Management Issues in the Treatment of an Ameloblastoma with an Atypical Presentation
Abstract
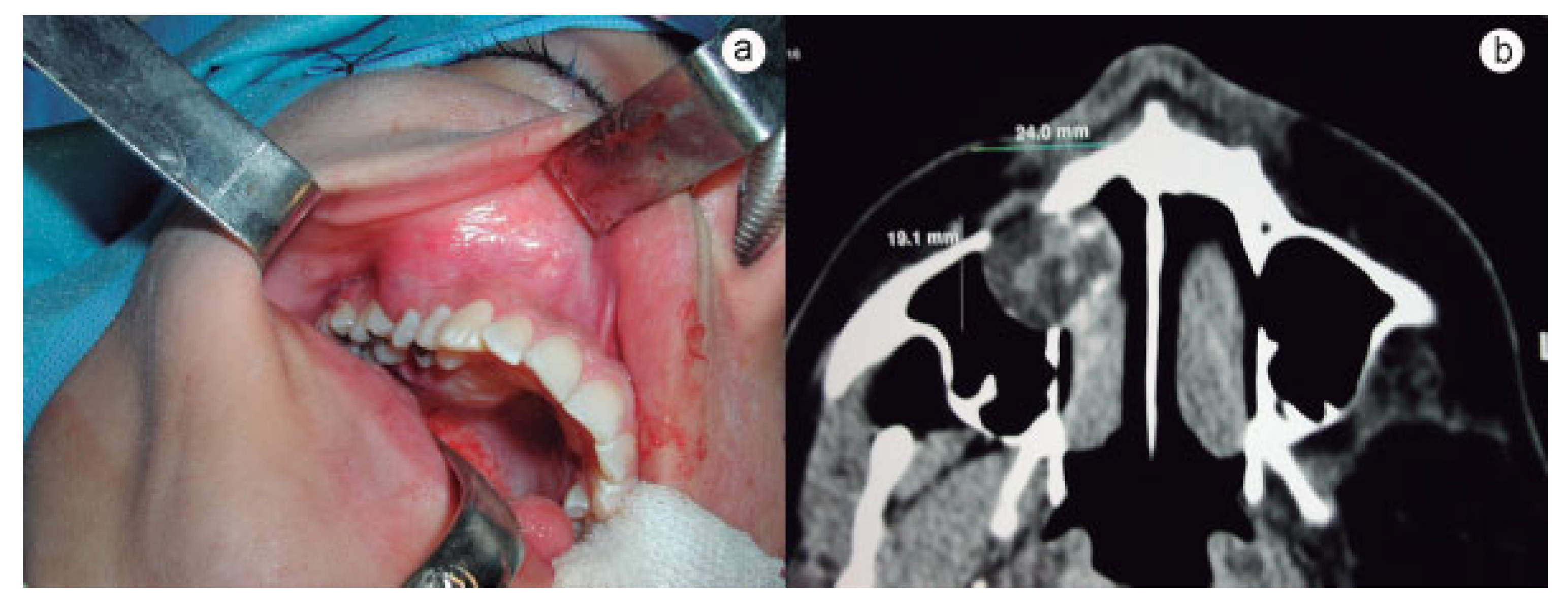
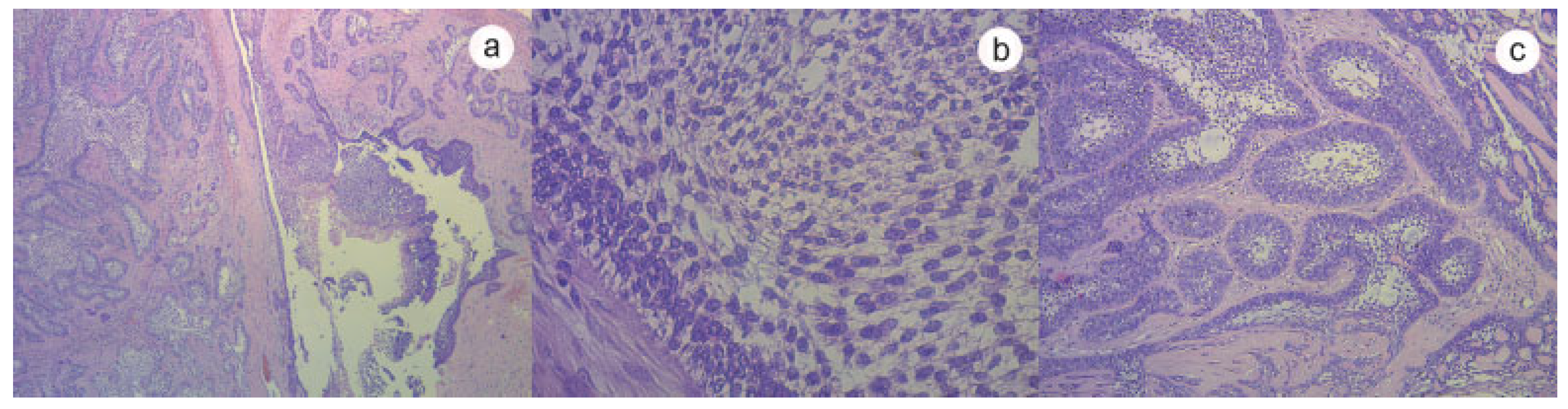
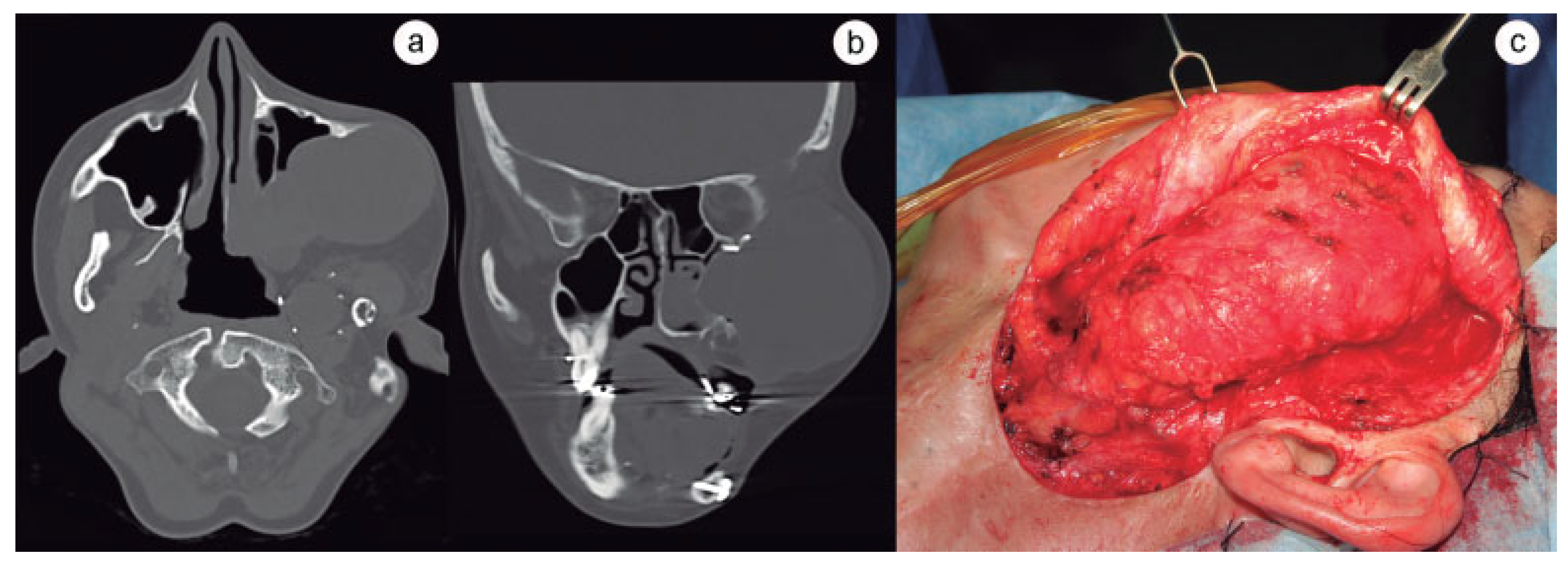
:Case History
Discussion


 |
Acknowledgments
References
- Adebayo, E.T.; Fomete, B.; Adekeye, E.O. Delayed soft tissue recurrence after treatment of ameloblastoma in a black African: Case report and review of the literature. J Craniomaxillofac Surg 2011, 39, 615–618. [Google Scholar] [CrossRef] [PubMed]
- Verneuil, A.; Sapp, P.; Huang, C.; Abemayor, E. Malignant ameloblastoma: Classification, diagnostic, and therapeutic challenges. Am J Otolaryngol 2002, 23, 44–48. [Google Scholar] [CrossRef] [PubMed]
- Goldenberg, D.; Sciubba, J.; Koch, W.; Tufano, R.P. Malignant odontogenic tumors: A 22-year experience. Laryngoscope 2004, 114, 1770–1774. [Google Scholar] [CrossRef] [PubMed]
- Duffey, D.C.; Bailet, J.W.; Newman, A. Ameloblastoma of the mandible with cervical lymph node metastasis. Am J Otolaryngol 1995, 16, 66–73. [Google Scholar] [CrossRef] [PubMed]
- Houston, G.; Davenport, W.; Keaton, W.; Harris, S. Malignant (metastatic) ameloblastoma: Report of a case. J Oral Maxillofac Surg 1993, 51, 1152–1155, discussion 1156–1157. [Google Scholar] [CrossRef] [PubMed]
- Berger, A.J.; Son, J.; Desai, N.K. Malignant ameloblastoma: Concurrent presentation of primary and distant disease and review of the literature. J Oral Maxillofac Surg 2012, 70, 2316–2326. [Google Scholar] [CrossRef] [PubMed]
- Inoue, N.; Shimojyo, M.; Iwai, H.; et al. Malignant ameloblastoma with pulmonary metastasis and hypercalcemia. Report of an autopsy case and review of the literature. Am J Clin Pathol 1988, 90, 474–481. [Google Scholar] [CrossRef] [PubMed]
- Emura, M. A case of metastatic ameloblastoma. Jpn J Surg 1923, 24, 760. [Google Scholar]
- Vorzimer, J.; Perla, D. An instance of adamantinoma of the jaw with metastases to the right lung. Am J Pathol 1932, 8, 445,3. [Google Scholar]
- Lin, Y.; He, J.F.; Li, Z.Y.; Liu, J.H. Ameloblastoma with varied sites of metastasis: Report of two cases and literature review. J Craniomaxillofac Surg 2014, 42, e301–e304. [Google Scholar] [CrossRef] [PubMed]
- Jayaraj, G.; Sherlin, H.J.; Ramani, P.; et al. Metastasizing ameloblastoma—A perennial pathological enigma? Report of a case and review of literature. J Craniomaxillofac Surg 2014, 42, 772–779. [Google Scholar] [CrossRef] [PubMed]
- Van Dam, S.D.; Unni, K.K.; Keller, E.E. Metastasizing (malignant) ameloblastoma: Review of a unique histopathologic entity and report of Mayo Clinic experience. J Oral Maxillofac Surg 2010, 68, 2962–2974. [Google Scholar] [CrossRef] [PubMed]
- Sciubba, J.J.; Eversole, L.R.; Slootweg, P.J. Odontogenic/ameloblastic carcinomas. In World Health Organization Classification of Tumours; Barnes, L., Eveson, J.W., Reichart, P., Sidransky, Eds.; Pathology and Genetics of Head and Neck Tumours; IARC Press: Lyon, France, 2005; pp. 287–e289. [Google Scholar]
- Ueta, E.; Yoneda, K.; Ohno, A.; Osaki, T. Intraosseous carcinoma arising from mandibular ameloblastoma with progressive invasion and pulmonary metastasis. Int J Oral Maxillofac Surg 1996, 25, 370–372. [Google Scholar] [CrossRef] [PubMed]
- Zwahlen, R.A.; Grätz, K.W. Maxillary ameloblastomas: A review of the literature and of a 15-year database. J Craniomaxillofac Surg 2002, 30, 273–279. [Google Scholar] [CrossRef] [PubMed]
- Steinhäuser, E. An ameloblastoma with distant metastases. Fortschr Kiefer Gesichtschir 1972, 15, 202–206. [Google Scholar] [PubMed]
- Devenney-Cakir, B.; Dunfee, B.; Subramaniam, R.; et al. Ameloblastic carcinoma of the mandible with metastasis to the skull and lung: Advanced imaging appearance including computed tomography, magnetic resonance imaging and positron emission tomography computed tomography. Dentomaxillofac Radiol 2010, 39, 449–453. [Google Scholar] [CrossRef] [PubMed]
- Dao, T.V.; Bastidas, J.A.; Kelsch, R.; Kraut, R.A. Malignant ameloblastoma: A case report of a recent onset of neck swelling in a patient with a previously treated ameloblastoma. J Oral Maxillofac Surg 2009, 67, 2685–2689. [Google Scholar] [CrossRef] [PubMed]
- Henderson, J.M.; Sonnet, J.R.; Schlesinger, C.; Ord, R.A. Pulmonary metastasis of ameloblastoma: Case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1999, 88, 170–176. [Google Scholar] [PubMed]
- Laughlin, E.H. Metastasizing ameloblastoma. Cancer 1989, 64, 776–780. [Google Scholar] [CrossRef] [PubMed]
- Amzerin, M.; Fadoukhair, Z.; Belbaraka, R.; et al. Metastatic ameloblastoma responding to combination chemotherapy: Case report and review of the literature. J Med Case Rep. 2011, 5, 491. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the author. The Author(s) 2015.
Share and Cite
Larrañaga, J.J.; Sahovaler, A.; Picco, P.I.; Mazzaro, E.L.; Figari, M.F. Management Issues in the Treatment of an Ameloblastoma with an Atypical Presentation. Craniomaxillofac. Trauma Reconstr. 2015, 8, 257-261. https://doi.org/10.1055/s-0035-1549012
Larrañaga JJ, Sahovaler A, Picco PI, Mazzaro EL, Figari MF. Management Issues in the Treatment of an Ameloblastoma with an Atypical Presentation. Craniomaxillofacial Trauma & Reconstruction. 2015; 8(3):257-261. https://doi.org/10.1055/s-0035-1549012
Chicago/Turabian StyleLarrañaga, Juan José, Axel Sahovaler, Pedro Ignacio Picco, Eduardo Luis Mazzaro, and Marcelo Fernando Figari. 2015. "Management Issues in the Treatment of an Ameloblastoma with an Atypical Presentation" Craniomaxillofacial Trauma & Reconstruction 8, no. 3: 257-261. https://doi.org/10.1055/s-0035-1549012
APA StyleLarrañaga, J. J., Sahovaler, A., Picco, P. I., Mazzaro, E. L., & Figari, M. F. (2015). Management Issues in the Treatment of an Ameloblastoma with an Atypical Presentation. Craniomaxillofacial Trauma & Reconstruction, 8(3), 257-261. https://doi.org/10.1055/s-0035-1549012



