Medial Wall Fracture and Orbital Emphysema Mimicking Inferior Rectus Entrapment in a Child
Abstract
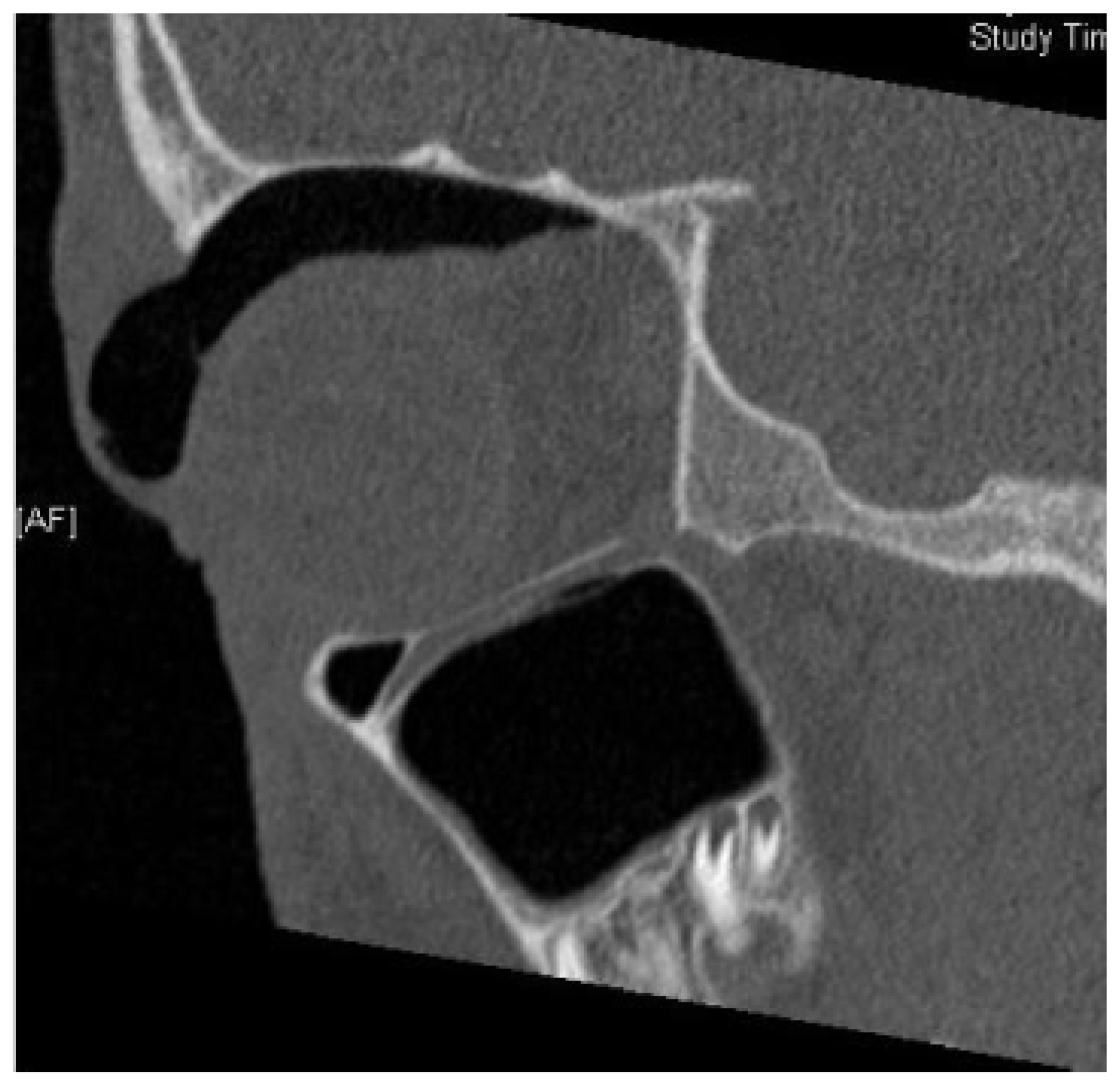
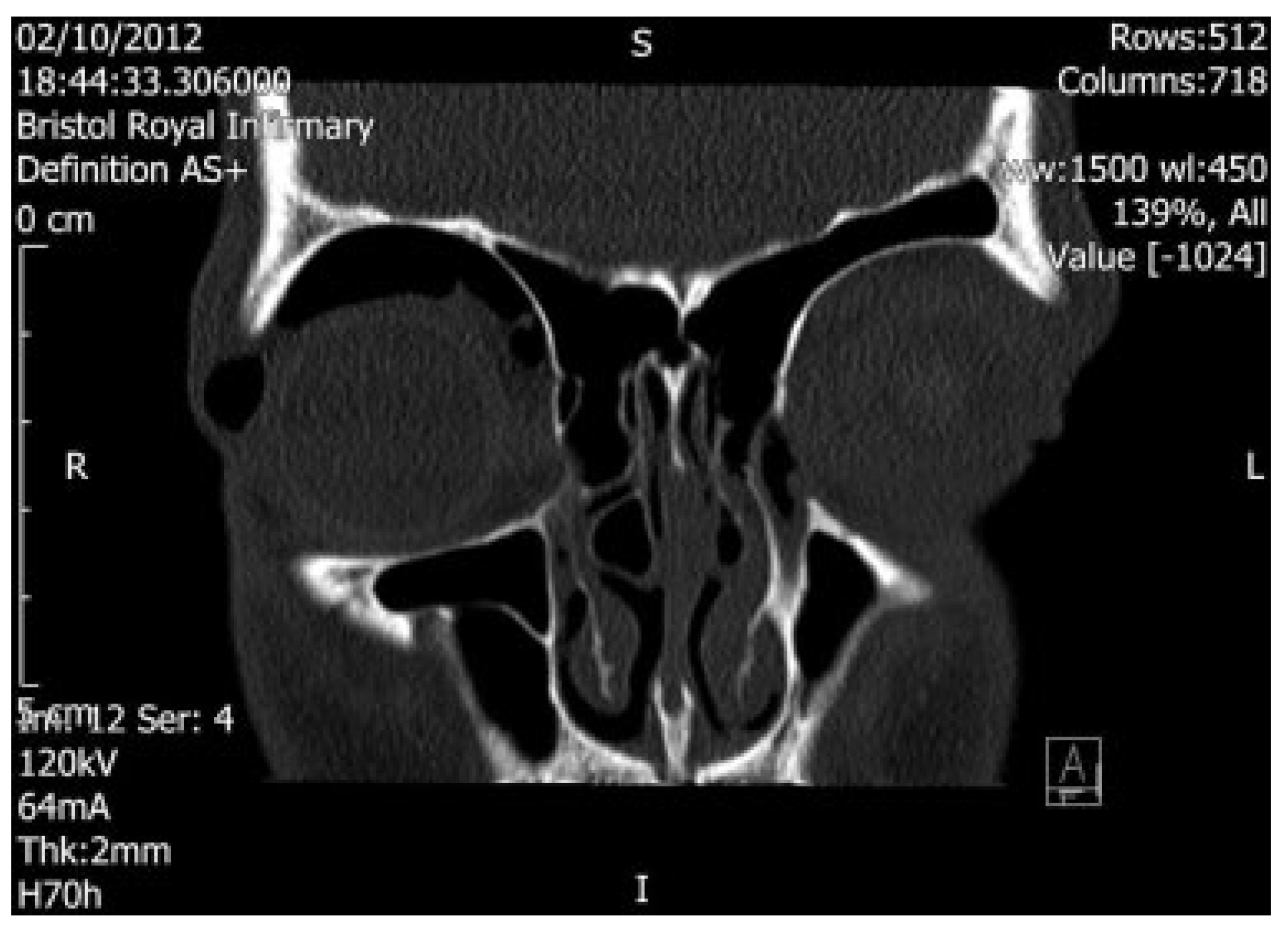
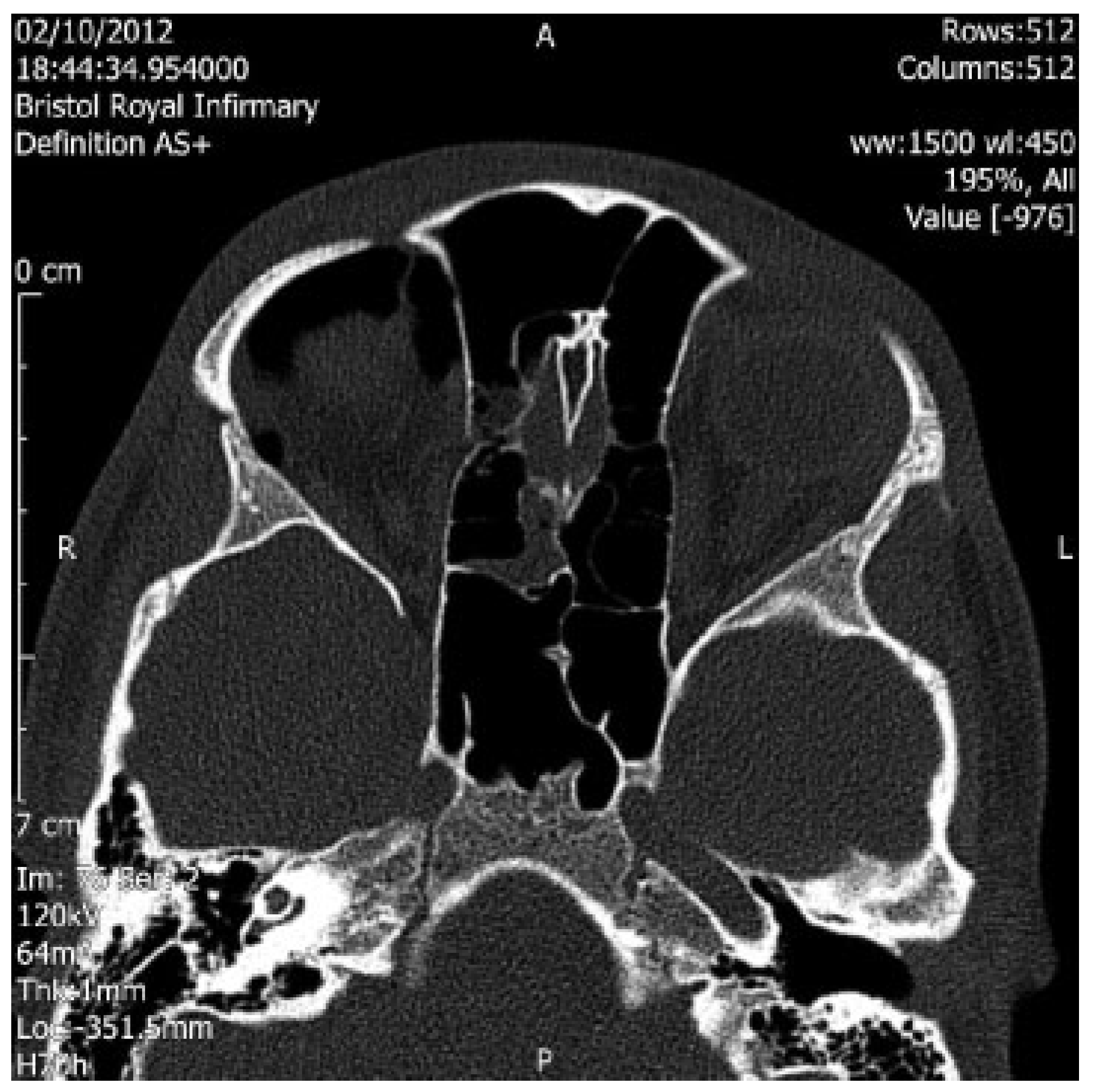
:Case Report
Discussion
Conflicts of Interest
References
- Lloyd, G.A. Orbital emphysema. Br J Radiol 1966, 39, 933–938. [Google Scholar] [CrossRef] [PubMed]
- Furlani, B.d.e.A.; Diniz, B.; Bitelli, L.G.; Martins, E.N. Sight-threatening orbital emphysema after nose blowing: case report [in Portuguese]. Arq Bras Oftalmol 2009, 72, 251–253. [Google Scholar] [CrossRef] [PubMed]
- Hunts, J.H.; Patrinely, J.R.; Holds, J.B.; Anderson, R.L. Orbital emphysema. Staging and acute management. Ophthalmology 1994, 101, 960–966. [Google Scholar] [CrossRef] [PubMed]
- Linberg, J.V. Orbital compartment syndromes following trauma. Adv Ophthalmic Plast Reconstr Surg 1987, 6, 51–62. [Google Scholar] [PubMed]
- Harmer, S.G.; Ethunandan, M.; Zaki, G.A.; Brennan, P.A. Sudden transient complete loss of vision caused by nose blowing after a fracture of the orbital floor. Br J Oral Maxillofac Surg 2007, 45, 154–155. [Google Scholar] [CrossRef] [PubMed]
- Dobler, A.A.; Nathenson, A.L.; Cameron, J.D.; Carpel, E.T.; Janda, A.M.; Pederson, J.E. A case of orbital emphysema as an ocular emergency. Retina 1993, 13, 166–168. [Google Scholar] [PubMed]
- Singh, M.; Phua, V.M.; Sundar, G. Sight-threatening orbital emphysema treated with needle decompression. Clin Experiment Ophthalmol 2007, 35, 386–387. [Google Scholar] [CrossRef] [PubMed]
- Burt, B.; Jamieson, M.; Sloan, B. Medial wall fracture- induced pneumo-orbita mimicking inferior rectus entrapment. Am J Emerg Med 2010, 28, 119.e1–119.e3. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the author. The Author(s) 2015.
Share and Cite
Collin, J.; Afshar, F.; Thomas, S. Medial Wall Fracture and Orbital Emphysema Mimicking Inferior Rectus Entrapment in a Child. Craniomaxillofac. Trauma Reconstr. 2015, 8, 345-347. https://doi.org/10.1055/s-0034-1399802
Collin J, Afshar F, Thomas S. Medial Wall Fracture and Orbital Emphysema Mimicking Inferior Rectus Entrapment in a Child. Craniomaxillofacial Trauma & Reconstruction. 2015; 8(4):345-347. https://doi.org/10.1055/s-0034-1399802
Chicago/Turabian StyleCollin, John, Farid Afshar, and Steven Thomas. 2015. "Medial Wall Fracture and Orbital Emphysema Mimicking Inferior Rectus Entrapment in a Child" Craniomaxillofacial Trauma & Reconstruction 8, no. 4: 345-347. https://doi.org/10.1055/s-0034-1399802
APA StyleCollin, J., Afshar, F., & Thomas, S. (2015). Medial Wall Fracture and Orbital Emphysema Mimicking Inferior Rectus Entrapment in a Child. Craniomaxillofacial Trauma & Reconstruction, 8(4), 345-347. https://doi.org/10.1055/s-0034-1399802


