Correlation of Third Molar Status with Incidence of Condylar and Angle Fractures
Abstract
:Materials and Method
Study Design and Sample
Statistical Analysis
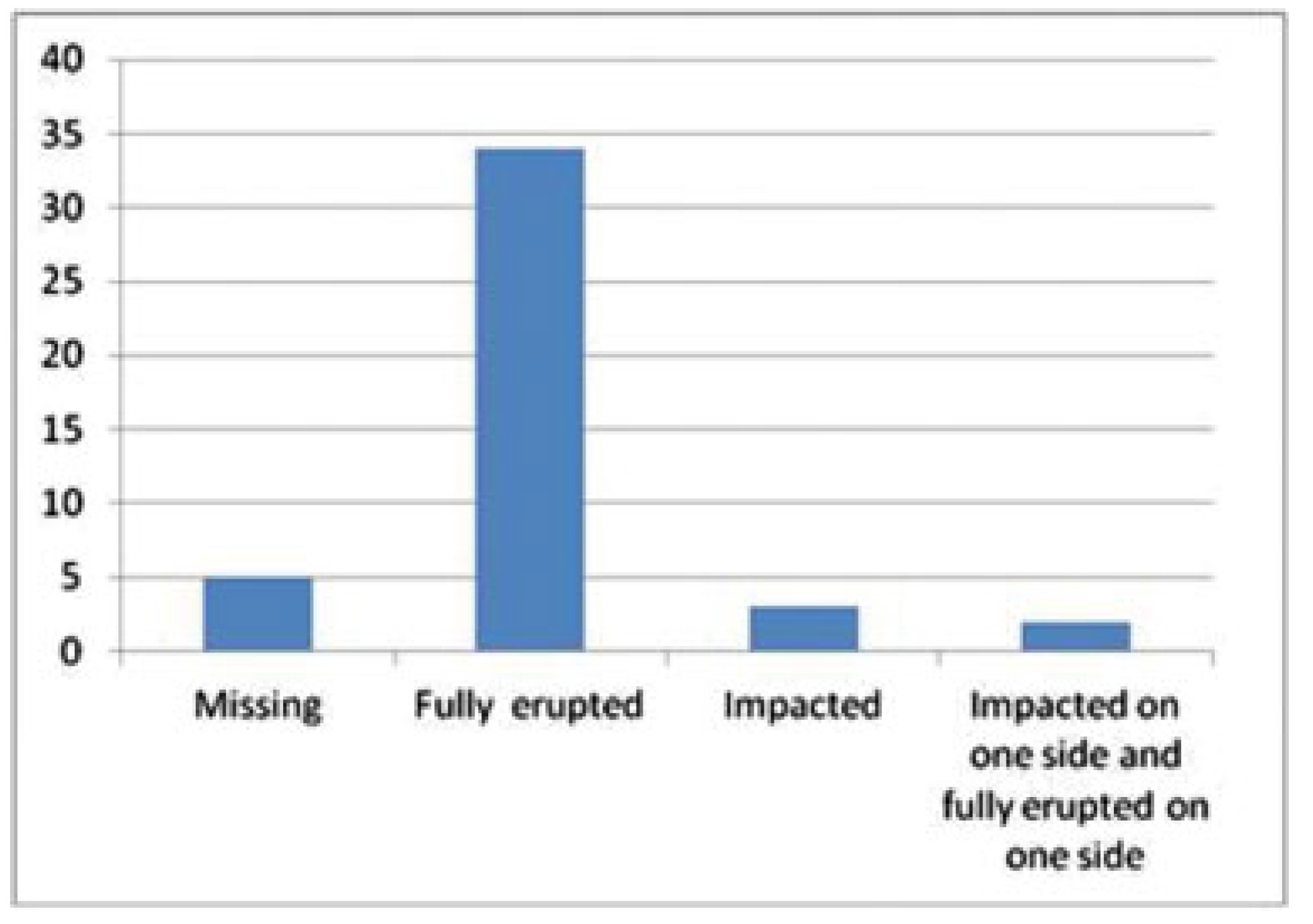
Results
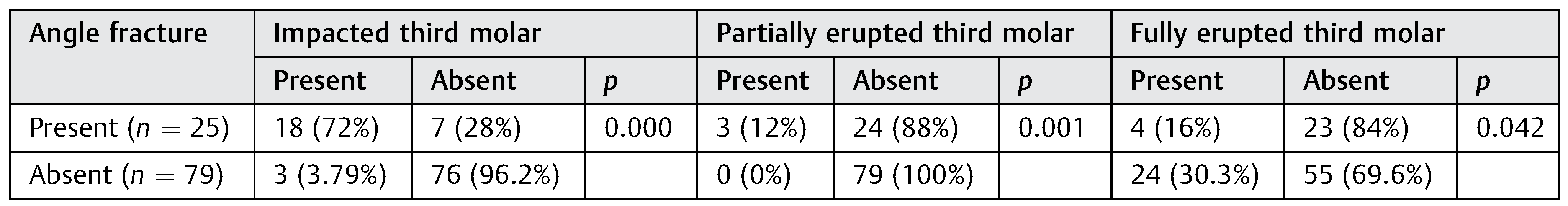
Angle Fracture
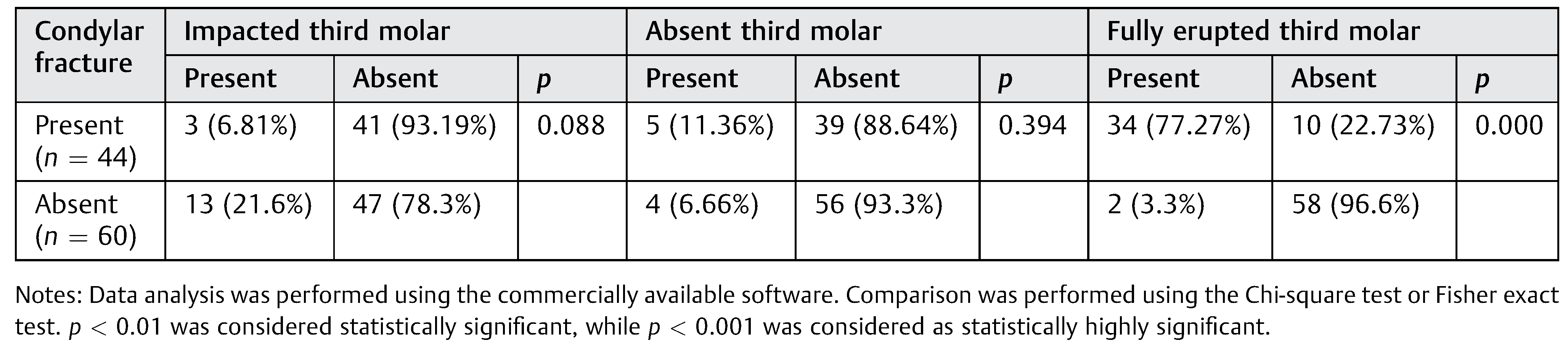
Condylar Fracture
Discussion
Conclusion
References
- Ellis, E.I.I.I.; Moos, K.F.; el-Attar, A. Ten years of mandibular fractures: an analysis of 2,137 cases. Oral Surg Oral Med Oral Pathol 1985, 59, 120–129. [Google Scholar] [CrossRef]
- Schubert, W.; Kobienia, B.J.; Pollock, R.A. Cross-sectional area of the mandible. Discussion J Oral Maxillofac Surg 1997, 55, 689–692, discussion 693. [Google Scholar] [CrossRef]
- Halazonetis, J.A. The ‘weak’ regions of the mandible. Br J Oral Surg 1968, 6, 37–48. [Google Scholar] [CrossRef] [PubMed]
- Moore, J.R. Principles of Oral Surgery, 2nd ed; Manchester: Manchester University Press, 1976. [Google Scholar]
- Tams, J.; van Loon, J.P.; Rozema, F.R.; Otten, E.; Bos, R.R. A threedimensional study of loads across the fracture for different fracture sites of the mandible. Br J Oral Maxillofac Surg 1996, 34, 400–405. [Google Scholar] [CrossRef]
- Meisami, T.; Sojat, A.; Sàndor, G.K.; Lawrence, H.P.; Clokie, C.M. Impacted third molars and risk of angle fracture. Int J Oral Maxillofac Surg 2002, 31, 140–144. [Google Scholar] [CrossRef] [PubMed]
- Bezerra, T.P.; Silva Junior, F.I.; Scarparo, H.C.; Costa, F.W.; Studart-Soares, E.C. Do erupted third molars weaken the mandibular angle after trauma to the chin region? A 3D finite element study. Int J Oral Maxillofac Surg 2013, 42, 474–480. [Google Scholar] [CrossRef]
- Huelke, D.F.; Harger, J.H. Maxillofacial injuries: their nature and mechanisms of production. J Oral Surg 1969, 27, 451–460. [Google Scholar] [PubMed]
- Szucs, A.; Bujtár, P.; Sándor, G.K.; Barabás, J. Finite element analysis of the human mandible to assess the effect of removing an impacted third molar. J Can Dent Assoc 2010, 76, a72. [Google Scholar]
- Wolujewicz, M.A. Fractures of the mandible involving impacted 3rd molar tooth: an analysis of 47 cases. Br J Surg 1980, 18, 125–131. [Google Scholar]
- Tevepaugh, D.B.; Dodson, T.B. Are mandibular third molars a risk factor for angle fractures? A retrospective cohort study. J Oral Maxillofac Surg 1995, 53, 646–649, discussion 649–650. [Google Scholar] [CrossRef]
- Safdar, N.; Meechan, J.G. Relationship between fractures of the mandibular angle and the presence and state of eruption of the lower third molar. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1995, 79, 680–684. [Google Scholar] [CrossRef] [PubMed]
- Tankersly, K.; Abubaker, A.O.; Laskin, D.M. The relationship between presence of mandibular third molars and mandibular angle fractures. J Dent Res 1995, 74, 80. [Google Scholar]
- Iida, S.; Hassfeld, S.; Reuther, T.; Nomura, K.; Mühling, J. Relationship between the risk of mandibular angle fractures and the status of incompletely erupted mandibular third molars. J Craniomaxillofac Surg 2005, 33, 158–163. [Google Scholar] [CrossRef]
- Ugboko, V.I.; Oginni, F.O.; Owotade, F.J. An investigation into the relationship between mandibular third molars and angle fractures in Nigerians. Br J Oral Maxillofac Surg 2000, 38, 427–429. [Google Scholar] [CrossRef]
- Ellis, E., III. A prospective study of 3 treatment methods for isolated fractures of the mandibular angle. J Oral Maxillofac Surg 2010, 68, 2743–2754. [Google Scholar] [CrossRef]
- Halmos, D.R.; Ellis, E.I.I.I.; Dodson, T.B. Mandibular third molars and angle fractures. J Oral Maxillofac Surg 2004, 62, 1076–1081. [Google Scholar] [CrossRef]
- Tevepaugh, D.B.; Dodson, T.B. Are mandibular third molars a risk factor for angle fractures? A retrospective cohort study. J Oral Maxillofac Surg 1995, 53, 646–649, discussion 649–650. [Google Scholar] [CrossRef] [PubMed]
- Reitzik, M.; Lownie, J.F.; Cleaton-Jones, P.; Austin, J. Experimental fractures of monkey mandibles. Int J Oral Surg 1978, 7, 100–103. [Google Scholar] [CrossRef]
- Fuselier, J.C.; Ellis, E.E.I.I.I.; Dodson, T.B. Do mandibular third molars alter the risk of angle fracture? J Oral Maxillofac Surg 2002, 60, 514–518. [Google Scholar] [CrossRef]
- Subhashraj, K. A study on the impact of mandibular third molars on angle fractures. J Oral Maxillofac Surg 2009, 67, 968–972. [Google Scholar] [CrossRef]
- Ma’aita, J.; Alwrikat, A. Is the mandibular third molar a risk factor for mandibular angle fracture? Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000, 89, 143–146. [Google Scholar] [CrossRef] [PubMed]
- Amaratunga, N.A. A comparative study of the clinical aspects of edentulous and dentulous mandibular fractures. J Oral Maxillofac Surg 1988, 46, 3–5. [Google Scholar] [CrossRef]
- Lee, J.T.; Dodson, T.B. The effect of mandibular third molar presence and position on the risk of an angle fracture. J Oral Maxillofac Surg 2000, 58, 394–398, discussion 399. [Google Scholar] [CrossRef]
- Choi, B.J.; Park, S.; Lee, D.W.; Ohe, J.Y.; Kwon, Y.D. Effect of lower third molars on the incidence of mandibular angle and condylar fractures. J Craniofac Surg 2011, 22, 1521–1525. [Google Scholar] [CrossRef]
- Inaoka, S.D.; Carneiro, S.C.; Vasconcelos, B.C.; Leal, J.; Porto, G.G. Relationship between mandibular fracture and impacted lower third molar. Med Oral Patol Oral Cir Bucal 2009, 14, E349–E354. [Google Scholar]
- Duan, D.H.; Zhang, Y. Does the presence of mandibular third molars increase the risk of angle fracture and simultaneously decrease the risk of condylar fracture? Int J Oral Maxillofac Surg 2008, 37, 25–28. [Google Scholar] [CrossRef]
- Iida, S.; Nomura, K.; Okura, M.; Kogo, M. Influence of the incompletely erupted lower third molar on mandibular angle and condylar fractures. J Trauma 2004, 57, 613–617. [Google Scholar] [CrossRef]
- Zhu, S.J.; Choi, B.H.; Kim, H.J.; et al. Relationship between the presence of unerupted mandibular third molars and fractures of the mandibular condyle. Int J Oral Maxillofac Surg 2005, 34, 382–385. [Google Scholar] [CrossRef]
- Thangavelu, A.; Yoganandha, R.; Vaidhyanathan, A. Impact of impacted mandibular third molars in mandibular angle and condylar fractures. Int J Oral Maxillofac Surg 2010, 39, 136–139. [Google Scholar] [CrossRef]
- Patil, P.M. Unerupted lower third molars and their influence on fractures of the mandibular angle and condyle. Br J Oral Maxillofac Surg 2012, 50, 443–446. [Google Scholar] [CrossRef]
- Schwimmer, A.; Stern, R.; Kritchman, D. Impacted third molars: a contributing factor in mandibular fractures in contact sports. Am J Sports Med 1983, 11, 262–266. [Google Scholar] [CrossRef] [PubMed]


 |
 |
© 2016 by the author. The Author(s) 2016.
Share and Cite
Menon, S.; Kumar, V.; V., S.; Priyadarshini, Y. Correlation of Third Molar Status with Incidence of Condylar and Angle Fractures. Craniomaxillofac. Trauma Reconstr. 2016, 9, 224-228. https://doi.org/10.1055/s-0036-1584400
Menon S, Kumar V, V. S, Priyadarshini Y. Correlation of Third Molar Status with Incidence of Condylar and Angle Fractures. Craniomaxillofacial Trauma & Reconstruction. 2016; 9(3):224-228. https://doi.org/10.1055/s-0036-1584400
Chicago/Turabian StyleMenon, Suresh, Veerendra Kumar, Srihari V., and Yogitha Priyadarshini. 2016. "Correlation of Third Molar Status with Incidence of Condylar and Angle Fractures" Craniomaxillofacial Trauma & Reconstruction 9, no. 3: 224-228. https://doi.org/10.1055/s-0036-1584400
APA StyleMenon, S., Kumar, V., V., S., & Priyadarshini, Y. (2016). Correlation of Third Molar Status with Incidence of Condylar and Angle Fractures. Craniomaxillofacial Trauma & Reconstruction, 9(3), 224-228. https://doi.org/10.1055/s-0036-1584400



