The condyle is the most frequently injured anatomical region of the mandible and condylar fractures comprise between 17.5 and 62% of all mandibular fractures; unilateral condylar fractures comprise approximately two-thirds of all of these fractures [
1,
2,
3].
Possible complications from such fractures include temporomandibular (TMJ) ankylosis and dysfunction, including chronic dislocation, pain, and malocclusion. Moreover, condylar fractures in a growing patient may result in growth disturbances at multiple facial levels, including the orbits, cheeks, maxilla, and mandible [
3,
4,
5].
Treatment of condylar fractures is variable and controversial. Options for management include surgical and nonsurgical methods. The nonsurgical approach is generally preferred for intracapsular or high subcondylar fractures, especially in the growing patient [
6,
7]. There are few absolute indications for surgical treatment: nonsurgical treatment cannot reestablish the pretraumatic occlusion, stability of the occlusion is limited, fractured segment is displaced into the middle cranial fossa, and patient preference. In the absence of these factors, nonsurgical approach can be considered, and whenever a nonsurgical method is as effective as the surgical one, the former is preferred [
1,
8].
The purpose of this article is to present three patients with significantly displaced condylar fractures treated nonsurgically with pre- and posttreatment imaging. The first two cases described are adult patients with high-quality computed tomography (CT) imaging and three-dimensional (3D) reconstructions, and the third case is a toddler with plain film imaging and a 14.5-year clinical follow-up. It is especially rare and not documented in the literature to have pre- and posttreatment CT scans with 3D reconstruction in patients treated nonsurgically. As such, this report is useful in presenting three examples of repositioning and reformation of displaced condylar fractures in a postmenarche 14-year-old female patient, a 21-year-old male patient, and an 18-month-old male patient.
Three Patient Series
A postmenarche 14-year-old female patient was referred to the Division of Oral and Maxillofacial Surgery by her orthodontist for malocclusion 1 day following jaw trauma. The orthodontic treatment was being performed for dental crowding and was near completion with a class I occlusion.
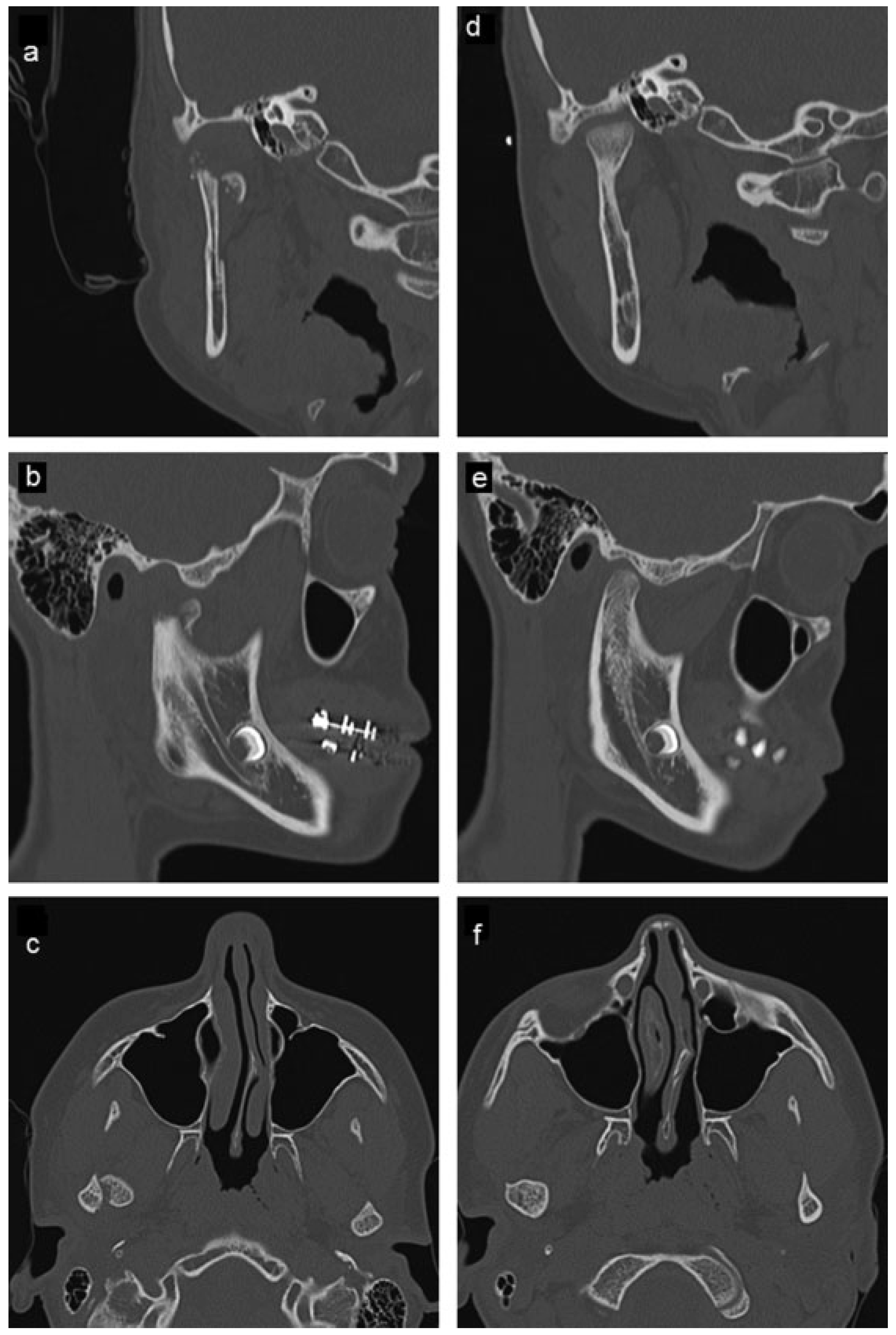
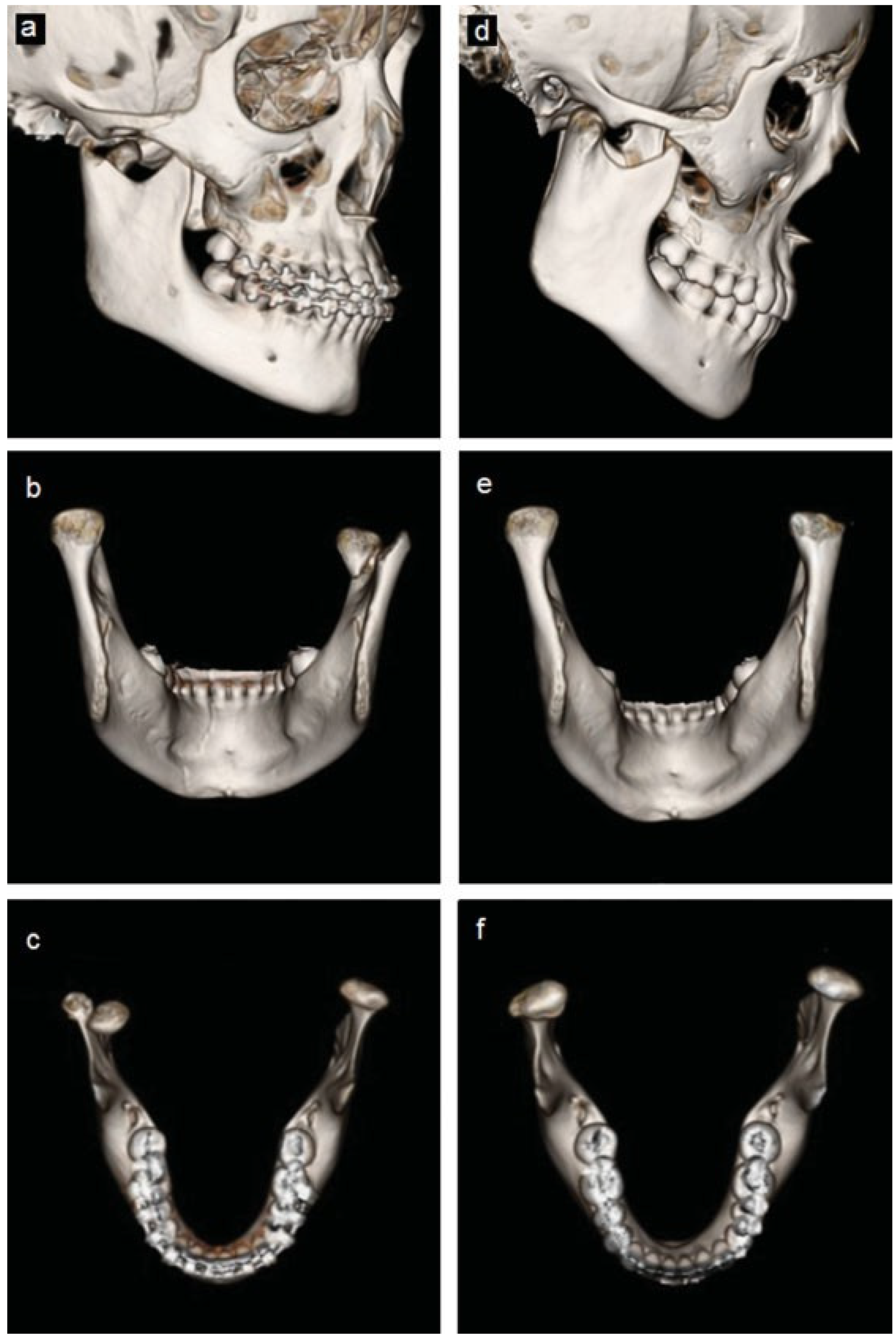
The patient experienced right preauricular pain with jaw movement. An end-to-end unilateral class II malocclusion with a shift of the mandibular midline 2 mm to the left and trismus was documented. CT imaging revealed a displaced, oblique right-sided high subcondylar fracture, and a left nondisplaced parasymphyseal fracture. The fractured right condylar head was displaced anteriorly, medially, and inferiorly (
Figure 1a–c and
Figure 2a–c). Nonsurgical treatment was instituted, with light intermaxillary elastics on the existing orthodontic appliances with a blenderized diet for 6 weeks. She was compliant with the treatment. During the first 6 weeks of observation the patient was documented to have a stable class I occlusion. She was instructed to continue nocturnal elastics as long as the orthodontist advised and to return to a normal diet as tolerated.
The patient returned in 1 year. At this visit, her only complaint was a sporadic mild dull ache of the right face with prolonged heavy chewing function. She denied joint noise or limitation of motion and tolerated a normal diet. A class I occlusion with excellent intercuspation and excellent mandibular range of motion was documented. There was no myofascial or joint pain with occlusal loading. A CT scan was obtained which showed complete healing of the right condyle which was appropriately positioned in the glenoid fossa (
Figure 1d–f and
Figure 2d–f). A normal joint space was presented with no evidence of condylar or the glenoid fossa cortical or cancellous osseous abnormalities.
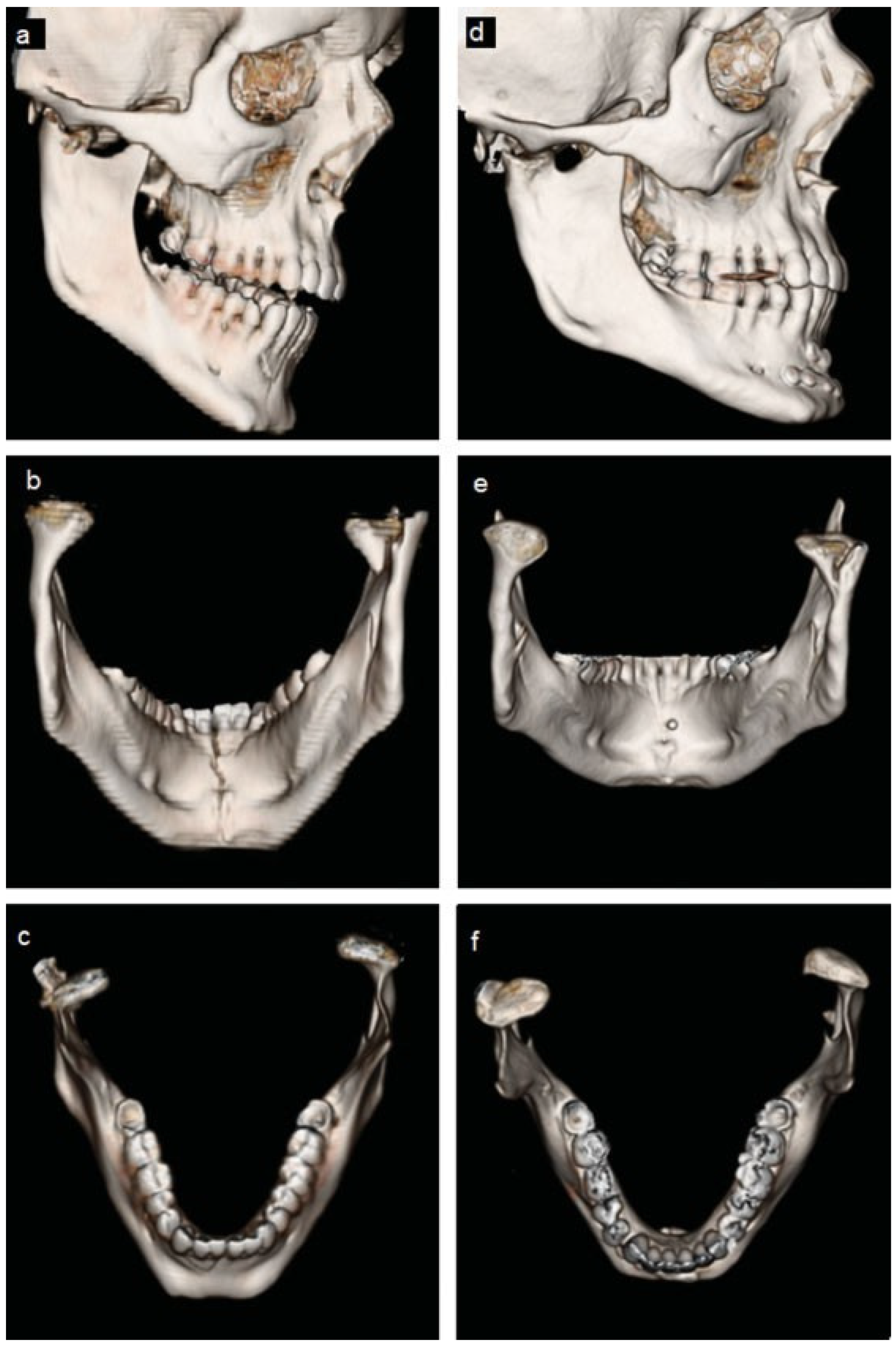
The second patient, a healthy 21-year-old male patient presented to the emergency department at another health institution after being involved in interpersonal violence and falling on his chin. He suffered a right-sided displaced and left-sided nondisplaced condylar neck fractures and a displaced mandibular symphysis fracture. A CT scan was taken (
Figure 3a–c and
Figure 4a–c). The patient underwent open reduction and internal fixation of the symphysis fracture; and nonsurgical treatment of the bilateral condylar fractures with placement of Erich arch bars and intermaxillary elastics with light function.
The patient was first seen at our clinic for a follow-up evaluation 6 months after the initial treatment. At this time he had regained full mandibular function and denied myofascial or TMJ symptoms. He also denied limitation of motion, noise with TMJ function, and was tolerating a normal diet. His occlusion was a stable class I with good interdigitation. There was an excellent range of motion with slight deviation to the right with wide opening. There was no myofascial pain or joint pain with occlusal loading. A CT scan was obtained due to concerns by his previous physician regarding the possible need to surgically reposition the previously displaced condyle d–f and
Figure 4d–f). This CT scan showed reformation and repositioning of the right condyle with normal cortical and cancellous anatomy but with a slight anteroinferiorly displaced position with associated mild flattening of the condylar head. Additional treatment was not advised.
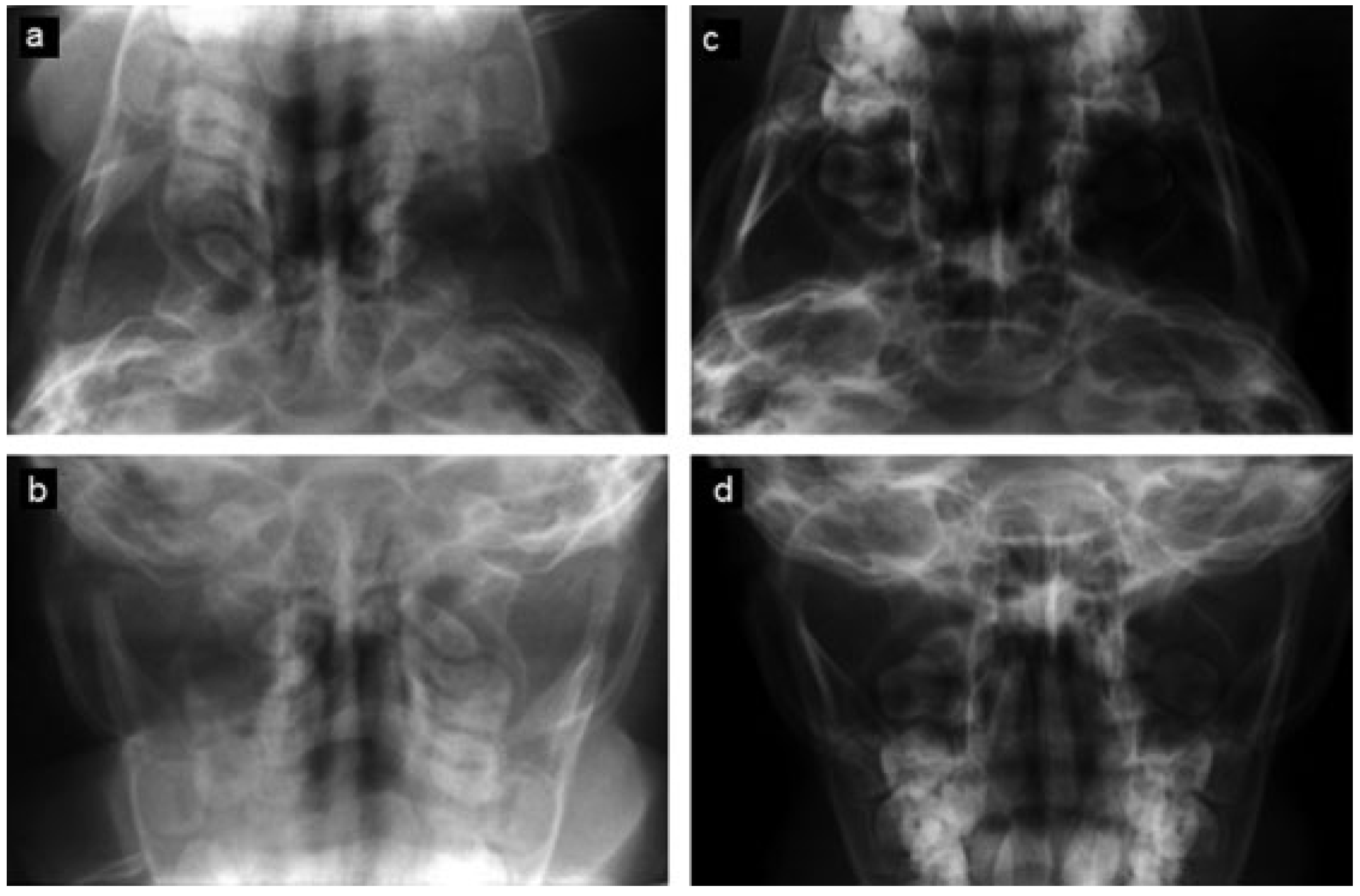
The third patient was an 18-month-old male patient who fell out of his crib and sustained bilateral subcondylar fractures and was allowed to continue bottle feedings and use of a pacifier. A Towne view radiograph documented normal condylar anatomy and position at age 5 (
Figure 5). He returned at the age of 16 for third molar removal. At that time, he exhibited class I dental and skeletal occlusion and no history or physical findings of myofascial or TMJ symptoms.
Discussion
Condylar fractures can be considered as a protective mechanism; protecting the brain in the event of major anterior– posterior mandibular impact. A limited portion of the glenoid fossa is formed by thin bone, but the condylar head is larger than this thinned area. The impact almost always causes the relatively thin and weak condylar neck to fracture first, preventing intracranial displacement [
9].
Treatment of condylar fractures is controversial. Surgical reduction and internal fixation should be considered when (1) the occlusion cannot be predictably reestablished because of severe malposition of the fractured condylar segment, (2) the fractured segment is displaced into the middle cranial fossa, (3) a foreign body is present, (4) instability of the occlusion is present, or (5) other patient factors, such as noncompliance and uncontrolled seizure disorders that could limit the success of a nonsurgical approach [
1,
8]. Although justified controversy still exists, closed treatment is generally accepted as a highly successful, proven, and effective treatment option. Surgical reduction is commonly associated with significant morbidity [
2]. These include facial nerve damage, hypertrophic scar formation, intraoperative hemorrhage, and vascular compromise to the proximal segment, which loses a significant amount of its periosteal blood supply [
3]. Instability of the repositioned condyle with loss of skeletal fixation can also occur [
10].
Successful treatment outcome criteria include a return to the preinjury occlusion, normal jaw opening, pain-free joint function, symmetry of the mandible, and minimal surgical morbidity [
2]. Exact anatomical repositioning is not always required for a satisfactory result as demonstrated by our second patient [
11]. In general, the treatment with favorable risk/benefit ratio should be the treatment of choice [
12].
With closed reduction treatment the amount of displacement of the condylar fragments dictates the amount of adaptations necessary to maintain normal occlusal relationship [
13]. These adaptations are neuromuscular, skeletal, and dentoalveolar. Neuromuscular adaptation in the muscles of mastication keeps normal occlusion. However, most patients do not develop adequate neuromuscular adaptations to allow maintenance of a normal occlusion and require assistance in the form of guiding intermaxillary elastics as demonstrated in two of our three patients. The dentoalveolus may respond/adapt by extrusion of the anterior teeth and/or intrusion of the posterior teeth [
13]. In all of our patients, significant reformation and repositioning of the fractured condyle segments occurred as documented by our long-term posttrauma imaging.
It has been shown that a certain magnitude of skeletal remodeling takes place in the proximal segment after a condylar fracture. This is more evident in younger children with complete return to normal skeletal relations, the so called “restitutional remodeling,” as seen in radiographs from our pediatric patient treated for displaced condylar fractures. This is less predictable in teenagers and happens through only minor remodeling in adults, where healing occurs by “functional remodeling.” In our other patients this functional remodeling was quite significant.
Moreover, experimental evidence shows that the glenoid fossa grows downward and becomes shallow to adapt to the new position of the condyle [
14]. These adaptations likely allow the functional success of nonsurgical treatment in most adults [
13]. In fact, this remodeling through downward growth and increased shallowness of the glenoid fossa is evident in the 14-year-old female patient (
Figure 1), but only to a much lesser degree in the 21-year-old male patient (
Figure 3).
There is controversy in the reported literature as to the type of treatment preferred for displaced condylar fractures. As a result, surgeons may be averse to conservative treatment of such cases. The severity of displacement of the fractured condyle is not necessarily a contraindication for closed treatment as demonstrated by our patients [
3,
15,
16,
17].
Current literature shows that with closed treatment of a fracture of the head, neck, or subcondyle, the TMJ remodels to form a functional articular process with satisfactory long-term results. Outcomes of closed treatment of condylar fractures have been studied extensively with respect to function using plain film radiography, but not tomography and 3D imaging [
2,
8,
14,
18,
19]. Our study presented two patients illustrating the extensive remodeling after trauma with the aid of 3D reconstructed CT imaging to demonstrate the successful functional treatment of displaced condylar fractures. Another case of remodeling and repositioning was documented in the pediatric patient through plain film radiographs. The treatment protocol included approximately 6 weeks of guiding elastics physiotherapy, allowing continuous limited jaw motion and a soft diet, and all patients attained satisfactory functional results.
Note
There are no sources of financial support to be reported.