Orbital roof fractures in adults are rare and often associated with high-impact trauma to the head and face. The life-threatening injuries should be stabilized first, followed by managing the craniofacial fractures by a multidisciplinary team [
1,
2,
3].
A distinction is made between isolated and nonisolated orbital roof fractures. In the nonisolated cases, most of the literature recommends early reconstruction [
3,
4,
5]. This early surgical intervention is presumed necessary to prevent meningitis, encephalocele, and brain abscess formation [
1,
6,
7] and would provide a better function and cosmetic result. With regard to the isolated orbital roof fractures, the nondisplaced versus the displaced types must be distinguished. In general, the displaced fractures are also recommended to be reconstructed immediately [
2,
3,
8,
9] and only the nondisplaced fractures are regarded not to be in need of surgical intervention [
1,
2,
3]. This difference lies in the assumption that a nondisplaced fracture has a lower incidence of ocular and neurological complications (e.g., exophthalmus/hyperglobus, enophthalmus/hypoglobus, proptosis, diplopia, restricted eye movement, vision loss, pain, and discomfort) [
1,
2,
3].
In this article, we present four cases of displaced orbital roof fractures that were not surgically treated. In these cases, a “wait and see” policy was followed by keeping the patient under observation. The outcome of the follow-up of these patients sheds an interesting light on the question, “should we indeed treat these fractures immediately, as literature dictates, or is a ‘wait and see’ approach justifiable?”
Case Reports
Case 1
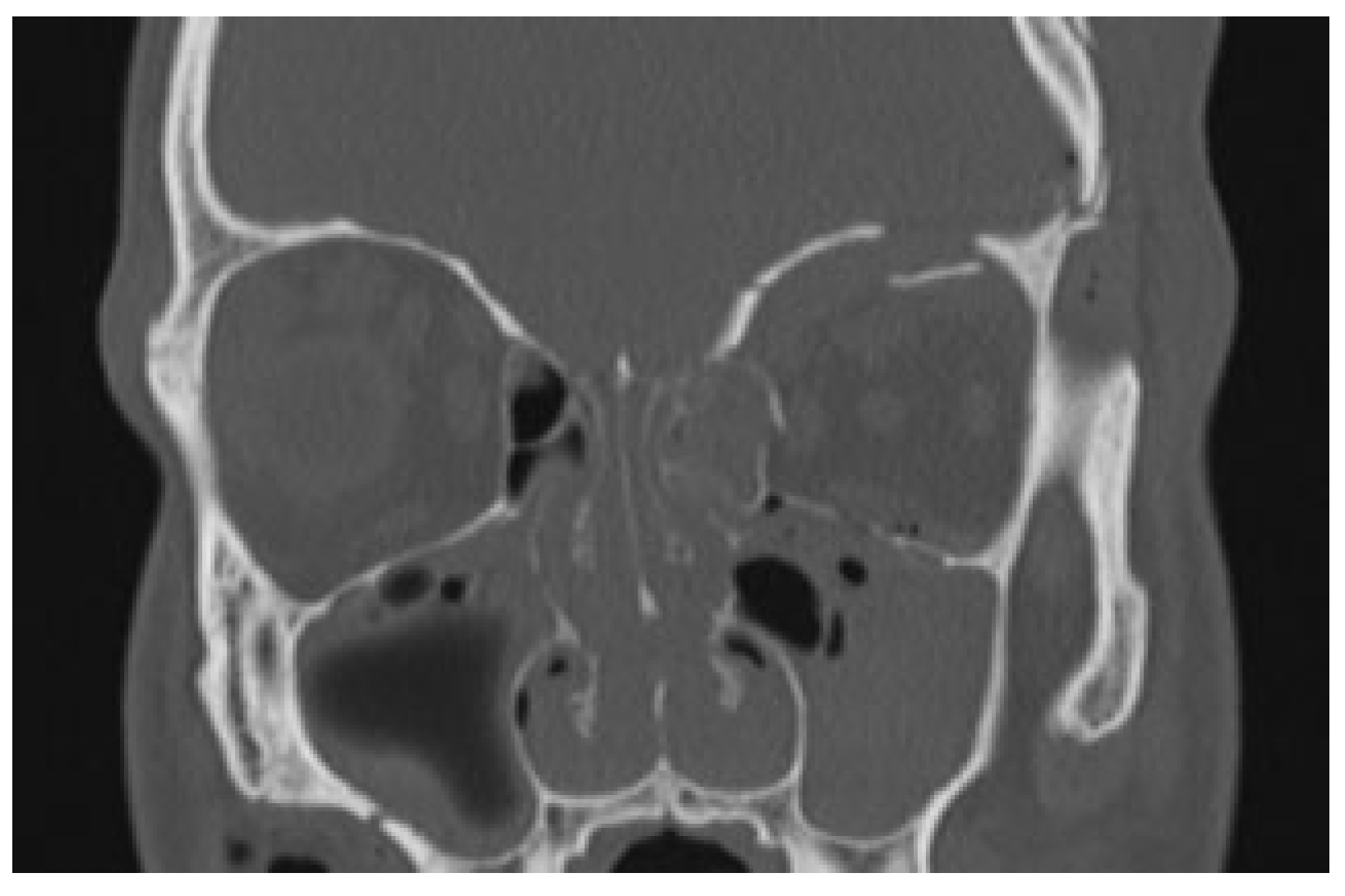
The first case is about a 22-year-old male who was involved in a high-energy trauma, scooter versus parked car. When the ambulance arrived, the patient had a maximal Glasgow coma scale despite of the fact that he had not been wearing a helmet. The patient was seen according the Advanced Trauma Life Support protocol. During the primary survey in the emergency room, there were no evident injuries to the neck, chest, abdomen, or extremities. In addition, the patient had no vision loss, no diplopia, and the sensitivity of the forehead was intact. The computed tomography (CT) showed an impression of the left frontal bone with contusion of the brain and an orbital medial wall fracture without dislocation on the left side and an orbital roof fracture on the left side with downward displacement of the fragment (
Figure 1 and
Figure 2) Despite the dislocated orbital roof fracture, it was decided to keep him under observation.
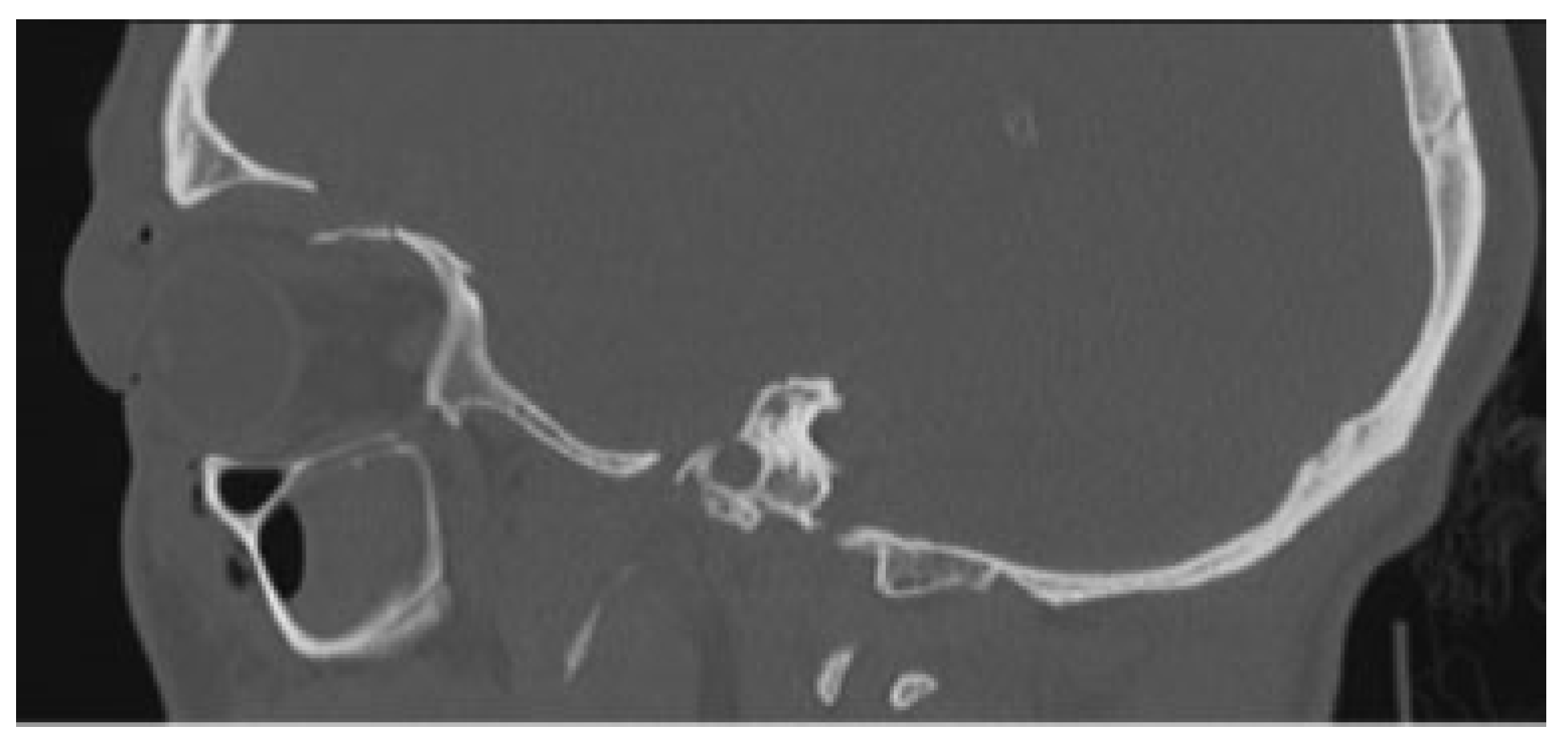
During follow-up, 2 weeks, 2.5, 9 months, and 1 year following the trauma, there were no functional or esthetic problems. CT scan obtained 1 year after trauma showed complete reposition of the left orbital roof fracture (
Figure 3 and
Figure 4).
Case 2
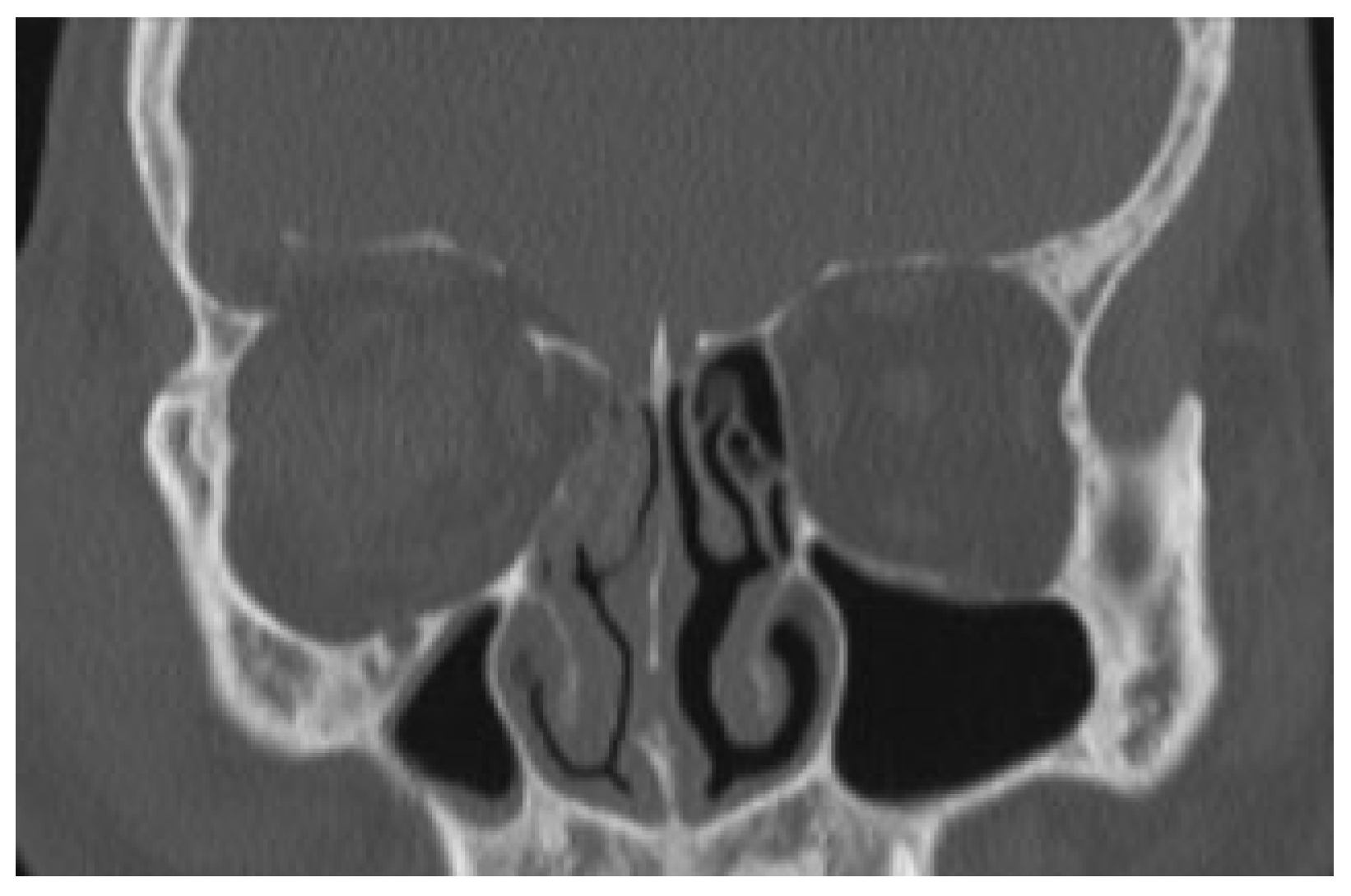
The second case is a 37-year-old male who got into a fight in April 2012. When he arrived at the emergency department of the Erasmus Medical Centre, the only complaint he had was the swelling around his right eye. His eyes had full range of motion, there was no vision loss, and both pupillary reflexes were normal. During further investigation, the CT scan showed a blow-out fracture of the right orbital roof with intracranial displacement of the intraorbital fat and superior rectus muscle and a fracture of the lamina papyracea (
Figure 5). The neurosurgeon was consulted regarding the intracranial displacement and he agreed with the suggested “wait and see” policy. During follow-up, 1, 4 weeks, and 4 months following the trauma, the patient had normal function of his right eye without any esthetic complaints. The cone-beam CT scan at 4 months showed a complete repositioning of the fracture (
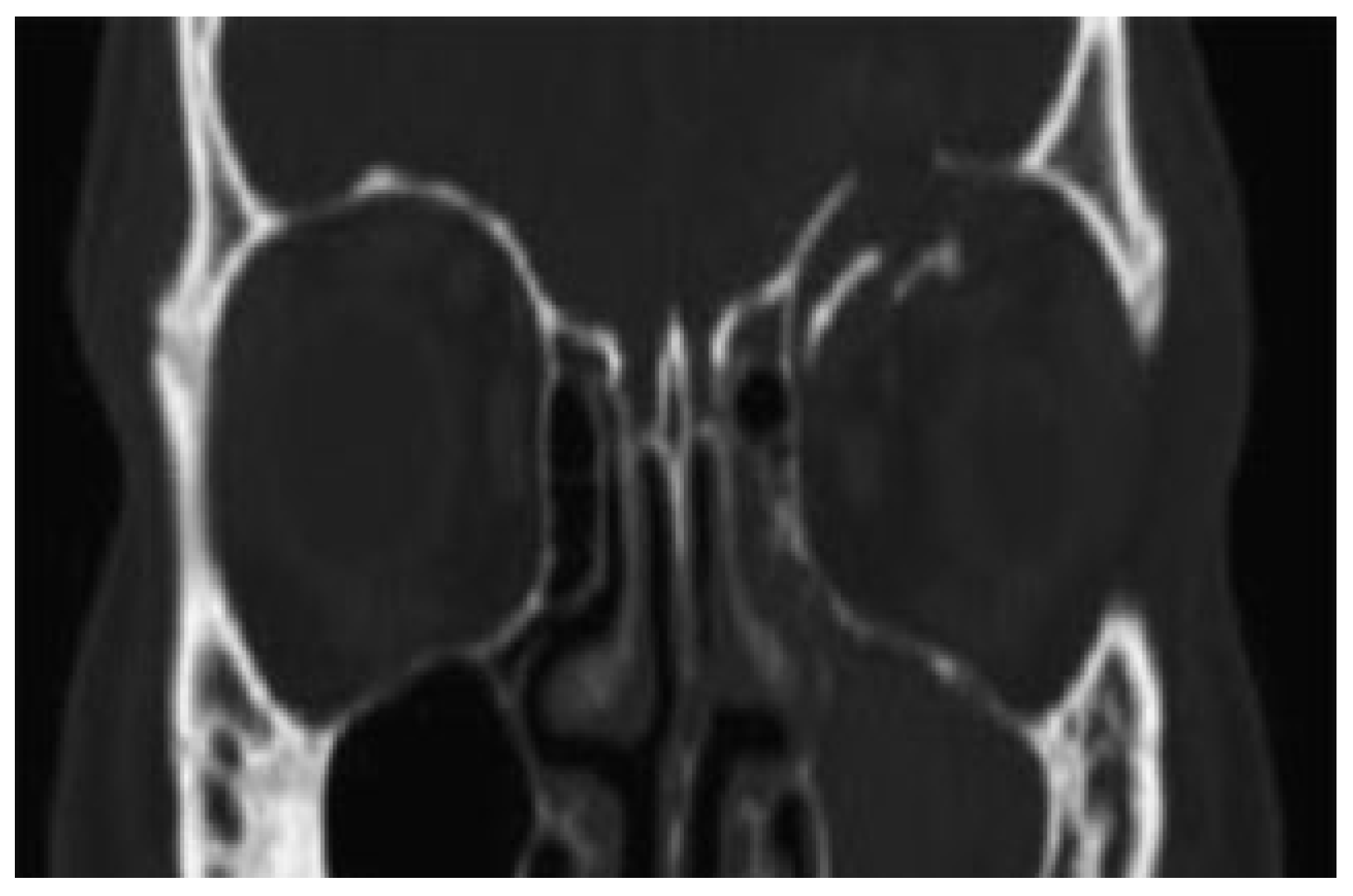
Figure 6).
Case 3
The third case is about a 17-year-old female who was an unrestrained passenger in a motor vehicle accident. She was ejected from the vehicle and sustained forehead abrasions, loss of consciousness, and an orbital roof blow in fracture which was documented on her admitting CT (
Figure 7 and
Figure 8). She was initially lethargic and regained consciousness over the next few days, without any visual problems. Based on the profound displacement of the orbital roof fractures, several members of the surgical team felt that a surgical intervention would have to be performed. Based on one of the author’s previous experience with orbital roof displacements of this nature self-correcting, a repeat CT was obtained 6 days after admission (
Figure 9 and
Figure 10) The second CT revealed an excellent anatomical alignment of the patient’s orbital fractures. Even after 6 years the patient is still doing well without any complications or surgical interventions.
Case 4
In the fourth case, a 20-year-old female was riding a motorcycle as a passenger with her husband, neither wore helmets. A deer jumped out in front of them. Due to the accident the women had a mutilated face with multiple facial fractures and a traumatic enucleation of her right eye. The CT scan (
Figure 11), made at the day of trauma, showed an upward displacement of multiple fragments of the orbital roof bilaterally and a significant orbital floor fracture on the left. The second CT scan (
Figure 12) was made only 2 weeks after the trauma and showed a complete reduction of the bilateral orbital roof fractures without any treatment. The left orbital floor was treated with an open reduction and internal fixation of the orbital floor fracture.
Discussion
Orbital roof fractures are rare in comparison with other facial fractures and even more so in their isolated form. If the orbital roof is fractured, it is often displaced downward and (maybe) associated with a retrobulbar hemorrhage [
5]. Usually, it concerns males between 20 and 40 years old who are involved in traffic accidents, violence, falling, sports, and work-related accidents or fireworks [
2,
10,
11,
12].
Kim et al. [
3], Gazioğlu et al. [
7], and Penfold et al. [
13] recommend early reconstruction in every case of orbital roof fractures, to reduce intracranial and ocular complications. Variable autologous and alloplastic materials are reposted to reconstruct the orbit. In case of coronal flap raising, the harvesting of calvarial bone is obvious. Otherwise, alloplastic materials can be applied like titanium mesh and polyethylene implants.
A clear distinction has to be made between children and adults since there are numerous differences between the bony structures present. In children, the bones are more vascularized, constitute of more cancellous bone, and are less brittle then of adults. In addition, they are lined with a stronger and thicker periosteum [
14]. As a result of this, the fracture pattern is different in children. The treatment used in adults cannot directly be extrapolated to children. In general, it is advised to be even more conservative in children to avoid disturbing growth potential, and the use of alloplastic materials is not recommended.
In the four described adult cases in this article, no surgical intervention was performed and that provides an excellent opportunity to study the natural course of displaced orbital roof fractures. The nonsurgical management seemed justified, since in all four cases no symptoms, including orbital complications like diplopia, were observed. They all showed (near) complete reduction of the fracture in younger than 1 year, even after 6 days, without complications.
A theory which might explain this finding is the equilibrium between the intraorbital and intracranial pressures repositioning and stabilizing the fractured roof in it is original position. In displaced isolated orbital roof fractures, it seems justifiable to be conservative and repeat the CT after the edema has resolved.
In conclusion, in case of an orbital roof fracture, isolated or nonisolated, with the absence of intracranial and orbital symptoms, such as diplopia or central spinal fluid leak, a nonsurgical policy can be considered. In a strict follow-up protocol for at least several weeks, the position of the orbital roof fracture can be monitored using routine CT scans. Spontaneous reduction of the displaced fractured roof can be expected. However, in case of intracranial and orbital symptoms and complications, surgical intervention is necessary and planned instantly.