Abstract
The primary goals in repairing complex craniofacial fractures are restoration of occlusion and mastication, and anatomic reconstruction of a symmetric facial skeleton. Failure to accomplish these goals may result in the need for secondary operations. Recognition of malreduction may not be appreciated until review of a postoperative computed tomographic (CT) scan. Intraoperative CT scanning enables immediate on-table assessment of reduction and fixation, allowing alteration of the surgical plan as needed. We report using intraoperative CT scanning while repairing a panfacial injury in which malreduction was appreciated intraoperatively and corrected. Intraoperative CT can be used to improve outcomes and quality of complex facial fracture repair.
Repair of complex craniofacial fractures involves more than simply “putting the pieces together.” Goals include restoration of occlusion, mastication [1], and reconstruction of an esthetic and symmetric facial skeleton [2]. Injuries are well managed with the craniofacial principles of wide subperiosteal exposure, anatomic reduction, and rigid internal fixation [3]. Visual inspection alone, particularly in complex injuries, may not fully demonstrate the adequacy of fracture reduction, requiring the use of a postoperative computed tomography (CT) scan [4]. If fracture alignment is not adequate, secondary operations may be required [5].
Intraoperative CT technology has been used by other surgical specialties for many years, and has been shown to change intraoperative decision making in orthopedic surgery, spine surgery, and neurosurgery by earlier assessment of outcome and immediate intervention when warranted [6,7]. Stanley [8] described the use of intraoperative CT in craniofacial reconstruction in 1999 specifically in orbitozygomatic injuries, and the indications continue to expand [9]. Our goal is to explore the use of this technology in complex craniofacial trauma and present a case in which early recognition of inadequate reduction intraoperatively enabled on-table correction and improved outcome.
Case Report
A 42-year-old male was involved in an unhelmeted motorcycle accident. Emergency CT scan demonstrated intracranial hemorrhage, as well as panfacial fractures including the right frontal bone and sinus, right orbital roof, right orbitozygomaticomaxillary complex, bilateral Le Fort I/II, bilateral nasoorbital-ethmoid, palatal, and a comminuted parasymphyseal mandible fractures with a median wedge fragment (Figure 1). He also had right globe rupture. He was taken emergently to the operating room for decompressive right frontal craniectomy and tracheostomy.

Figure 1.
The patient’s computed tomographic scan after decompressive craniectomy but before facial fracture fixation.
After stabilization of his life-threatening injuries, he was taken back to the operating room by plastic surgeon with the help of neurosurgeon and ophthalmologist. He underwent enucleation of the right globe with conformer placement, repair of a dural laceration, cranialization of his frontal sinus, obliteration of the nasofrontal ducts, frontal skull reconstruction with calvarial bone grafting, and open reduction internal fixation (ORIF) of his panfacial fractures.
Following wide subperiosteal elevation and exposure of all upper, middle, and lower facial fractures, we began our reconstruction with the mandible to restore the occlusal relationship and establish a platform on which to reconstruct the remaining facial fractures. Through an intraoral incision, we reduced the comminuted parasymphyseal mandible fracture, specifically with the goal of avoiding splaying on the lingual aspect of the fracture. The maxillary arch was not available as a guide to proper mandibular arch width due to the maxillary and palatal fractures. We applied arch bars and circumdental wires and re-established what we believed to be centric relation and centric occlusion, despite the extensive mandibular, maxillary, and palatal fractures. We then applied intermaxillary fixation and related the maxillary dentition to the reduced mandible. On the mandible, we placed an upper border tension band plate with monocortical screws and a lower border reconstruction plate with lag screws across the oblique portion of the comminuted symphyseal fracture and locking bicortical screws in the remaining plate. Because all subsequent midfacial fracture fixation and facial width would rely upon precise anatomic reduction of the mandible, we next obtained an intraoperative CT scan using the BodyTom CT scanner (Neurologica Corp., Danvers, MA). Despite efforts to properly reduce the symphyseal fracture with lag and locking screws, the intraoperative CT elucidated splaying at the lingual surface of the mandibular fracture and dislocation of the right condyle, which could not be viewed directly through the intraoral approach (Figure 2). Early CT recognition of this malreduction allowed revision before potentially performing sequential operative errors with broadening of the middle and upper face due to an increased intercondylar distance.
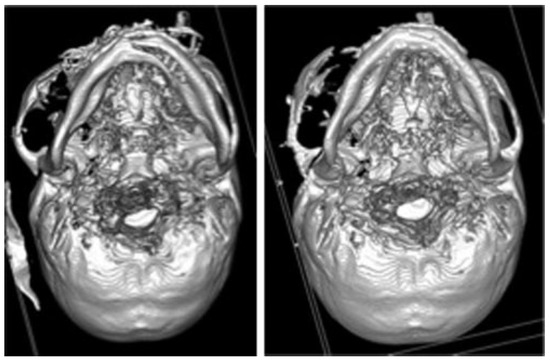
Figure 2.
(Left) Intraoperative CT scan after mandibular reduction and fixation demonstrates a classic example of splaying at the lingual surface of the oblique parasymphyseal mandibular fracture by the bicortical screws. The result is an increased intercondylar distance with right condylar dislocation from the mandibular fossa. (Right) Intraoperative CT scan after re-reduction and fixation of the oblique parasymphyseal mandibular fracture. Proper anatomic fracture reduction and fixation is confirmed with appropriate intercondylar distance and centric relation with the right condyle reduced in the mandibular fossa. CT, computed tomography.
Using this information, we removed our mandibular hardware and re-reduced and re-plated the mandibular fractures. Repeat CT confirmed anatomic reduction of the fracture and relocation of the right condyle with proper intercondylar distance (Figure 2). With restoration of proper centric occlusion and centric relation while in intermaxillary fixation, we related, then fixed the midface beginning with the less severe left maxillary fractures as they were a more stable point of fixation. Finally, we fixed the upper facial skeleton, including cranialization of the frontal sinus, obliteration of the nasofrontal ducts with cortical and cancellous bone and a vascularized pericranial flap, repair of the dural lacerations with a vascularized pericranial flap, construction of a right orbital rim and roof with split cranium, and fixation of the naso-orbital-ethmoid fractures. At the conclusion of the operation, we released intermaxillary fixation and confirmed restoration of centric occlusion and relation. Postoperative CT demonstrated satisfactory reduction and fixation (Figure 3). The patient had no postoperative complications, demonstrated significant neurologic recovery, and subsequently underwent elective frontal cranioplasty with a custom implant.
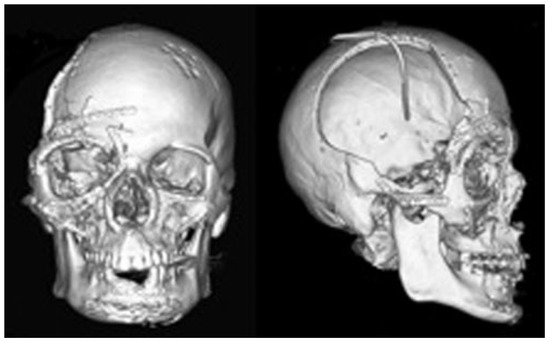
Figure 3.
Postoperative computed tomographic scan with adequate bony reduction. Although the right globe was enucleated, critical review demonstrates a relatively enlarged right orbit, which was reconstructed along the superior orbital rim and roof with split calvarial bone.
Discussion
The use of a technology in surgical practice relies on its ability to ultimately improve outcomes, quality, and safety for our patients. Many patients with complex facial injuries have been well managed over the years using classic craniofacial principles [3,10]. Nevertheless, some patients require secondary operations [5,11], due to malreduction, which may have been prevented if recognized intraoperatively.
We provide a case example demonstrating how intraoperative CT technology can improve intraoperative decision making and quality of outcomes by preventing surgical errors in reduction. The intraoperative CT allowed immediate detection, correction, confirmation of reduction, and confidence to proceed by knowing we had appropriately reduced the mandible, intercondylar distance, and lower facial width. Previous studies on small cohorts of craniofacial trauma patients have also demonstrated that intraoperative CT resulted in real-time alterations in the surgical plan [4,12,13]. On the contrary, delayed recognition by postoperative imaging is disappointing and may require return to the operating room for preventable secondary operations.
In our experience, using intraoperative CT adds little operative time, taking approximately 5 additional minutes per scan. Others have also reported the efficiency of intraoperative CT scans [8,9]. Overall, it may shorten operative time and be more cost-effective by immediately establishing the outcome of surgical maneuvers without wasted time in indecision or need to secondarily correct surgical errors. A prospective trial comparing operative time, cost, and outcome of reduction would be valuable. While early intraoperative CT technology such as cone beam CT and fan beam scanners with small gantries only allowed limited views, modern fan beam scanners such as the one in this case provide axial, coronal, and sagittal reconstructions as well as three-dimensional reformats to further aid in real-time assessment [9]
Potential limitations in the use of intraoperative CT scanners include access to the machines themselves, and the need to have a radiology technician available to perform the scanning. We were fortunate that our hospital recently purchased the machine for neurosurgical operations and so using it for our purposes in craniofacial trauma was straightforward.
As CT use rises [14], there is growing concern regarding the amount of radiation exposure to the patient. Because we are interested primarily in bony anatomy when using the CT for traumatic craniofacial reconstruction, we are able to use lower doses of radiation with bone windows only.
In addition to intraoperative CT, there are other options to assess anatomic reduction. An extraoral incision, for example, provides more direct evaluation of the lingual surface of the symphysis. Nevertheless, this incision has additional risk of injury to the marginal mandibular branch of the facial nerve and creates a visible cutaneous scar. Another option is to change the operative sequence of panfacial fractures and begin with more stable points in the midface rather than the mandible. In the patient we present, some surgeons may have preferred to begin with the more stable left midface, to which the mandible and other facial fractures could then be related. We prefer to begin our reduction and fixation with the mandible, which then serves as a stable platform on which to build the remaining craniofacial skeleton. Finally, other forms of technology, such as intraoperative navigation [15] have been described as adjuncts to assess anatomic reduction of the craniofacial skeleton. Intraoperative navigation is particularly useful when reduction can be based on a mirror image of the contralateral uninjured structures, such as the zygomaticomaxillary complex or orbit. Navigation for panfacial injuries is limited by the lack of uninjured contralateral structures on which to base a mirrored reconstruction. In conclusion, we feel that using intraoperative CT for complex craniofacial fractures provides efficient and valuable information for assessing anatomic reduction and fixation, while permitting immediate revision if needed. Clearly, it is not an appropriate utilization of resources to use this technology in every facial trauma operation, but in complex injuries with loss of normal landmarks guiding anatomic reduction, its use may be warranted. Our early experience with this technology leads us to believe that it improves operative efficiency by establishing confidence in reduction and can improve outcomes for our patients by decreasing the need for secondary operations.
Conflicts of Interest
The authors have no conflicts of interest to disclose.
References
- Ellis, E., III; Miles, B.A. Fractures of the mandible: A technical perspective. Plast Reconstr Surg 2007, 120 (Suppl. S2), 76S–89S. [Google Scholar] [CrossRef] [PubMed]
- Kelley, P.; Hopper, R.; Gruss, J. Evaluation and treatment of zygomatic fractures. Plast Reconstr Surg 2007, 120 (Suppl. S2), 5S–15S. [Google Scholar] [CrossRef] [PubMed]
- Manson, P.N.; Clark, N.; Robertson, B.; Crawley, W.A. Comprehensive management of pan-facial fractures. J Craniomaxillofac Trauma 1995, 1, 43–56. [Google Scholar] [PubMed]
- Rabie, A.; Ibrahim, A.M.; Lee, B.T.; Lin, S.J. Use of intraoperative computed tomography in complex facial fracture reduction and fixation. J Craniofac Surg 2011, 22, 1466–1467. [Google Scholar] [CrossRef] [PubMed]
- Buchanan, E.P.; Hopper, R.A.; Suver, D.W.; Hayes, A.G.; Gruss, J.S.; Birgfeld, C.B. Zygomaticomaxillary complex fractures and their association with naso-orbito-ethmoid fractures: A 5-year review. Plast Reconstr Surg 2012, 130, 1296–1304. [Google Scholar] [CrossRef] [PubMed]
- Holly, L.T.; Foley, K.T. Intraoperative spinal navigation. Spine 2003, 28, S54–S61. [Google Scholar] [CrossRef] [PubMed]
- Carlson, A.P.; Phelps, J.; Yonas, H. Alterations in surgical plan based on intraoperative portable head computed tomography imaging. J Neuroimaging 2012, 22, 324–328. [Google Scholar] [CrossRef] [PubMed]
- Stanley, R.B., Jr. Use of intraoperative computed tomography during repair of orbitozygomatic fractures. Arch Facial Plast Surg 1999, 1, 19–24. [Google Scholar] [CrossRef] [PubMed]
- Strong, E.B. Intraoperative computed tomography for repair of facial fractures. Arch Facial Plast Surg 2012, 14, 159–161. [Google Scholar] [CrossRef] [PubMed]
- Gruss, J.S.; Bubak, P.J.; Egbert, M.A. Craniofacial fractures. An algorithm to optimize results. Clin Plast Surg 1992, 19, 195–206. [Google Scholar] [CrossRef] [PubMed]
- Imola, M.J.; Ducic, Y.; Adelson, R.T. The secondary correction of posttraumatic craniofacial deformities. Otolaryngol Head Neck Surg 2008, 139, 654–660. [Google Scholar] [CrossRef] [PubMed]
- Hoelzle, F.; Klein, M.; Schwerdtner, O.; et al. Intraoperative computed tomography with the mobile CT Tomoscan M during surgical treatment of orbital fractures. Int J Oral Maxillofac Surg 2001, 30, 26–31. [Google Scholar] [CrossRef] [PubMed]
- DeFatta, R.J.; Ducic, Y.; Adelson, R.T.; Sabatini, P.R. Comparison of closed reduction alone versus primary open repair of acute nasoseptal fractures. J Otolaryngol Head Neck Surg 2008, 37, 502–506. [Google Scholar] [PubMed]
- Brenner, D.J. Should we be concerned about the rapid increase in CT usage? Rev Environ Health 2010, 25, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Morrison, C.S.; Taylor, H.O.; Sullivan, S.R. Utilization of intraoperative 3D navigation for delayed reconstruction of orbitozygomatic complex fractures. J Craniofac Surg 2013, 24, e284–e286. [Google Scholar] [CrossRef] [PubMed]
© 2014 by the author. The Author(s) 2014.