Hard palate tumors may arise in the midline without affecting the alveolar ridge. In this cases a Brown class IA maxillectomy must be performed to carry out the tumor resection, preserving the dental arcade and therefore achieving better functional results [
1]. The way this maxillectomy is executed is variable depending on the tumor size and the surgeon’s preferences. In those tumors developing as endophytic masses with extension into the nasal cavity, it may be difficult to guarantee a deep tumor-free margin if the resection is made through a palatine approach. In this situation, a Le Fort I downfracture approach simplifies the surgical procedure improving the visualization of the entire tumor and the nearby structures, such as the descending palatine artery. In this manner, a complete tumor resection is guaranteed and the potential complications are reduced. At the same time, this procedure enables the reconstruction with a temporal muscle flap that otherwise could not be accomplished in a dentate patient [
2].
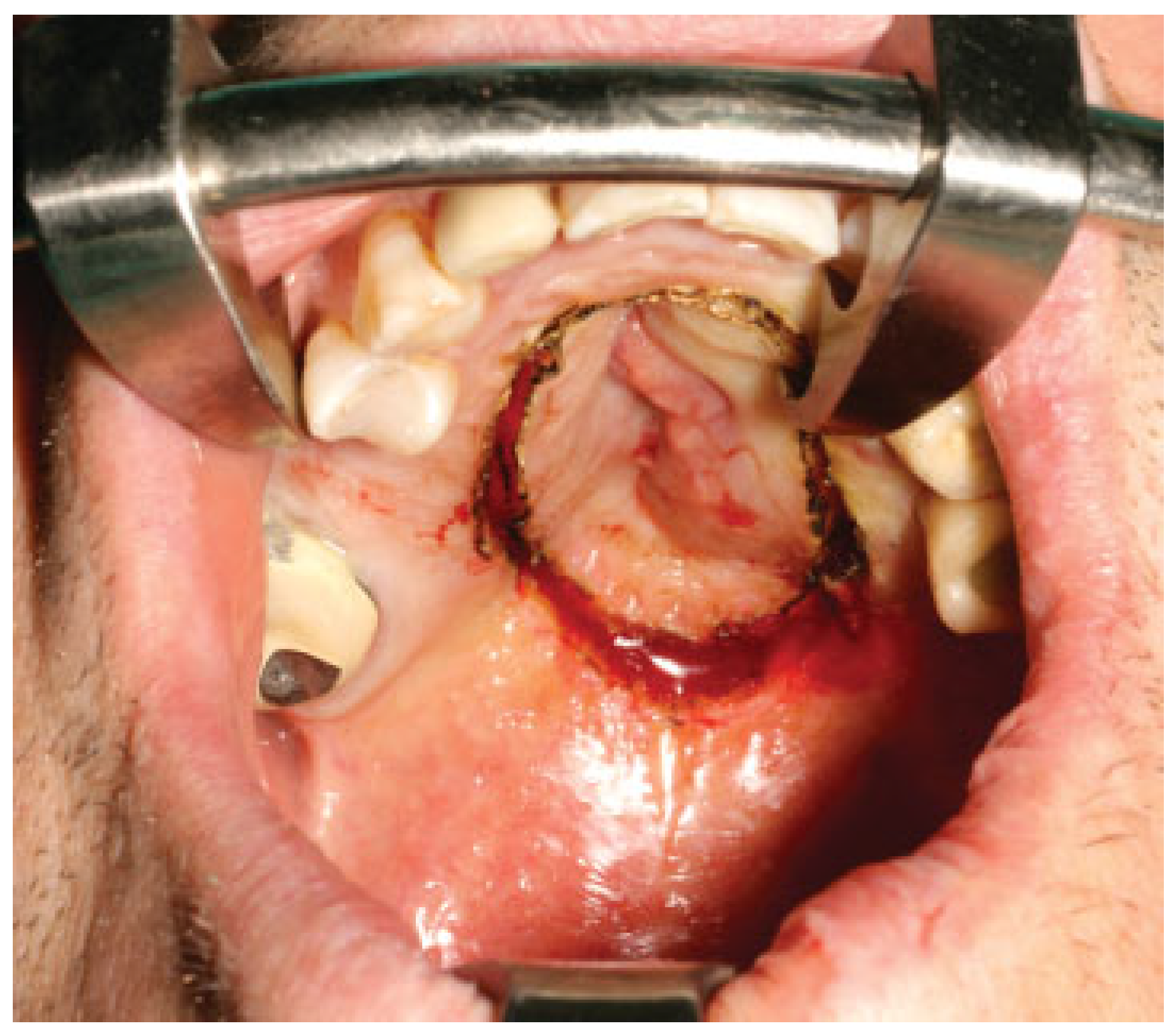
Once in the operating room, the kind of intubation should be individualized. For unilateral tumors, intranasal intubation is preferred to improve the intraoral visualization and facility tumor resection. Submental intubation represents an effective alternative especially with tumors affecting both nostrils. This technique places the endotracheal tube away from our surgical field and improves the tumor visualization. In the surgical technique, first, a free margin is delimitated on the palatine mucosa reaching the bone layer and a palatine osteotomy is done using an oscillating saw (
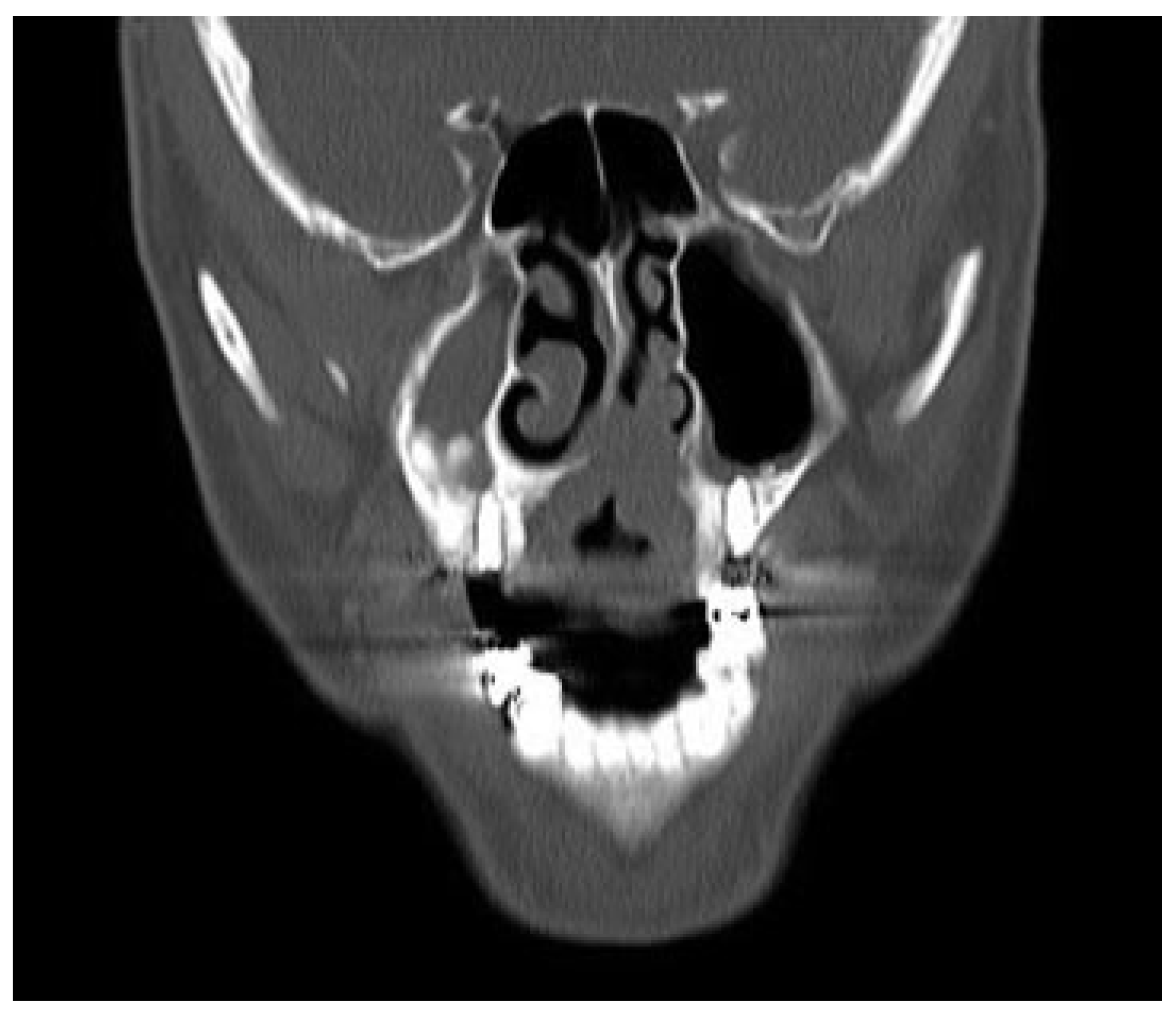
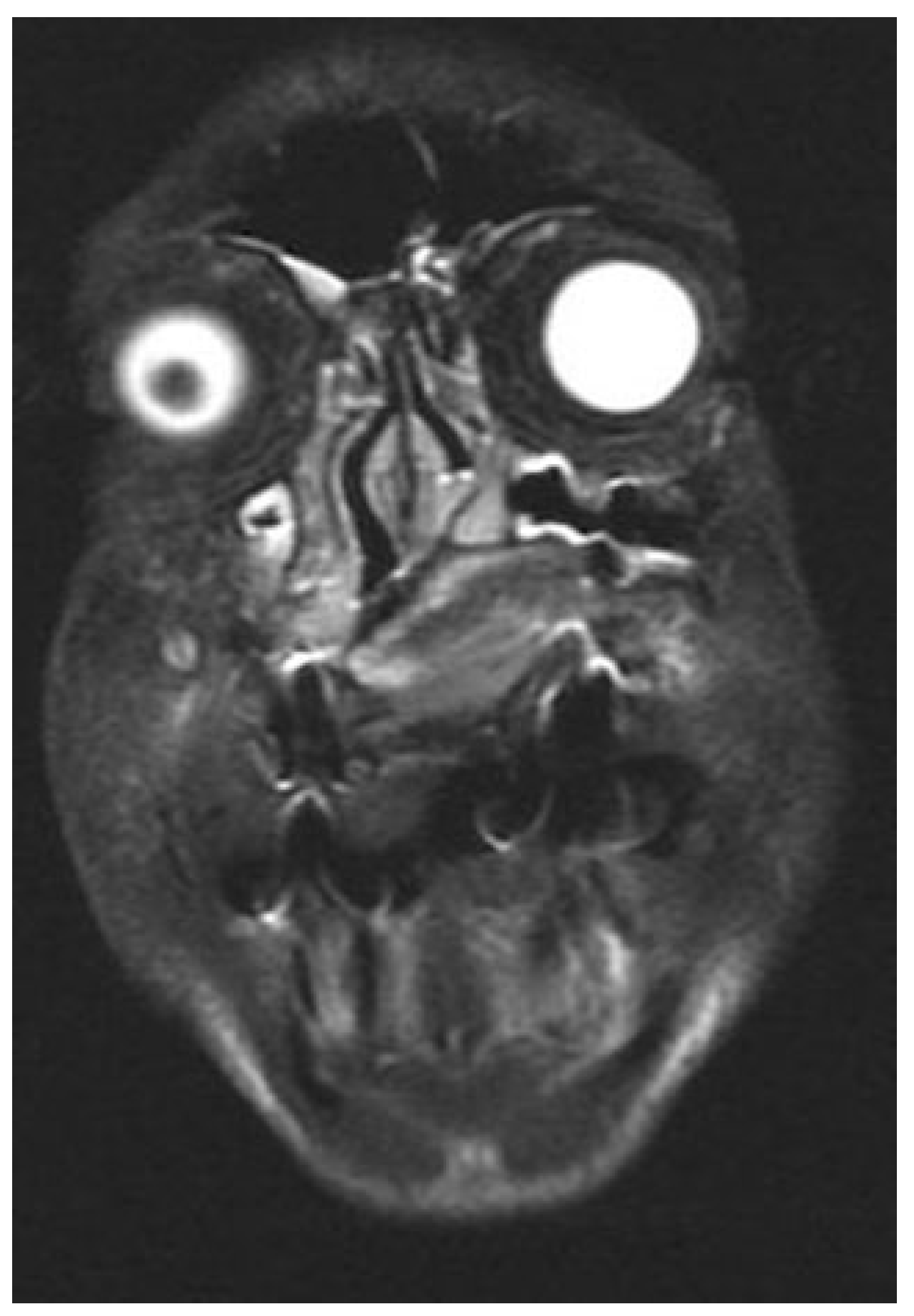
Figure 1). Next, a vestibular maxillary approach is done and microplates are fixed at both sides of the maxilla to guarantee the correct reposition of the maxilla at the end of the procedure. Screws and microplates are removed and a Le Fort I osteotomy is performed. This represent the most critical point of the approach and attention must be directed to the piriform aperture, lateral nasal walls, and the septum in order to make the cuts without entering into the tumor. Preoperative imaging is crucial to determine the intranasal extension of the tumor and decide the level of the Le Fort osteotomy (
Figure 2). Vertical extension of the tumor determines the most limiting factor and tumors with high intranasal extension may not be candidates for this kind of approach, as the risk of tumor disruption is higher in these cases.
Other authors have described endoscopic approach as a useful technique for the resection of midline tumors [
3]. Although this may help in the operating room to ensure the correct margin of the resection, we consider it is difficult to accomplish the entire resection with free margins. The Le Fort approach, however, allows the direct visualization of the margins as the osteotomy is performed and warrants a better resection. Instead of endoscopic assistance, intraoperative navigation could enhance the surgical procedure allowing defining the correct position of the osteotomy.
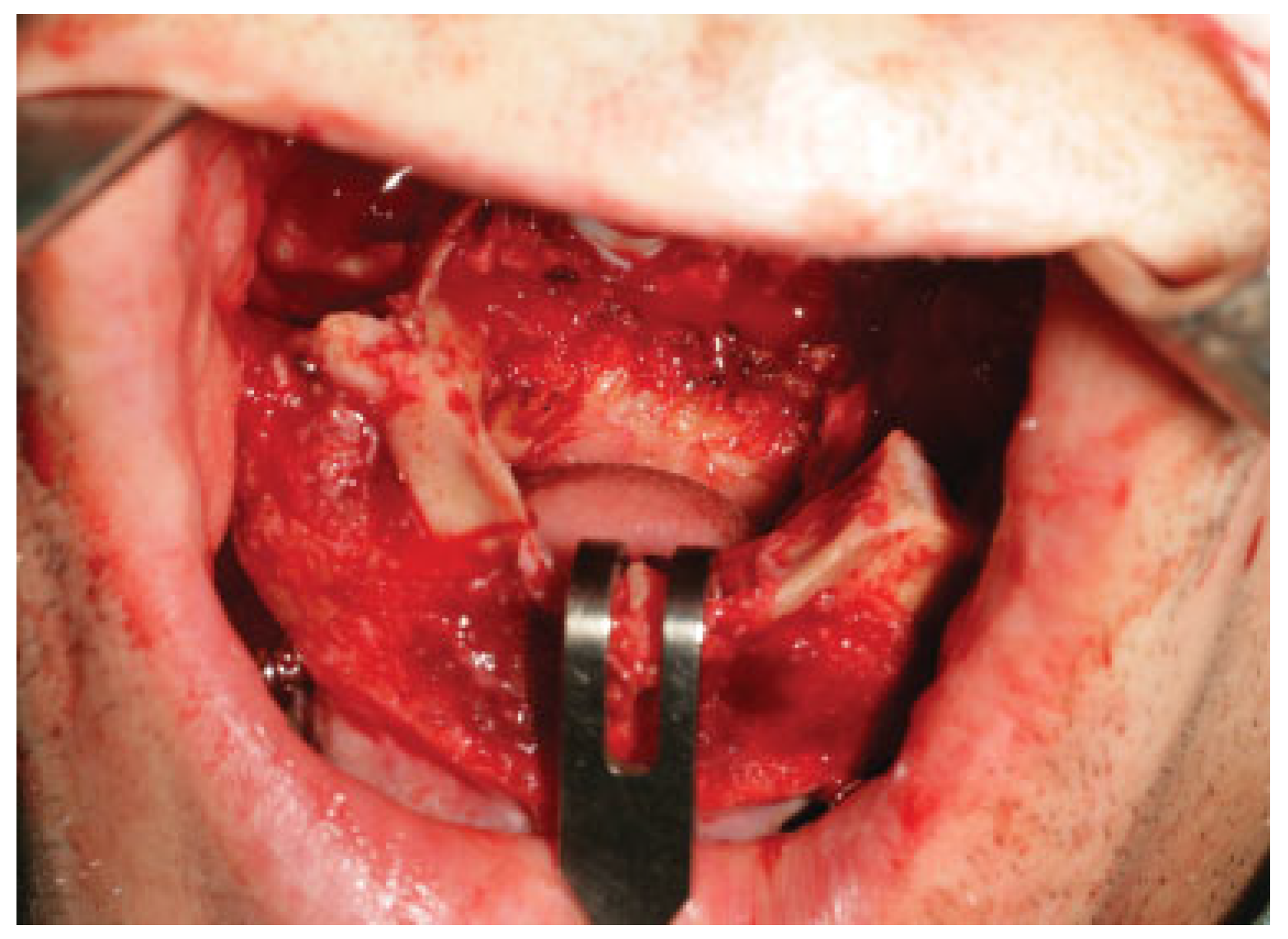
Once the osteotomy is completed, the maxilla is downfractured progressively ensuring that the tumor is completely detached from the rest of the maxilla (
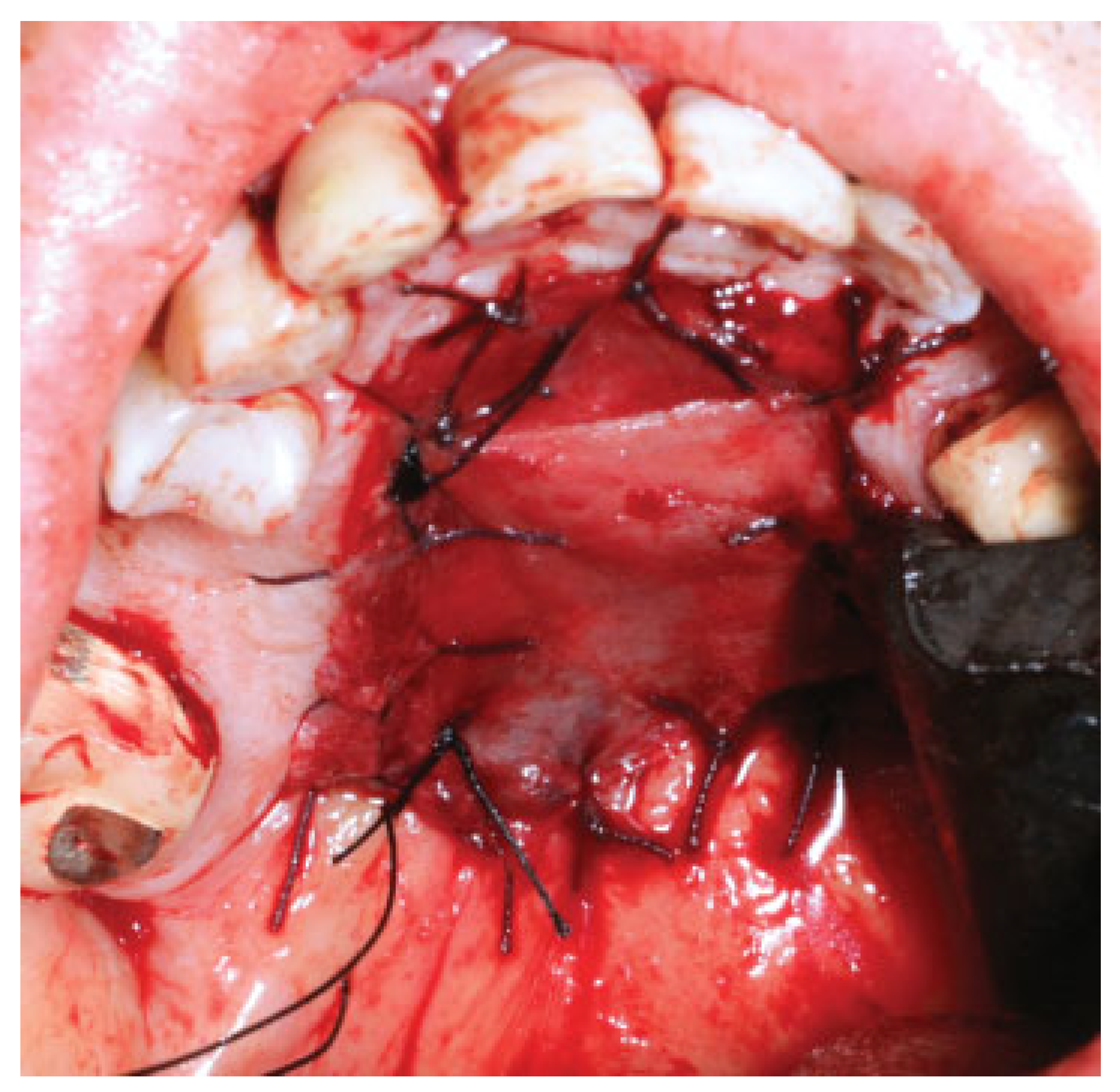
Figure 3). Finally, the tumor resection is completed by direct visualization of all the margins (
Figure 4 and
Figure 5). Before the maxilla is repositioned, the nasal lining closure is accomplished. For this purpose, the authors choose to use vomer or turbinate flaps when direct closure could not be achieved.
The temporal muscle flap is one of the main options for maxillectomy defects reconstruction, especially when considering midline palate defects in which bone tissue is not essential for functional rehabilitation or in elderly or pluripathologic patients, in which microsurgical reconstruction procedures are not feasible [
4,
5]. However, in dentate patients, this option may be restricted if there is any edentulous gap to cross the temporal muscle over the alveolar ridge. With the Le Fort approach for midline palatal tumors, the temporal muscle is passed through a window in the anterior wall of the maxillary sinus and sutured into the defect, before the maxilla is repositioned and fixated (
Figure 6 and
Figure 7).
We have applied this approach in five patients with squamous carcinoma of the palate accomplishing free surgical margins in all cases. However, two of these five patients required adjuvant radiation therapy (RT) in basis of the tumor size. Among the complications, one patient developed dehiscence of the muscle suture, probably in relation with his poor nutrition condition and needed a second surgical procedure 1 week later. No infections or cerebrospinal fluid leaks were demonstrated in any patient. With the exception of the patient with the muscle dehiscence, all the patients were discharged from the hospital within the first week, achieving good functional and aesthetic results in all cases. Initial muscle bulky inside the oral cavity may be present, but it is progressively decreased during the next months with the gradual atrophy process of the muscle (
Figure 8 and
Figure 9).
In our experience, temporal muscle reconstruction of these defects achieves better functional results than reconstructions with palatal obturators [
6]. All the cases presented represent midline tumors without extension to the alveolar ridge in dentate patients. In this situation, an obturator is more difficult to retain and the patients may show discomfort when wearing it. In our experience these patients show better adaptation and can quickly return to a normal diet with a temporal muscle reconstruction.
In summary, the Le Fort I osteotomy approach for midline maxillectomies in dentate patients guarantees a safe tumor resection under direct visualization and allows an immediate reconstruction with a temporal muscle flap.