Subclavicular Pectoralis Major Myocutaneous Flap for Optimal Reconstruction of Large Orbitozygomatic Defects: A Case Report
Abstract
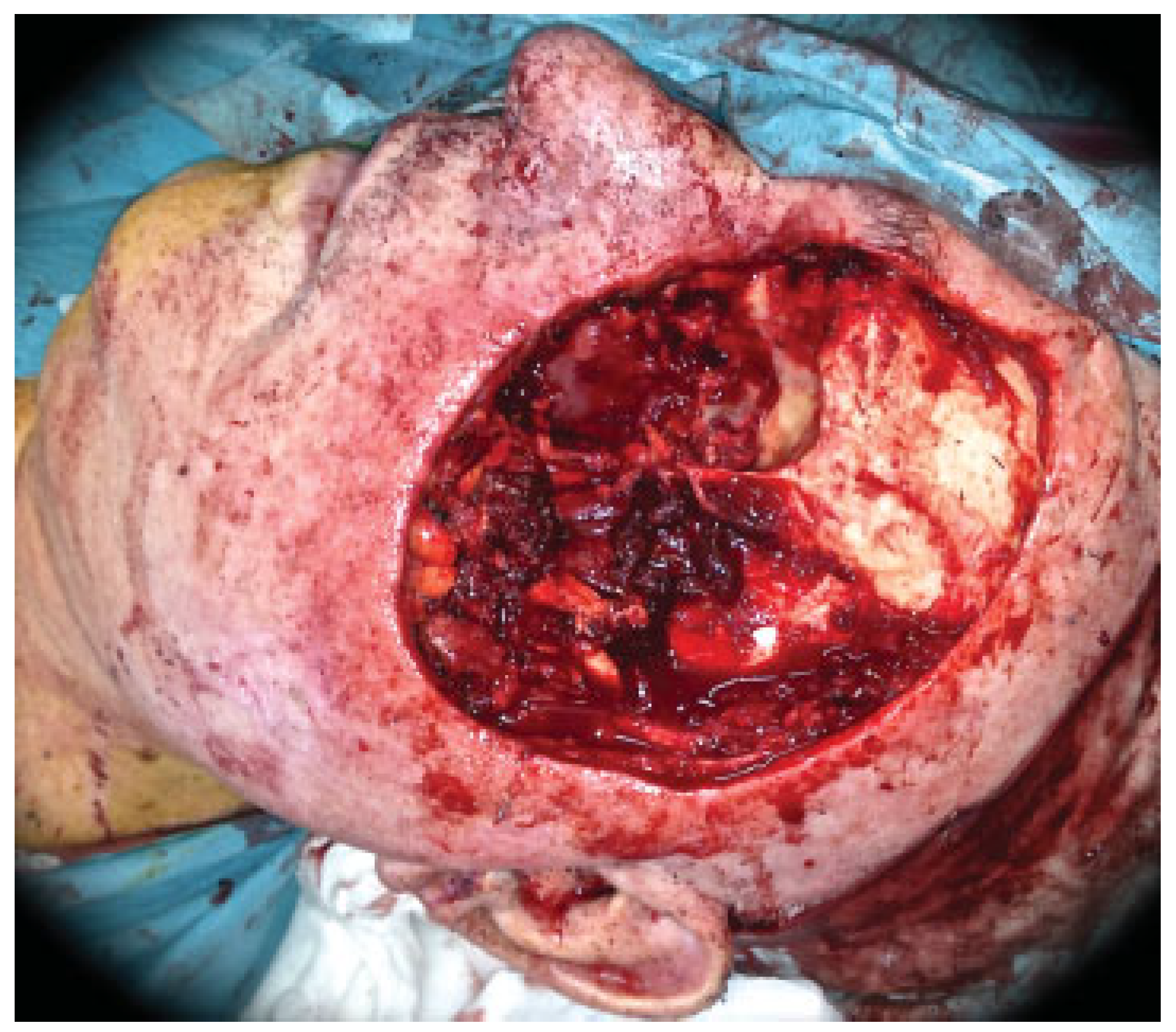
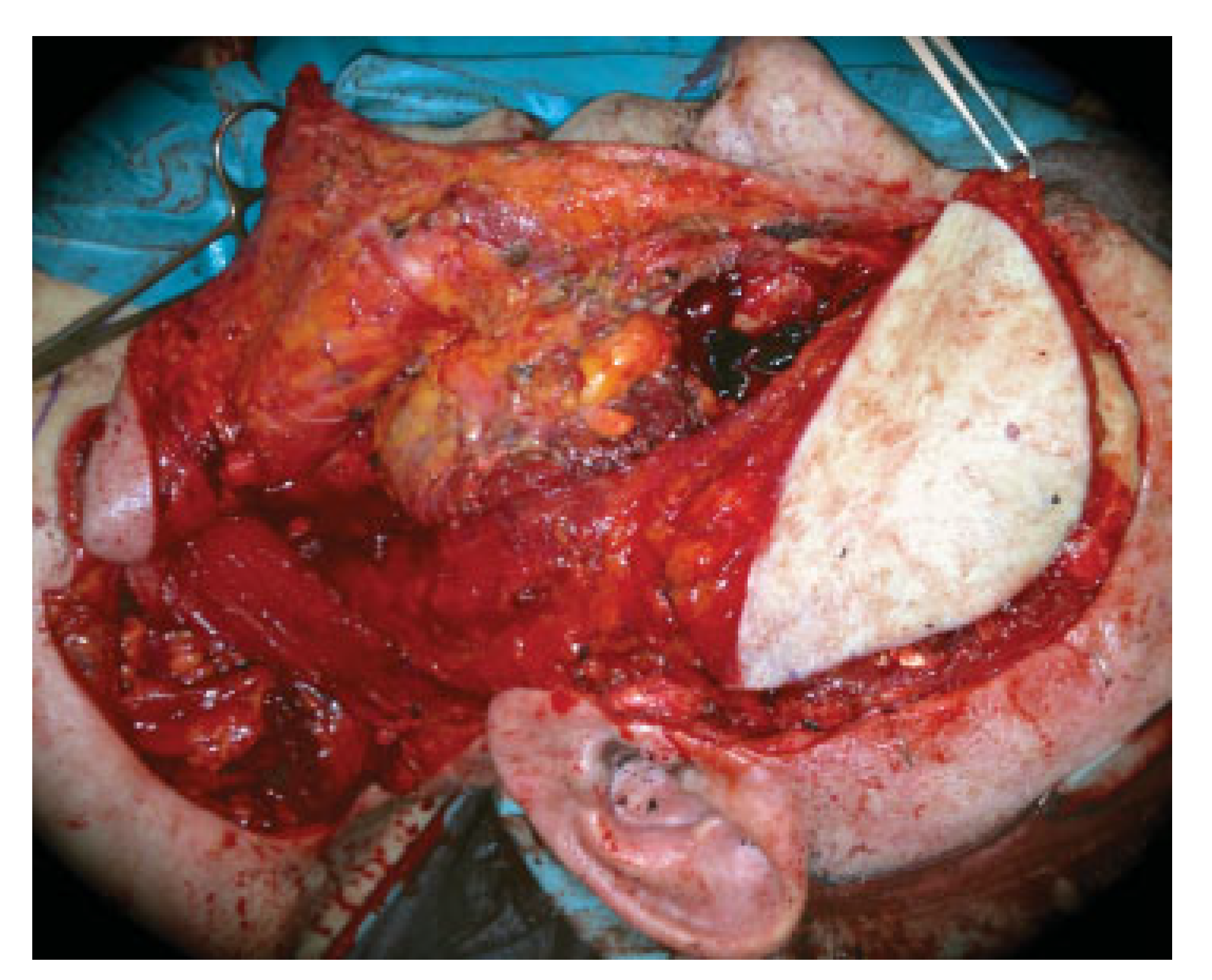
:Case Report
Discussion
Conclusion
References
- Kadlub, N.; Shin, J.H.; Ross, D.A.; et al. Use of the external pectoralis myocutaneous major flap in anterior skull base reconstruction. Int J Oral Maxillofac Surg 2013, 42, 453–457. [Google Scholar] [CrossRef] [PubMed]
- Chepeha, D.B.; Annich, G.; Pynnonen, M.A.; et al. Pectoralis major myocutaneous flap vs revascularized free tissue transfer: complications, gastrostomy tube dependence, and hospitalization. Arch Otolaryngol Head Neck Surg 2004, 130, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Liu, R.; Gullane, P.; Brown, D.; Irish, J. Pectoralis major myocutaneous pedicled flap in head and neck reconstruction: retrospective review of indications and results in 244 consecutive cases at the Toronto General Hospital. J Otolaryngol 2001, 30, 34–40. [Google Scholar] [CrossRef] [PubMed]
- Taylan, G.; Yildirim, S.; Aköz, T. Reconstruction of large orbital exenteration defects after resection of periorbital tumors of advanced stage. J Reconstr Microsurg 2006, 22, 583–589. [Google Scholar] [CrossRef] [PubMed]
- Vanni, C.M.; Pinto, F.R.; de Matos, L.L.; de Matos, M.G.; Kanda, J.L. The subclavicular versus the supraclavicular route for pectoralis major myocutaneous flap: a cadaveric anatomic study. Eur Arch Otorhinolaryngol 2010, 267, 1141–1146. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, T.K.; Balló, H.; Hauser, U.; Bier, H. The subclavicular route for the pectoralis major myocutaneous flap [in German]. HNO 2006, 54, 523–527. [Google Scholar] [CrossRef] [PubMed]
- Vartanian, J.G.; Carvalho, A.L.; Carvalho, S.M.; Mizobe, L.; Magrin, J.; Kowalski, L.P. Pectoralis major and other myofascial/myocutaneous flaps in head and neck cancer reconstruction: experience with 437 cases at a single institution. Head Neck 2004, 26, 1018–1023. [Google Scholar] [CrossRef] [PubMed]
- Lopez, R.; Dekeister, C.; Sleiman, Z.; Paoli, J.R. The temporal fasciocutaneous island flap for oncologic oral and facial reconstruction. J Oral Maxillofac Surg 2003, 61, 1150–1155. [Google Scholar] [CrossRef] [PubMed]
- Shah, J.P.; Haribhakti, V.; Loree, T.R.; Sutaria, P. Complications of the pectoralis major myocutaneous flap in head and neck reconstruction. Am J Surg 1990, 160, 352–355. [Google Scholar] [CrossRef] [PubMed]
- Milenović, A.; Virag, M.; Uglesić, V.; Aljinović-Ratković, N. The pectoralis major flap in head and neck reconstruction: first 500 patients. J Craniomaxillofac Surg 2006, 34, 340–343. [Google Scholar] [CrossRef] [PubMed]
- Kerawala, C.J.; Sun, J.; Zhang, Z.Y.; Guoyu, Z. The pectoralis major myocutaneous flap: Is the subclavicular route safe? Head Neck 2001, 23, 879–884. [Google Scholar] [CrossRef] [PubMed]




© 2014 by the author. The Author(s) 2014.
Share and Cite
Pingarron, L.; Ruiz, J.; Rey, J.; Maniegas, L.; Roson, S.; Martinez, D. Subclavicular Pectoralis Major Myocutaneous Flap for Optimal Reconstruction of Large Orbitozygomatic Defects: A Case Report. Craniomaxillofac. Trauma Reconstr. 2014, 7, 245-248. https://doi.org/10.1055/s-0034-1371975
Pingarron L, Ruiz J, Rey J, Maniegas L, Roson S, Martinez D. Subclavicular Pectoralis Major Myocutaneous Flap for Optimal Reconstruction of Large Orbitozygomatic Defects: A Case Report. Craniomaxillofacial Trauma & Reconstruction. 2014; 7(3):245-248. https://doi.org/10.1055/s-0034-1371975
Chicago/Turabian StylePingarron, Lorena, Julian Ruiz, Juan Rey, Lourdes Maniegas, Silvia Roson, and Dolores Martinez. 2014. "Subclavicular Pectoralis Major Myocutaneous Flap for Optimal Reconstruction of Large Orbitozygomatic Defects: A Case Report" Craniomaxillofacial Trauma & Reconstruction 7, no. 3: 245-248. https://doi.org/10.1055/s-0034-1371975
APA StylePingarron, L., Ruiz, J., Rey, J., Maniegas, L., Roson, S., & Martinez, D. (2014). Subclavicular Pectoralis Major Myocutaneous Flap for Optimal Reconstruction of Large Orbitozygomatic Defects: A Case Report. Craniomaxillofacial Trauma & Reconstruction, 7(3), 245-248. https://doi.org/10.1055/s-0034-1371975


