The transconjunctival approach to the lower eyelid was first described by Bourguet for blepharoplasty in 1924 [
1]. The approach was subsequently recommended by Tenzel and Miller and also popularized by Tessier and Converse et al., who applied this method successfully to the treatment of congenital and craniofacial deformities [
2,
3,
4]. Many variations of this approach have been described with technical aspects that differ significantly [
5,
6]. The transconjunctival approach has been demonstrated to be safe and effective, compared with subciliary and subtarsal approaches to the orbital floor, with lower overall complication rates [
5,
7,
8].
In acute orbital trauma, dissection is hindered by swelling and ecchymosis, which often makes correct tissue planes difficult to identify [
9]. Retrodisplacement of the inferior orbital rim, as commonly seen with orbital fractures, further hinders identification of the proper plane of dissection. It is easy for the resident, less experienced surgeon or anyone unfamiliar with orbital surgery to dissect into the wrong plane and stray either into the orbital fat pads or through the periorbital muscles and even perforate the skin. Dissection may result in injury to the inferior oblique or orbicularis muscles, either of which may negatively impact subsequent eyelid or eye function. Direct injury to the orbicularis muscle may result in contracture and scarring with subsequent static retraction of the lower eyelid. Damage to the innervation of the orbicularis muscle may also contribute to dynamic postoperative lower eyelid dysfunction [
10,
11,
12].
Incomplete release of the lateral canthal attachment may contribute to the difficulty of dissection when attempting the transconjunctival technique, especially when approaching more extensive fractures or when pronounced swelling is present.
As a result, many surgeons are still hesitant to utilize this approach. Familiarity with the anatomy and a safe technique of dissection will improve the speed of dissection with a technique that lessens the risk of inadvertent injury to surrounding structures.
A technique is described and illustrated for the transconjunctival approach to the orbital rim and floor by transection and repair of the tarsus medial to the lateral collateral ligament which focuses on the technical and anatomic details we feel make this approach simple and easy to perform.
Technique
After induction of general anesthesia, the patient is positioned. A horseshoe or donut headrest may be used depending on the preference of the surgeon. Ophthalmic Betadine is used for skin preparation of the upper face. The orbital area is carefully inspected and palpated on both sides at the beginning of the procedure and the presence or absence of symmetry of the orbits, globes, and eyelids is noted as a baseline for comparison at the end of the procedure. Old photographs can be helpful to establish and confirm preinjury architecture, although these are usually not available in the acute setting.
The eyes are irrigated with ophthalmic saline irrigation and corneal protectors are placed.
A 1- to 2-cm transverse line is drawn just below the ciliary margin for a skin–muscle incision. A short perpendicular extension is then drawn superiorly from this line across the lower lid margin such that this line is ~2 to 3 mm medial to the lateral canthus of the eye and it meets the transverse line at its midpoint (
Figure 1). The incision line can be extended medially beyond the vertical extension for increased exposure.
The resulting eyelid scar will be very difficult to appreciate if this incision is kept entirely within the eyelid skin. The eyelid skin is medial to the bony orbital rim and can be visibly identified by the difference of its appearance from the surrounding cheek and lateral orbital skin.
This incision line is infiltrated with a small amount of local anesthetic with epinephrine. Great care is taken to place this only in the subdermis. No more than 1 cc is usually necessary.
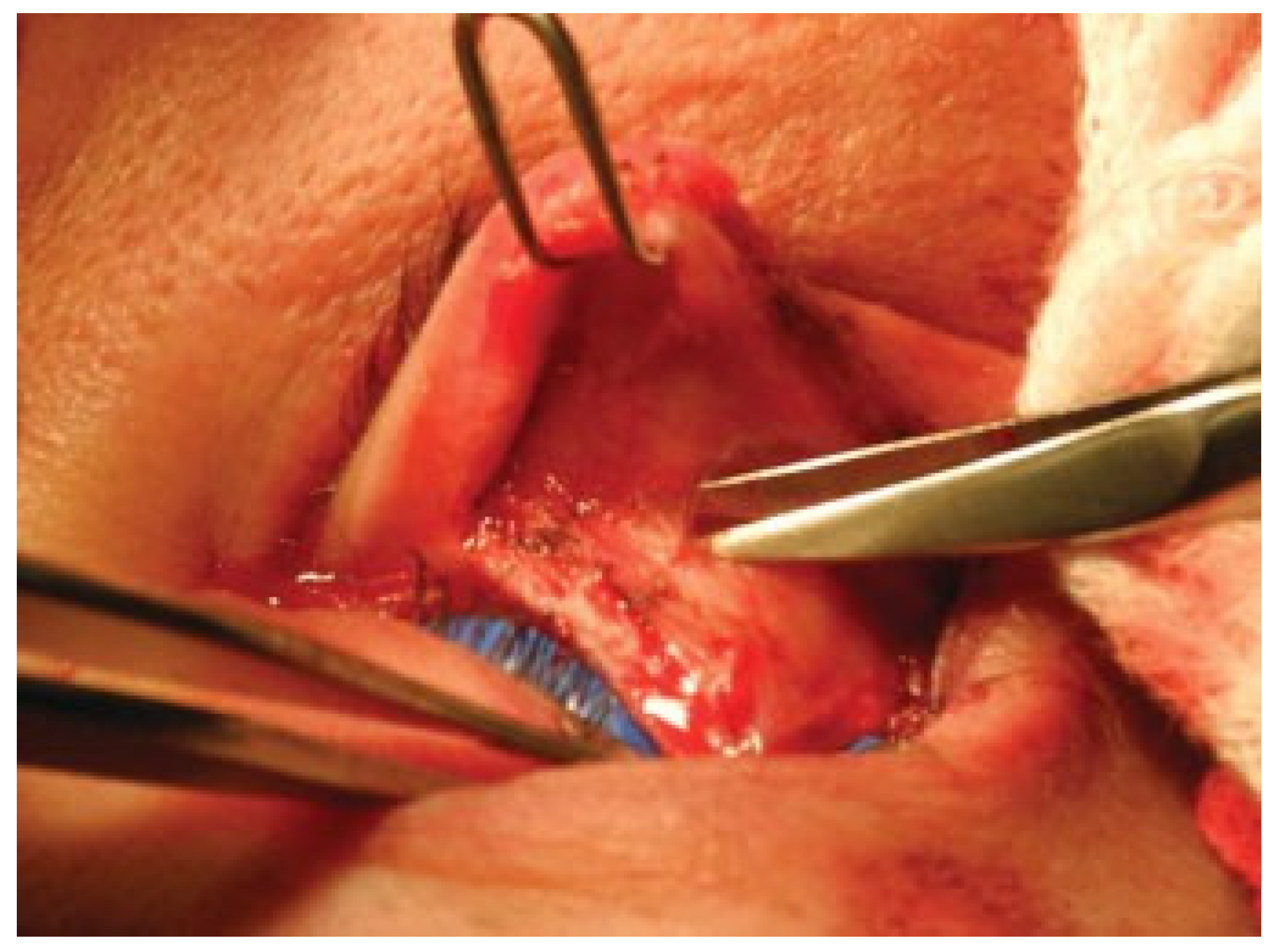
The skin is incised with the scalpel and the lateral end of the tarsal plate beneath is divided with scissors (
Figure 2). The lateral orbicularis muscle is divided with needlepoint cautery to release the lateral lower eyelid fully. A medium Joseph double hook or fine-toothed forceps is used to retract and evert the lower eyelid, and any residual restricting bands of fascia or muscle can be easily identified and divided. The lid should now easily retract to expose the conjunctiva, which is incised just inferior to the tarsal plate. Curved iris or Littler scissors are then inserted and used to elevate the conjunctiva in a gentle spreading fashion and then divide the elevated conjunctiva (
Figure 3). Alternatively, a fine needlepoint cautery on a low setting can be used to incise the conjunctiva. With the Joseph double hook retracting at an angle of 90 degrees to the facial plane and with countertraction applied by the surgeon with fine-toothed forceps to the divided conjunctiva directed cranially at an angle of 90 degrees to the Joseph double hook, the correct plane, either between the orbital fat and the orbital septum (retroseptal approach), or between the orbital septum and the orbicularis (preseptal approach), is usually easy to identify and follow with gentle spreading with scissors (
Figure 4 and
Figure 5).
The vector of dissection proceeds initially from cranial to caudal and then from lateral to medial (
Figure 1). It is usually easy to identify the lateral orbital rim laterally and from there locate the desired plane of dissection. This plane becomes more difficult to identify in swollen and hemorrhagic eyelids and is particularly difficult to find medially where it is easy to stray into the plane between the orbital fat pads and risk injury to the inferior oblique muscle.
The plane should appear as a layer of avascular areolar tissue (
Figure 4 and
Figure 5). If blood vessels are encountered, then the dissection may be proceeding inadvertently into the plane between the individual orbital fat pads rather than remaining in the correct plane either above or below the orbital septum.
The plane is followed to the inferior orbital rim and the white line of the arcus marginalis should be visible. With zygoma fractures, the rim may be displaced posteriorly and this may make it more difficult to identify the proper vector of dissection. Palpation with a fingertip will also help identify the position of the rim.
The periosteum is divided with cautery and further dissection is performed as dictated by the particular fracture pattern with a sharp periosteal elevator, using a malleable and/or Desmarres retractors. The incision can be extended medially to the posterior lacrimal crest in a retrocaruncular fashion to expose the medial orbital wall if necessary.
Closure is initiated with reapproximation of the periosteum over the infraorbital rim. A single buried submucosal suture of fine absorbable material at the lateral corner of the transconjunctival incision can help align the conjunctiva but it is important to bury this suture and its knot well to prevent corneal irritation. The inferior tarsal plate is then reapproximated with a single suture. Polypropylene or 6–0 Vicryl can be used for this purpose. If desired, a vertical tarsal resection can be performed at this point to tighten the lower eyelid. The placement of the incision 2 to 3 mm medial to the lateral canthus makes it relatively easy to align the lower lid properly (
Figure 6). The divided portion of the orbicularis muscle is now reapproximated with buried absorbable sutures, covering the canthal polypropylene suture. Finally, the lateral incision may be closed with fine buried absorbable sutures; external sutures are optional.
Discussion
The principles of management of facial fractures have been well established and these include adequate exposure of the fracture sites across the relevant bony buttresses, anatomic reduction of these buttresses, and rigid fixation in proper anatomic alignment.
Proper exposure of fracture sites is the critical first step to accurate reduction of facial fractures. The ideal approach for exposure should be technically easy to accomplish, rapid and accurate to perform, provide adequate exposure, have a low risk of complications, and leave minimal scarring.
There are several approaches to the inferior orbital rim and upper maxilla through the lower eyelid and modifications have been described for each of these. These approaches include subciliary, midtarsal, subtarsal, inferior orbital rim, and transconjunctival techniques. The subciliary approach with a skin–muscle flap was historically the most frequently employed and most familiar to plastic surgeons [
8]. Its drawbacks include a visible scar, persistent edema, and the risk of cicatricial deformation of the lower eyelid that can include lower lid malposition, ectropion, and exposure of the globe. Despite its limitations, most surgeons are very comfortable with this approach. In recent years, however, the transconjunctival approach has gained in popularity and become the preferred approach in the hands of many surgeons [
13].
In general, it is felt that the lower the incision is made on the lower lid, the more visible the resultant scar but the lower the likelihood of lower eyelid malposition sequelae such as ectropion, scleral show, and lid lag. For many, the transconjunctival approach is a way to avoid the trade-offs characteristic of the transcutaneous approaches. Ridgway et al., in their report and meta-analysis, found an overall lower risk of complications, including ectropion, lower lid edema, and hypertrophic scarring with the transconjunctival approach. They preferred to use the transconjunctival approach for isolated orbital floor fractures and recommended the addition of a canthotomy for the more difficult zygomatic complex fracture management [
5].
We feel the transconjunctival approach is ideal for access to the inferior orbital rim and orbital floor and with extension can provide good access to the lower medial and entire lateral orbital walls. Complication rates of 0.3 to 7% have been reported and these compare favorably with other approaches [
5,
6,
7,
14].
As the subciliary approach is still commonly used and taught, many residents and attending surgeons are more familiar with it, and becoming comfortable with the transconjunctival approach can be difficult for several reasons. There are many modifications to the transconjunctival approach including preseptal and postseptal dissection, addition of a lateral extension onto the eyelid skin, cantholysis, and the transcaruncular or retrocaruncular extension. In addition, details of dissection technique, which can make the utilization of this approach easier and more comfortable for the surgeon, are often lacking in the literature. Confusion regarding the relative merits of these modifications makes it difficult for residents and novice attendings to choose and become comfortable with one transconjunctival method and understand its indications and limitations. Identification of the appropriate plane of dissection can be difficult in the posttraumatic orbit where edema, ecchymosis, and retrodisplacement of the inferior rim are often present. These factors can make dissection more difficult, especially through any incision that seems to limit access and may increase the risk of injury to the orbicularis muscle or its nerves and potentially increase complications rates. The key to neutralizing these confounding factors, minimizing complications, and becoming comfortable with this approach is to develop a simple, fast, and accurate technique of dissection that provides excellent exposure of the site of injury.
The transconjunctival approach without release of the supporting structures of the lower lid leaves a completely hidden scar but is felt by many to offer more limited exposure of the inferior orbital rim and orbital floor. Achieving a greater degree of exposure requires extending the incision laterally and this can be accomplished either by dividing and releasing the entire lateral canthal tendon or by releasing only the lower lid supporting structures. Extension of the transconjunctival approach with the addition of a lateral tarsal plate and lid division will provide exposure equivalent to any other technique and without the need for canthal reattachment. We prefer limiting the release of the support structures to the lower lid only, as described by Salgarelli et al., Kim et al., and others [
3,
7,
15]. Extending the incision through the lateral aspect of the tarsal plate alone avoids disrupting the entire tendon and leaves an incision that is easy to reapproximate. By extending the incision along a preexisting crease in the lower lid, it is possible to carry the incision as far as one needs laterally and the exposure achieved is as adequate as that achieved with the subciliary approach. The resultant cutaneous scar is inconspicuous as long as the skin incision is not carried beyond the bony lateral orbital rim. By dividing only the lateral tarsal plate, reapproximation is made simpler and faster.
This approach can also be easily applied to cosmetic lower lid blepharoplasty. The excellent exposure is compatible with techniques for orbital fat pad manipulation and shortening or tightening of the lower lid can easily be achieved with direct vertical resection of the tarsus and skin as indicated in both traumatic and cosmetic applications (
Figure 7).
The other technical points described here are important in minimizing lower eyelid malfunction postoperatively. Finding the correct plane early makes it faster and easier to expose the lower rim and do so with minimal trauma to the orbicularis muscle, its innervation, and the remaining contents of the orbit. Ramirez, Mackinnon, and others have described the innervation of the lower eyelid orbicularis muscle arising from the zygomatic and buccal branches of the facial nerve [
10,
11]. These nerve branches enter the deep surface of the muscle at right angles to the muscle fibers along the lateral and inferior aspect of the muscle. Transection of the intramuscular portion of these nerves, by incisions that intentionally split the muscle fibers or by straying from the proper plane of dissection, can result in lid lag and ectropion due to dysfunction of the de-innervated portion of the muscle (
Figure 8). It is also possible for the dissection to stray into the orbital soft tissue planes, placing nerves and muscles of the orbit at risk for injury [
9]. Beginning the dissection laterally allows easy identification of the correct plane of dissection and rapid exposure of the arcus marginalis along the inferior orbital rim. The dissection can then be carried medially with greater certainty. We have found that spreading dissection with scissors helps identify the proper plane and this technique has been advocated by others [
7,
14]. Insertion of a Joseph double hook to apply traction at 90 degrees to the facial plane by an assistant, coupled with direct traction applied by the operating surgeon with Bishop-Harmon forceps to the orbital septum, demonstrates the loose avascular areolar plane that exists between the orbital septum and the orbicularis muscle nicely. It is easy to stray inadvertently between the overlapping medial and middle orbital fat pads during this portion of the dissection and finding the orbital rim laterally and progressing dissection from lateral to medial minimizes this risk by providing a reliable landmark for navigation. Once the arcus marginalis is identified, the remainder of the exposure is generally straightforward.
Closure is fairly simple. The periosteum is reapproximated across the inferior orbital rim. Minimizing stripping of periosteum during the initial approach will lessen the need to resuspend tissues at this point. Suturing of the conjunctiva is not absolutely necessary but we have found that a single subconjunctival suture of 5–0 fast absorbing gut placed at the point where the conjunctival incision makes the 90 degree turn below the tarsal plate is helpful to realign the conjunctiva and prevent inversion during healing. Division of the lateral aspect of the tarsal plate slightly medial to the lateral canthus makes it much easier to properly align the tendon and tissues. The muscle can then be closed with one or two sutures of 5–0 absorbable monofilament and finally skin is closed in whatever technique the surgeon prefers.
Conclusion
The transconjunctival approach to the orbit has been demonstrated to be safe and is associated with fewer complications than other approaches to the lower eyelid. However, the accurate application of this approach can be complicated by significant variations in technique, the difficulty in dissection in the acutely traumatized orbit, and concerns over incomplete exposure of the operative site. We present the technical details of a simple, rapid, and accurate technique that allows full exposure of the orbital floor and the medial/lateral orbital walls safely and expediently and review the literature regarding comparable approaches.