Orbital roof fractures are a challenge to manage due to their mechanism of injury, concomitant trauma, and the risks posed to the eye, extraocular muscles, and overlying frontal sinus and brain. In the assessment and management of orbital roof fractures, it is important to consider the anatomical structures of the roof, the degree of ocular, muscle, nerve, and brain involvement, and the potential morbidity that may result from both conservative and operative management.
The orbital roof is formed for the most part by the frontal bone, merging posteriorly with the lesser wing of the sphe- noid bone to end at the superior orbital fissure. The roof extends laterally to the zygoma and greater wing of sphenoid and medially to the orbital plate of the ethmoid, the lacrimal bone, and the frontal process of the maxilla.
Anteriorly the frontal sinus sits medially over the orbital roof, extending posteriorly for a variable distance. Above and behind the frontal sinus sits the anterior cranial fossa, housing the frontal lobes of the brain, which is lined by adherent dura and covers the upper surface of the orbital roof.
The structures that lie within or in close proximity to the roof of the orbit are the lacrimal gland, the superior oblique, levator palpebrae superioris and superior rectus muscles, the frontal nerve of the ophthalmic branch of the trigeminal (which becomes the supraorbital and supratrochlear nerves), the superior division of the oculomotor nerve, and the eye.
The stability of the eye relies on three main things: the bony attachment of the rectus muscles, the orbital fat, and forward pull of the oblique muscles. The eye is also supported by the presence of the suspensory ligament of Lockwood and the medial and lateral check ligaments [
1].
Orbital Roof Fractures
Orbital roof fractures are commonly the result of high impact trauma, accounting for approximately 1 to 9% of all facial bone fractures [
2]. Orbital roof fractures are considered to be a subregion of injury of frontobasal trauma [
3], which also includes the frontal sinuses, nasoethmoid, cribriform plate, lateral orbital wall, superior orbital rim, squamous temporal bone, and planum sphenoidale [
4]. These fractures rarely present in isolation and can be associated with significant complications involving the eye, orbit, extraocular muscles, and brain.
The typical mechanism of injury for orbital roof fractures is high-energy trauma such as motor vehicle/bike accidents, falls, and assaults. As a result, the majority of fractures are associated with concomitant craniofacial injuries, most commonly frontal sinus, orbital rim, naso-orbital-ethmoid (NOE), other orbital wall, and LeFort fractures. In addition to these injuries, a proportion of patients will also have multisystem injuries, which for the most part are neurological/intracranial [
5].
Patients may present with different symptoms indicative of the affected structures. Aside from periorbital edema and ecchymosis and some ocular discomfort and epiphora, facial lacerations as a result of the trauma may be present. If there is involvement of the superior oblique or rectus muscles, the patient may have limitation of vertical or inward gaze or diplopia. Altered sensation in the distribution of the supraorbital and supratrochlear nerves may be present, and if the fracture is displaced, exophthalmos, enophthalmos, hyperglobus, hypoglobus, or proptosis may result.
The diagnosis, while it can be inferred on clinical examination, is confirmed with radiology, preferably computed tomography (CT) of all facial bones (
Figure 1). Other imaging modalities including MRI for fine examination of extraocular muscles or neural/cerebral involvement may be used.
Associated Injuries and Complications
It is important to assess for the potentially severe injuries and complications associated with orbital roof fractures, which may have implications on treatment. The rarity of isolated roof fractures means that all possible associated injuries must be identified or excluded. Associated injuries can be grouped into the following four categories.
1. Skeletal
Skeletal injury consists of adjacent fractures of the facial skeleton including other orbital fractures (medial and lateral wall and floor). The more common associated fractures are those of the frontal sinus, orbital rim, and NOE region as discussed earlier. There is also potential for damage to the paranasal sinuses in high impact injury, which can lead to communication with the orbit and the cranial cavity.
2. Intracranial Injury
Intracranial injury also has the potential for severe consequences if not managed precipitously. The most common intracranial injury as a result of an orbital roof fracture is the presence of a cerebrospinal fluid (CSF) leak, most commonly clinically presenting with CSF rhinorrhoea [
7]. Other sequelae include extraocular motor dysfunction resulting in dysmotility of the eye with diplopia (either in primary or in other gaze), enophthalmos or exophthalmos, entropion or ectropion. Other more significant consequences include dural tear, tension pneumocephalus, encephalocoele, the potential for intracranial infection and damage to the cerebral tissue (frontal lobe contusions). Due to the typical high impact mechanism of these fractures, many patients will suffer traumatic intracranial hemorrhage or injury. If the patient has a poor neurological prognosis, it will likely impact the ability to appropriately assess them and determine suitability for surgery.
3. Intraorbital Contents and Periorbital Soft Tissues
Intraorbital injury encompasses all structures affected within the orbit, namely the eye, optic and other nerves, extraocular muscles, arteries and veins, and contents of the superior orbital fissure. Ocular injury is one of the main indications for emergency surgery in facial fractures and includes globe rupture, retrobulbar hematoma and hyphema, all of which, if not managed immediately, have the potential to cause permanent visual impairment. Studies have reported up to 25% incidence of ocular injury with orbital fractures [
6]. Other sequelae include extraocular motor dysfunction resulting in dysmotility of the eye with diplopia (either in primary or in other gaze), enophthalmos or exophthalmos, entropion or ectropion. This can carry a significant morbidity and impediment for the patient. Periorbital soft tissue damage includes eyelid (or orbicularis oculi) damage, lacerations, and periorbital hematomas or edema. Orbital roof fractures can also be associated with subcutaneous emphysema.
4. Frontal Sinus Injury
Frontal sinus injury occurs commonly with orbital roof fractures due to the typical mechanism of injury. Frontal sinus fractures that involve the orbit are more likely to be of the “blow-in” type [
8]. Injury can involve anterior and posterior tables of the sinuses and also the nasal frontal outflow tract (nasofrontal duct). If the posterior table is involved, then there may be underlying cerebral damage or a CSF leak. The communication between the sinus and the intracranial vault also increases the risk of cerebral infection. Damage to the nasal frontal outflow tract can result in a mucocele and localized infection [
9].
Methods
A review of the current literature was undertaken via a database search of PubMed, MEDLINE, and Embase. The search strategy was to include all articles published in medical literature involving the keywords “Orbital,” “Roof,” Fractures,” and “Frontobasal trauma.” No systematic or Cochrane reviews or meta-analyses were found on the topic. Current surgical references including publications from the AO Foundation were included.
A review of all patients from January 2011 to July 2013 was performed using the Royal Melbourne Hospital weekly facial fracture audit of patients treated by the Oral and Maxillofacial and Plastic and Reconstructive surgery units. Each patient’s case and imaging were reviewed for patient demographics, mechanism, associated injuries, and treatment.
Results
A total of 668 patients were treated with facial fractures at the Royal Melbourne Hospital between January 2011 and July 2013. Of these, 47 presented with orbital roof fractures, only 3 in isolation.
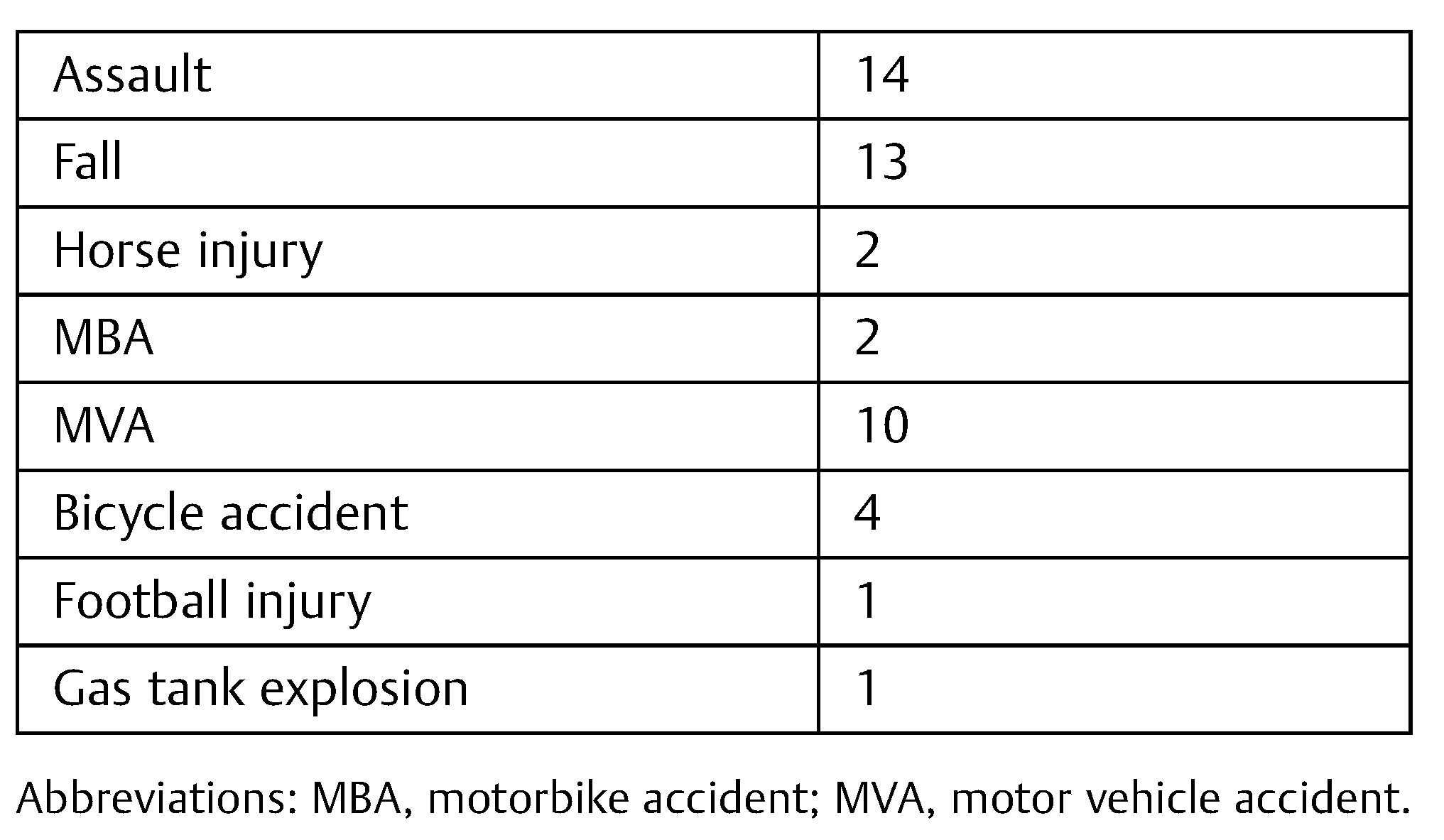
There were 40 males and 7 females, and the median age was 49 years old (range 17–88). The majority of fractures were as a result of an assault (14) or a fall (13) (
Table 1). Forty-two patients were managed conservatively and only five underwent operative fixation of their orbital roof fracture. Four of these were managed conservatively due mainly to their poor neurological status postinjury.
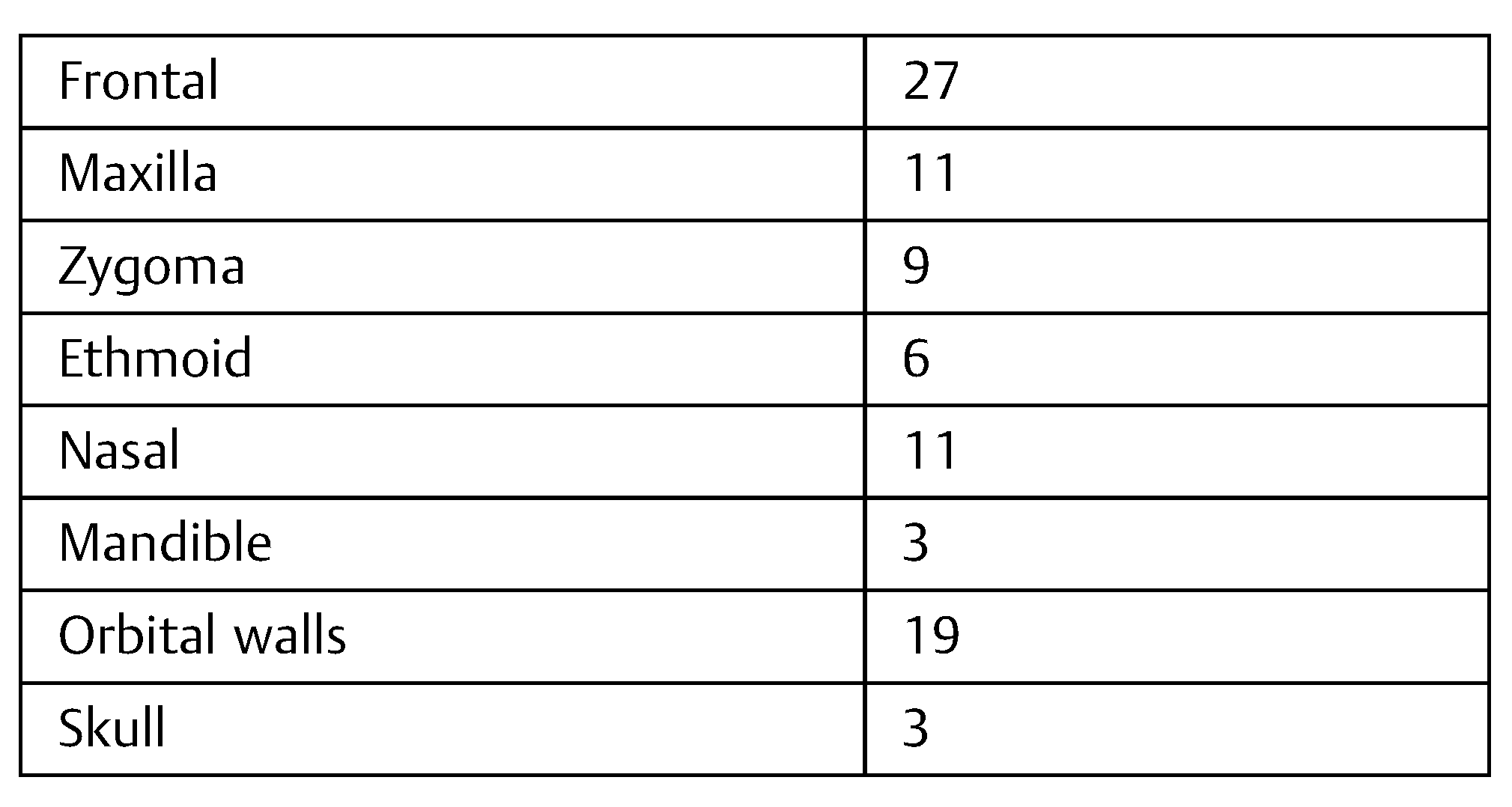
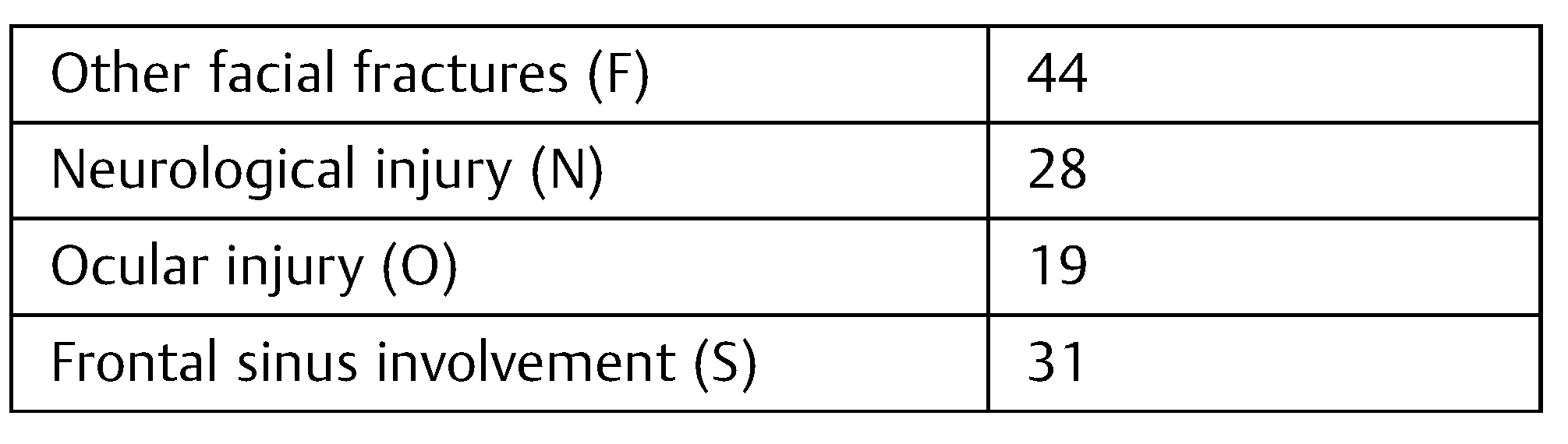
Twenty-eight patients had associated intracerebral injury such as contusions, traumatic subarachnoid hemorrhage, and extra-axial collections. Over half had associated frontal bone/sinus fractures (27) and a large proportion involving the other orbital walls (19) (
Table 2 and
Table 3).
Discussion
As part of the assessment of a patient with an orbital roof fracture, appropriate clinical examination and imaging are crucial. During this time, the treating specialist should ascertain not only the need for conservative or surgical management of the fracture but also the need for involvement of other specialties such as ophthalmology and neurosurgery.
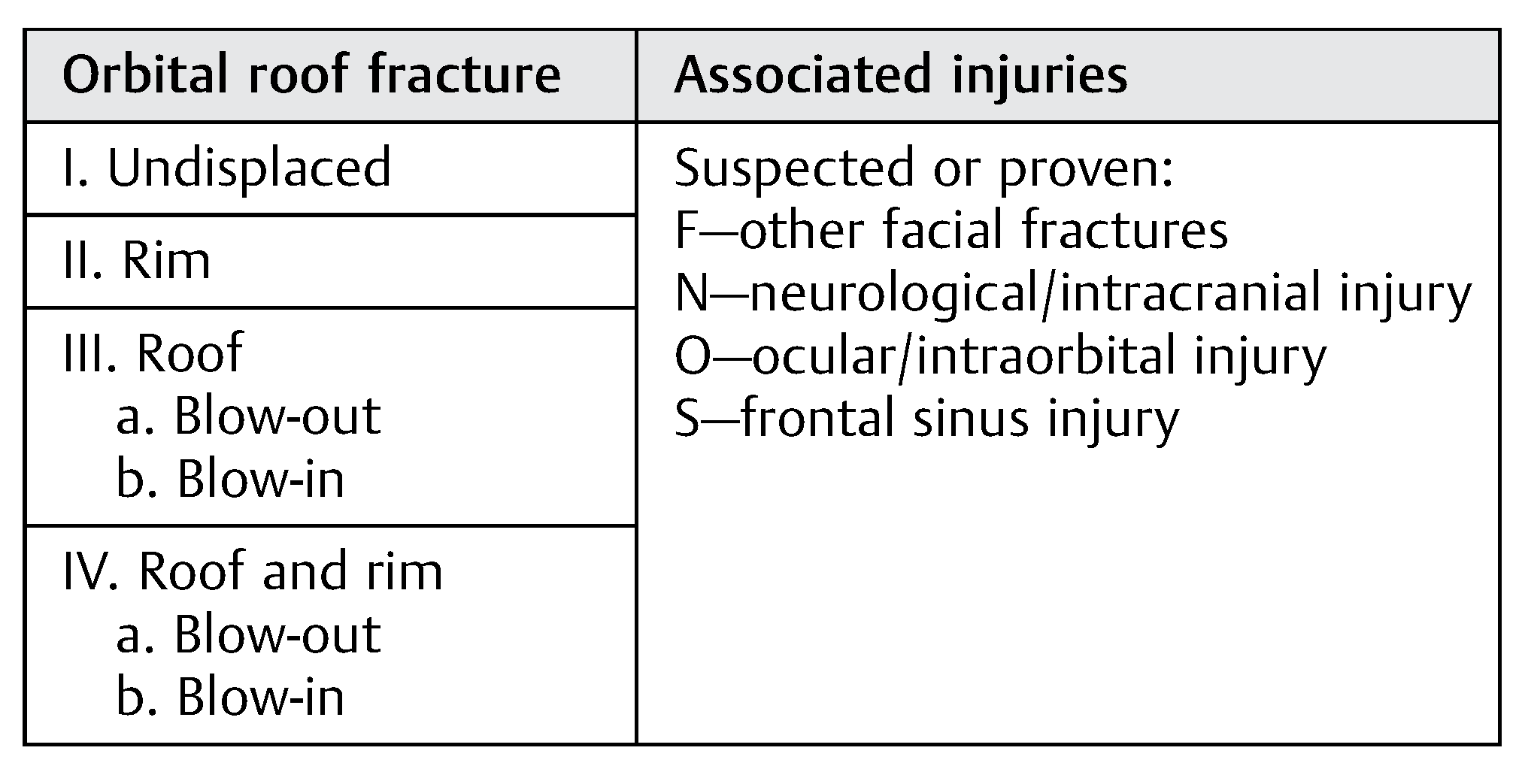
Currently, there is no specified classification system for orbital roof fractures [
8], but the following types of displaced fractures have been defined [
2]:
The “blow-in” fracture: inferior displacement of the orbital roof, due to an abnormal increase in intracranial pressure. Fracture fragments are present in the orbital cavity.
The “blow-up/out” fracture: superior displacement of the orbital roof into the anterior cranial fossa due to increased intraorbital pressure. Fracture fragments are present in the anterior cranial fossa.
Supraorbital rim fracture: indicative of a significant frontal force.
Frontal sinus fractures: involving the anterior, posterior or both tables of the frontal sinus, usually associated with high impact trauma.
In defining a new classification system for orbital roof fractures, we aim to allow accurate identification of the fracture and therefore also consideration of the mechanism and potential associated injuries. The classification will then provide guidance of potential management options in addition to the need for a referral based on the potential injuries inflicted and damage to neighboring structures. The decision for surgical intervention should be tailored to the individual patient; however, this classification system and algorithm will ensure that all elements are considered.
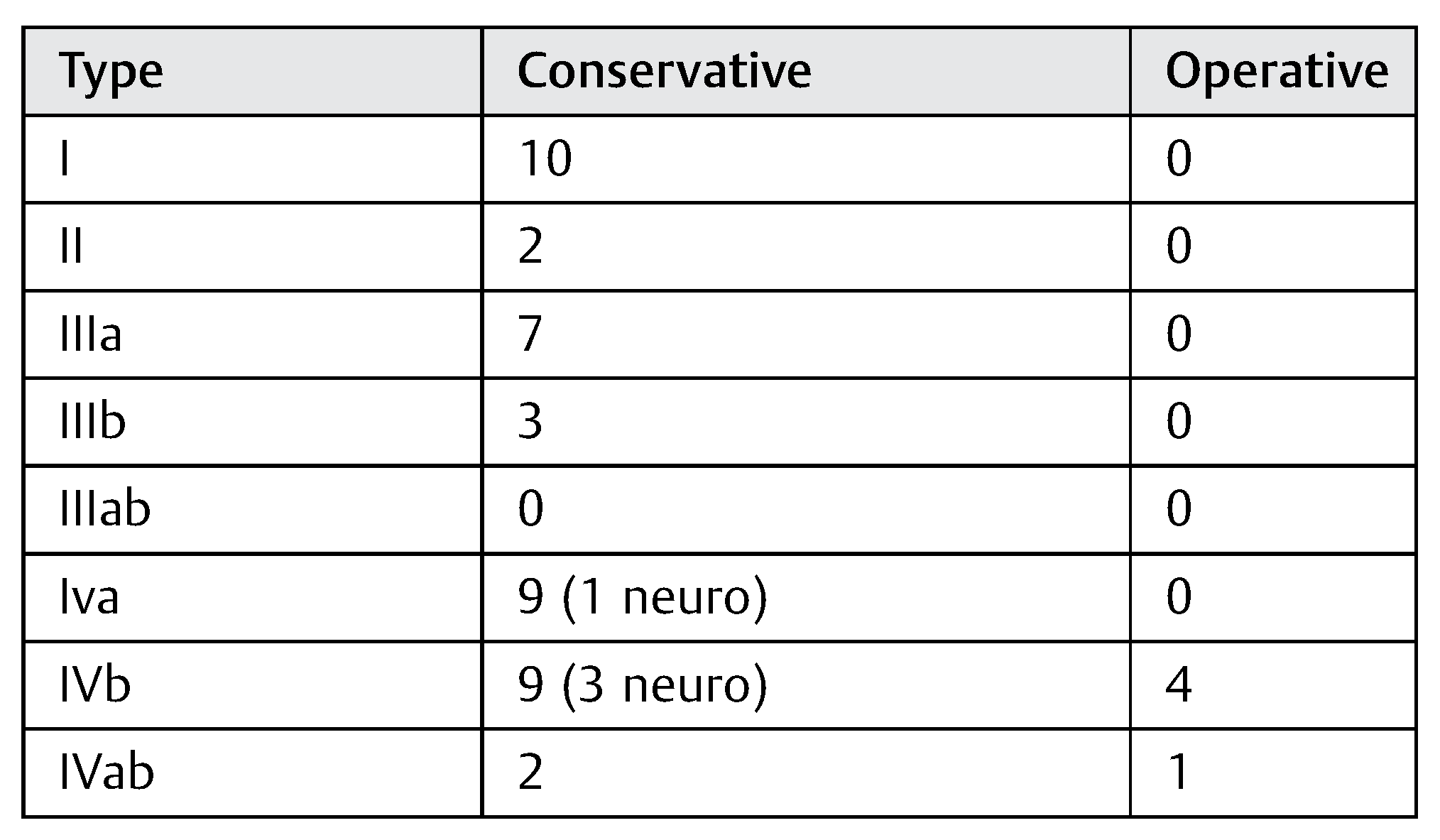
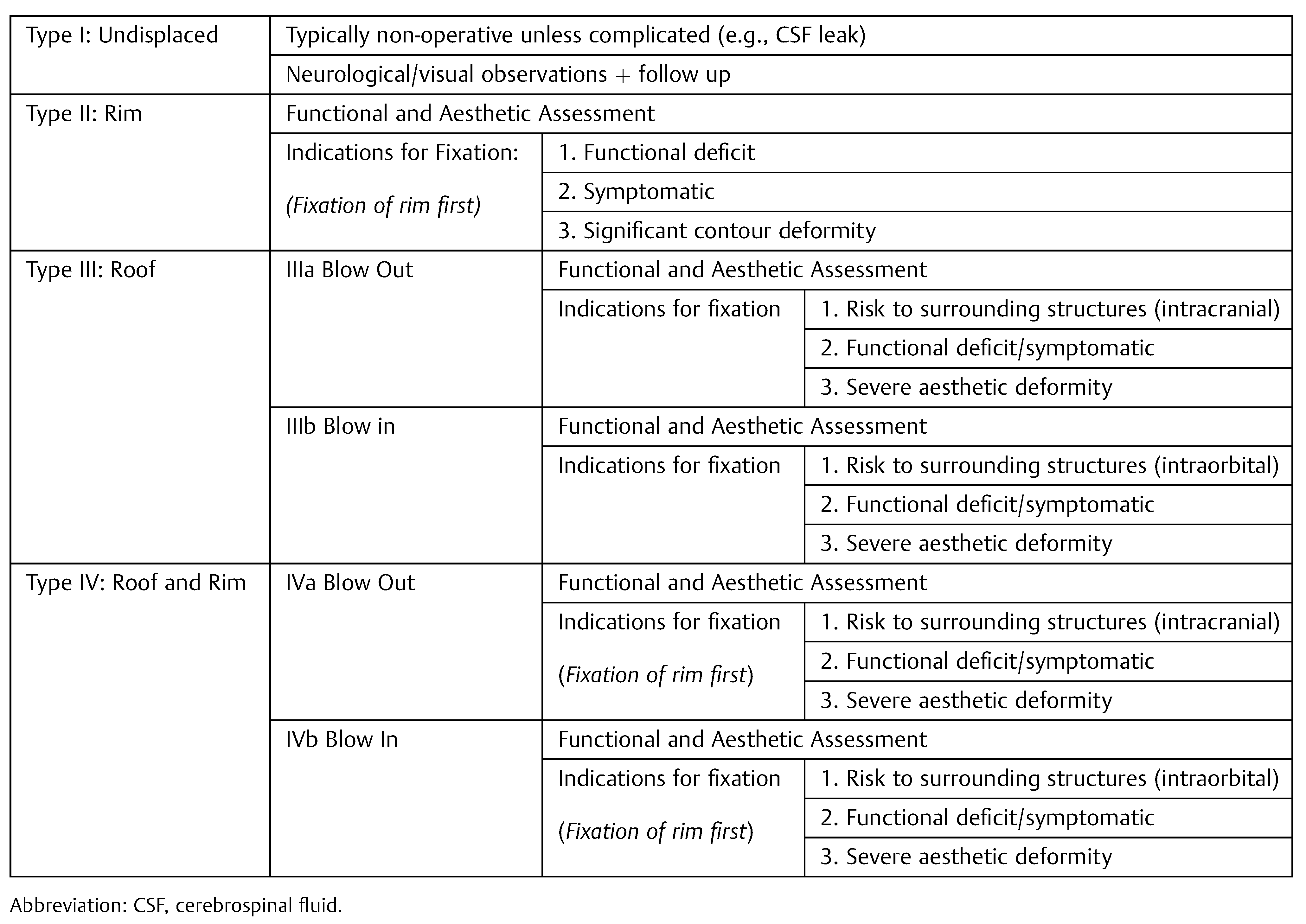
Each fracture type and associated injuries have implications for treatment and, accordingly, we propose a graduated four-point system (
Table 5).
We have divided the fractures according to displacement (undisplaced or displaced), anatomical location (rim, roof), and then fracture characteristics (blow-in or blow-out). Associated injuries are then described in addition to the fracture type (other facial fractures, neurological/intracranial injury, orbital injury, frontal sinus injury), as, due to the mechanism of injury, all the fracture types may be accompanied by these sequelae. The displacement and anatomical location are described in sequence of severity, with the higher type being typically associated with the higher intensity injury.
Operative intervention of an orbital roof fracture should be considered if the patient is symptomatic or at risk of severe complications. Potential indications for surgery include displaced bone fragments (which may cause symptoms, structural damage, infection, or an encephalocoele), compromise of orbital contents (eye, EOM), and prolapse of brain tissue into the orbit. Surgical treatment of every patient should be individualized, with consideration of all elements, aided by this classification.
Type I
Undisplaced fractures are typically managed conservatively, with neurological and visual observations to ensure no significant concomitant neurological injuries or deterioration [
10].
Type II
The supraorbital rim is the strongest part of the frontal bone and provides an outlining structure to the orbit. If it is displaced, the patient should be assessed aesthetically and functionally for consideration of fixation. If there is a noticeable contour defect or impairment of ocular movement or function, the patient should be offered surgery. If other fractures are present, reduction and fixation of the rim should usually be performed prior to fixing other fractures, as it provides horizontal buttress stabilization as per AOCMF principles. Surgery should be performed within 10 days to 2 weeks for acute defects or in minor fractures whose symptoms do not resolve within the same time frame [
10,
11].
Type III
The main sequelae associated with blow-in fractures are damage to the eye, extraocular muscles, and nerves. With the presence of any of these injuries, particularly exophthalmos or proptosis, surgical intervention should be considered.
While a blow-out fracture may not carry the same level of potential orbital injury, it may still cause enophthalmos or hyperglobus and more significantly can result in intracranial injury. All of these warrant consideration of surgical intervention and if intracranial injury is suspected or evident, intracranial access should be obtained via a craniotomy. This kind of surgical intervention is ideally undertaken with a multidisciplinary approach involving a neurosurgical team.
Type IV
Patients with type IV fractures should be treated as for both Type II and Type III fractures. In many cases if patients require fixation, stabilization of the orbital rim may suffice for correction of symptoms and function.
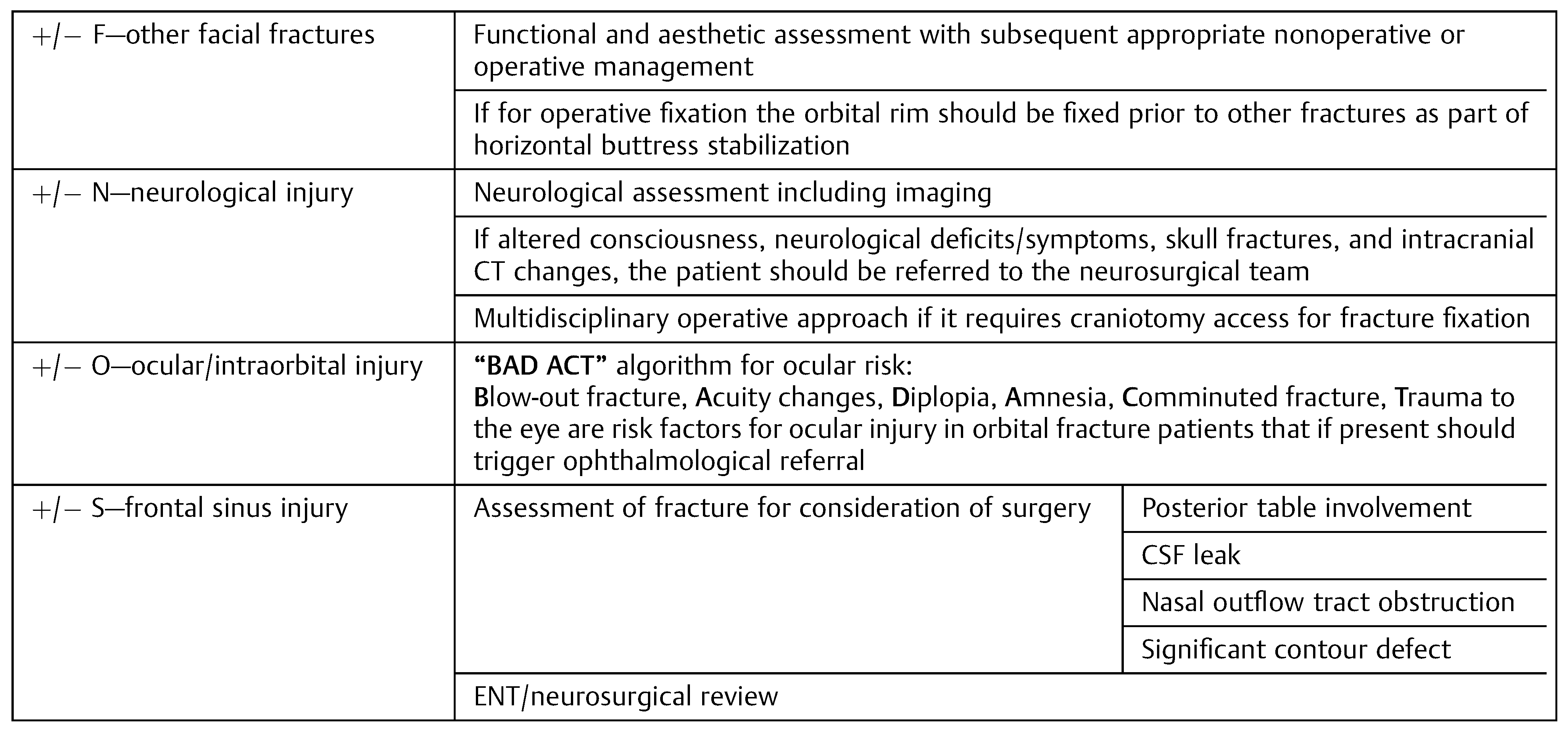
Suspected or Proven Associated Injuries
These additional subclassifications ensure consideration of potential associated injuries and therefore appropriate referral to the necessary specialty teams.
F—Facial Fractures
Other facial fractures present should be taken into account when considering surgery. Facial fracture reduction and sequenced repair should follow the buttress fixation model as per current AOCMF principles.
N—Neurological Injury
All patients with suspected or proven neurological injury should be reviewed by a neurosurgeon. Symptoms such as decreased consciousness Glasgow Coma Scale (GCS), amnesia, visual, sensory, or motor disturbances, CSF otorrhea or rhinorrhea, pupillary defects, evidence on imaging of intracranial damage or a blow-out fracture should be promptly reviewed by the neurosurgical team. Due to the high risk of intracranial infection if a breach of the dura is present, patients should be treated with a course of antibiotics. Patients should also be advised to avoid blowing their noses in the short-term posttraumatic period due to the risk of subcutaneous emphysema and pneumocephalus. If pneumocephalus is present, patients should be advised regarding air travel.
O—Ocular/Intraorbital Injury
As discussed by Al-Qurainy and colleagues [
12], it is important to recognize the risk of and therefore assess and detect potential injuries to the eye with a detailed ophthalmological examination. Their acronym “BAD ACT” (
Blow-out fracture,
Acuity,
Diplopia,
Amnesia,
Comminuted,
Trauma) provides a straightforward list of risk factors for ocular injury in orbital fracture patients that should trigger ophthalmological referral. Using the “BAD ACT” acronym, patients at risk of ocular injury should be assessed by an ophthalmologist. The presence of globe injury will necessitate immediate ophthalmological intervention for watertight wound closure, with any procedures that will raise intraocular pressure contraindicated, including fracture reduction. However, depending on the fracture, emergency reduction may be required to relieve pressure on the globe [
13]. Traumatic optic neuropathy may delay facial fracture reduction as the patient undergoes high-dose steroid treatment in an effort to improve their vision (followed by optic canal decompression if this is not successful) [
14].
S—Frontal Sinus Fractures
Frontal sinus fractures should be assessed regarding requirement for fixation both independently and in the context of the orbital roof fracture. Consideration for surgery should occur in the presence of a CSF leak/dural tear, severe injury of the posterior table, significant contour defect, or damage of the nasofrontal duct [
9]. Although the trend is more toward conservative management of these fractures, any fracture causing communication of the sinus with either the orbit or cranial cavity should be commenced on prophylactic antibiotics (
Table 6 and
Table 7;
Figure 2).
Operative Intervention
Reconstruction of the orbital roof using titanium and microscrews has been shown to yield the most stable and effective results [
15]. Surgical access is facilitated via a coronal approach, superolateral orbital rim approach (either supraorbital eyebrow or upper eyelid incisions), or via existing lacerations that may be present due to the initial trauma. Special attention must be paid to intracranial and intraocular structures to ensure no harm is done during the repair.
In addition to ensuring complete reduction and stable fixation of major fragments, it is important to remove any smaller bony fragments that may potentially impact intraorbital structures (especially the optic nerve) or brain tissue, with the possible formation of an encephalocoele if any foreign body is left in the cranial cavity.
Current practice advocates the use of intraoperative CT imaging to ensure safe and accurate placement of plates and adequate fixation, reducing morbidity and the need for further corrective operations [
16]. If not used intraoperatively, postoperative imaging (CT) should be performed to confirm adequate reduction and plate placement.
Optimally, patients that undergo operative intervention are nursed at 45 degrees postoperatively, with no nose blowing, a course of oral antibiotics, and avoidance of sport/contact activities. Patients should be followed up at 2- and 6-week intervals to ensure good recovery and monitored long term for delayed complications, avoiding contact activities during this time. If patients remain symptomatic, they should undergo longer term follow-up with investigation and corrective surgery if required. This may be the case in intraocular entrapment from plate placement or retained fragments.
Out of 47 orbital roof fracture patients, the most common fracture type was Type IVb (13) (
Table 4). However, as demonstrated by our cases series, the majority of patients despite their injury will not require operative management. Surgical intervention should be initiated if the patient has deficits as a result of their injury, either functional or aesthetic, and is expected to recover well following surgery.
Conclusion
As an infrequent presentation, orbital roof fractures have not as yet been thoroughly examined and classified. Through our limited case series and a literature review, we propose a clinically based classification and management algorithm. This will provide a structured and straightforward way of evaluating orbital roof fractures and guiding their management. Although the majority of fractures will be treated conservatively, it is important for the few with significant sequelae that they are managed appropriately to achieve the best possible functional and cosmetic outcome for the patient.