Hemifacial microsomia (HFM) is a chromosomal abnormality with an incidence of 1:5,600. Bone grafting, alloplastic grafting, orthognathic surgery, orthomorphic surgery and distraction osteogenesis (DO) are the various options available for the management of HFM. DO has been used for the correction of the mandibular corpus length and ramal deficiency, but there is no previous report stating its use in increasing the height of the mandible [
1]. Basal osteotomy of the mandible has been reported for reduction of the height of the mandible and advancement of the mandibular corpus [
2]. We present a method incorporating the basal osteotomy with the principles of DO to correct hemimandibular hypoplasia associated with HFM type I.
Case Report
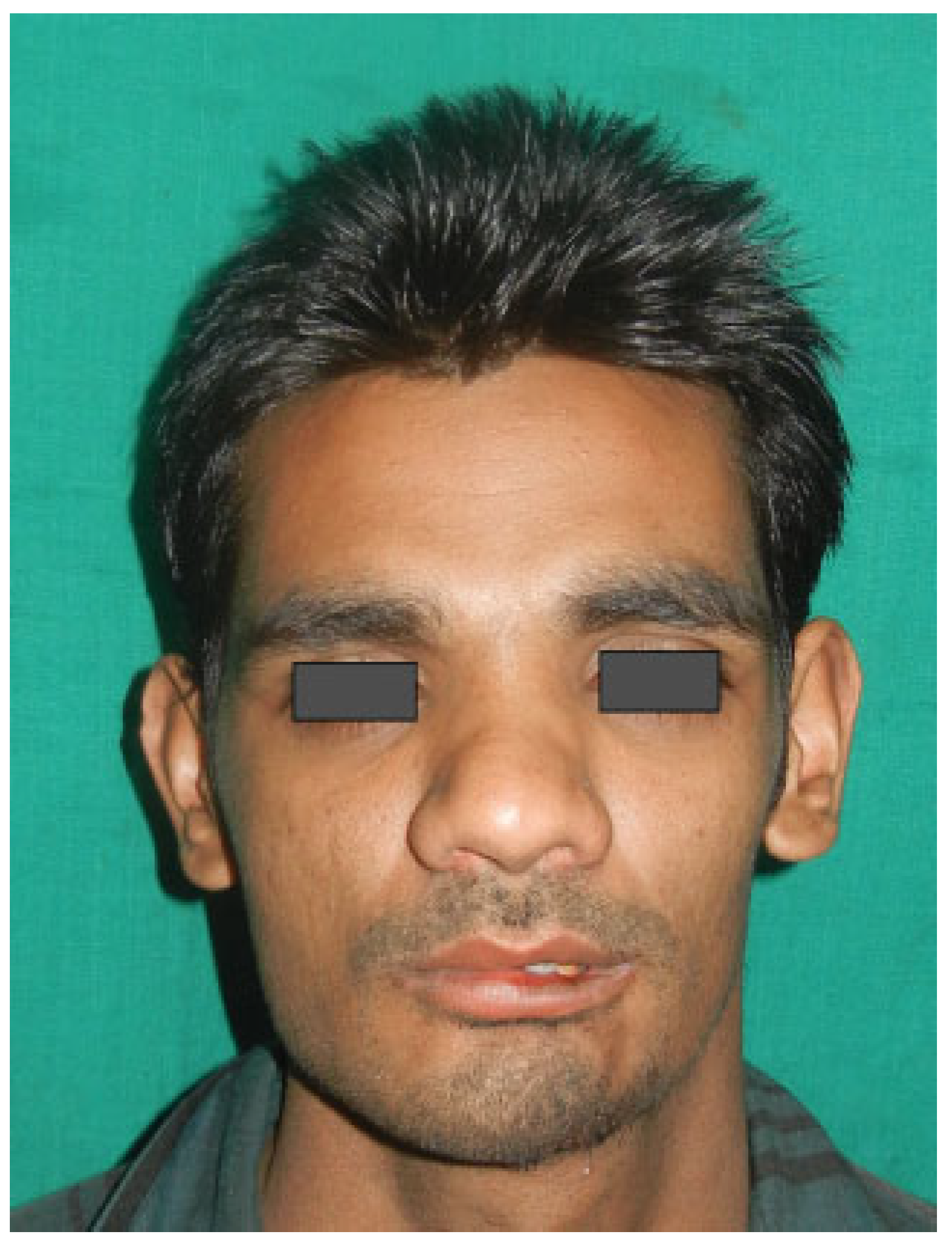
A 20-year-old male patient presented with a chief complaint of asymptomatic asymmetry of the face first noticed in the childhood that worsened over the period of time. He has no history of trauma or major hospitalizations. He presented with gross asymmetric face with decreased lower facial height on the left side. The chin was deviated to the right side (
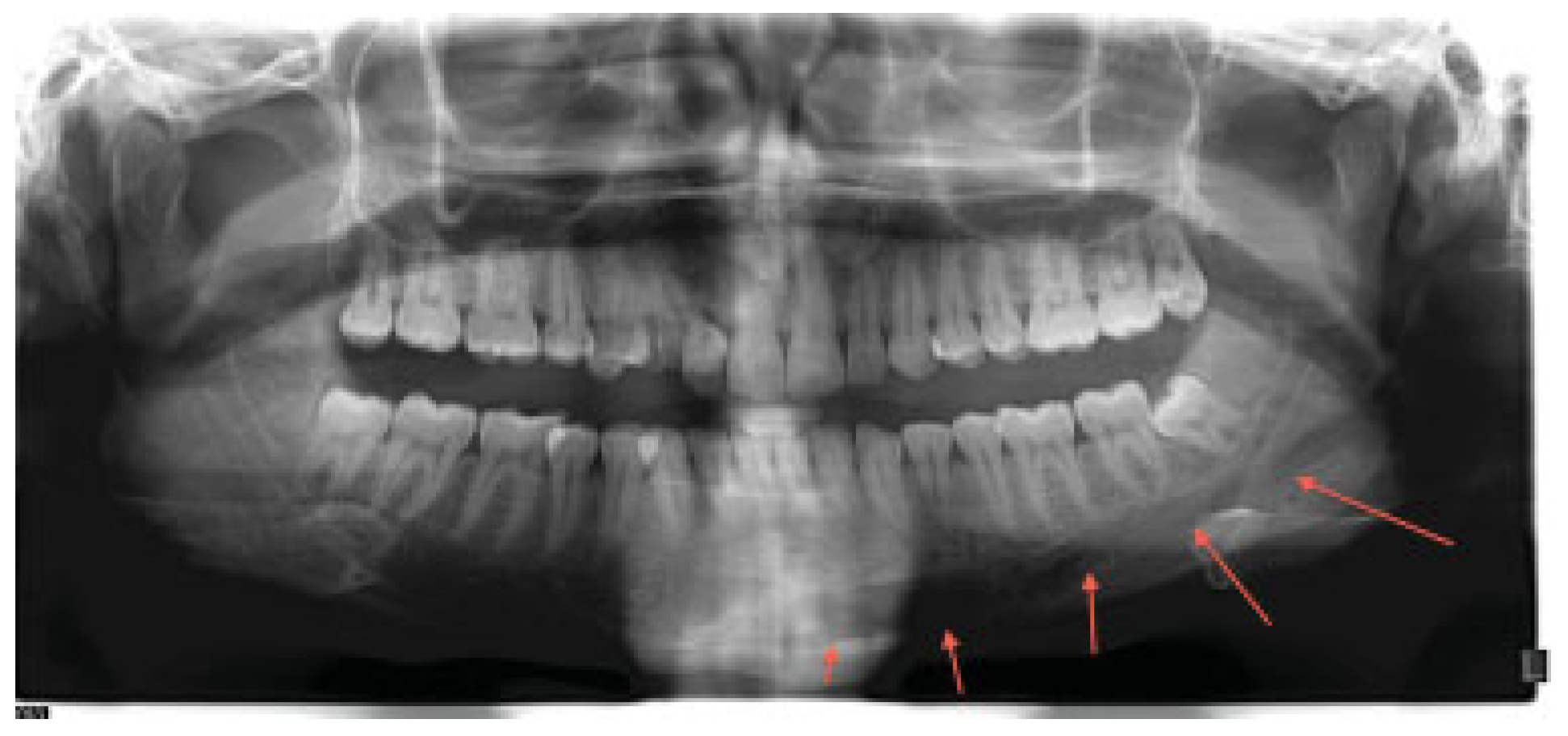
Figure 1). On temporomandibular joint (TMJ) evaluation, jaw movements were normal bilaterally. On orthopantomograph (OPG), the mandible on the left side was smaller in size with maintained anatomy. Condyles were symmetrical, and teeth were symmetrical which was reconfirmed using study models.
Audiometry revealed decreased hearing capability on the left side. No cardiac abnormalities, no abdominal, or visceral abnormalities were noted. An IQ score of 86 was obtained on Stanford-Binet Intelligence scale suggesting low average. The condition was diagnosed as asymmetry secondary to mandibular hemihypoplasia associated with HFM type I.
Discussion
Cohen has explained the biological basis of asymmetries, which are divided into asymmetric embryopathies, common asymmetries, hemiasymmetries, craniosynostoses, and hamartoses [
3]. Asymmetry may result from alteration in one tissue such as bone with secondary regional consequences or multiple tissues on a primary basis [
4]. In this case, only bony involvements with secondary regional changes were seen.
Hemifacial hypoplasia is heterogenic in nature associated with chromosomal abnormalities and environmental causes such as thalidomide, primidone, and retinoic acid administered during pregnancy, infants born to diabetic mothers [
5]. Poswillo proposed that the pathogenesis was based on embryonic hematoma formation arising from the anastomosis that precedes formation of the stapedial artery stem [
6]. Severity of the deformity depends on size and extent of hematoma formation.
Conventional orthognathic surgery and bone grafting form the main stay in the correction of type I asymmetric faces. Usual combinations include Le Fort I osteotomy for occlusal cant corrections and maxillomandibular horizontal and vertical positioning, concomitant mandibular bilateral sagittal split osteotomy or bilateral vertical ramus osteotomy or an ipsilateral vertical ramus osteotomy with contralateral sagittal split osteotomy [
7]. HFM type I deformity without occlusal cant deformity can be corrected with orthomorphic surgery as suggested by Salins et al. [
8] or augmentation of the mandible using alloplastic materials. In types II B and III HFM requiring
TMJ rehabilitation and bony material replacement, the combination of the conventional orthognathic surgeries with costochondral and iliac crest grafts or alloplastic reconstructive materials are used to reconstruct the ramus condyle unit [
7]. With the evolution of DO, large segments of jaws can be grown to regenerate the lost bone and to attain good cosmesis [
1].
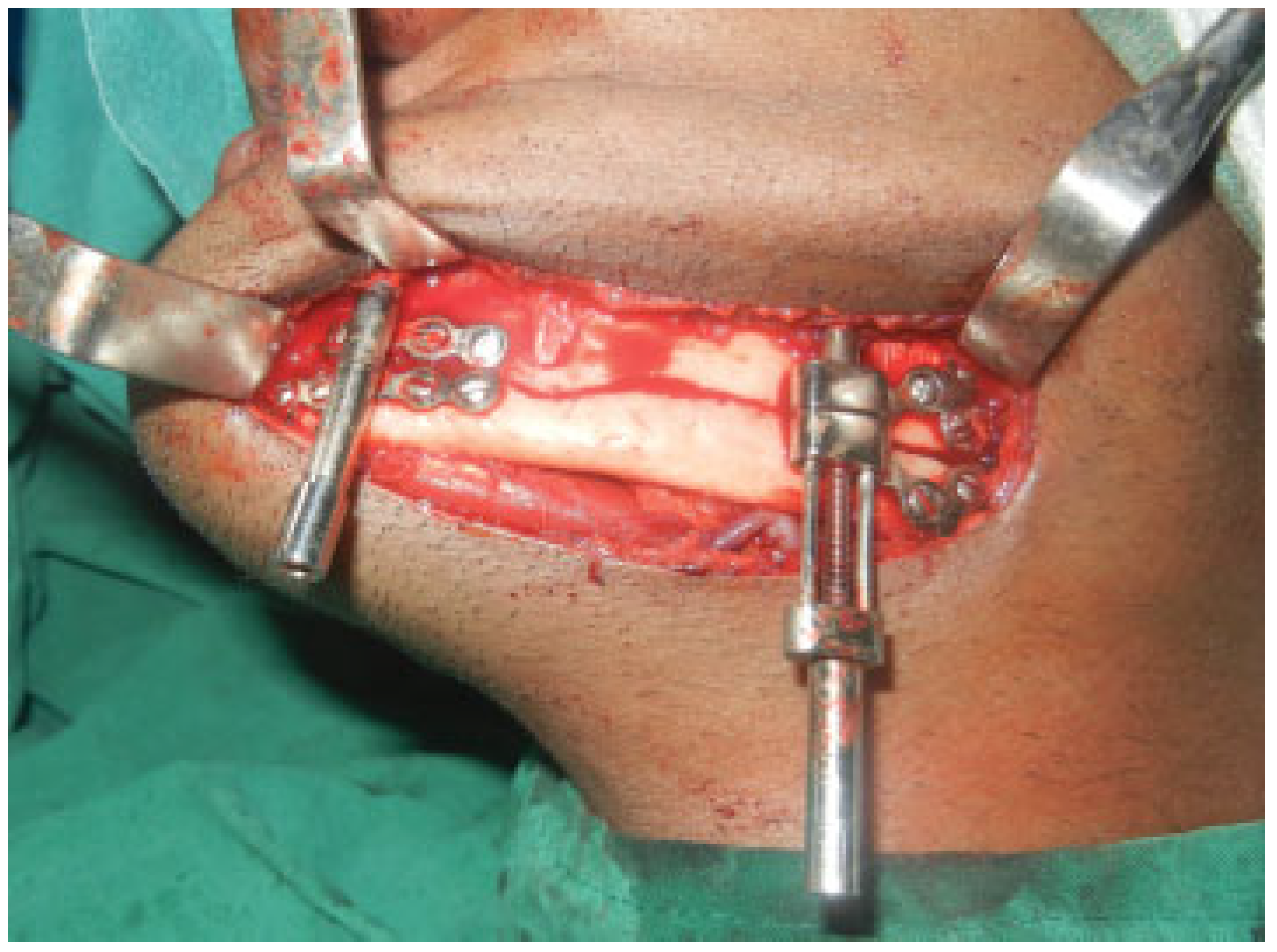
Lopez et al. [
2] suggested mandibular basal osteotomy correction of deficiency, excess, and/or asymmetry of the inferior mandibular border. So, we incorporated the basal osteotomy with the principles of DO using the D1 and D2 to increase the height of the mandible.
The advantage of the technique over the classic orthognathic and distraction methods involves the fact that the occlusion is never disturbed in this method. Our patient was encouraged to start oral diet at the earliest without any deleterious effects. However, the limitation of the procedure is that it cannot be used in a case with severe occlusal cant, which needs to be corrected with bimaxillary surgery.
Complications of the procedure anticipated were inferior alveolar nerve injury, marginal mandibular nerve injury, scar, bad split, incomplete osteotomy, injury to submandibular salivary gland. However, good surgical technique can help avoid the same. Inferior alveolar nerve repositioning was done when the osteotomy was completed and the resultant paresthesia was present for 5 weeks following which the neural function returned. Marginal mandibular nerve was not injured during the procedure, scar caused by the exit wound was treated by Z plasty, no other complications occurred during the procedure. In this technique, we preferred an external approach because the mobile lower segment of the mandible was intended to be distracted away using the fixed superior border as an anchorage. Our main concern was that intraoral placement might risk the contamination from oral fluids. So, the distractor was placed through an external approach. Though the lower border of the mandible has less cancellous bone between the buccal and lingual cortical plates, the regenerate formed was healthy and shows good ossification after consolidation.
Autologous fat grafting and rhinoplasty procedures were ancillary procedures for finer refinement of the cosmesis of the patient. Basal osteotomy of the mandible and DO is a feasible option in the treatment of mandibular asymmetries without affecting the occlusion.