlying anterior wall of the esophagus
- Dilators “expand” the inter-ring space, to favor untethered entry of the tracheostomy tube, into the trachea. Cartilage is neither incised nor excised; every effort is made to ensure it remains intact and is not fractured.
Acknowledgments
References
- Schon, L. An Economic History of Modern Sweden; Routledge: Abingdon, 2012. [Google Scholar]
- Doby, T. Development of Angiography and Cardiovascular Catheterization; John Wright: Littleton, CO, 1976. [Google Scholar]
- Doby, T. A tribute to Sven-Ivar Seldinger. AJR Am J Roentgenol 1984, 142, 1–4. [Google Scholar]
- Dos Santos, R.; Lamas, A.C.; Caldas, J.P. Arteriographie des Membres et de l’aorte Abdominale; Masson et Cie: Paris, 1931. [Google Scholar]
- Farinas, P.L. A new technique for the arteriographic examination if the abdominal aorta and its branches. AJR 1941, 46, 641–645. [Google Scholar]
- Farinas, P.L. Retrograde abdominal aortography; a contribution to the study of the abdominal aorta and iliac arteries. Radiology 1946, 47, 344–348. [Google Scholar] [CrossRef]
- Sourkes, T.L. Nobel Prize Winners in Medicine and Physiology; Abelard-Schuman: London, 1966; [Forrsmann, Cournand, and Richards won the Nobel Prize in 1956 for their work concerning ‘heart catheterization and pathological changes in the circulatory system.’]. [Google Scholar]
- Radner, S. Thoracic aortography by catheterization. Acta Radiol (Stockh) 1948, 29, 179–180. [Google Scholar]
- Freeman, N.E.; Miller, E.R. Retrograde arteriography in the diagnosis of cardiovascular lesions; visualization of aneurysms and peripheral arteries. Ann Intern Med 1949, 30, 330–342. [Google Scholar]
- Jonsson, G. Thoracic aortography by means of a cannula inserted percutaneously into the common carotid artery. Acta Radiol 1949, 31, 376–386. [Google Scholar] [CrossRef]
- Euler, H.E. Die peroesophagale Aortenpunktion. Arch Ohren Nassen Kehlk 1949, 155, 536–567. [Google Scholar] [CrossRef]
- Helmsworth, J.A.; McGuire, J.; Felson, B. Arteriography of the aorta and its branches by means of the polyethylene catheter. Am J Roentgenol Radium Ther 1950, 64, 196–213. [Google Scholar]
- Goodwin, W.E.; Scardino, P.L.; Scott, W.W. Translumbar aortic puncture and retrograde catheterization of the aorta in aortography and renal arteriography. Ann Surg 1950, 132, 944–958. [Google Scholar]
- Ponsdomenech, E.R.; Beato Nunez, V. Heart puncture in man for Diodrast visualization of the ventricular chambers and great arteries. Am Heart J 1951, 41, 643–650. [Google Scholar]
- Peirce, E.C., II. Percutaneous femoral artery catheterization in man with special reference to aortography. Surg Gynecol Obstet 1951, 93, 56–74. [Google Scholar]
- Seldinger, S.I. A leaf out of the history of angiography. In Pioneers in Angiography; Silvestre, M.E., Abecasis, F., Veiga-Pires, J.A., Eds.; Excerpta Medica (Elsevier): New York, 1987. [Google Scholar]
- Seldinger, S.I.; Edholm, P. Principles of percutaneous selective angiography. In Vascular Roentgenology; Schobinger, R.A., Ruzicka, F.F., Eds.; Macmillan: New York, 1964; pp. 41–45. [Google Scholar]
- Thomas, C.; O’Leary, J.P. Sven Ivar Seldinger. Am Surg 1996, 62, 783–784. [Google Scholar]
- Higgs, Z.C.; Macafee, D.A.; Braithwaite, B.D.; Maxwell-Armstrong, C.A. The Seldinger technique: 50 years on. Lancet 2005, 366, 1407–1409. [Google Scholar]
- Seldinger, S.I. Catheter replacement of the needle in percutaneous arteriography; a new technique. Acta Radiol 1953, 39, 368–376. [Google Scholar]
- Seldinger, S.I. Localization of parathyroid adenomata by arteriography. Acta Radiol 1954, 42, 353–366. [Google Scholar]
- Edholm, P.; Seldinger, S.I. Percutaneous catheterization of the renal artery. Acta Radiol 1956, 45, 15–20. [Google Scholar]
- Seldinger, S.I. Visualization of aortic and arterial occlusion by percutaneous puncture or catheterization of peripheral arteries. Angiology 1957, 8, 73–86. [Google Scholar]
- Seldinger, S.I. A simple method of catheterization of the spleen and liver. Acta Radiol 1957, 48, 93–96. [Google Scholar]
- Odman, P. Percutaneous selective angiography of the main branches of the aorta. Acta Radiol 1956, 45, 1–14. [Google Scholar]
- Cunningham, J.J.; Thurber, B. The abdominal aortogram: an historic perspective. Am J Roentgenol Radium Ther Nucl Med 1972, 116, 441–444. [Google Scholar]
- Flodmark, O.; Greitz, T. Obituary. Sven-Ivar Seldinger. Interv Neuroradiol 1999, 5, 9–10. [Google Scholar]
- Egidio Ciaglia Dies, Was Local Pharmacist; Utica Daily Press, 1966.
- Nates, J. Obitulogy: Pasquale Ciaglia, M.D., F.A.C.S. Internet J Emerg Intensive Care Med 2001, 52, 1–3, [written by Doctor Ciaglia; the date of death was postdated]. [Google Scholar]
- Clarke, T.W. Utica: For a Century and a Half, Widtman Press: Utica, 1952.
- Cardarelli, M.J. East Utica: Macchiata d’Amore; Ikon: Utica, NY, 2005. [Google Scholar]
- Bean, P.A. La Colonia: Italian Life and Politics in Utica, NY, 1860–1985; Syracuse University Press: Syracuse, NY, 2005. [Google Scholar]
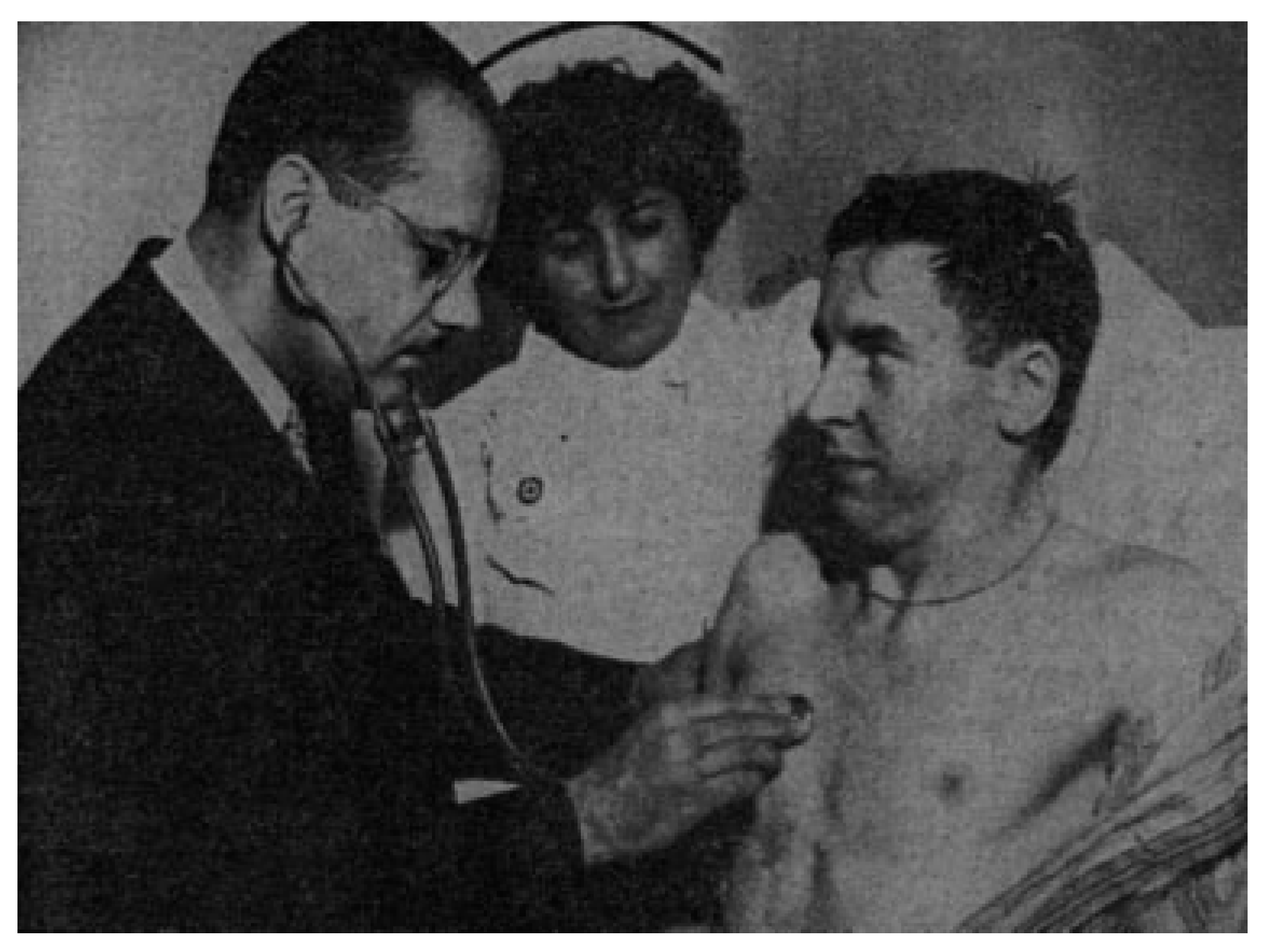
- Ciaglia, P.; Firshing, R.; Syniec, C. Elective percutaneous dilational tracheostomy, a new simple beside procedure: preliminary report. Chest 1985, 87, 815–819. [Google Scholar]
- Shelden, C.H.; Pudenz, R.H.; Freshwater, D.B.; Crue, B.L. A new method for tracheotomy. J Neurosurg 1955, 12, 428–431. [Google Scholar] [PubMed]
- Toy, F.J.; Weinstein, J.D. A percutaneous tracheostomy device. Surgery 1969, 65, 384–389. [Google Scholar]
- Smith, V.M. Perforation of trachea during tracheotomy performed with Sheldon tracheotome. J Am Med Assoc 1957, 165, 2074–2076. [Google Scholar]
- Byhahn, C.; Wilke, H.J.; Halbig, S.; Lischke, V.; Westphal, K. Percutaneous tracheostomy: Ciaglia blue rhino versus the basic Ciaglia technique of percutaneous dilational tracheostomy. Anesth Analg 2000, 91, 882–886. [Google Scholar]
- Bowen, C.P.; Whitney, L.R.; Truwit, J.D.; Durbin, C.G.; Moore, M.M. Comparison of safety and cost of percutaneous versus surgical tracheostomy. Am Surg 2001, 67, 54–60. [Google Scholar]
- Scultetus, J. Armamentarium Chirugicum; Kuhnen: Ulm, Germany, 1653. [Google Scholar]
- Trousseau, A. Memoire sur un cas de tracheotomie pratiquee dans la periode extreme de croup. J des Connaissance Medico-Chirurgicales. 1833, 1, 41. [Google Scholar]
- Browd, S.R.; MacDonald, J.D. Percutaneous dilational tracheostomy in neurosurgical patients. Neurocrit Care 2005, 2, 268–273. [Google Scholar]
- Pollock, R.A.; Dingman, R.O. Management and reconstruction of athletic injuries of the face, anterior neck and upper respiratory tract. In Sports Injuries: Mechanism, Prevention, and Treatment; Schneider, R.C., Kennedy, J.C., Plant, M., Fleming, W., Eds.; Williams & Wilkins Publishing Co: Baltimore, MD, 1985. [Google Scholar]
- Manson, P.N.; Clark, N.; Robertson, B.; Crawley, W.A. Comprehensive management of pan-facial fractures. J Craniomaxillofac Trauma 1995, 1, 43–56. [Google Scholar] [PubMed]
- Marcus, J.; Erdmann, D.; Rodriguez, E.D. Essentials of Craniomaxillofacial Trauma; Quality Medical: St. Louis, MO, 2012. [Google Scholar]
- Pollock, R.A. Craniomaxillofacial Buttresses: Anatomy and Operative Repair, Thieme Medical Publishing: New York, 2012.
- Pollock, R.A.; Purvis, J.M.; Apple DFJr Murray, H.H. Esophageal and hypopharyngeal injuries in patients with cervical spine trauma. Ann Otol Rhinol Laryngol 1981, 90 Pt 1, 323–327. [Google Scholar] [CrossRef] [PubMed]
- Yarmus, L.; Pandian, V.; Gilbert, C.; et al. Safety and efficiency of interventional pulmonologists performing percutaneous tracheostomy. Respiration 2012, 84, 123–127. [Google Scholar] [CrossRef] [PubMed]
- Patel, H.H.; Siltumens, A.; Bess, L.; Camacho, F.; Goldenberg, D. The decline of tracheotomy among otolaryngologists: a 14-year review. Otolaryngol Head Neck Surg 2015, 152, 465–469. [Google Scholar] [CrossRef]










© 2016 by the author. The Author(s) 2016.
Share and Cite
Pollock, R.A. Percutaneous Tracheostomy and Percutaneous Angiography: The Diuturnity of Sven-Ivar Seldinger of Mora, Pasquale Ciaglia of Utica. Craniomaxillofac. Trauma Reconstr. 2016, 9, 323-334. https://doi.org/10.1055/s-0036-1584526
Pollock RA. Percutaneous Tracheostomy and Percutaneous Angiography: The Diuturnity of Sven-Ivar Seldinger of Mora, Pasquale Ciaglia of Utica. Craniomaxillofacial Trauma & Reconstruction. 2016; 9(4):323-334. https://doi.org/10.1055/s-0036-1584526
Chicago/Turabian StylePollock, Richard A. 2016. "Percutaneous Tracheostomy and Percutaneous Angiography: The Diuturnity of Sven-Ivar Seldinger of Mora, Pasquale Ciaglia of Utica" Craniomaxillofacial Trauma & Reconstruction 9, no. 4: 323-334. https://doi.org/10.1055/s-0036-1584526
APA StylePollock, R. A. (2016). Percutaneous Tracheostomy and Percutaneous Angiography: The Diuturnity of Sven-Ivar Seldinger of Mora, Pasquale Ciaglia of Utica. Craniomaxillofacial Trauma & Reconstruction, 9(4), 323-334. https://doi.org/10.1055/s-0036-1584526


