Orbital infections resulting from trauma have been reported in the literature [
10,
11,
12,
13,
14]. One study reported 262 periorbital infections. Trauma was the etiology of 89 (39%) of the preseptal infections and 4 (11%) of the postseptal infections. The authors did acknowledge some of these cases were caused by insect bites, viral ulcers, and scratches [
10]. There has been a case report of chronic maxillary sinusitis that developed into an orbital cellulitis after fracture of the left zygomatic bone [
11]. Another study postulated that a hematoma formed in the maxillary sinus following an undiagnosed minimally displaced zygomatic complex fracture subsequently became infected leading to subperiosteal abscess of the orbit [
12]. A retrospective study was performed to determine the incidence of orbital cellulitis following orbital floor fractures. The study included 497 patients at two centers of which 4 patients developed orbital cellulitis for an incidence of 0.8%. Three out of the four patients received antibiotics immediately following the fracture and still developed orbital abscess [
13]. A frontal sinus fracture with an associated soft tissue laceration which violated the superior orbital rim that led to an infection of the orbit and sinuses was also reported [
14]. There are a small number of cases of orbital cellulitis and abscess caused by trauma reported in the literature. Zygomaticomaxillary complex, frontal sinus, and orbital fractures can lead to orbital infection and preexisting sinus disease appears to contribute to the risk of infection.
This article presents a case of a patient who developed a severe multifascial space infection following orbital trauma associated with existing maxillary sinusitis that led to involvement of the parapharyngeal space.
Case Report
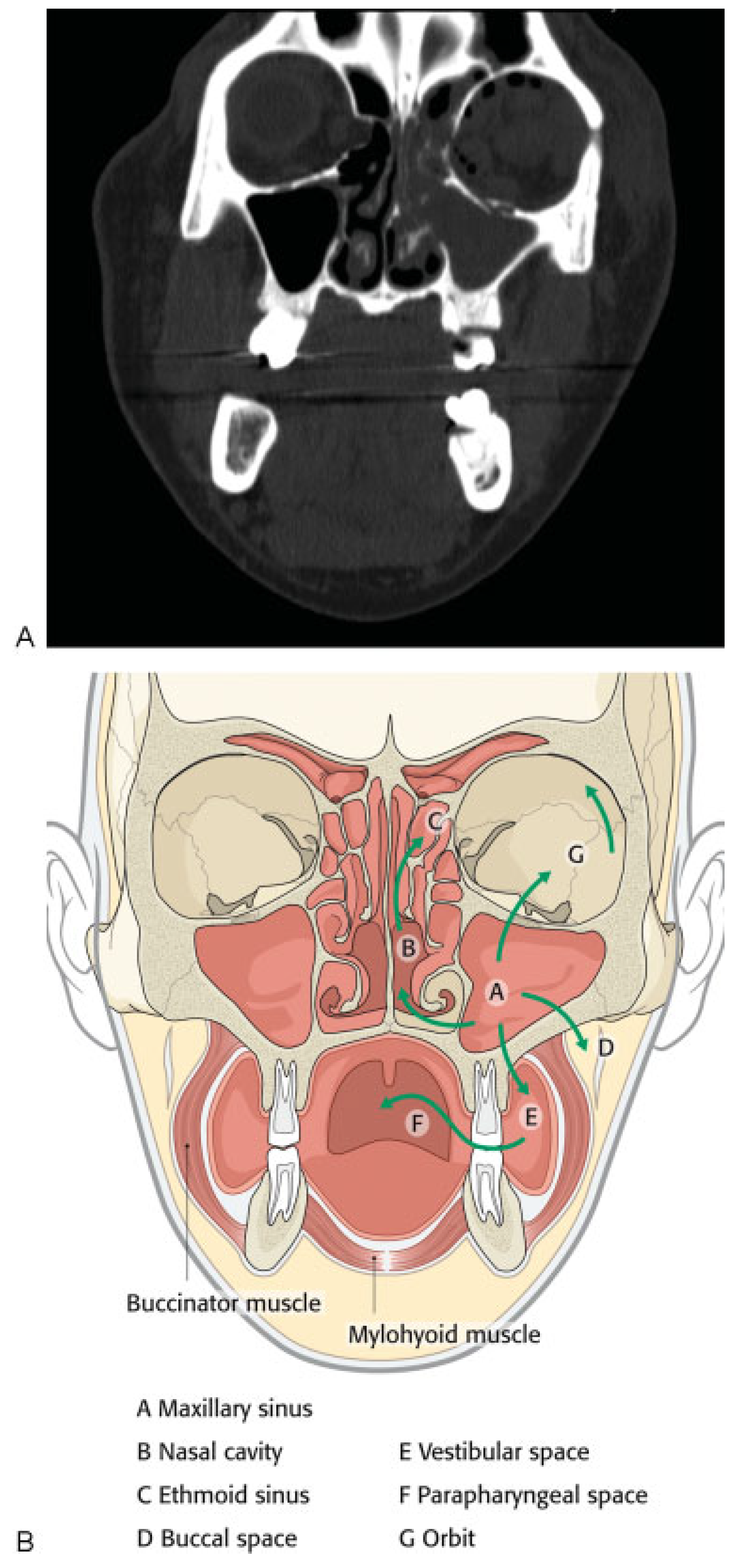
A 43-year-old woman presented to our clinic with a complaint of left sided facial pain and periorbital swelling secondary to her involvement in a motor vehicle collision the previous night. She reported no other injuries. Her medical history was significant for diabetes mellitus type II which was poorly controlled and hypertension for which she was taking metformin, glyburide, and lisinopril. The patient also had amblyopia in her left eye since childhood resulting in poor vision and diplopia. Her past surgical history was significant for cataract surgery of the left eye in 2009. A maxillofacial CT scan revealed a minimally displaced left orbital floor and medial orbital wall fractures (►
Figure 1A). In the clinic, the patient was afebrile with stable vital signs. Her finger stick blood glucose (FSBG) was measured as 363. On physical examination, her left periorbita was edematous and she had tenderness to palpation of the left periorbital, temporal, and zygomatic regions, which were all consistent and normal with expected posttraumatic signs. Her vision in the right eye and left eye was 20/25 and 20/400, respectively, and the patient denied any acute visual acuity changes. Of note, 20/200 is considered legally blind in the United States. Bilateral extraocular movements were intact with no evidence of entrapment. Cranial nerve examination revealed grossly intact cranial nerves 3 to 12 with the exception being the left eye having vision changes of 20/400 and cranial nerve V2 paresthesia. Glasgow Coma Scale score was 15. The patient was prescribed pain medication, and asked to return to clinic in 4 days for reevaluation once the swelling subsided for surgical workup. The patient was sent to ophthalmology clinic that day and was evaluated. She was not prescribed antibiotics.
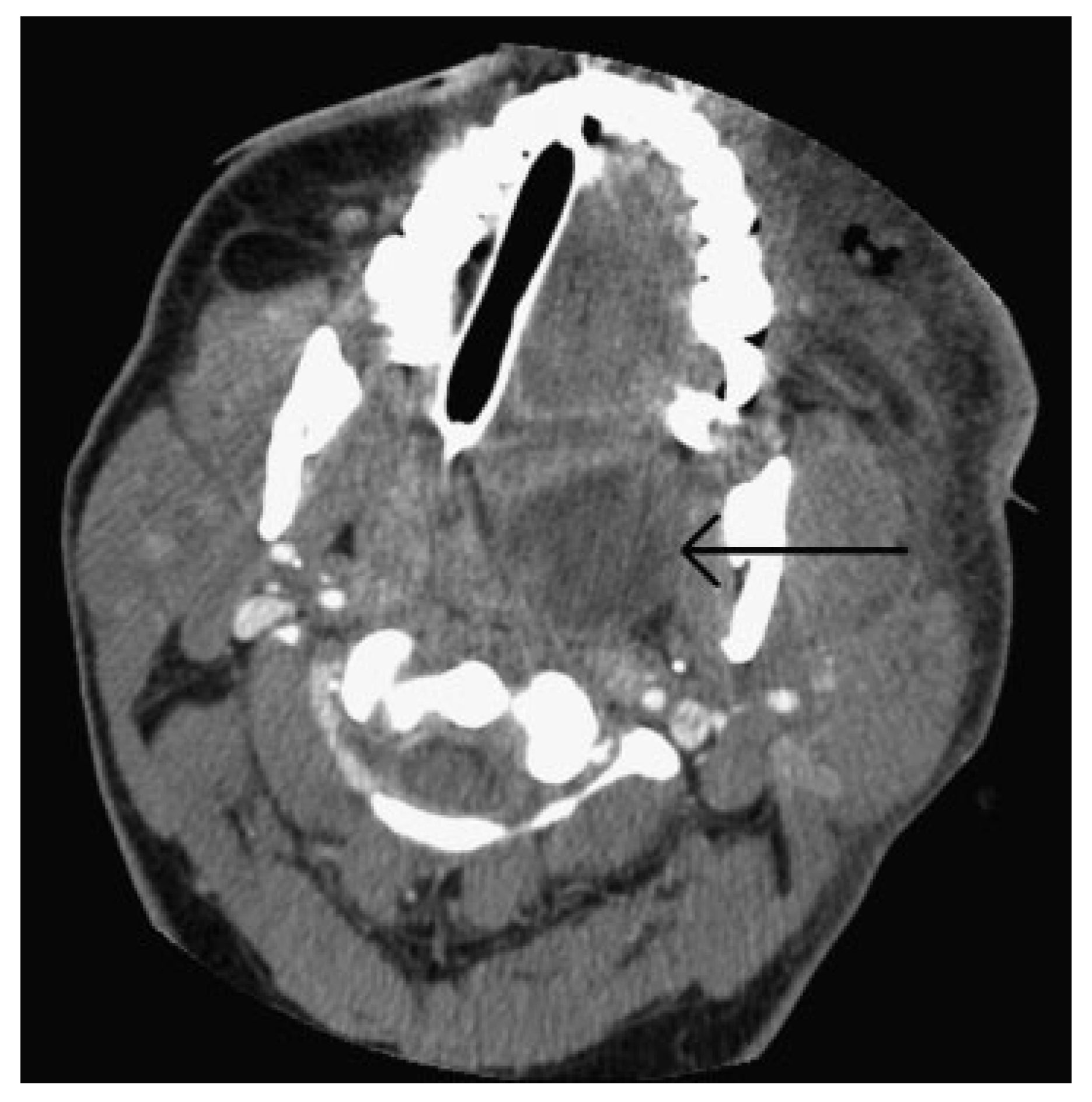
She returned to our clinic 4 days later with a dramatic change from her initial presentation. At that time, the patient had malaise, pain, and significant malodorous purulent drainage from the left upper and lower lid and left naris. She was febrile and her left periorbital, frontal, temporal, zygomatic, and infraorbital regions as well as her right periorbital region were significantly swollen, tender, and erythematous. Her FSBG was 306. The left lower lid was blackened. The patient noticed first drainage the day before (►
Figure 2A,B). Ptosis of the left upper lid, proptosis, chemosis, and impairment of extraocular motility in all gaze positions were also observed. No dysphagia, odynophagia, trismus, and dyspnea were present. Ophthalmologic examination revealed continued decreased visual acuity in the affected eye of 20/400 secondary to amblyopia with diplopia in all visual fields.
The patient was taken immediately to the operating room due to her worsening clinical presentation and the authors’ suspicion for necrotizing soft tissue infection. Incision and drainage and debridement of the necrotic tissue were performed on the left periorbital, zygomatic, and temporal regions (►
Figure 3A–D). Copious purulent drainage was obtained which was submitted for Gram stain and cultures. Irrigation of the wound was then performed until no further murky fluid was appreciated with approximately 5 L of 0.9% normal saline. The wound was then packed in a standard wetto-dry fashion. The patient was placed on vancomycin, piper-acillin/tazobactam, and metronidazole and transferred to the intensive care unit (ICU) where she remained intubated and sedated. In the ICU, she was supported medically, including optimization of her blood glucose. Overnight, the patient remained tachycardic and febrile with a maximum temperature of 103°F (39.4 °C). At that time, a maxillofacial CT with contrast was obtained, which revealed left periorbital, orbital, and buccal inflammatory changes. Proptosis, lateral and downward displacement of the globe, and homogeneous opacification of the frontal, ethmoid, and maxillary sinuses were appreciated on the left side. The right ethmoid sinus was partially opacified, which justified the inflammatory changes in the right orbit. Additionally, a large fluid loculation of the left lateral pharyngeal space was present (►
Figure 4). The intraoral examination revealed a large localized swelling of the left oropharynx and nasopharynx, with deviation of the palatal uvula from the midline. Ophthalmology was reconsulted. On postoperative day 2, the patient was taken back to the operating room for incision and drainage of the left maxillary sinus and left lateral pharyngeal space and washout of existing wound. An intraoral incision was made on the left posterior oropharynx and blunt dissection was performed to enter the left lateral pharyngeal space where approximately 15 mL of purulence was obtained and samples were sent for cultures and sensitivities. Three nonrestorable, grossly carious left maxillary posterior teeth were then extracted to negate any possible source of odontogenic infection; however, no purulence or periapical involvement of the teeth was evident upon extraction. This made an odontogenic cause of the infection unlikely. The left maxillary sinus was entered via a standard Caldwell-Luc approach to drain the fluid collection appreciated on CT and an additional 5 to 10 mL of purulence was obtained. After copious irrigation of the sites, two ½ inch Penrose drains were placed, one in the left maxillary sinus and the other in the left lateral pharyngeal space. The drains were then secured to the oral mucosa with sutures. Washout and redressing of the left periorbital wound was then performed and the patient returned to the ICU intubated. Laboratory values showed white blood cell count of 15.9 g/dL, hemoglobin of 12 g/dL, hematocrit of 36.4%, and platelet count of 226,000/µL. Chemistry showed sodium level of 134 mmol/L, potassium level of 3.5 mmol/L, chloride level of 97 mmol/L, bicarbonate level of 27 mmol/L, blood urea nitrogen level of 6 mg/dL, creatinine level of 0.7 mg/dL, and glucose level of 375 mg/dL. Hemoglobin A
1C was 12.8 and C-reactive protein was 34.2 mg/dL. The patient’s previously recorded hemoglobin A
1C was 13.0 recorded 26 months earlier at the medicine clinic showing long-term poor diabetic control. Over the next few days, the patient clinically improved and her vital signs stabilized with the exception of a persistent elevated temperature of 101°F. Cultures came back as group C β hemolytic Steptococcus and
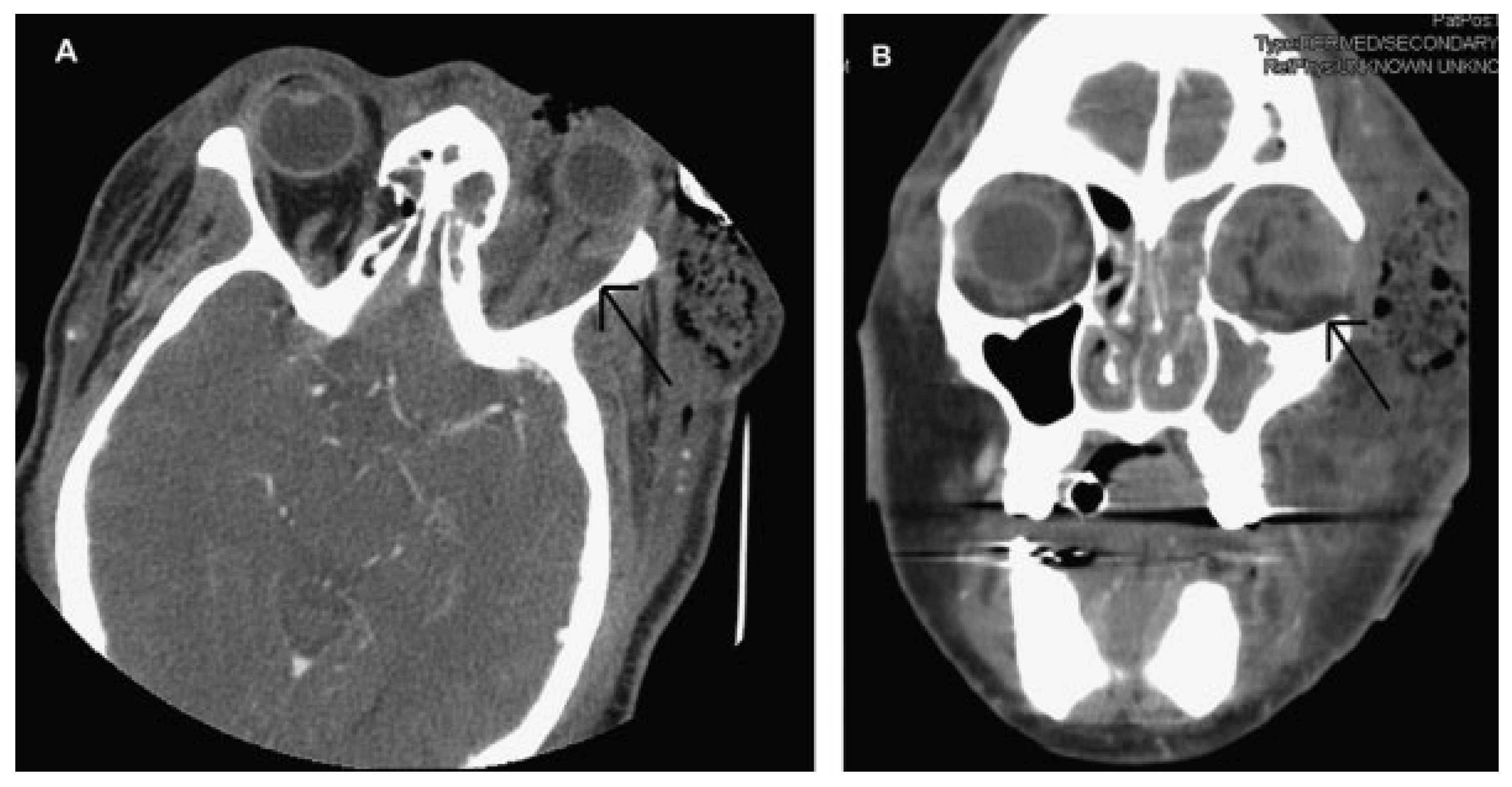
Proteus mirabilis. After consultation with the infectious disease service, the antibiotics were narrowed to ampicillin/sulbactam and clindamycin. A repeat CT scan was obtained on hospital day 5 and a loculation was noted at the superior and lateral aspect of the left orbit, suggestive of subperiosteal abscess (►
Figure 5A,B). Ophthalmology service recommended no intervention for the left orbital subperiosteal abscess. However, as the patient was still having low-grade temperature of 101°F (38.3 °C), the authors took the patient back to the operating room for incision and drainage of this area. We approached the superior-lateral orbit via an existing incision, and approximately 5 mL of purulence was obtained. Postoperatively, the patient improved clinically, and became afebrile. The intraoral drains were removed, and after cons ultation with the wound nurse, the wet-to-dry dressing of the skin was changed to petroleum-impregnated gauze. Despite our objection, the patient remained intubated for a prolonged period due to the discomfort of the ICU team in extubating the patient. The patient was extubated on hospital day 12. On the day of discharge, examination revealed significant decrease in left periorbital swelling, decrease proptosis, and increase extraocular movement in all directions; however, she continued to have 20/400 vision in the left eye and diplopia. Due to the defect in the left upper and lower eyelids, a home care nurse was assigned for daily dressing changes. Intraoral examination demonstrated resolution of swelling of the oropharynx. A maxillofacial CT scan revealed resolution of the original fluid loculations and a patent airway. Throughout the postoperative hospital stay, the patient’s glucose level and blood pressure were controlled. The patient was discharged on hospital day 13 with oral antibiotics, amoxicillin/clavulanic acid, and clindamycin, as well as her home antihypertensive and diabetic medications. The patient was closely followed up and her condition continued to improve. At 4 months follow-up, the patient presented with resolution of facial swelling; had proptosis and eyelid ptosis, normal extraocular movements; and her baseline visual acuity of her left eye remained 20/400. The patient was seen 1 year postoperatively and had continued resolution of her wounds with appropriate wound closure; however, she had continued strabismus, ptosis of the upper and lower lid secondary to scar contraction, as well as left V2 paresthesia (►
Figure 6A,B). The orbital wound continued to heal via secondary intention with anticipated reconstruction and scar revision in the near future.
Discussion
Infectious disease may spread into the orbital cavity from numerous sources and can occur via three routes: directly through the skin or conjunctiva, as an extension from neighboring structures, or, rarely, hematogenous spread [
4]. The majority of preseptal cellulitis cases are due to a localized infection of the eyelid and adjacent structures, such as dacryocystitis, dacryoadenitis, hordeolum, chalazion, conjunctivitis, or secondary to superficial trauma to the skin, such as abrasions and insect bites [
2,
15]. On the contrary, postseptal orbital infections mostly spread from adjacent structures, mainly from paranasal sinusitis [
2], most frequently via the ethmoid sinus. Odontogenic etiology has also been reported [
16] and orbital involvement can also be present in typhoid, tuberculosis, syphilis, tick fever, scarlet fever, herpes simplex, herpes zoster, mononucleosis, and influenza A [
17].
From an anatomic perspective, the knowledge of the anatomy of the face and neck, especially the orbital region, is crucial for understanding the route that the infection propagates. Sinus infections may spread directly through the sinus walls or communicating facial veins, particularly into the orbital cavity [
8]. The roof, floor, and medial orbital walls that separate the orbital contents from the frontal, maxillary, and ethmoid sinuses, respectively, are thin and relatively weak. Therefore, aggressive infections may spread directly from the intact sinus bony walls into the orbit[
3] or from naturally occurring bony dehiscences [
4]. However, the orbital veins which lack valves play an important role in the spread of infection. It allows the spread of infection in both anterograde and retrograde directions among orbital, facial, sinus, and nasal cavity veins, and also the pterygoid plexus and cavernous sinus [
1,
3,
18]. Although rare, possible complications of sinus infections include intracranial dissemination, resulting in osteomyelitis, epidural and subdural empyema, meningitis, cerebritis, and brain abscess [
3,
4,
8]. Therefore, a detailed neurologic and ocular examination should be performed particularly when orbital and neurological symptoms are present [
3].
In this case, we believe that the infection originated in the maxillary sinus and extended into the orbital cavity through the fractured orbital floor, resulting in preseptal and postseptal orbital cellulitis progressing to abscess. The infection then likely spread to the face via the ophthalmic and angular vein, reaching the left buccal space. The lack of host response secondary to uncontrolled diabetes mellitus may have contributed to further dissemination of the infection to two other ipsilateral spaces: (1) from the maxillary sinus to the nasal cavity through the medial maxillary sinus wall and (2) from the buccal to the parapharyngeal space through the pterygomandibular raphe, a ligamentous band of the buccopharyngeal fascia, located between the superior pharyngeal constrictor and the middle portion of the buccinator muscles (►
Figure 1B).
Infections in the parapharyngeal space are a result of direct extension from surrounding spaces. Dental and tonsillar diseases are the most common sources among adults and children, respectively [
19,
20], with a reported prevalence ranging from 5.9 to 18% among deep neck infections [
5,
20]. Sore throat, odynophagia, dysphonia, fever, and neck pain are the most common symptoms, while neck swelling and its limitation of movements, cervical lymphadenopathy, dyspnea, and trismus are the most common signs [
20,
21]. Pneumonia, mediastinitis, necrotizing fasciitis, and septic shock with disseminated intravascular coagulation syndrome are the potential complications that can occur within a few hours. Cranial nerve paralysis and neuro-encephalopathy can result in dysphagia, a risk factor to aspiration pneumonia [
5]. Complications due to orbital infections include visual impairment, orbital and intracranial abscesses, and venous sinus thrombosis [
2].
The anatomical complexity of the deep neck spaces makes the diagnosis and management of these infections challenging and highly complex for many reasons. First, the clinical examination is impaired because many times the spaces are difficult to palpate and visualize. Second, the parapharyngeal and retropharyngeal spaces have a direct communication between one another, thus making the spread of infection to other portions of the neck and mediastinum easier. Finally, the deep neck spaces are surrounded by many vital structures that may become involved in the inflammatory process [
6]. The anterior compartment (prestyloid) is crossed by the internal maxillary artery and the inferior alveolar, lingual, and auriculotemporal nerves. The poststyloid compartment contains the carotid sheath (internal carotid artery, internal jugular vein, and vagus nerve), glossopharyngeal, hypoglossal, and accessory nerves, as well as the cervical sympathetic chain and lymph nodes [
20].
The presence of large blood vessels and several cranial nerves that cross the parapharyngeal space makes the intraoral surgical drainage a debated topic in the literature. In a retrospective review of 47 children over a 5-year period admitted with clinical diagnosis of retropharyngeal or parapharyngeal infection, the authors performed a transoral approach in 22 of the 23 surgical cases (96%), without mortal complications. They also emphasized that contrast-enhanced CT scan served as a guide to the location and extent of the abscess, as well as the location of the great vessels preoperatively [
22]. In a prospective study, 55.9% of the 34 patients with parapharyngeal infection were successfully treated by conservative management. Of the 15 patients treated with surgical drainage, 80% had transoral approach with no reported postoperative complications. The authors also pointed out that surgical management is imperative when imminent complications are present, when no improvement is observed with intravenous antibiotics after 48 h, and when lobulated and large abscesses are present [
20]. Amar and Manoukian [
23] also recommended intraoral drainage for the surgical management of the parapharyngeal space. They conducted an 11-year retrospective study among 25 patients who underwent transoral or external neck drainage. They observed that the intraoral drainage shortened the anesthesia period by a medium of 31.7 min when compared with the transcervical approach. And it was also associated with a decrease in postoperative intravenous antibiotic duration and length of postoperative hospital stay [
20]. The decision for surgical or conservative management should be made by a combination of both clinical and radiographic findings, with the pharmacological therapy reserved for small abscesses and when there is no evidence of airway compromise [
21]. In our case, the severity of the infection demonstrated by clinical and CT findings necessitated surgical intervention. The transoral approach performed provided adequate access to perform suitable drainage of the parapharyngeal space, as previously reported in the literature [
20,
22,
23].
Medial displacement of the lateral pharyngeal wall and palatine tonsils are characteristic findings of parapharyngeal space infection [
6], and may result in compression of the airway, even in the absence of large abscesses [
19]. Such patients often require hospitalization in an ICU and prolonged intubation. An 11-year retrospective study in 286 consecutive patients demonstrated that retropharyngeal and parapharyngeal infections were the most severe diseases among deep neck infections, requiring the highest number of tracheotomies, even when compared with cases of Ludwig angina. The authors found a high rate of mortality among patients with retropharyngeal and parapharyngeal infections, ranging from 41 to 50% for adults and children, respectively [
5]. In this report, the patient underwent endotracheal intubation for 12 days, the period necessary to resolve the swelling in the oropharynx region with no impairment to the upper airway.
The medical management of orbital infections is directed to three major pillars: (1) surgical drainage when an abscess is present; (2) antibiotics; and (3) primary source eradication [
12]. Severe infections require empiric treatment with broadspectrum intravenous antibiotics [
2]. As the culture and sensitivity results become available, the antibiotic selection should be modified accordingly [
17,
18]. Historically, the most common pathogen involved in orbital infection until 1985 was
Haemophilus influenzae type B (Hib) [
2,
4]. After the introduction of Hib vaccination, a marked decline in the number of orbital infections due to Hib was observed, resulting in a change in the microbiological spectrum, with the most common positive cultures attributed to
Staphylococcus and
Streptococcus specimens [
2,
4,
18,
24,
25,
26,
27]. Some authors suggested that Hib may have facilitated the pathogenicity of others microorganisms because not only a sharp decline in the number of periorbital and orbital cellulitis was observed after the vaccine introduction but also the annual case rate, which was significantly lower after the introduction of the vaccine. The authors observed that of the 315 cases of orbital infection analyzed, 70% of them occurred before 1990, and just 30% were present between 1990 and 1998 [
25].
According to Lee and Yen [
18], another important consideration is that different communities may have distinctive flora, with different pathogens associated with the infection. For example, the authors reported a great prevalence (75%) of methicillin-resistant
Staphylococcus aureus in community-acquired infections, which justified the introduction of vancomycin as the first administrated antibiotics. In our case, in addition to vancomycin, to provide a broader coverage to anaerobic, gram-negative, and β-lactamase microorganisms, we also administered metronidazole and piperacillin/tazobactam. After the culture results and consultation with the infectious disease service, the antibiotics were changed to clindamycin and ampicillin/sulbactam. The admission blood glucose level in uncontrolled diabetes mellitus is an important risk factor that significantly affects the clinical outcomes of patients with multifascial space infection of the head and neck regions. Diabetic patients tend to have a longer length of hospital stay and complications when compared with nondiabetic patients [
28]. For our patient, we believe that her uncontrolled diabetes (hemoglobin A
1C 12.8), contributed to the rapid progression and dissemination of the infection.
Early detection is vital for favorable outcomes in these severe cases. A thorough early clinical exam is critical and CT/MRI imaging is needed to assess the extent of traumatic injury and any present abscess or cellulitis. Consultations with the appropriate services are also indicated, such as ophthalmology, oral and maxillofacial surgery, infectious disease, internal medicine, and plastic or oculoplastic surgery to help in the management and resolution of the traumatic injuries, infection, and medical comorbidities.