Evaluation of the Mandibular Function, After Nonsurgical Treatment of Unilateral Subcondylar Fracture: A 1-Year Follow-Up Study
Abstract
:Methodology
Inclusion Criteria
- Subcondylar fracture of mandible less than 1 week old demonstrated on roentgenograms
- Malocclusion
- Reduced mouth opening
Exclusion Criteria
- Patients with history of any psychiatric disorders or mental retardation
- Patients who had mandibular function impairment or temporomandibular joint (TMJ) pain or pain in the muscles of mastication prior to fracturing the mandibular condyle
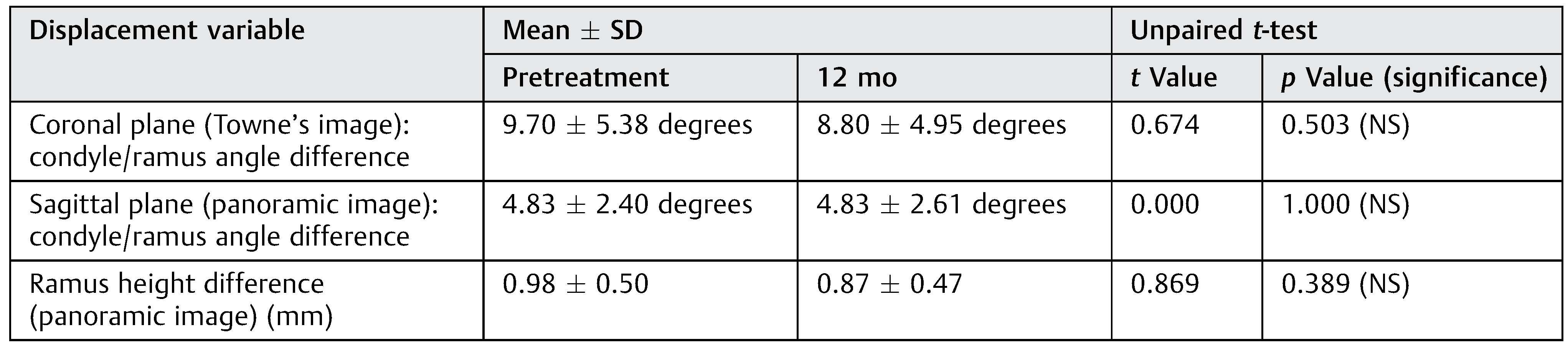
Radiographic Evaluation
- Good complement of teeth, especially posterior teeth must be present. Without them, there is a significant loss of posterior vertical dimension and an increase in the mandibular and occlusal plane angles.
- Cooperative patient who wear their elastics. Functional exercises should be done regularly and should be present for periodic follow-up.
- Surgeon should examine the patient on follow-up visits to assess treatment and alter functional therapy if necessary. Although closed techniques do not reduce subcondylar fractures, they do manage the occlusion, and most patients achieve satisfactory results [28]. In this study, all these criteria were met and closed treatment without a period of intermaxillary fixation (IMF) was chosen as the treatment option.
Conclusion
References
- Iida, S.; Kogo, M.; Sugiura, T.; Mima, T.; Matsuya, T. Retrospective analysis of 1502 patients with facial fractures. Int J Oral Maxillofac Surg 2001, 30, 286–290. [Google Scholar] [CrossRef]
- Maladière, E.; Bado, F.; Meningaud, J.P.; Guilbert, F.; Bertrand, J.C. Aetiology and incidence of facial fractures sustained during sports: A prospective study of 140 patients. Int J Oral Maxillofac Surg 2001, 30, 291–295. [Google Scholar] [CrossRef] [PubMed]
- Andersson, J.; Hallmer, F.; Eriksson, L. Unilateral mandibular condylar fractures: A 31-year follow-up of nonsurgical treatment. Int J Oral Maxillofac Surg 2007, 36, 310–314. [Google Scholar] [CrossRef]
- Jensen, T.; Jensen, J.; Nørholt, S.E.; Dahl, M.; Lenk-Hansen, L.; Svensson, P. Open reduction and rigid internal fixation of mandibular condylar fractures by an intraoral approach: A long-term follow-up study of 15 patients. J Oral Maxillofac Surg 2006, 64, 1771–1779. [Google Scholar] [CrossRef] [PubMed]
- van Beek, G.J.; Merkx, C.A. Changes in the pattern of fractures of the maxillofacial skeleton. Int J Oral Maxillofac Surg 1999, 28, 424–428. [Google Scholar] [CrossRef]
- Zachariades, N.; Mezitis, M.; Mourouzis, C.; Papadakis, D.; Spanou, A. Fractures of the mandibular condyle: A review of 466 cases. Literature review, reflections on treatment and proposals. J Craniomaxillofac Surg 2006, 34, 421–432. [Google Scholar] [CrossRef] [PubMed]
- Landes, C.A.; Day, K.; Lipphardt, R.; Sader, R. Closed versus open operative treatment of nondisplaced diacapitular (Class VI) fractures. J Oral Maxillofac Surg 2008, 66, 1586–1594. [Google Scholar] [CrossRef]
- Ellis, E.I.I.I.; Throckmorton, G.S. Treatment of mandibular condylar process fractures: Biological considerations. J Oral Maxillofac Surg 2005, 63, 115–134. [Google Scholar] [CrossRef]
- Haug, R.H.; Brandt, M.T. Closed reduction, open reduction, and endoscopic assistance: Current thoughts on the management of mandibular condyle fractures. Plast Reconstr Surg 2007, 120 (Suppl. 2), 90s–102s. [Google Scholar] [CrossRef]
- Troulis, M.J.; Kaban, L.B. Endoscopic approach to the ramus/condyle unit: Clinical applications. J Oral Maxillofac Surg 2001, 59, 503–509. [Google Scholar] [CrossRef]
- Zide, M.F.; Kent, J.N. Indications for open reduction of mandibular condyle fractures. J Oral Maxillofac Surg 1983, 41, 89–98. [Google Scholar] [CrossRef]
- Goss, A.N.; Bosanquet, A.G. The arthroscopic appearance of acute temporomandibular joint trauma. J Oral Maxillofac Surg 1990, 48, 780–783, discussion 784. [Google Scholar] [CrossRef]
- Wood, G.D. Assessment of function following fracture of the mandible. Br Dent J 1980, 149, 137–141. [Google Scholar] [CrossRef] [PubMed]
- Dijkstra, P.U.; Kropmans, T.J.; Stegenga, B.; de Bont, L.G. Ratio between vertical and horizontal mandibular range of motion. J Oral Rehabil 1998, 25, 353–357. [Google Scholar] [CrossRef]
- Jensen, M.P.; Chen, C.; Brugger, A.M. Interpretation of visual analog scale ratings and change scores: A reanalysis of two clinical trials of postoperative pain. J Pain 2003, 4, 407–414. [Google Scholar] [CrossRef]
- Niezen, E.T.; Bos, R.R.M.; de Bont, L.G.M.; Stegenga, B.; Dijkstra, P.U. Complaints related to mandibular function impairment after closed treatment of fractures of the mandibular condyle. Int J Oral Maxillofac Surg 2010, 39, 660–665. [Google Scholar] [CrossRef] [PubMed]
- Palmieri, C.; Ellis, E.I.I.I.; Throckmorton, G. Mandibular motion after closed and open treatment of unilateral mandibular condylar process fractures. J Oral Maxillofac Surg 1999, 57, 764–775, discussion 775–776. [Google Scholar] [CrossRef]
- Santler, G.; Kärcher, H.; Ruda, C.; Köle, E. Fractures of the condylar process: Surgical versus nonsurgical treatment. J Oral Maxillofac Surg 1999, 57, 392–397, discussion 397–398. [Google Scholar] [CrossRef] [PubMed]
- MacLennan, W.D. Fractures of the mandibular condylar process. Br J Oral Surg 1969, 7, 31–39. [Google Scholar] [CrossRef]
- Newman, L. A clinical evaluation of the long-term outcome of patients treated for bilateral fracture of the mandibular condyles. Br J Oral Maxillofac Surg 1998, 36, 176–179. [Google Scholar] [CrossRef]
- Smets, L.M.; Van Damme, P.A.; Stoelinga, P.J. Nonsurgical treatment of condylar fractures in adults: A retrospective analysis. J Craniomaxillofac Surg 2003, 31, 162–167. [Google Scholar] [CrossRef] [PubMed]
- Silvennoinen, U.; Iizuka, T.; Oikarinen, K.; Lindqvist, C. Analysis of possible factors leading to problems after nonsurgical treatment of condylar fractures. J Oral Maxillofac Surg 1994, 52, 793–799. [Google Scholar] [CrossRef] [PubMed]
- Eckelt, U.; Schneider, M.; Erasmus, F.; et al. Open versus closed treatment of fractures of the mandibular condylar process-a prospective randomized multi-centre study. J Craniomaxillofac Surg 2006, 34, 306–314. [Google Scholar] [CrossRef] [PubMed]
- Takenoshita, Y.; Ishibashi, H.; Oka, M. Comparison of functional recovery after nonsurgical and surgical treatment of condylar fractures. J Oral Maxillofac Surg 1990, 48, 1191–1195. [Google Scholar] [CrossRef] [PubMed]
- Oezmen, Y.; Mischkowski, R.A.; Lenzen, J.; Fischbach, R. MRI examination of the TMJ and functional results after conservative and surgical treatment of mandibular condyle fractures. Int J Oral Maxillofac Surg 1998, 27, 33–37. [Google Scholar] [CrossRef]
- Worsaae, N.; Thorn, J.J. Surgical versus nonsurgical treatment of unilateral dislocated low subcondylar fractures: A clinical study of 52 cases. J Oral Maxillofac Surg 1994, 52, 353–360, discussion 360–361. [Google Scholar] [CrossRef]
- Walker, R.V. Condylar fractures: Nonsurgical management. J Oral Maxillofac Surg 1994, 52, 1185–1188. [Google Scholar] [CrossRef]
- Ellis, E.I.I.I.; Kellman, R.M.; Vural, E. Subcondylar fractures. Facial Plast Surg Clin North Am 2012, 20, 365–382. [Google Scholar] [CrossRef]

 |
 |
 |
 |
 |
© 2016 by the author. The Author(s) 2016.
Share and Cite
K. M., S.; Desai, R.; K. S. N., S.B.; S., S. Evaluation of the Mandibular Function, After Nonsurgical Treatment of Unilateral Subcondylar Fracture: A 1-Year Follow-Up Study. Craniomaxillofac. Trauma Reconstr. 2016, 9, 229-234. https://doi.org/10.1055/s-0036-1584399
K. M. S, Desai R, K. S. N. SB, S. S. Evaluation of the Mandibular Function, After Nonsurgical Treatment of Unilateral Subcondylar Fracture: A 1-Year Follow-Up Study. Craniomaxillofacial Trauma & Reconstruction. 2016; 9(3):229-234. https://doi.org/10.1055/s-0036-1584399
Chicago/Turabian StyleK. M., Sudheesh, Rajendra Desai, Siva Bharani K. S. N., and Subhalakshmi S. 2016. "Evaluation of the Mandibular Function, After Nonsurgical Treatment of Unilateral Subcondylar Fracture: A 1-Year Follow-Up Study" Craniomaxillofacial Trauma & Reconstruction 9, no. 3: 229-234. https://doi.org/10.1055/s-0036-1584399
APA StyleK. M., S., Desai, R., K. S. N., S. B., & S., S. (2016). Evaluation of the Mandibular Function, After Nonsurgical Treatment of Unilateral Subcondylar Fracture: A 1-Year Follow-Up Study. Craniomaxillofacial Trauma & Reconstruction, 9(3), 229-234. https://doi.org/10.1055/s-0036-1584399



