Rapid prototyping, also known as three-dimensional (3D) printing, is an additive manufacturing technology that allows expedient and accurate reproduction of osseous anatomy. It was originally introduced in the mechanical engineering field during the 1980s and this technology has gained interest in craniomaxillofacial surgery as a tool for assessment and preoperative surgical planning [
1,
2]. For orbital floor fractures, rapid prototyping can provide an accurate anatomical representation of the osseous defect, allowing the clinician to preoperatively adapt a titanium plate for reconstruction. This theoretically reduces the operative time required, risk of orbital plate malposition, poor anatomical contour, and trauma to soft tissues due to multiple insertions during trimming and adaptation of the titanium orbital plate. We propose that the use of rapid prototyping and preoperative plate adaptation can significantly reduce the operative time taken while improving patient outcome.
Methods
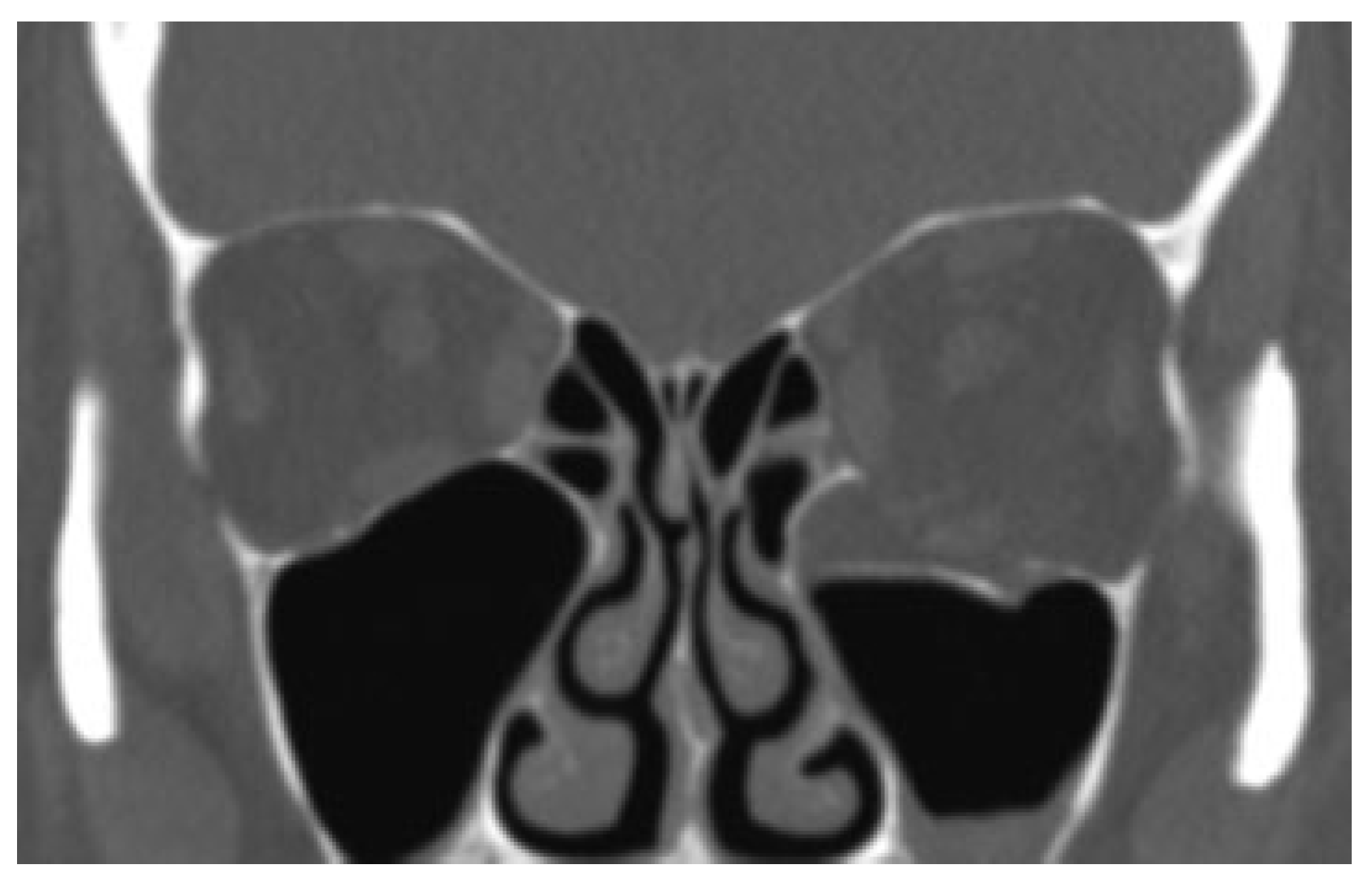
Computed tomography (CT) data were processed via an imaging software program (e.g., 3D slicer, Osirix [Osirix-Pixmeo, Bernex, Geneva, Switzerland]), cropped and then exported as a stereolithographic file (.stl) (
Figure 1) which was then used for fabrication of a 3D model via 3D printing. CT orbital parameters used were 0.5 mm slice thickness, 0.4 mm increments, J70h kernel (Safire reconstruction), 120 kV, ref mAs 200, and Digital Imaging and Communication in Medicine (DICOM) data. A titanium orbital plate (Synthes [Synthes, Solothurn, Switzerland]) was subsequently adapted to the defect in each case before the procedure. The titanium orbital plate was sterilized before insertion and intraoperative CT imaging was used to assess final titanium plate position.
Case 1
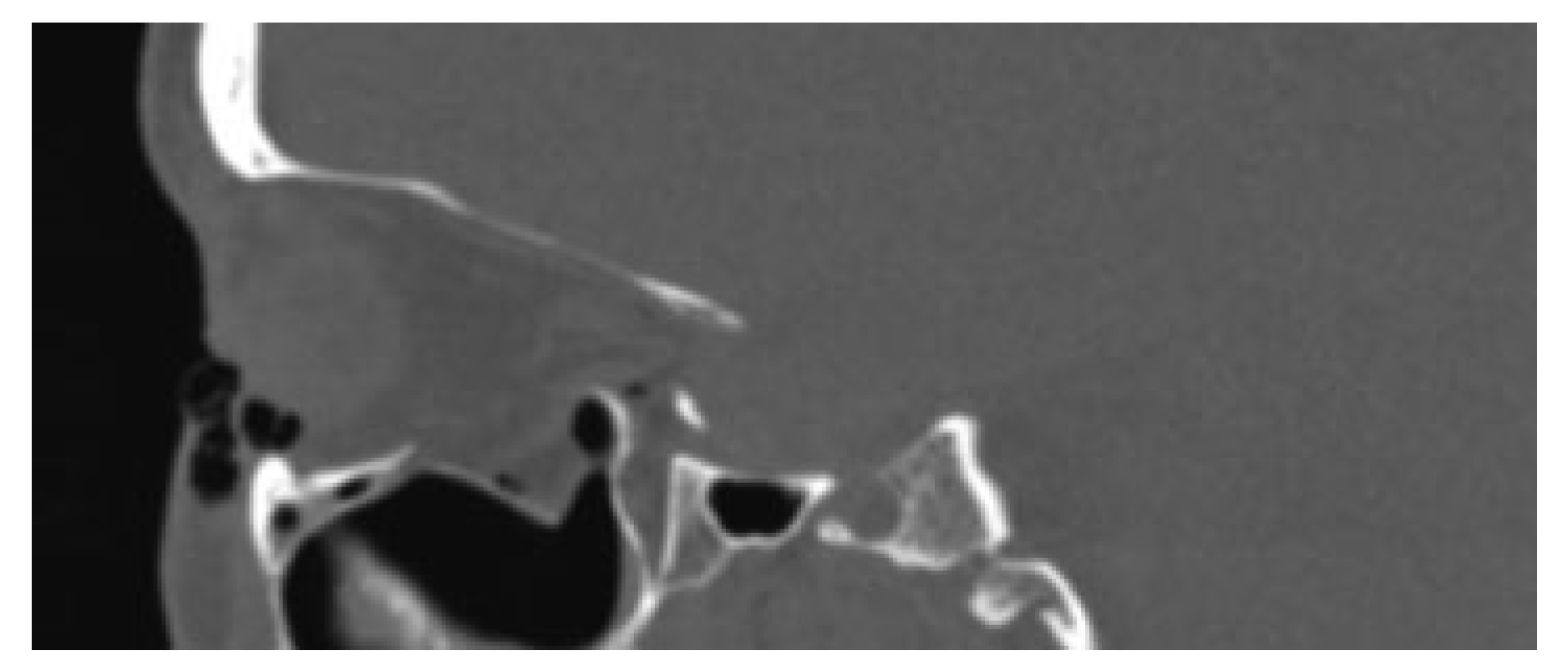
A 59-year-old female presented to the maxillofacial outpatient department following a mechanical fall resulting in a left orbital floor fracture. Enophthalmos of 2 mm was present and a CT scan revealed a large floor defect (
Figure 2 and
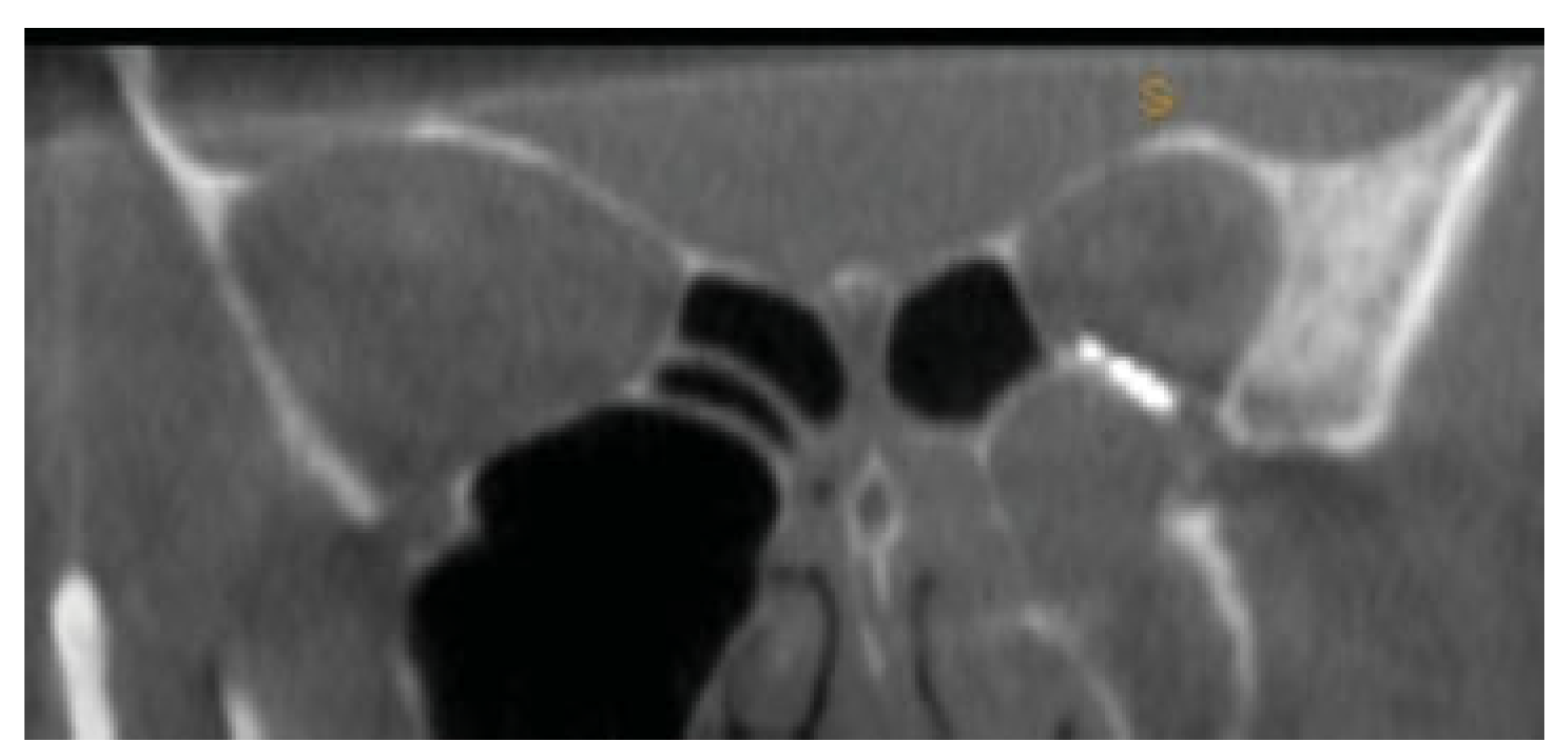
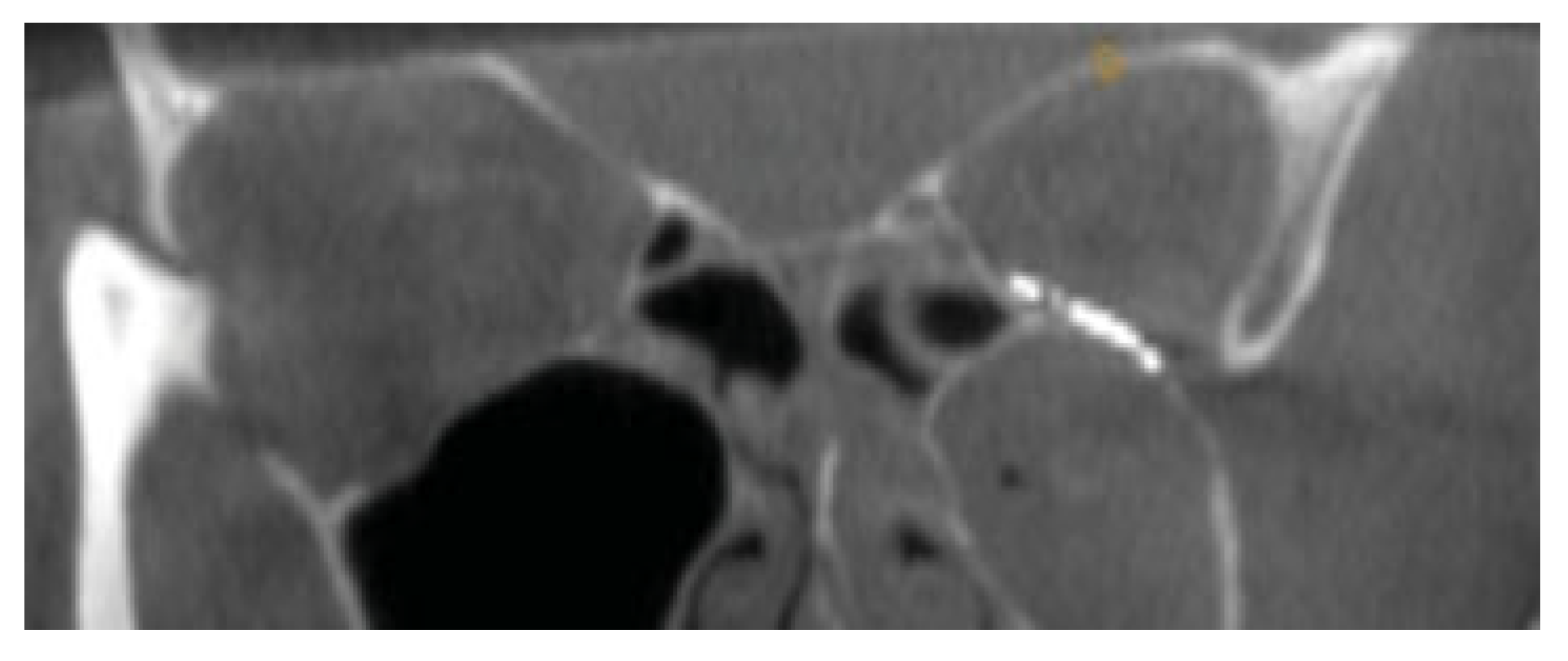
Figure 3). Diplopia was present on upward gaze. A rapid prototyping model was fabricated and a Synthes titanium orbital plate was further adapted preoperatively. The orbital floor was accessed via a mid-lid approach and the modified titanium orbital plate was inserted. No further adaptation of the plate was required and the time taken from insertion of the plate to final fixation was less than 1 minute, as no further adaptation was necessary. Position was confirmed with an intraoperative CT scan (O-arm, Medtronic [Medtronic, Minneapolis, MN]) (
Figure 4,
Figure 5 and
Figure 6). The patient’s diplopia and enophthalmos had resolved 2 weeks postoperatively and no complications were noted at the 6th week follow-up.
Case 2
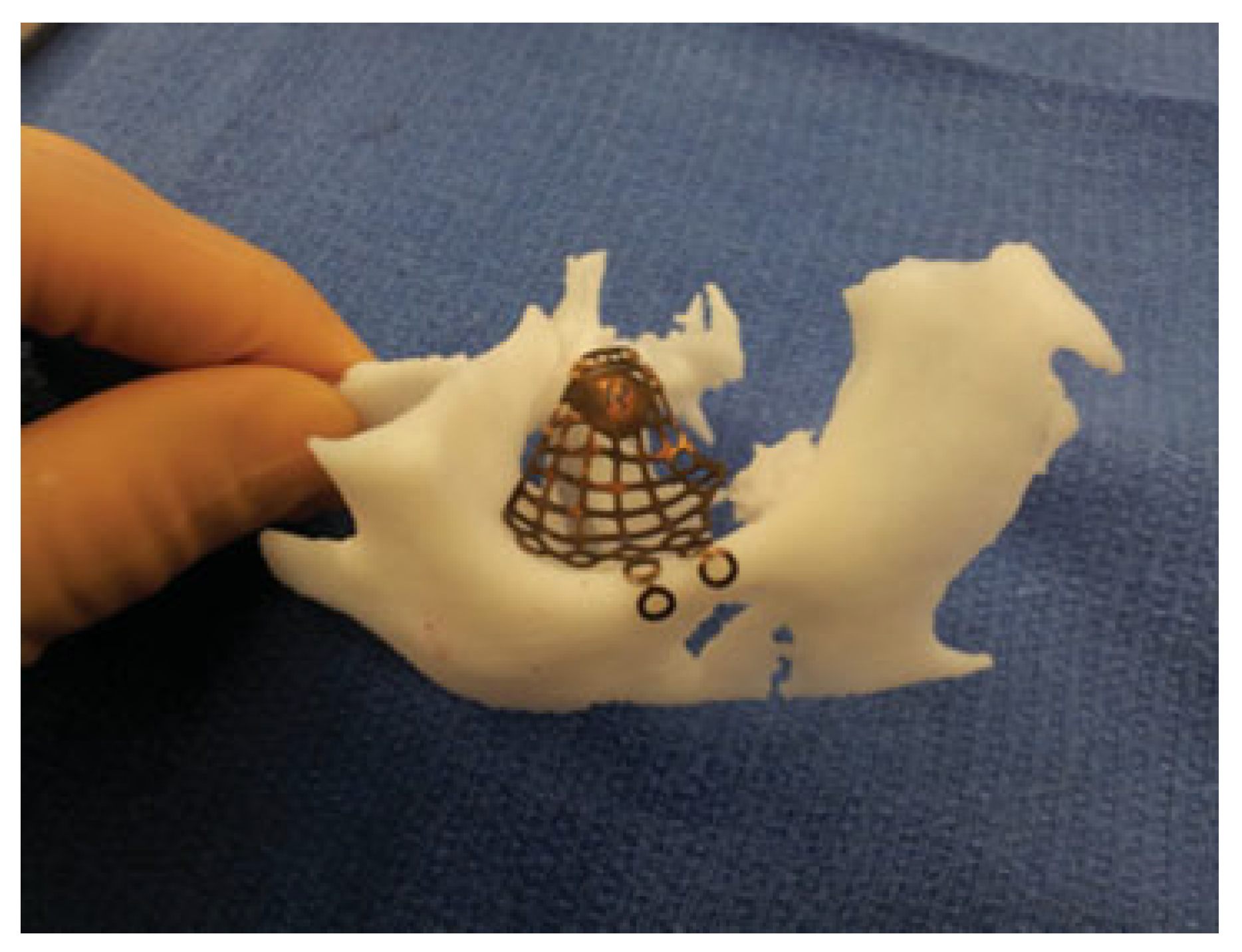
A 50-year-old female was referred to our department from an ophthalmologist with a primary concern of enophthalmos of the right eye following a right-sided facial injury 10 months previously. Enophthalmos of 4 mm and vertical dystopia of 2 mm were noted with no subjective diplopia. A CT scan revealed a large right orbital floor defect with herniation of orbital contents into the maxillary sinus. A rapid prototyping model was fabricated and a titanium orbital plate was adapted to the biomodel (
Figure 7) as per Case 1. The orbital defect was accessed via a transconjunctival approach and lateral canthotomy followed by the modified titanium orbital plate being inserted and fixed to the orbital rim. The position of the plate was examined via an intraoperative CT, which noted a correct anteroposterior position but required medial repositioning to achieve an anatomically correct transverse placement. A second scan was subsequently taken demonstrating correct positioning of the plate. No further adaptation of the plate was required and both the enophthalmos and vertical dystopia resolved. Total time taken for plate positioning was less than 5 minutes. Cosmesis was restored and no complications were noted 6 months postoperatively.
Case 3
A 34-year-old male was referred to the maxillofacial department from an ophthalmologist with a primary concern of enophthalmos due to an orbital floor fracture secondary to an alleged assault. A rapid prototyping model and a titanium orbital plate were used as per the previous cases with the defect accessed via a transconjunctival approach and lateral canthotomy. The adapted plate was inserted and again no further adaptation was needed, as an excellent anatomical contour was noted on the intraoperative CT scan. The total time taken for plate positioning was less than 6 minutes, but this time also included a delay due to intraoperative navigation which was also used to verify anatomical landmarks. Six-week follow-up demonstrated resolution of enophthalmos and no diplopia.
Discussion
Rapid prototyping is an emerging technology and is gaining popularity among oral and maxillofacial surgeons [
3,
4] as a cost-effective method of producing accurate 3D anatomical models. For orbital reconstruction, this process allows for precise adaptation of the titanium plate with respect to important landmarks (e.g., posterior ledge, ethmoidal bulge), which are often difficult to determine intraoperatively. Traditionally, intraoperative trimming of the plate can lead to multiple “try-ins” that can traumatize delicate soft tissue with poor adaptation and positioning, often necessitating revision procedures. Placement of an orbital titanium plate without further adaptation reduces operating time, risk of soft tissue trauma, and allows precise plate positioning and restoration of orbital volume. In the cases above, titanium orbital plates were placed almost immediately with minimal or no further manipulation and no revision surgery was necessary after evaluating implant position with CT. We found there was considerable anatomic variation with regard to the orbital anatomy between the three cases described. Even the “preformed” Synthes orbital titanium plates required a reasonable degree of adaptation on the 3D model to obtain the correct anatomic contour.
3D reproductions of models and their use in surgery have been well documented, but routine use in orbital trauma surgery has probably been underutilized most likely due to high costs associated with third-party propriety model construction. Previous reports have found a higher degree of anatomical accuracy with pre-bent titanium mesh [
5,
6]. A recent study by Strong et al reported that this had “the greatest contour accuracy” when compared with freehand bending in cadaveric orbits [
7]. However, they also noted that stereolithographic modeling incurred the highest cost [
7]. Currently, the price of anatomical models outsourced to medical modeling companies can be considerable. Rapid prototyping models in the above cases were produced for less than
$5 NZD each. Free open source software is available for the image processing and the 3D printer used was less than
$2,000 NZD. The model construction takes less than 90 minutes for a unilateral orbital floor defect. In addition, operating time costs in New Zealand are approximately
$40 NZD per minute. Direct trimming and adaptation intraoperatively may take prolong operative time depending on the extent of the defect and experience of the surgeon when compared with these examples.
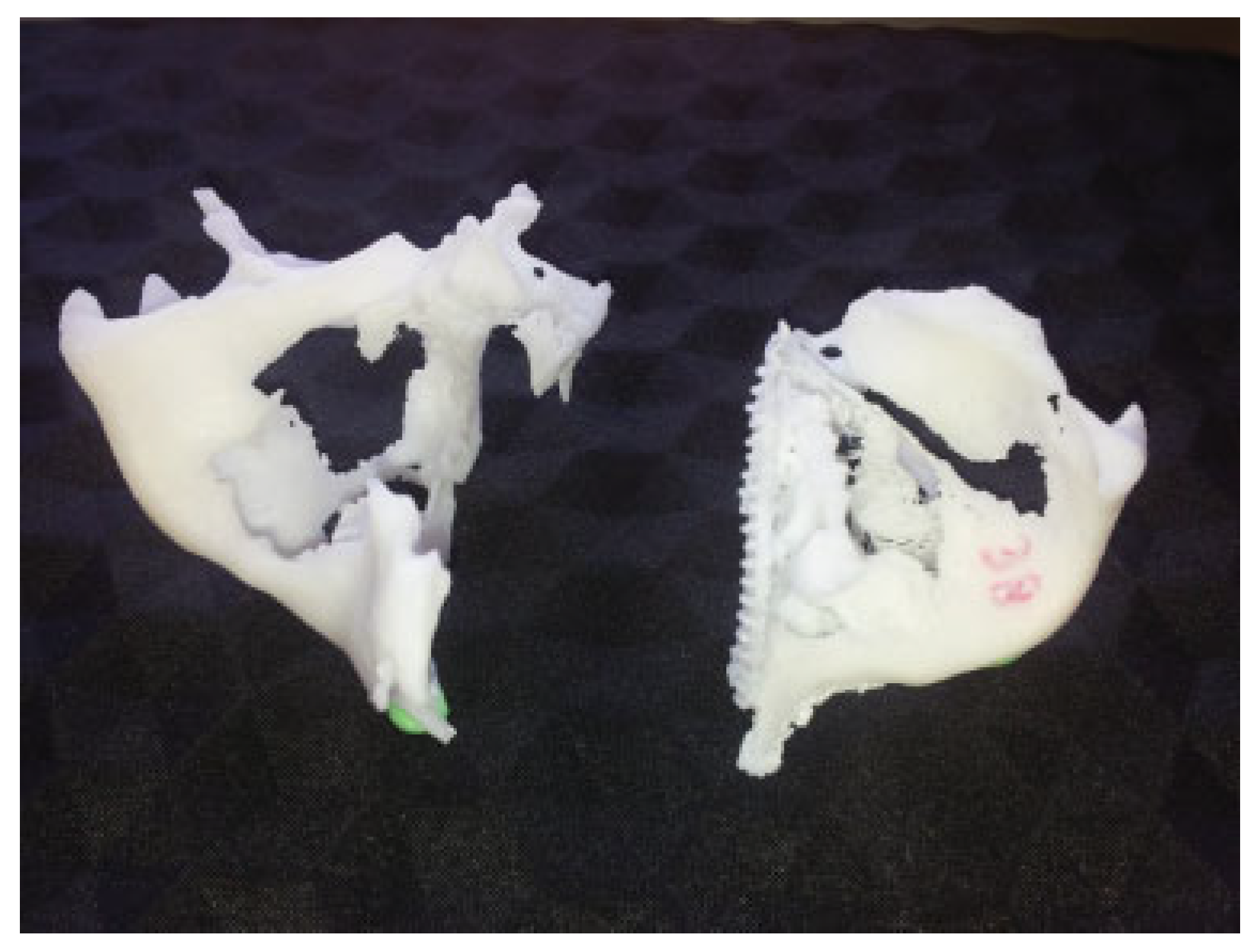
In terms of anatomical detail, we found the data obtained from the CT to be the limiting factor. The previously mentioned CT parameters appear to produce the best anatomic detail. The difference is apparent between the first two cases (
Figure 8) wherein the 3D biomodel for Case 1 had significantly more anatomic surface detail than for Case 2 because improved CT parameters were used. Additionally, dimensional error has been measured for biomodel construction between 0.18 and 0.55% [
8]. This is negligible when compared with limited accuracy of the CT and also negates the need for expensive 3D printers for model construction.
Conclusion
Rapid prototyping gives an economically viable and clinically accurate way to reconstruct orbital floor fractures. The cost of production is minimal and we are using it in our unit to obtain better anatomical contour for orbital fracture repair as well as to reduce operating time. We are undertaking a prospective series of patients for further evaluation.