Abstract
Intracranial hemorrhage (ICH) is a potentially fatal injury accompanying fractures of the cranium and facial skeleton. When occurring at a young age, ICH can lead to developmental delay, cerebral palsy, epilepsy, and death. It is therefore important for clinicians to recognize the presence of ICH early, and understand the factors that affect its prognosis. In this study, we aim to identify diagnostic and prognostic signs for ICH in pediatric facial fracture patients by examining aspects of patient presentation, concomitant injuries, and fracture patterns. Data were collected for all radiologically diagnosed facial fractures between January 2000 and December 2012 at a level I trauma center in Newark, NJ. This was then further refined to include only patients 18 years of age or younger who had a documented ICH. Patient age, Glasgow coma scale (GCS) on presentation, fracture location, type of hemorrhage, and certain aspects of management were collected from these records. Data were then analyzed by either Pearson chi-square test or a t-test to determine significant relationships. A total of 285 pediatric patients were found to have sustained a facial fracture during this time period, 67 of which had concomitant ICH; 46 of these patients were male and 21 were female, with average ages of 14.26 and 9.52 (p < 0.01), respectively. Causes of injury included motor vehicle accidents, pedestrians struck, assault, falls, gunshot injuries, and sports-related injuries. All patients who suffered injuries as a result of violent crimes (assault and gunshot injuries) were male. Although nearly all fracture patterns were significantly associated with the presence of ICH, mandibular fractures showed a significant negative association with the presence of ICH. In addition, patients who received surgical intervention were significantly younger than those who did not (7.7 vs. 13.7, p < 0.05). The GCS was significantly lower in patients who underwent ICP (intracranial pressure) monitoring or EVD (external ventricular drain) placement, suffered intraventricular hemorrhage, experienced worsening of hemorrhage on repeat imaging, and suffered fatal injuries. Our data also showed a significant association between the need for intubation in the emergency department and fatality. Because the consequence of ICH can be life threatening, proper diagnosis and management are imperative. The purpose of this study is to describe patterns associated with ICH in pediatric facial fracture patients to promote early recognition of the injury and understanding of poor prognostic signs.
Despite advancements in child safety, trauma remains the leading cause of pediatric mortality in the United States [1], and an estimated 11.3% of pediatric emergency room visits are from craniofacial injuries [2]. The increased incidence of pediatric craniofacial injuries relative to adults reflects the activities in which children engage and is likely exacerbated by the relatively high cranial mass-to-body mass ratio [3,4]. Despite the prominence of craniofacial injury in the pediatric population, the incidence of associated facial fractures in children is lower than it is for adults [5]. The anatomic and developmental differences between the adult and pediatric facial skeleton are responsible for the differences in fracture pattern between the two populations. At birth, the ratio of cranial to facial volume is approximately 8:1, while that of the adult is 2.5:1 [6]. The cranium grows rapidly in the first 5 years of life, while the midface and mandible do not reach adult proportions until the teenage years. Furthermore, the maxillary and frontal sinuses do not complete pneumatization until the ages of 5 and 8 years, respectively [7]. The presence of unerupted teeth in the maxilla and mandible further increases the density of the pediatric facial skeleton and adds to its structural stability [5]. The low volume and high density of the face relative to the cranium produces a pattern of increased cranial and frontoorbital injury relative to facial injury in children. As children age, the vertical growth of the facial skeleton shifts the injury pattern toward that of adults, with an increase in the incidence of facial fractures [8].
The disparity between craniofacial fracture patterns in children and adults may present different complication profiles. Many studies have shown that pediatric facial trauma shares a strong association with concomitant extra-facial head and neck injury [3,5,9,10,11]. One complication of particular importance is intracranial hemorrhage (ICH), which has been well documented to occur in association with facial fractures [12,13,14]. ICH is an important complication to recognize, as it can cause death or lifelong disability in children (Figure 1). Though possible causes include brain tumors, congenital heart disease, and vascular lesions, the most common cause of ICH in children, and the one with the highest associated morbidity and mortality, is trauma [15,16]. Because ICH at an early age is associated with developmental delay, cerebral palsy, epilepsy, and death, early recognition is imperative. Presenting signs include mental status changes, headaches, convulsions, focal neurological deficits, and vomiting [15]. Specifically, skull fracture, focal neurological deficit, seizure, and Glasgow coma scale (GCS) < 15 were all significantly correlated with ICH according to a 2014 meta-analysis investigating the association of particular symptoms to ICH in pediatric patients with minor head trauma. The utility of the GCS was further corroborated by a study showing a very low incidence of ICH in pediatric patients with minor head trauma and a GCS of 15 [17]. Important considerations in management include GCS, type of hemorrhage, and presence of high-risk comorbidities. Intraventricular hemorrhage, epidural hematoma, and comorbidities such as shunted hydrocephalus and arteriovenous malformation have been implicated in radiologic progression of hemorrhage, and are therefore indications for monitoring in an intensive care setting [18].
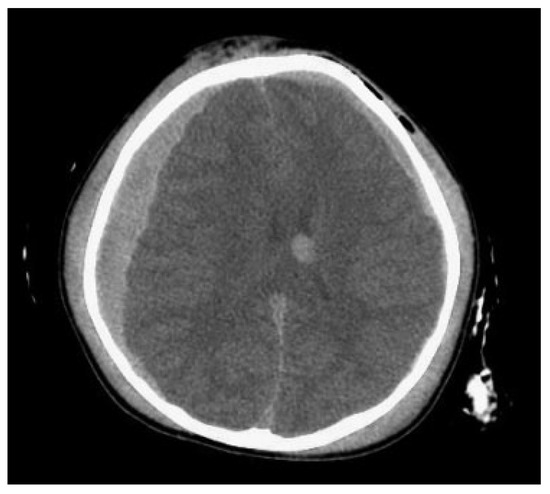
Figure 1.
A 2-year-old child with significant intracranial injury following a fall.
It is our goal to further the limited fund of knowledge on this topic by exploring patterns within this subset of patients. The purpose of our study is to aid clinicians in recognizing and managing ICH in the setting of pediatric facial fracture by examining its association with patient presentation, concomitant injuries, and fracture pattern at a level I trauma center in an urban environment.
Methods
Following institutional review board approval, data from January 2000 to December 2012 were collected by searching International Classification of Disease, Revision 9 codes to isolate facial fracture patients diagnosed radiologically at a level 1 trauma center (the University Hospital, Newark, NJ). The list of facial fracture patients was further refined to only include patients of 18 years or younger and those with a documented ICH. Patient age, GCS on presentation, fracture location, type of hemorrhage, and management strategies were collected from the remaining patient charts and subject to analysis. Categorical data were analyzed by Pearson chisquare test for independence and continuous data were analyzed by the t-test for comparison of means. A preset p-value of 0.05 was used to determine significance.
Results
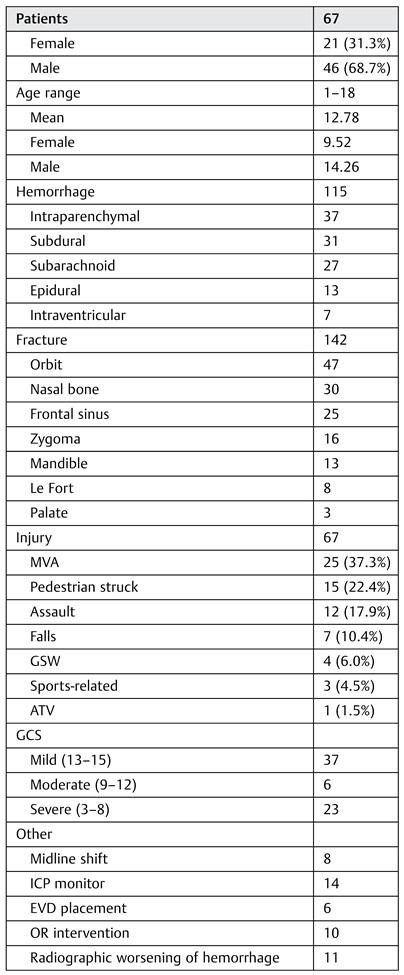
During this time period, 3,147 patients with facial fractures were treated at our institution. There were 353 patients, 18 years of age or younger, and 68 were excluded due to insufficient data. A summary of the demographic data, hemorrhage type, fracture location, and cause of injury for the remaining 285 pediatric facial fractures patients can be found in Table 1.

Table 1.
Summary of pediatric facial fracture patients with concomitant intracranial hemorrhage.
To determine whether or not, there was an association between each fracture location and the occurrence of ICH, we analyzed our data by a chi-square test for independence. Our results showed that the presence of each fracture and the incidence of ICH were not independent of each other (with the exception of palate fractures, which failed to show significance). All fracture types were associated with increase in ICH, with one notable exception being mandibular fractures. Whereas 36.5% of our patients without mandibular fractures had associated ICH, only 9.49% of our patients with mandibular fractures had associated ICH.
We further analyzed our subset of 67 patients with ICH to determine whether any fracture patterns were associated with a specific type of hemorrhage. Our analysis revealed that the presence of orbital (χ2 [1, n = 67] = 6.86, p = 0.01) and frontal sinus (χ2 [1, n = 67] = 4.05, p = 0.04) fractures was associated with an increase in epidural hemorrhage (EDH) incidence, while the presence of mandible (χ2 [1, n = 67] = 3.88, p = 0.05) and nasal (χ2 [1, n = 67] = 5.64, p = 0.02) fractures was associated with a decrease in EDH. Despite differences in associated hemorrhages, no particular fracture was associated with a change in mortality. Indeed, the only recorded variable that was associated with an increase in fatality was intubation in the emergency department (χ2 [1, n = 67] = 7.45, p = 0.01).
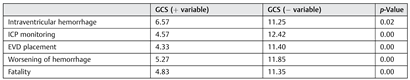
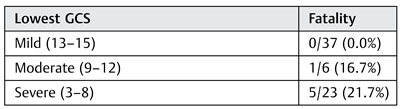
The mean patient age and GCS were calculated with regard to fatality, each type of hemorrhage, midline shift, ICP monitoring, EVD placement, OR (operating room) intervention, and worsening of hemorrhage on repeat imaging. Means were subject to analysis by t-test for comparison of means in the presence and absence of the above-stated variables. Our analysis indicates that patients who received surgical intervention were significantly younger than those who did not (7.7 vs. 13.7, p < 0.05). We also found a significantly decreased GCS in patients who underwent ICP monitoring and EVD placement, as well as those who suffered intraventricular hemorrhage, worsening of hemorrhage on repeat imaging, and fatality (Table 2 and Table 3).

Table 2.
Average lowest GCS score in the presence versus absence of listed variables.

Table 3.
Fatality rate stratified by GCS category.
Discussion
There is a limited amount of scientific literature detailing the prevalence and patterns of ICH in pediatric facial fracture patients. The importance of identifying such an injury in the context of facial fractures is important not only because of the gravity of the consequences but also because of the ability for facial fractures to obscure signs of ICH. In a study describing this masking effect, the incidence of ICH was investigated in a sample of 2,195 maxillofacial fracture patients with a mean age of 34.9 years. In this study, 9.7% of the patients suffered ICH, with the strongest predictors being basal skull and cranial vault fractures [19]. Ferreira et al. investigated the incidence of complications specifically in the pediatric facial fracture population, and found that 10.0% of the 1,416 patients enrolled in the study suffered ICH. The incidence of ICH (23.5%) in our study was higher than the incidence reported in either of these studies. This difference may be explained by the high proportion of violent crimes (assault and gunshot wounds) and low proportion of sports injuries and falls when comparing our study to previous studies.
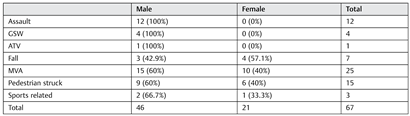
Craniofacial trauma presents differently in the pediatric and adult populations. These differences stem not only from the differences in the types of injuries sustained by children and adults but also from differences in pediatric and adult facial anatomy. In our study, the most common fractures observed were those of the orbit, nasal bone, frontal sinus, and zygoma, while mandibular, mid-facial, and palatal fractures were less common. Such a pattern can be explained by the increased cranial-to-facial volume, presence of unerupted teeth, and incomplete pneumatization of sinuses found in children [3,4,6,7,8]. The predominance of fronto-orbital factures in our study reflected that of the literature, as did the predominance of intraparenchymal, subdural, and subarachnoid hemorrhages and low incidence of intraventricular and EDHs [16,18]. Also in line with much of the facial fracture literature was the strong male predominance [3,5,8,9,11,19,20,21]. Interestingly, there was a significant (12.78 vs. 9.52, p < 0.01) age difference between male and female patients in this study. In the previous study, we reported a significant difference between the ages of male and female pediatric facial fracture patients (14.7 vs. 12.7, p < 0.05) [22]. It seems that, among the subset of facial fracture patients with ICH, this age difference is exaggerated. This divide is likely a consequence of the differences in cause of injury between sexes. In this study, violent crimes, which were prevalent in the male patients while absent in the female patients, tend to occur in older individuals (Table 4) [20,21,23].

Table 4.
Causes of injury in male versus female patients.
Upon analysis of fracture pattern and incidence of ICH, an interesting trend was discovered. Although the majority of facture locations were associated with the expected increase in ICH, mandibular fractures were actually associated with the absence of ICH. A similar phenomenon was described by Lee et al., who reported a relative decrease in closed-head injuries when comparing patients with fractures of the lower face to those with mid- and upper face injuries [13]. The proposed explanation was that the triplanar arrangement of facial bones could act as a cushion against violent forces to the cranium. Keenan et al. disputed the assertion that the face protects the brain, for their data show that facial fractures impart a 10-fold increased risk for intracranial injury compared with patients with similar injuries but no facial fractures. Within the stratified facial fracture data presented in this study, however, mandibular fractures alone failed to show a significant increase in intracranial injury [24].
We also looked at certain aspects of patient presentation and hospital course to determine if these parameters had any significant association with patient outcomes. In doing so, we found a significant association between fatality and the need for intubation in the emergency department. Furthermore, patients who suffered fatal injury also had a significantly lower GCS compared with those who survived (4.83 vs. 11.35, p < 0.01). A low GCS was also associated with the presence of intraventricular hemorrhage, the need for EVD placement or ICP monitoring, and radiographic worsening of hemorrhage. These findings stress the importance of the GCS as an indicator for injury severity and support studies describing its association with prognosis [16,17,18].
Conclusion
The substantial differences between pediatric and adult facial fractures highlighted in this article advocate the importance of studying these injuries separately. Although the reports of ICH in the context of pediatric facial fractures are abundant, there are limited data describing the patterns and outcomes of this complication specifically. Our study attempts to fill this void, and to do so from the unique perspective of an urban trauma center with a high incidence of violent injury. In this population, we have found a negative association between fracture of the mandible and ICH. Furthermore, there was a significant association between the need for intubation in the emergency department and the outcome of fatality in our patients. Finally, our results support the use of the GCS as a prognostic indicator, as GCS was significantly lower in patients who experienced radiologic worsening of hemorrhage and as well as those who suffered fatal injuries. It is our goal that these findings will aid clinicians in early recognition of ICH in the setting of a facial fracture and promote understanding of poor prognostic signs in hopes that we may better avoid the life-threatening consequences of this injury.
References
- Heron, M. Deaths: Leading causes for 2010. National vital statistics reports: From the Centers for Disease Control and Prevention, National Center for Health Statistics. National Vital Statistics System 2013, 62, 1–96. [Google Scholar]
- Nawar, E.W.; Niska, R.W.; Xu, J. National Hospital Ambulatory Medical Care Survey: 2005 Emergency Department Survey. Adv Data 2007, 1–32. [Google Scholar]
- Eggensperger Wymann, N.M.; Hölzle, A.; Zachariou, Z.; Iizuka, T. Pediatric craniofacial trauma. J Oral Maxillofac Surg 2008, 66, 58–64. [Google Scholar] [CrossRef]
- Pal’a, A.; Kapapa, M.; Posovszky, C.; et al. Head injury in children: Has a change in circumstances caused an increase in treatment numbers? J Child Neurol 2014, 4. [Google Scholar]
- Gassner, R.; Tuli, T.; Hächl, O.; Moreira, R.; Ulmer, H. Craniomaxillofacial trauma in children: A review of 3,385 cases with 6,060 injuries in 10 years. J Oral Maxillofac Surg 2004, 62, 399–407. [Google Scholar] [CrossRef]
- Cole, P.; Kaufman, Y.; Hollier, L.H., Jr. Managing the pediatric facial fracture. Craniomaxillofac Trauma Reconstr 2009, 2, 77–83. [Google Scholar] [CrossRef] [PubMed]
- Shah, R.K.; Dhingra, J.K.; Carter, B.L.; Rebeiz, E.E. Paranasal sinus development: A radiographic study. Laryngoscope 2003, 113, 205–209. [Google Scholar] [CrossRef]
- Boyette, J.R. Facial fractures in children. Otolaryngol Clin North Am 2014, 47, 747–761. [Google Scholar]
- Imahara, S.D.; Hopper, R.A.; Wang, J.; Rivara, F.P.; Klein, M.B. Patterns and outcomes of pediatric facial fractures in the United States: A survey of the National Trauma Data Bank. J Am Coll Surg 2008, 207, 710–716. [Google Scholar] [CrossRef]
- Ferreira, P.C.; Amarante, J.M.; Silva, P.N.; et al. Retrospective study of 1251 maxillofacial fractures in children and adolescents. Plast Reconstr Surg 2005, 115, 1500–1508. [Google Scholar] [CrossRef]
- Ferreira, P.C.; Barbosa, J.; Braga, J.M.; Rodrigues, A.; Silva, A.C.; Amarante, J.M. Pediatric facial fractures: A review of 2071 fractures. Ann Plast Surg 2015, 30. [Google Scholar]
- Haug, R.H.; Savage, J.D.; Likavec, M.J.; Conforti, P.J. A review of 100 closed head injuries associated with facial fractures. J Oral Maxillofac Surg 1992, 50, 218–222. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.F.; Wagner, L.K.; Lee, Y.E.; Suh, J.H.; Lee, S.R. The impact-absorbing effects of facial fractures in closed-head injuries. An analysis of 210 patients. J Neurosurg 1987, 66, 542–547. [Google Scholar] [CrossRef] [PubMed]
- Hoppe, I.C.; Kordahi, A.M.; Paik, A.M.; Lee, E.S.; Granick, M.S. Examination of life-threatening injuries in 431 pediatric facial fractures at a level 1 trauma center. J Craniofac Surg 2014, 25, 1825–1828. [Google Scholar] [CrossRef]
- Lo, W.D.; Lee, J.; Rusin, J.; Perkins, E.; Roach, E.S. Intracranial hemorrhage in children: An evolving spectrum. Arch Neurol 2008, 65, 1629–1633. [Google Scholar] [CrossRef]
- Zakhary, M.M.; Wesolowski, J.R.; Sewick, A.E.; et al. Prevalence and etiology of intracranial hemorrhage in term children under the age of two years: A retrospective study of computerized tomographic imaging and clinical outcome in 798 children. Acad Radiol 2009, 16, 572–577. [Google Scholar] [CrossRef]
- Hamilton, M.; Mrazik, M.; Johnson, D.W. Incidence of delayed intracranial hemorrhage in children after uncomplicated minor head injuries. Pediatrics 2010, 126, e33–e39. [Google Scholar] [CrossRef]
- Greenberg, J.K.; Stoev, I.T.; Park, T.S.; et al. Management of children with mild traumatic brain injury and intracranial hemorrhage. J Trauma Acute Care Surg 2014, 76, 1089–1095. [Google Scholar] [CrossRef]
- Hohlrieder, M.; Hinterhoelzl, J.; Ulmer, H.; Hackl, W.; Schmutzhard, E.; Gassner, R. Maxillofacial fractures masking traumatic intracranial hemorrhages. Int J Oral Maxillofac Surg 2004, 33, 389–395. [Google Scholar] [CrossRef]
- Kim, S.H.; Lee, S.H.; Cho, P.D. Analysis of 809 facial bone fractures in a pediatric and adolescent population. Arch Plast Surg 2012, 39, 606–611. [Google Scholar] [CrossRef][Green Version]
- Grunwaldt, L.; Smith, D.M.; Zuckerbraun, N.S.; et al. Pediatric facial fractures: Demographics, injury patterns, and associated injuries in 772 consecutive patients. Plast Reconstr Surg 2011, 128, 1263–1271. [Google Scholar] [CrossRef] [PubMed]
- Hoppe, I.C.; Kordahi, A.M.; Paik, A.M.; Lee, E.S.; Granick, M.S. Age and sex-related differences in 431 pediatric facial fractures at a level 1 trauma center. J Craniomaxillofac Surg 2014, 42, 1408–1411. [Google Scholar] [CrossRef] [PubMed]
- Hoppe, I.C.; Kordahi, A.M.; Paik, A.M.; Lee, E.S.; Granick, M.S. Pediatric facial fractures as a result of gunshot injuries: An examination of associated injuries and trends in management. J Craniofac Surg 2014, 25, 400–405. [Google Scholar] [CrossRef] [PubMed]
- Keenan, H.T.; Brundage, S.I.; Thompson, D.C.; Maier, R.V.; Rivara, F.P. Does the face protect the brain? A case-control study of traumatic brain injury and facial fractures. Arch Surg 1999, 134, 14–17. [Google Scholar] [CrossRef]
© 2015 by the author. The Author(s) 2015.