The mandible is a common site of maxillofacial fractures because of its position and prominence. The overall goals of treatment of pediatric mandibular fractures are to restore proper function (mastication and articular movements). This is achieved by reduction of fracture, proper fixation to ensure union of the fractured segments, and the reestablishment of the patient’s normal occlusion.[
1]
Titanium plates and screws are routinely used for osteo-fixation of maxillofacial fractures including mandibular fractures. However, titanium devices have several potential problems which could necessitate removal.[
2] These include allergic hypersensitivity, thermal conductivity, unacceptable palpability, and infection around the hardware.[
3] Pain and irritation also were reported causes of plate removal.[
4]
In a retrospective review of 279 patients with isolated mandibular fractures fixed with titanium miniplates, Tuovinen et al reported a plate removal rate of 11.5%.[
5] Matthew and Frame interviewed 23 consultant oral and maxillofacial surgeons and concluded that the incidence of plate removal ranged from 5 to 40%, with a mean removal rate of 13%.[
6]
In children, metal plates should be removed after bone healing to avoid growth disturbances. This is also associated with additional hospitalization time, relatively high morbidity, and an increased burden on the health system.[
7]
Bioresorbable plates have become an established alternative to metal fixation in reconstructive, trauma, and orthognathic craniomaxillofacial surgery.[
8] Currently, there are different materials of biodegradable devices in the market. Also, different manufacturing technologies could affect the physical character of the device. The main advantage of the use of the biodegradable devices in children is the avoidance of a second surgery to remove the metal plates.
We are reporting our early experience with one type of biodegradable fixation system (self-reinforced poly-l/dl-lactide [SR-PLDLA]) in pediatric patients younger 12 years. Stability and efficiency of biodegradable plates and screws for fixation of pediatric mandibular fractures were assessed.
Patients and Methods
This is a prospective study performed in the period from October 2011 to February 2013. It included pediatric patients (12 years or younger) presented to the emergency department in a tertiary referral university hospital with mandibular fractures amenable for open reduction and internal fixation with miniplates and screws and who express the ability to return for follow-up.
Patient evaluation included the demographic data and the history related to the mandibular trauma as the cause and time of injury. History also included dental hygiene, tooth disease, preinjury malocclusion, and any temporomandibular joint (TMJ) symptoms. History of any previous facial injuries or maxillofacial surgeries done was also included. Patients were examined for signs of mandibular fracture including swelling, ecchymosis, deformity, crepitus, gingival lacerations, missing teeth, stability of remaining teeth, malocclusion, and restrictions or deviations in opening, closing, or protrusion. Computed tomography (CT) radiographs were taken preoperatively. Fractures were classified according to the site and also according to displacement into undisplaced, slightly displaced (less than one cortical thickness overlap) and severely displaced (more than one cortical thickness overlap) fractures. A penicillin-based antibiotic (amoxicillin/clavulanic acid, 50 mg/kg/d divided in two doses) was administered once the patient is seen and for 1 week postoperatively.
The Operative Procedure
The procedures were done under general anesthesia and nasal intubation. Fracture exposure was done through either transbuccal approach (in symphyseal or anterior body fractures) or submandibular approach (in angle fractures). Maxillomandibular fixation (MMF) was done to restore the patient’s occlusion by one of the following methods: Erich arch bars, Ernst ligatures, or circummandibular wiring and maxillary screws according to the state of dentition. The fracture was reduced and osteosynthesis was achieved with 2.0 or 2.5 mm biodegradable self-reinforced poly (
l/
dl)lactic acid plates and screws (INION, Tampere, Finland) (
Figure 1). The plates were adapted to the fracture site by bending. The screw holes were drilled and tapped, then screws were applied (
Figure 2). When the fractures were at the symphyseal region or severely displaced, two plates were used; otherwise
one plate was used. Monocortical screws were used in all the cases. After surgery, MMF was maintained for 1 week postoperatively.
The follow-up appointments were at 1 week, 6 weeks, 3 months, and 12 months postoperatively with the assessment of any wound complications as infection, dehiscence, and fistula formation, stability, displacement, malocclusion, mouth opening limitation, TMJ ankylosis, and disturbances of sensation. Radiographic follow-up by CT scan was done to observe any displacement and fracture healing at 1 week, 3 months, and 12 months postoperatively.
Results
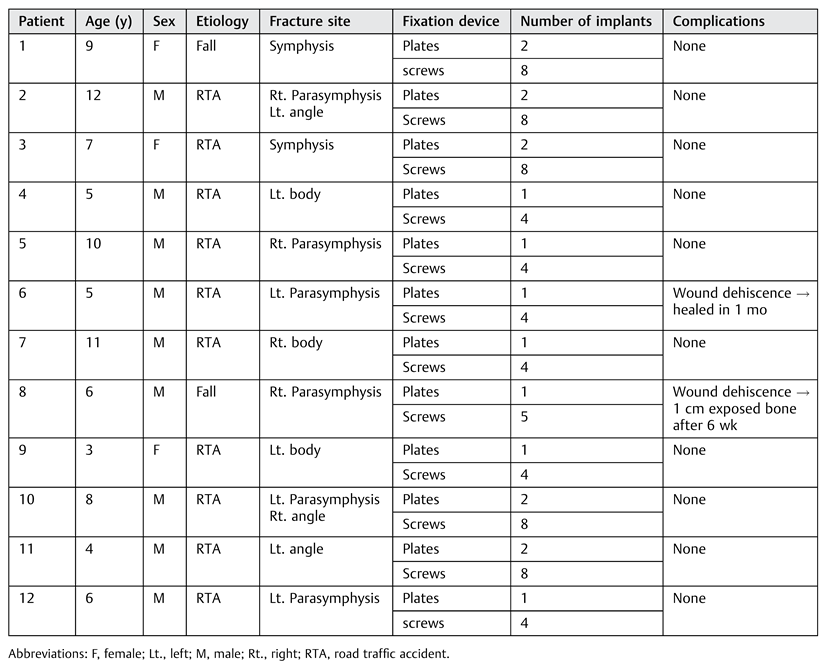
In the period from October 2011 to February 2013, 12 children with mandibular fractures (
Table 1) were managed using the biodegradable plating system. The average age was 7.16 years (range from 3 to 12 years), nine males and three females giving male-to-female ratio (3:1). The time interval between the occurrence of trauma and surgical intervention was variable with an average of 2 days (range, 0–5 days). The etiology of the fractures was road traffic accident in 10 patients (83.3%) and falls in 2 patients (16.7%). These patients had 14 fractures (10 single and 2 double): 2 symphyseal, 6 parasymphyseal, 3 bodies, and 3 angle fractures. Fractures were undisplaced in three cases, slightly displaced in four cases, and severely displaced in seven cases. The mean hospital stay was 4 days. The number of plates used per patient ranged from one to two, and the number of screws from four to eight.
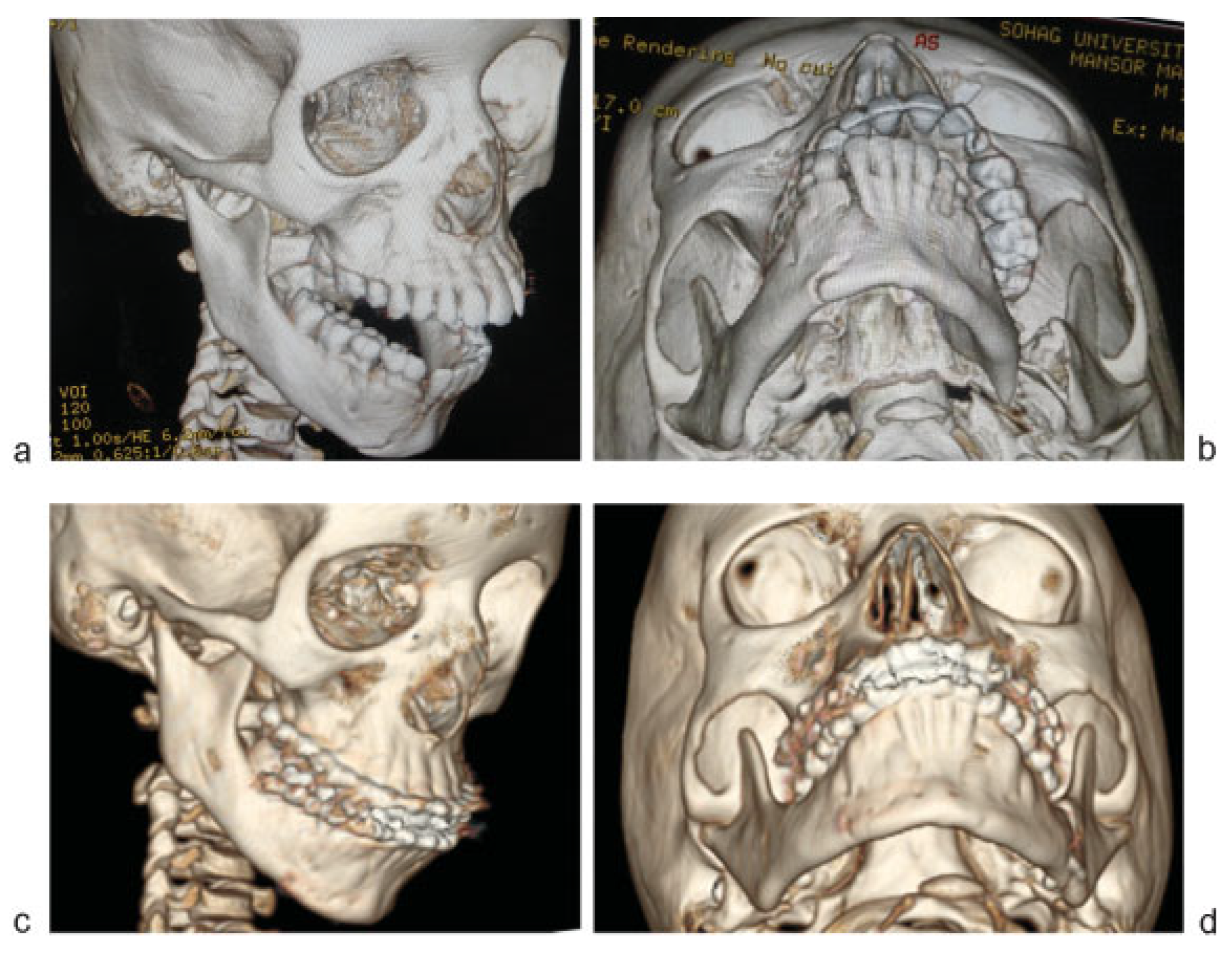
Healing of soft tissue was good in all patients except two patients had buccal wound dehiscence after 1 week. After 6 weeks, only one patient had dehiscence with 1 cm exposed bone which was managed conservatively by mouth wash and antibiotics. This patient had a bad oral hygiene and complete healing was reported at the 3 months follow-up visit. The radiographic follow-up of all the patients showed good bone healing without any signs of instability of the fixation (
Figure 3 and
Figure 4). Other complications such as mouth opening limitation and TMJ ankylosis were not identified. No disturbances of sensation were observed. During the follow-up, no evidence of tissue intolerance or malocclusion was noticed. Normal occlusion could be restored in all the cases (
Figure 5).
In all the cases, the biodegradable fixation system provided enough stability to enablebonehealing both clinicallyandradio-logically. The clinical outcome was excellent in 11 of the 12 cases (91.6%). The complication reported did not affect bone healing.
Discussion
Beside the average, 13% removal rate with the use of titanium plates due to complications, the metal plates in children should be removed routinely to avoid the possibility of growth restriction. The use of biodegradable materials provides children the advantage to avoid undergoing a second surgery to remove the metal plates.
Many biodegradable materials have been proved to be reliable in numerous studies such as polydioxanone, polyglycolic acid (PGA), poly-
l-lactic acid (PLLA), poly-
l/
d-lactic acid (PLDLA), and their copolymers.[
7]
Several studies reported the use of biodegradable plates and screws for craniomaxillofacial osteosynthesis. Self-reinforced polylactide materials (lag screws) were formerly used for fixation of sagittal split osteotomies of the mandible with good results.[
9] Turvey et al[
10] used SR-P(L/DL)LA plates and screws for fixation of 336 osteotomies of the maxilla and mandible in 130 orthognathic patients, concluding the efficiency of this material. The material showed enough initial strength to ensure stability of bone segments. At 15 months, the drill holes were filled with bone. Resorption of the material was complete by 2 to 3 years. Ylikontiola et al[
11] used SR-PLDLA plates for the fixation of anterior mandibular fractures in 10 patients. The patients were followed for 3 to 6 months with good bone and soft tissue healing and only a minor complication was reported in one patient. Leonhardt et al[
8] also used SR-PLDLA (INION) plates for the fixation of mandibular fractures in 30 patients with heterogeneous age group with a mean follow-up period of 6 months. All the fractures healed both clinically and radiologically. All patients had perfect occlusions. No serious complications were reported in any of these studies and long-term stability was comparable to clinical reports on metallic devices.
In this study, we used self-reinforced material. The self-reinforcing technique enables the formation of small devices of ultra-high strength and bending tolerability. In this technique, a composite structure is made of a polymeric matrix reinforced with oriented reinforcing units. These units are in the form of fibrils or fibers arranged in the orientation of the axis and have the same chemical structure as the matrix itself.[
12]
Earlier, it was not possible to apply bioresorbable materials in mandibular fractures due to their lower strength than the metal systems. The self-reinforcement technique improved the biomechanical characteristics of plates and screws and increased their strength.[
7] In spite of the smaller size of these plates and screws compared with nonreinforced devices; they show high bending strength due to the self-reinforcement technology.[
11] SR plates of the copolymer poly (L/DL) lactide are stronger than other commercially available biodegradable plates.[
10] These self-reinforced biodegradable plates and screws can give adequate strength and stability for fixation of bone even in high-load areas such as the mandible.[
13] Only the Inion plates are approved by the US Food and Drug Administration (FDA) for fixation of mandibular fractures with an appropriate period of MMF.[
14]
The data presented show that the biodegradable INION system gives sufficient stability to allow bone healing. All fractures in this series healed successfully. As the PLDLA materials gain their final stability after 3 days in place; to reach a biomechanical rigidity similar to that of titanium plates,[
15] we kept the MMF for a period of 1 week postoperative to prevent early instability. The FDA recommends not using the biodegradable plates in the mandible without an appropriate period of MMF.[
16]
In this series, two cases developed buccal wound dehiscence (2/12) which did not affect bone healing. This incidence is comparable to the incidence reported in other studies.[
17] Adequate soft tissue coverage prevents problems with healing and plate exposure. If implant exposure occur, the exposed part can be excised after fracture healing, which takes 6 to 8 weeks. On the contrary, exposure of titanium plates represents a more problematic situation which can be managed conservatively or may require removal of the whole plate and screws in some cases.[
18]
The copolymer PLDLA has a resorption time of 2 to 3 years. The degradation of polylactic acid involves hydrolytic enzymes.[
19] There is a transient foreign body reaction which is responsible for the postoperative swelling. However, these foreign body reactions have a lower incidence and are rarely clinically manifested with SR devices in comparison with the ordinary PGA or PLLA.[
12]
The blunt tips of the biodegradable screws and their eventual degradation reduce the harm on the developing teeth particularly in young children in the primary and mixed dentition periods. Another advantage is that the biodegradable materials are radiolucent and do not interfere with imaging techniques.
The advantages of biodegradable plates avoiding the burden of removing the titanium plates (cost, time, further painful procedure for plate removal, much scar tissue formation) outweigh its disadvantages (cost and more difficult operative technique).
Conclusions
Biodegradable SR-PLDLA plates and screws can give the initial strength needed for fixation of mandibular fractures followed by degradation and elimination from the body. The use of biodegradable osteofixation devices avoids secondary surgery to remove the plates and therefore reduce the overall cost. This also avoids the possible allergic reactions, cold sensitivity, pain, irritation, infection, and palpability of the metal plate. This is also associated with decreased physical and psychological trauma to the child. However, further clinical studies are needed to assess the long-term results of mandibular fractures treatment with biodegradable systems.