Involvement of the temporomandibular joint (TMJ) in most head and neck oncological or infective processes is not common [
1]. This may be explained by the relative protective distance from most intraoral tumors that would first infiltrate the mandibular body with only late extension to the TMJ. Equally uncommon is the direct infiltration of the TMJ from cutaneous and subcutaneous tumors, but infiltration due to larger parotid tumors does occur. Metastatic oncological disease involvement of the TMJ is also not seen often and is seldom an indication for ablative surgery [
2,
3].
The TMJ may be afflicted by medial or lateral bony infiltration of the condylar head or neck that would make preservation of the condyle impossible or by infiltration from inferior, mostly due to direct spread from the vertical ramus or involvement of the surrounding soft tissues or alternatively due to involvement of the skull base and glenoid fossa [
3,
4].
Infective infiltration from the middle ear is a seldom-seen occurrence; however, conditions such as osteoradionecrosis (ORN) and osteomyelitis with condylar involvement are occasionally seen and may be an indication for condylar resection.
Preservation of the condylar head with potential benefits of growth in the growing individual and improved function is the obvious first choice in the management of tumors in this area; however, due to oncological safety and limited area for screw fixation, this approach is not always possible. The tolerance factor in various institutions regarding the required safety margin in this area may explain the various approaches in the same clinical setting. Extracorporeal attachment of the condyle to the bony component of the free flap is possible, with good function, although resorption of the condylar head is common but of apparently minor long-term consequence [
5].
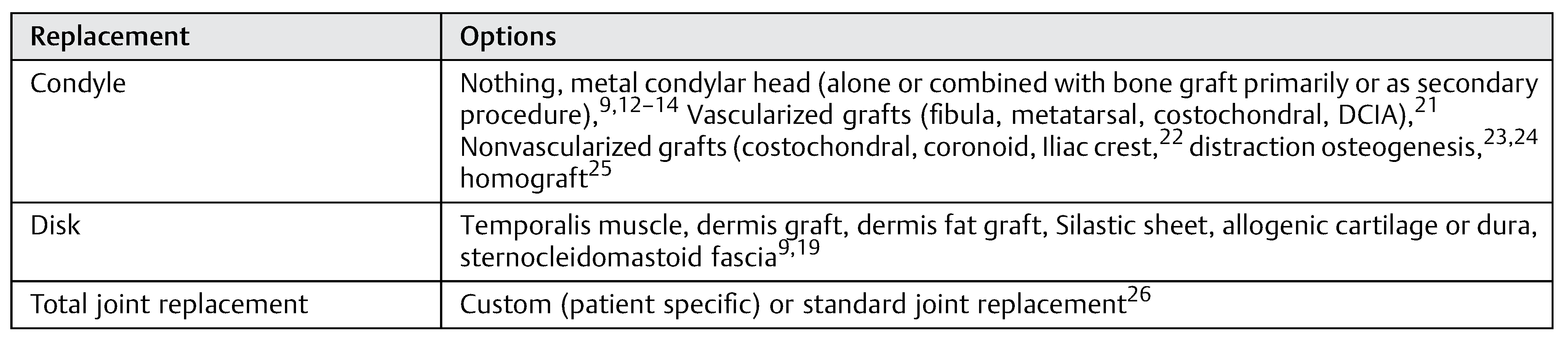
Early and late management of the involved TMJ varies greatly, ranging from no substitute, nonvascularized autologous grafts to vascularized grafts to partial or total prosthetic replacement [
6,
7,
8] (
Table 1). Despite numerous case and comparative case series reports, very few guidelines exist regarding management of resected components of the TMJ in oncological patients.
Oncological or infective indications for reconstruction of the TMJ add several compounding factors, namely, scarring and tissue loss due to previous surgery or destruction and possible poor vascularization [
1], which may lead to an increase in complications and limited function and decreased quality of life.
Even in nononcological reconstruction of the TMJ, there are challenges and significant differences in opinion as to the correct path to reconstruction. Use of autogenous tissues appears to be a possibility in a group of patients, especially those with growth potential.
Literature reports regarding guidelines for treatment selection exist but are mostly experience based and are supported by low levels of evidence. Marx et al published the largest series of 132 alloplastic condylar reconstructions in the management 131 tumor and trauma patients with the limitation of an inhomogeneous group [
9].
The aim of the study was to establish risk-based guidelines for the management of the TMJ after ablative surgery. The goal of this article is to derive a risk-based management protocol and options for the TMJ in patients after ablative surgery, excluding internal derangement cases, based on our case series as well as reports in the literature.
Patients and Methods
An analysis of all patients’ records receiving ablative surgery involving the TMJ in the Department of Cranio-Maxillofacial and Oral Surgery, University Hospital of Zürich, from 2001 to 2012, was performed and included. Exclusion criteria were the preservation of part of the condyle as well as insufficient data. A Medline- and PubMed-based literature search was done to identify all literature with the search terms “temporomandibular joint” and “reconstruction.” All studies since 1989 that obtained relevant data on reconstruction after ablative surgery were evaluated for inclusion. Excluded were all studies in which the joint resection was due to internal derangement or chronic pain. In total, seven studies showing adequate relevant information met the mentioned criteria (
Table 1).
All patients in whom surgical removal of at least the condyle was performed due to oncological or infective involvement of the TMJ were identified by a retrospective chart review. Included in this group were not only primary but also patients treated secondary to the primary ablative surgery. The following information was extracted from the records: age, gender, initial diagnosis, indication for reconstruction, radiation therapy or not, reconstructive method, primary or secondary reconstruction, complications, and function (
Table 2). Based on our own experiences and the literature, a “risk for complication”-based workflow of reconstructive options was derived.
Results
In 15 patients, 14 ablative surgical interventions were recorded, with 14 receiving primary or secondary reconstructive procedures; in one patient, no reconstructive procedure was performed due to a compounding medical condition (
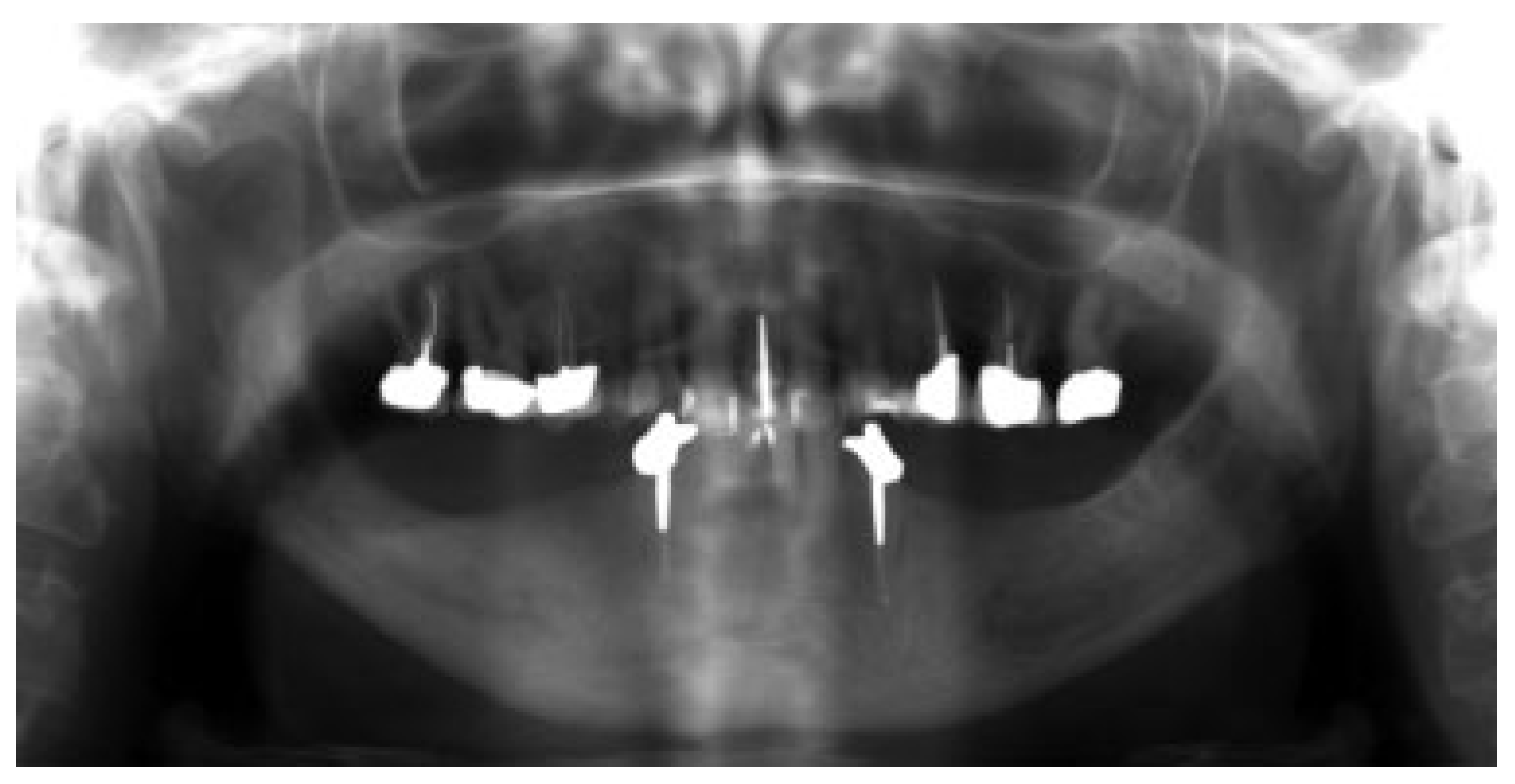
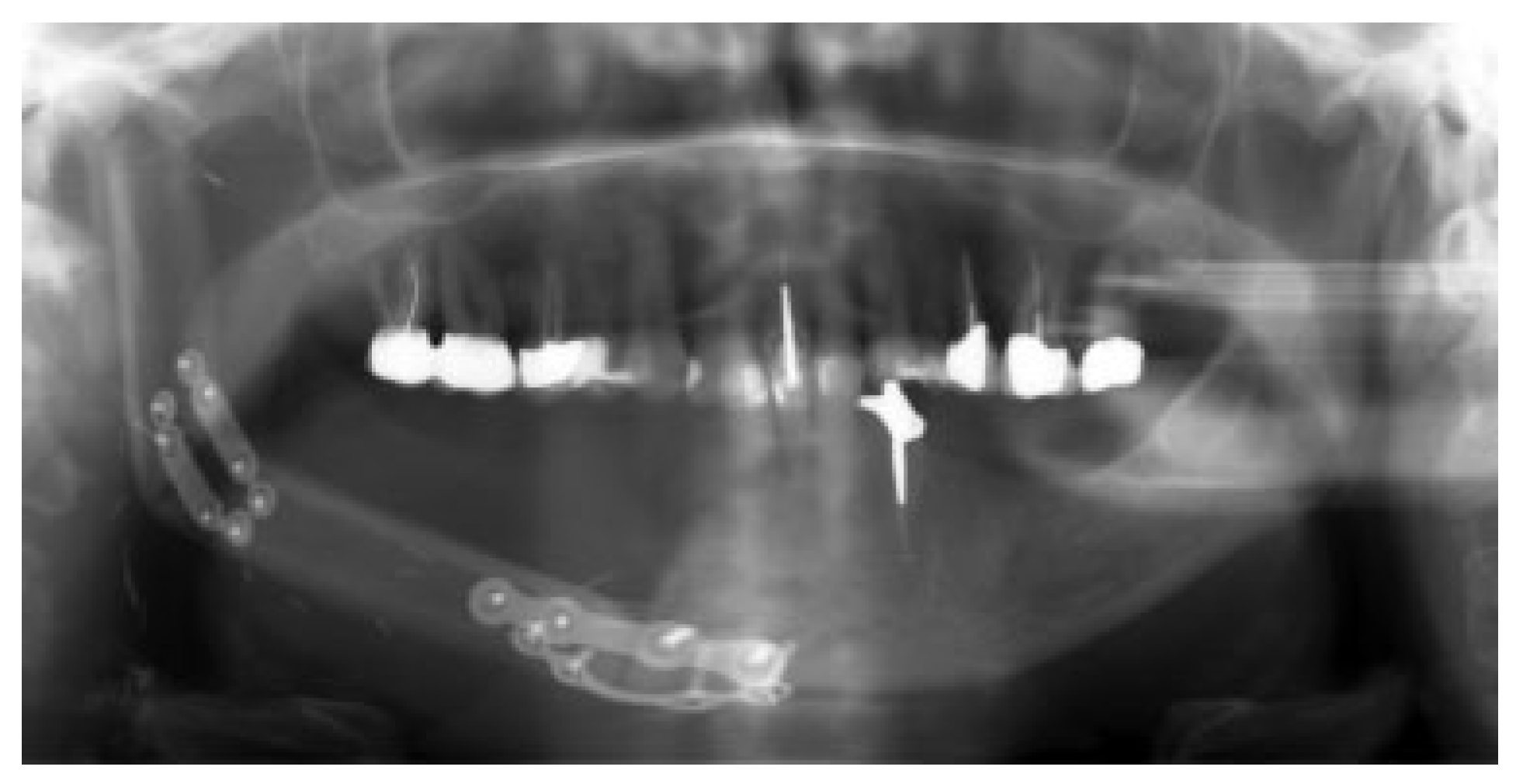
Table 2). This patient was excluded from further analysis due to lack of reconstruction. Eight patients had primary head and neck cancer, but in only four patients the condyle was involved due to infiltration, while four suffered from ORN. One patient suffered from a rare benign tenosynovial giant cell tumor. Two patients suffered from extensive osteomyelitis, and bisphosphonate osteonecrosis afflicted two patients. One patient had to be operated on twice due to hypertrophic bone formation around the metal condylar head and represents the only major complication in our series. She suffered facial nerve damage during the second surgery in a postradiated field, with the facial nerve lying on the reconstruction plate used in the first surgery (
Figure 1). Six of the fourteen reconstruction surgeries took place in a radiated field, explaining the two plate exposures in an unrelated area, away from the condylar reconstruction. Two patients received total joint reconstructions combined with one and in the other two free flaps. Five patients received fibula flaps alone and one received a vascularized costochondral graft, while all of the others had metal condylar prostheses with or without a free flap (
Figure 2,
Figure 3 and
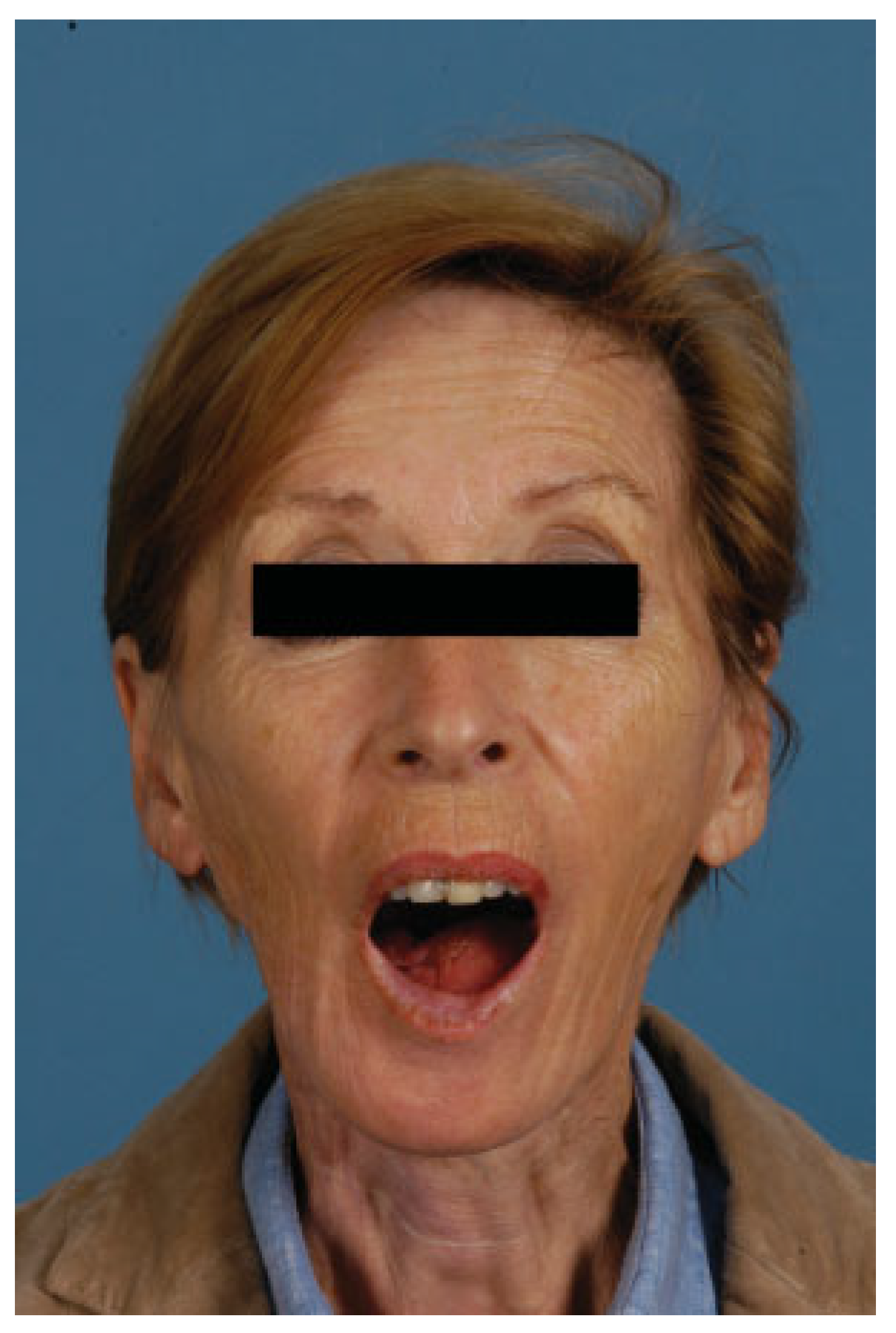
Figure 4). Follow-up ranged from 2 to 84 months with an average of 30 months. In total, five patients suffered from complications that could be considered acceptable, as they all could be corrected with minor revision surgery or occlusal adjustment. One patient suffered from facial nerve damage after a reconstruction plate in which metal condyle had to be removed in a radiate. In 11 patients, reliable information was obtained regarding mouth opening of which 9 showed a marked improvement of more than 5 mm. Three patients had a decrease in mouth opening, but all could be regarded as functional as no mouth opening of less than 30 mm was recorded (
Figure 4).
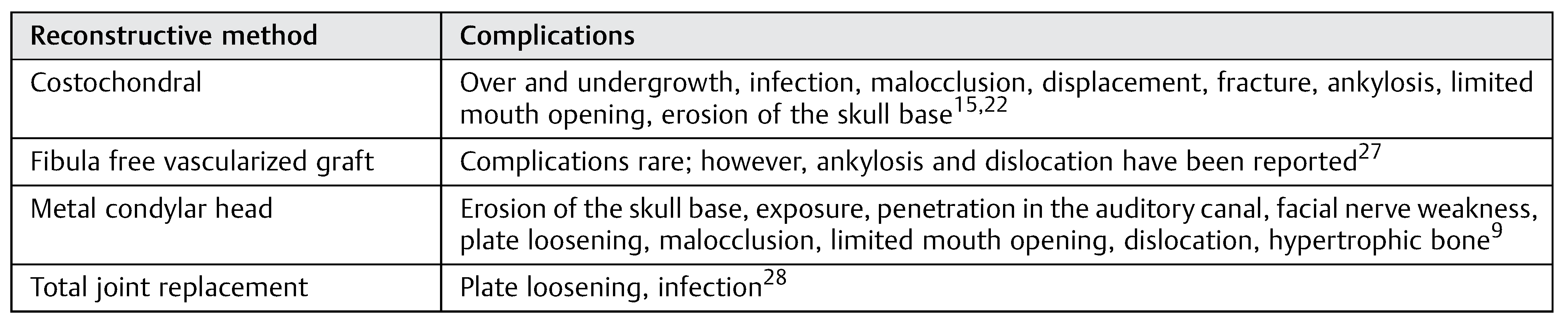
Options in the management of the TMJ after ablative surgery as found in the literature vary greatly and are summarized in
Table 3. Literature reports are mainly limited case series. Marx et al described the largest series of patients, consisting of an inhomogeneous that also included posttraumatic reconstructions [
9]. Studies relating to this subject are summarized in
Table 1. Plate exposure, especially in radiated patients, is the most common complication, especially associated with a radiated surgical field. It would appear as if there is a lower incidence of complications when a fibulafree vascularized graft is used versus metal plate with condylar attachment. It is unclear if disk preservation plays a role, but several authors attempted to preserve this structure diligently [
10,
11]. Complications reported are summarized in
Table 4. Additionally, a selection of possible risk factors according to the literature and our experience is listed in
Table 5.
In summary, it appears as if free fibula flap reconstructions have a lower complication rate than a plate with a metal condyle. Radiotherapy predisposes patients to plate exposure and is associated with the majority of complications.
Discussion
Due to the limited number of patients requiring reconstructive surgery after ablative surgery, limited evidence-based information is available.
Imaging modalities used in the preoperative determination of involvement of the TMJ in tumor and infective processes are seldom mentioned in the literature. However, this should not differ from the currently accepted methods of using computed tomography (CT) and magnetic resonance imaging (MRI), as well as positron emission tomography (PET)–CT. Although ultrasound can be used as well, no data regarding the use of this diagnostic modality in this setting were found in the literature. A combination of hard and soft tissue imaging will optimize the diagnosis of whether TMJ is involved.
Reports on partial and total reconstruction of the TMJ are plentiful [
16]. Equally so are the reports on complications found in the reconstruction of the TMJ; however, most of these reports focus on cases in which the indications for reconstructive surgery were due to internal derangement [
17].
Patients suffering from tumors or chronic infections affecting the TMJ are, however, a unique subset of patients with common unique risk factors for complications that may contribute to the importance of decision making. These factors include primary extensive surgery that affects both the hard and soft tissues, previous surgeries with resultant scarring and functional impairments, pre- or postoperative radiotherapy that may have a negative impact on both hard and soft tissues, preexisting limited mouth opening due to direct TMJ, or infiltration of surrounding musculature [
14]. In this subgroup of patients, the dentition is often in a poor state leading to reduced occlusal support and fewer adaptive abilities due to the burden of extensive surgery and/or chemo- and or radiotherapy, compounded by more advanced age [
15]. From the literature, it is clear that radiation, as well as multiple previous surgeries, as expected, plays an important role in the complication rate and has to be taken into account in any surgery decision-making process [
9]. In our case series, plate exposure, although away from the TMJ area, was associated with previous radiotherapy.
Similarly, patients with infective conditions such as osteomyelitis represent a group with similar poor tissue conditions with the additional risk of infection and bio film contamination of hardware. More often than not, these patients are subject to several decortication and sequestrectomy surgeries before definitive ablation. In our case series, five patients suffered from chronic infection before the surgery, two of which suffered from post operative complications. Plate exposure developed in a previously radiated patient who was treated with segmental removal of the plate, and another suffered from an occlusal disturbance. Although this case series is small, there seems to be no contraindication to the replacement of the condyle in an infected area.
With this in mind, it is important to consider the wide array of surgery- and material-based options in the management of loss of the whole TMJ or only the condylar component of the TMJ (
Table 3). Due to negative reports regarding costochondral grafts, there has been a gradual move away from this practice, favoring free vascularized (especially fibula) grafts, which show lower complication rates [
5,
11,
19,
27]. This trend is supported by our clinical observations due to the improved soft tissue conditions generated by fresh vascularized tissues. In favorable circumstances, the free vascularized fibula graft can be combined with a metal condyle, a practice that was employed in four patients with one occlusal disturbance noted in this group. In fact 12 of 14 patients with condylar reconstructions involved concurrent free flap transfer, emphasizing the importance of adequate soft tissue coverage. The liberal use of free vascularized grafts also may explain the good mouth opening in this series. In all recorded patients, a mouth opening of more than 30 mm was achieved, despite compromised soft tissue conditions due to radiotherapy and previous surgery scarring.
The use of autogenous fat or dermis fat grafts is well documented in the literature, and the proposed advantages of preventing ankylosis or re-ankylosis and improving mobility have been well demonstrated [
18]. It is now nearly routinely used around alloplastic total joint replacements, and its successful use has been described as a disk replacement. Dermis fat graft probably has a role in instances in which the ingrowth of scar tissue is to be prevented and dermis fat grafts may be an option where disk replacement is indicated or fear of ankylosis is present. Although it is a free tissue transplant, infection is not a common finding [
18]. Longer-term studies are indicated in this regard.
Apart from the large case series of Marx et al. [
9] reporting on a rather-inhomogeneous group of not only tumor patients, no large series exists regarding the reconstruction of the TMJ in patients after ablative surgery for tumors or patients suffering from osteomyelitis. Other literature reports are limited to few patients, often with a description of a single technique (
Table 1) [
20]. Despite these limiting factors, there are some indicators based on careful subanalysis and experience combined with sound clinical judgment on which to base a clinical decision-making process. Obviously such an analysis lacks statistical power and has a low level of evidence and should be interpreted as such. Despite these limitations, there should be attention to the reported complications in the different reconstruction options reported in the literature (
Table 4). The most common complications appear to be malocclusion, limited mouth opening, erosion of the skull base, plate loosening, and infection. These complications were linked to risk factors (
Table 5) according to the reported literature and clinical experience in our patient cohort.
By using the before-mentioned and experience-based risk factors—namely, pre- or postoperative radiotherapy, covering soft tissue quality and quantity, the absence of an intact disk, and loss of occlusal support—a treatment algorithm of management of the TMJ in tumor patients was developed. The algorithm is based on both risk factors for complications and structure preservation that should be taken into account in cases of primary or even secondary reconstruction after ablative tumor surgery. Low-risk patients can be defined as those without malignant disease, adequate covering soft tissue quality and quantity, no radiation, preserved disk, and sufficient occlusal support. High-risk patients are those who have been previously radiated, suffer from malignant disease, have the absence of a disk, and/or have poor occlusal support. Within each group, the safest method of full or partial TMJ reconstruction is suggested according to the risk profile (
Figure 5).
Conclusion
There is sparse evidence on the optimal reconstruction of the TMJ after ablative surgery. Decision making in the reconstruction of the TMJ after ablative tumor surgery will remain challenging. Risk factors for complications such as radiation, disk preservation, and soft tissue conditions must be taken into account when planning surgery. Free vascularized grafts, specifically fibula, appear to be the option with the lowest surgical complication rate and good function that must be weighed against donor-site morbidity in high-risk cases.