Though extensive literature on the management of orbital floor fractures is available, literature on medial wall fractures is scarce, reflecting the difficulties in the treatment of these particular injuries due to the limitations of conventional approaches, difficult manipulation of orbital contents, and limitation of autogenous and alloplastic materials in restoring the complex 3D anatomy of the medial orbital wall, in particular when associated with concomitant orbital floor fractures.
Although these reports seem to overcome the lack of consensus on the ideal approach and materials that can be used for the repair of fractures of the medial orbital wall, treatment of these fractures is still challenging.
This study aims to retrospectively evaluate the outcomes in the repair of medial orbital wall fractures (isolated or combined with orbital floor fractures) using a retrocaruncular approach and titanium meshes, comparing the placement of the titanium mesh with three different techniques: (1) conventional free hand under direct vision, (2) an endoscope assisted, and (c) a navigation system assisted.
Material and Methods
The present study includes 18 patients (age range, 20–74 years) surgically treated for medial wall orbital fracture (isolated or combined with orbital floor fractures) from 2010 to 2013 at the Division of Maxillofacial Surgery of the University of Turin, Turin, Italy.
Indication for surgical treatment was medial wall fracture (isolated or combined with orbital floor fracture) with defect size larger than 2 cm2 with evidence of soft tissue herniation into the defect, muscular entrapment with associated diplopia, and enophthalmos clinically evident (>2 mm).
An institutional review board approved the study. Inclusion criteria included (1) age older than 18 years at the time of surgery, (2) no other facial fractures associated, (3) complete pre- and postoperative clinical and medical records, (4) pre- and postoperative spiral multislice computed tomographic (CT) scan (0.625–1.0 mm slice thickness, (5) no history of previous orbital surgery, (6) surgical technique as described below, and (7) follow-up of at least 6 months. Patients who did not meet these criteria were excluded from the study.
Study variables include the following: patient demographics, etiology of the injury, fracture characteristics, visual acuity, and concurrent ocular injuries (
Table 1). Outcomes measures include the following: (1) pre- and postoperative diplopia severity score (rated on 0–3 scale,
Table 2); (2) pre- and postoperative globe position: clinical (normal or abnormal = residual clinically significant enophthalmos >2 m); (c) intra- and postoperative complications; (d) secondary operation rate; and (e) assessment of quality of orbital reconstruction on postoperative CT scan in terms of shape and volume (relationship between bony perimeter of the fracture and mesh limit, orientation, and shape of the implant listed as: satisfactory, anatomical, or almost anatomical reconstruction; good, minor defects not requiring reoperation; bad, requiring revision surgery).
The patients were classified in three groups based on the technique of implant placement: group 1 (CONV), conventional free hand under direct vision; group 2 (ENDO), with the assistance of an endoscope inserted through the transconj incision; group 3 (NAVI), operated with the assistance of a navigation system.
Surgical Technique
All patients were operated under general anesthesia within 10 days of the trauma. Preoperative antibiotics for sinus coverage (ampicillin with clavulanic acid) were given perioperatively for 6 days. Retrocaruncular incision and path of dissection as described by Grant and by AOCMF were used to gain access to the medial wall [
7,
8]. The bony perimeter of the fracture was isolated, with particular attention to the posterior bony ledge. In case of concomitant fracture of the floor, the medial retrocaruncular incision was extended to connect with a retroseptal transconjunctival incision in order to approach the fractured orbital floor. The medial and inferior dissections were joined to create a single dissection plane. The inferior oblique muscle was either disinserted from the bone just posteriorly the inferomedial rim with a periosteal elevator or divided with Stevens scissor to create “a panoramic corridor” to correctly access the entire medial wall and orbital floor [
4].
In isolated medial wall fractures, we used radial titanium orbital mesh (Synthes, Oberdorf, Switzerland) tailored and cut to fill the entire defect. In fractures involving both medial wall and orbital floor preformed, specifically designed matrix titanium orbital meshes were used (Synthes).
In combined fractures the medial wall portion of the preformed mesh was inserted first and the remainder of the plate was then rotated to reach the correct anatomic position.
In group 1 (CONV), the mesh was placed free hand under direct vision. In group 2 (ENDO), an endoscope 4 mm 0 degree (Karl Storz GmbH & Co KG, Tuttlingen, Germany), with video camera and monitor, was inserted into the retro-caruncular incision to allow better visualization of the surgical fields, thanks to magnification and high-intensity cool light. The endoscope was used to check the completed dissection of the bony margin and to verify clear identification in particular of the posteromedial ledge of the fracture in direction of the orbital apex. The endoscope was then retracted and used again to check the correct seating of the titanium mesh, in particular to verify that the mesh properly and passively reaches the superior and posteroinferior margin of the fractures. In group 3 (NAVI), a navigation system (BrainLab) was used for computer-assisted preoperative planning with virtual reconstruction and intraoperative control of virtual orbital contours, as described by many authors [
9,
10,
11].
Mirroring of the unaffected orbit into the fractured side, a virtual template to simulate the ideal reconstruction was created. This template was navigated during surgery, and navigation was used both to verify the posterior ledges of the fracture and the position and shape of the implant relative to the correct anatomic position of the native bone.
The mesh was fixed with two monocortical screws to the inferior orbital rim. Forced duction testing was done to confirm normal ocular mobility. The conjunctiva was closed with few interrupted 5.0 Vicryl rapid sutures.
Results
The present study includes 18 patients (13 men and 5 women) with their age range 20 to 74 years. Two patients were excluded from the study because of incomplete postop records and imaging. Etiology of the fracture was interpersonal violence in 11 patients, fall in 1 patient, sport accident in 2 patients, and motor vehicle (road) accident in 2 patients.
Isolated orbital fractures were present in 8 patients, combined medial wall/floor fractures in 10 patients. Radial orbital mesh was used in isolated medial wall fractures, and preformed orbital mesh plates were used to treat combined medial wall/floor fractures.
No intra- or postoperative complication was registered. The minimum follow-up was 6 months.
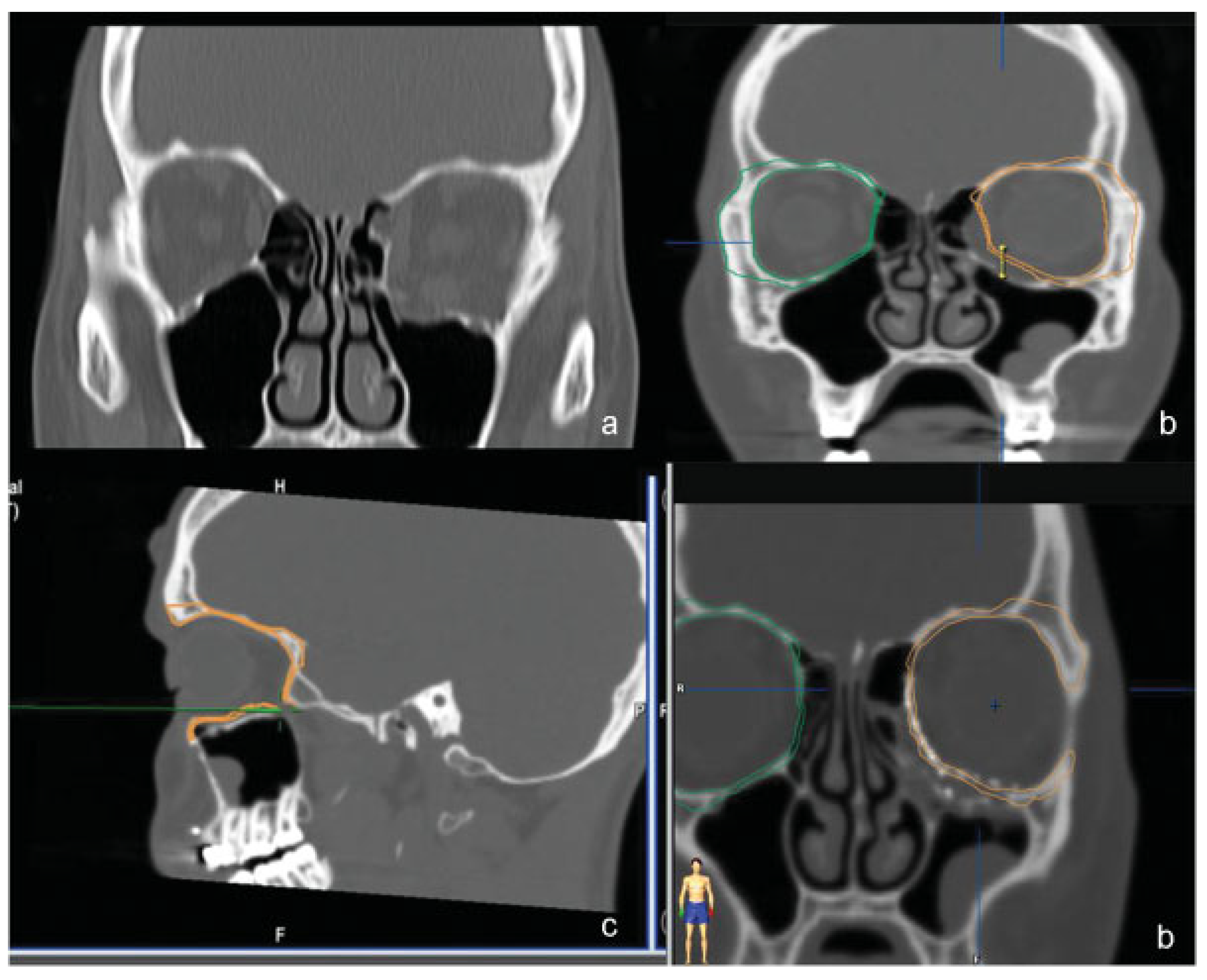
The outcomes measures are summarized in
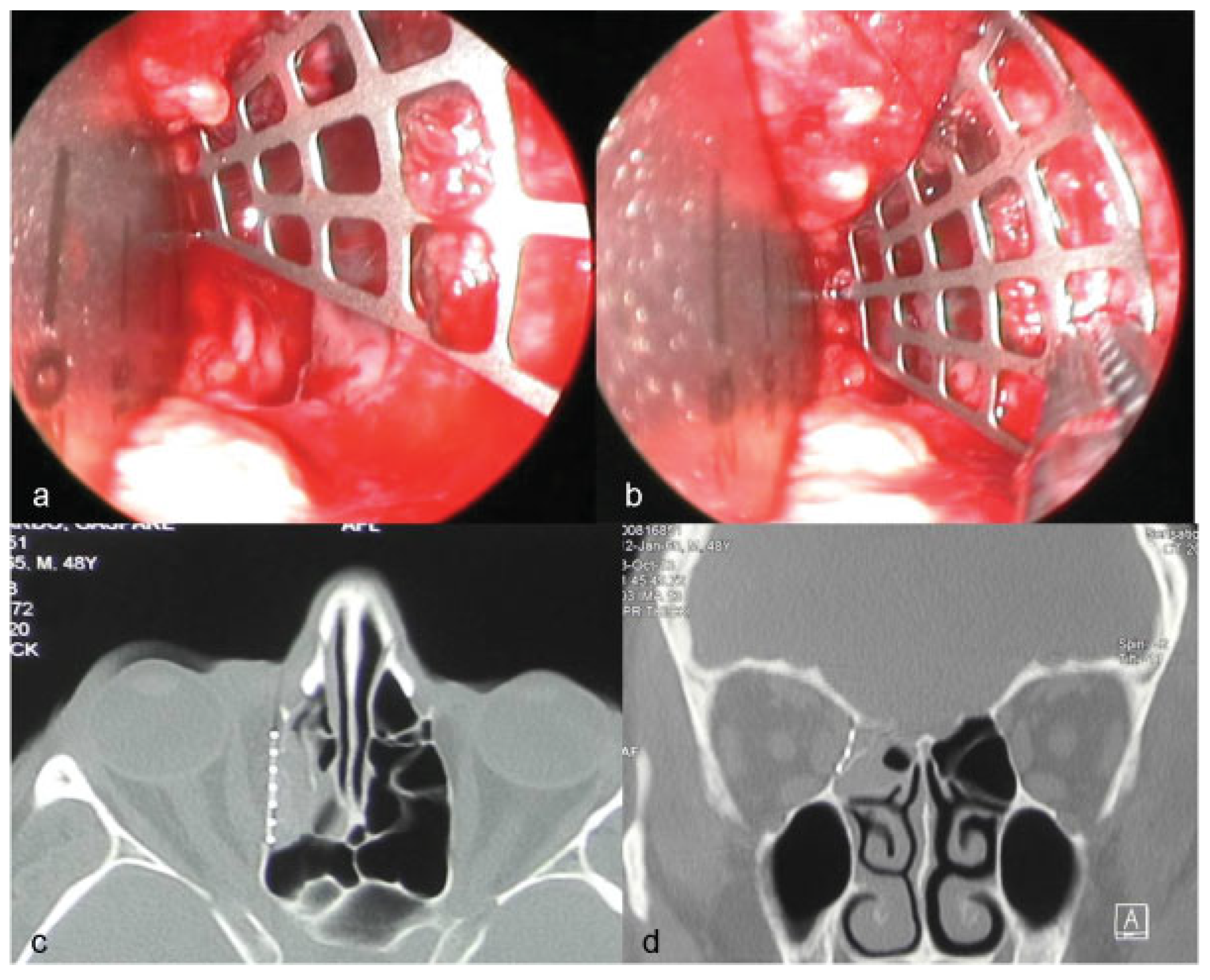
Table 3. The quality of orbital reconstruction was assessed as satisfactory in 12 cases, good in 4 cases, Unsatisfactory in 2 cases. In particular in group 1 (CONV) in four of eight patients, the posterior ledge of the fracture was not reached by the implant (
Figure 1a), and in one patients in group 1 the mesh hinged toward the ethmoid (
Figure 1b). In group 3 (NAVI) in one of five patients, the posterior ledge of the fracture was not reached.
In two patients reoperation was indicated. One patient was reoperated with satisfactory results, and one refused the intervention because no functional deficit was evident.
Discussion
The goal in repair of severe orbital fracture is the recovery of undisturbed function and preinjury globe position.
Since the 1980s, Manson showed that the cardinal principles for successful orbital reconstruction are the restoration of preinjury anatomical shape and volume, with concomitant liberation and repositioning of prolapsed orbital soft tissue [
12]. The crucial technical steps, which constitute fundamental Manson’s legacy for a successful orbit operation include (1) wide and complete exposure with careful subperiosteal dissection of the fracture bony margins and (2) anatomical reconstruction of the shape and contour of the orbital walls. The complex soft tissue and bone anatomy of the medial orbit makes much more difficult to accomplish these steps for the medial wall fracture in comparison to the more common orbital floor fracture.
In orbital medial wall fractures, the first challenge is exploration and identification of the posteromedial ledge of the fracture, which is proximal to the orbital apex and pertinent vital orbital structures.
Visualization of the posteromedial orbit is very difficult with conventional transcutaneous access because medial canthal tendon insertion and lacrimal system must be preserved. Moreover, visible scar of medial transpalpebral incision is another important limiting factor in treatment of these fractures. The coronal flap allows panoramic exposure of the medial wall but presents unfavorable benefit/risk balance in terms of morbidity and time consumed for isolated fracture of the medial wall [
4].
In addition to the proper exposition challenge, the surgeon must face a second technical difficult challenge in medial wall fractures, which is anatomical reconstruction.
Because the orbit modifies its shape from quadrangular pyramidal to conical in the posterior third, this corresponds to a distinct bony convergences profile in the posteromedial region, where the orbital floor inclines superiorly to meet the medial wall. In combined medial wall and floor fractures, in particular when the inferomedial orbital strut is involved, reconstruction of this unique 3D anatomy requires the replication of slopes and curves with difficult sizing and shaping of the implant [
3].
Recently, few papers [
3,
4,
7], combining transconjunctival retro/transcaruncular approach with the use of prebent titanium or porous polyethylene/titanium meshes and implants, reported excellent results in the treatment of medial wall fractures (isolated or combined with orbital floor fractures).
The trans- and the retrocaruncular incisions provide excellent exposure of the medial orbit without external visible scar [
13].
In case of association of a medial wall fracture with an orbital floor fracture, the retrocaruncular incision can easily be extended laterally in the inferior conjunctival fornix with a retroseptal incision, resulting in a transconjunctival C-shaped incision.
In this situation it is necessary to disinsert the inferior oblique muscle to expose beautifully the entire surgical field creating a panoramic corridor between the medial wall and the floor of the orbit and to gain adequate access to insert and anatomically position a two-wall implant.
In this case series we either stripped the muscle with a periosteal elevator from its origin or divided it with Stevens scissor and reapproximated at the end of the operation. It has been reported that following inferior oblique muscle disinsertion or myotomy, patients can develop a pseudo-Brown syndrome, characterized by a limitation of ocular elevation in adduction and a consequent torsional diplopia [
14].
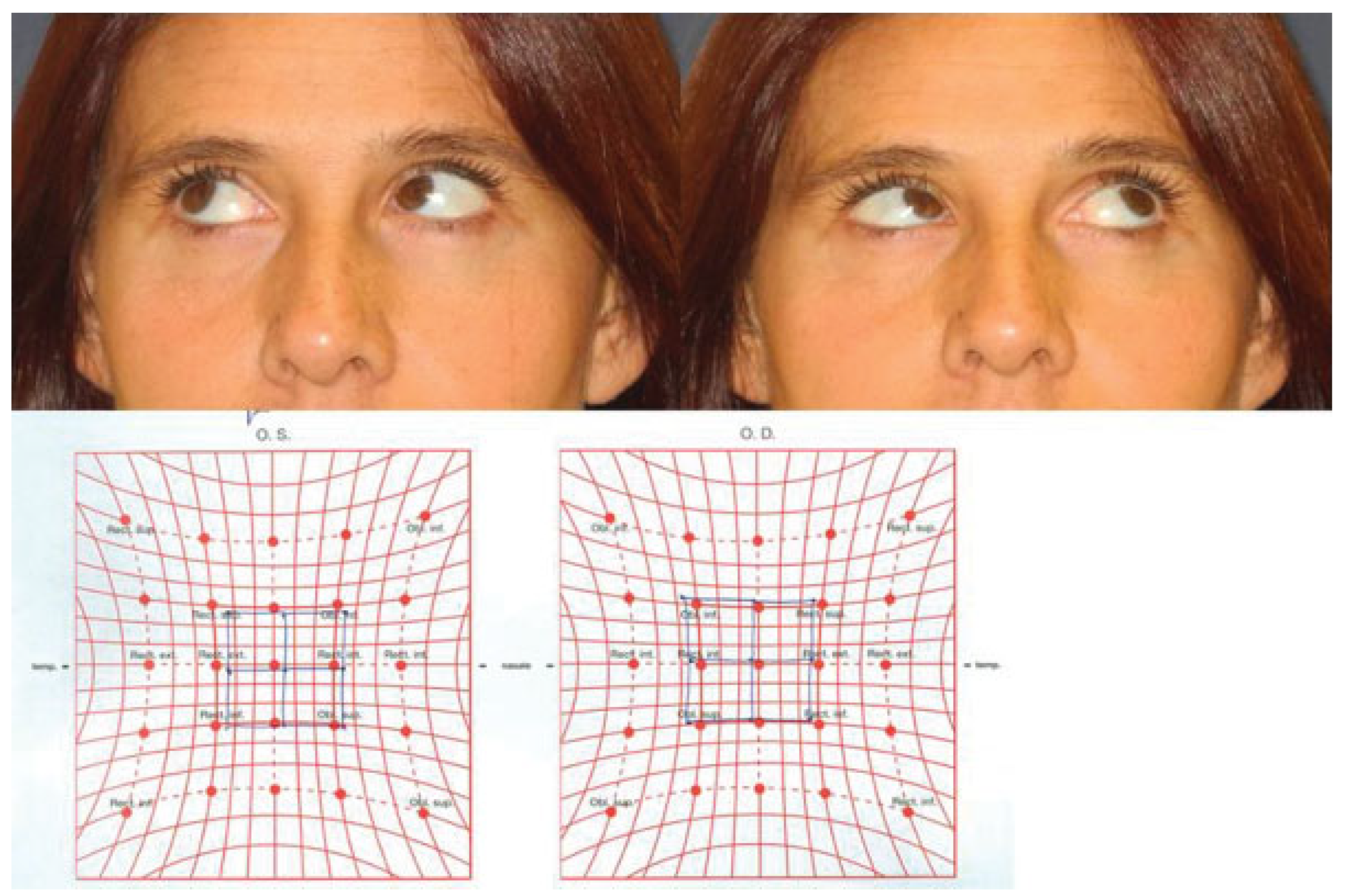
In our series 2 of 10 patients (
Figure 2) who underwent detachment of the inferior oblique muscle developed a diplopia in the extreme lateral upgaze. This is a nonhandicapping diplopia, which did not affect patients’ everyday life and it was found only after orthoptic examination at the end of follow-up.
We do feel that patients should be informed before surgery of this possible limited functional impairment, but this does not alternate the balance benefits/risks when using this C-shaped incision for medial wall/floor-combined fractures.
In our experience, complete and clear visualization of the posteromedial ledge of the fracture, when the defect reaches superiorly the posterior ethmoidal vessels and inferiorly along the inferomedial strut in direction of the apical region, becomes increasingly difficult due to the difficult manipulation of prolapsed orbital soft tissue.
In our case series, in group 1 (CONV), 4 of 10 implants did not reach the posterior ledge, whereas 1 prebent implant had a wrong angulation hinging toward the ethmoid.
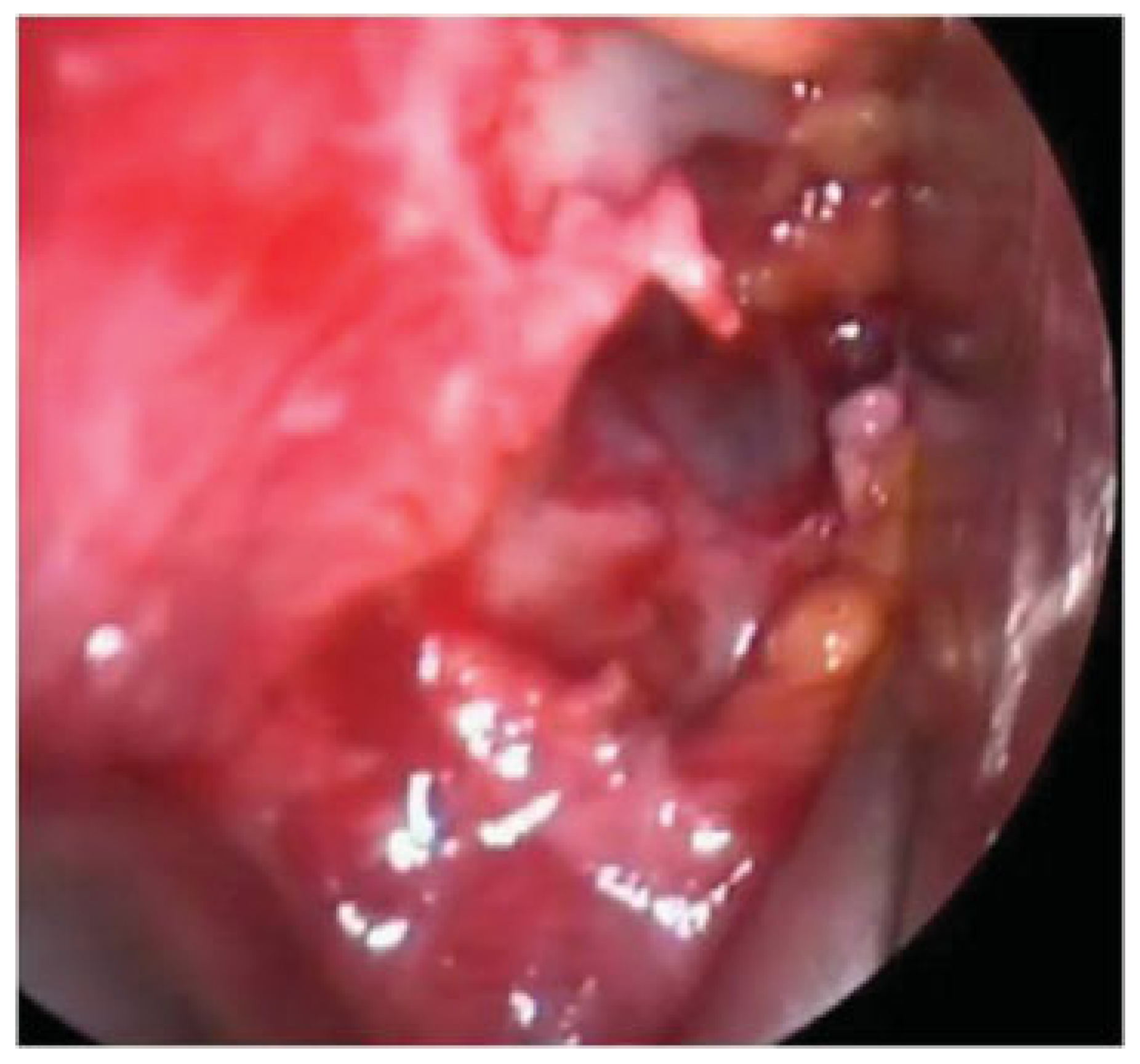
Introducing an endoscope through the incision, as described by Chen and Davies [
3], Meningaud et al. [
5], and Woo et al. [
6], facilitates the visualization of the margin of the fracture (
Figure 3) and allows a precise control of the spatial relationship of the implant margins and fracture perimeter (
Figure 4).
In our series, endoscope assistance proved to be very helpful because of high-intensity cool light and image magnification. It is also very helpful for medical education in surgical anatomy for young residents.
In the group 2 (ENDO) the quality of orbital reconstruction has significantly improved, with the totality of implants correctly placed (
Figure 5).
Endoscope-assisted surgery, as performed in our study, is a completely different procedure from pure transnasal endoscopic medial wall fracture treatment.
It does not need technical skills, time, and specific instrumentation required for transnasal endoscopic surgery.
Moreover, transnasal endoscopic treatment of medial wall fracture relies on indirect fracture reduction through a narrow and tortuous pathway. The transnasal completely endoscopical approach is reserved for isolated fracture with a simple shape. In larger and more complex defects, we feel that direct vision and control are required for proper placement and fixation of larger implants in terms of shape and contour [
15].
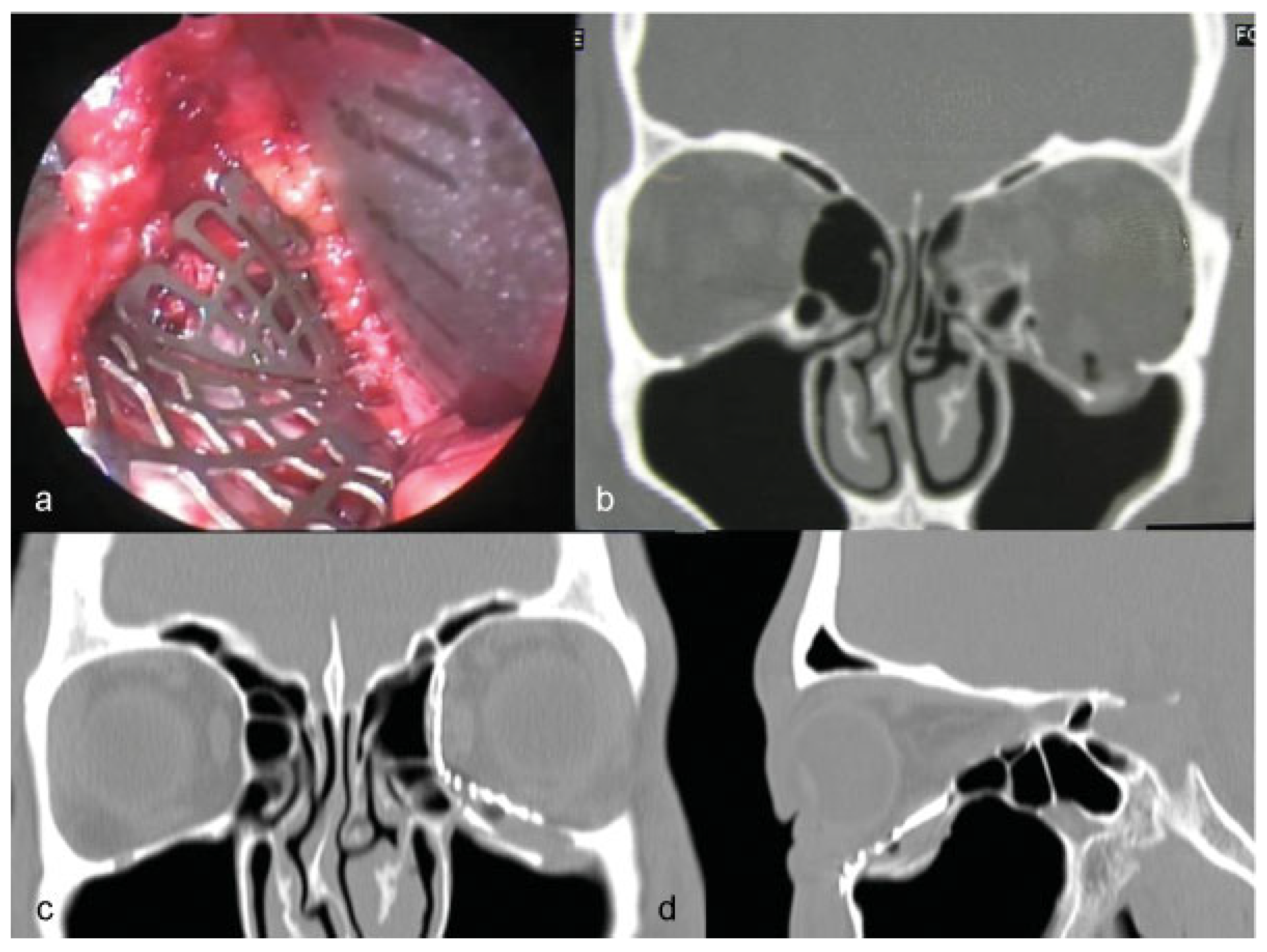
In group 3 (NAVI), navigation-assisted orbital reconstruction was performed. At the time of surgery, navigation was used to assess the accuracy of dissection confirming that we have reached the posterior ledges of the fracture and the position and shape of the implant, according to virtual planning (
Figure 6).
In our study, navigation-assisted orbital reconstruction is reliable in restoring orbital shape and volume. We totally agree with Markiewicz et al. [
11] and Bly et al. [
9] that navigation-aided surgery improves outcomes in complex orbital reconstruction.
Our reoperation indication rate 2/18 is consistent with literature, as Cho reports an 18% of second intervention necessary.
Nonpreformed radial plates were used for isolated medial wall fractures and required accurate bending, sizing, and trimming to reduce interferences with surrounding soft tissues. In combined medial wall/floor fractures, preformed titanium meshes were used. Recent studies have shown that this 3D prebent anatomical titanium plate, made using contour-averaged CT data from human orbits, allows for precise reconstitution of the original anatomy of combined fractures of medial wall and floor of the orbit [
16].
This study reports some inherent limitations. We reported data obtained from a retrospective cohort and the sample size is small. These data, even if all the surgical operations were made under the supervision of the senior author (G.G.), were collected in different stages of the learning curve of the operating surgeon.
The diplopia severity scoring system and the clinical evaluation of globe projection may content possible reporting bias in their determination due to the operator. However, clinical assessments were by the same surgeon in all cases.
In conclusion this study confirms that the use of titanium orbital mesh plates placed through a transconjunctival retrocaruncular approach allows for safe and accurate orbital reconstruction in patients with medial wall fractures (isolated or combined with orbital floor fractures). The use of endoscopic assistance through the surgical incisions improves accuracy of treatment allowing better visualization of the posterior ledges of the fractures. Navigation-aided surgery is a reliable technique for complex orbital reconstruction after trauma and has the potential to improve predictability and outcomes in orbital repair.
Financial Disclosure and Products
None of the authors has a financial interest in any of the products or devices mentioned in this article.