Reconstruction of craniofacial defects due to tumor extirpation or traumatic injuries can be a daunting challenge for a recon structive surgeon. Loss of key structures has significant functional and cosmetic consequences. The maxilla is functionally involved in digestion, respiration, speech, and facial aesthetics. A maxillectomy for removal of a large tumor can result in defects of the gingiva, palate, maxilla, alveolar bone, zygomatic bone, paranasal sinus, and affect the orbital floor [
1]. Reconstruction of these defects should attempt to obliterate orbital and nasopharynx communication, provide orbital support, reconstruct the palatal surface, and achieve good cosmesis and facial symmetry [
1,
2]. Many methods have been described in the literature to reconstruct maxillectomy defects including obturator prosthesis and numerous flaps (local flaps, pedicled flaps, and microvascular free tissue transfer) [
1,
3,
4,
5,
6,
7]. In scenarios where there is adequate skeletal support, soft tissue augmentation with fat grafting or a free flap may be an option [
1,
5,
6]. For large bony defects, calvarial bone graft or a free bone transfer may be necessary to reconstruct load bearing areas [
1,
4,
6,
8]. In the setting where the tissues have not been irradiated and are free of infection, alloplastic material may provide a satisfactory reconstruction [
9].
Autologous bone and cartilage grafts have been the gold standard for craniofacial skeletal reconstruction. These options carry their own risks with additional morbidity related to increased operation time and an additional operation field. Bone resorption is unpredictable and these grafts may be contraindicated or unfeasible in certain types of reconstruction [
9]. Therefore, alloplastic materials have become a more important aspect of the oromaxillofacial and plastic surgeons armamentarium. The use of porous polypropylene (MEDPOR, Stryker Craniomaxillofacial [CMF], Portage, MI) implants has been well-documented for the augmentation of the facial skeleton [
9,
10,
11,
12]. MEDPOR is a biocompatible substance that does not resorb or degenerate. It can be contoured and carved to obtain a precise, three-dimensional (3-D) construct for fixation. At times, it can be difficult to shape these implants to the exact proportions with the soft tissue envelope obstructing visualization and placement. To overcome this difficulty, the use of a 3-D model for craniofacial skeletal defects can be used, optimizing the modification of prefabricated porous polypropylene facial implants following tumor resection.
In this article, we present a patient that underwent suprastructure maxillectomy 8-months before for a benign tumor. He was reconstructed with a MEDPOR 2/3 orbit porous polypropylene implant which was modified with the aid of a preoperative 3-D model.
Clinical Report
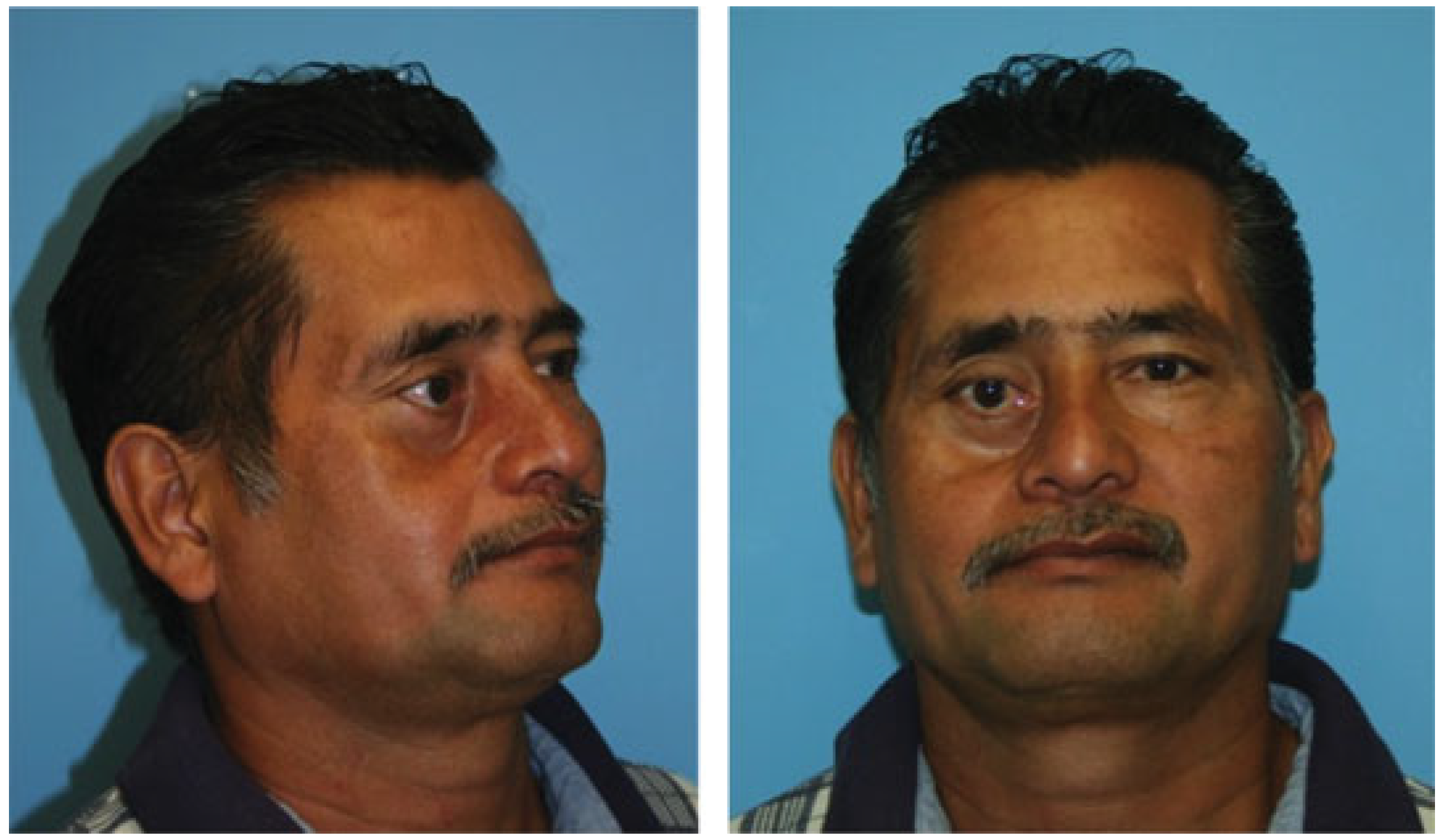
A 52-year-old gentleman was referred to the plastic surgery clinic with a significant right zygomaticomaxillary depression, hypoglobus, and symptomatic diplopia (
Figure 1). Around 8-months back, the patient was diagnosed with a right maxillary sinus mass, which was initially suspected to be a malignant tumor due to the extent of local destruction and orbital invasion. He underwent a right suprastructure maxillectomy via a Weber-Ferguson incision to remove the mass. Due to concerns for an aggressive tumor, the head and neck surgery service did not reconstruct his resultant defect at the time of resection. The final pathology demonstrated that the maxillary sinus mass was a cellular myxoma and the patient would not need post-operative radiation. Unfortunately, the patient was lost to follow-up for several months, at which point he was referred to the plastic surgery clinic for reconstruction.
After discussion of surgical options, the patient was interested in the route requiring the least amount of surgery to correct his defect and vision. The patient’s nonirradiated skin envelope on his right face appeared soft and supple, and the only deficiency was the underlying skeletal support. It was felt that a prefabricated MEDPOR 2/3 orbital implant porous polypropylene implant could adequately correct the contour deformity and reposition the right globe. There would be no skin defect with the subsequent skeletal reconstruction.
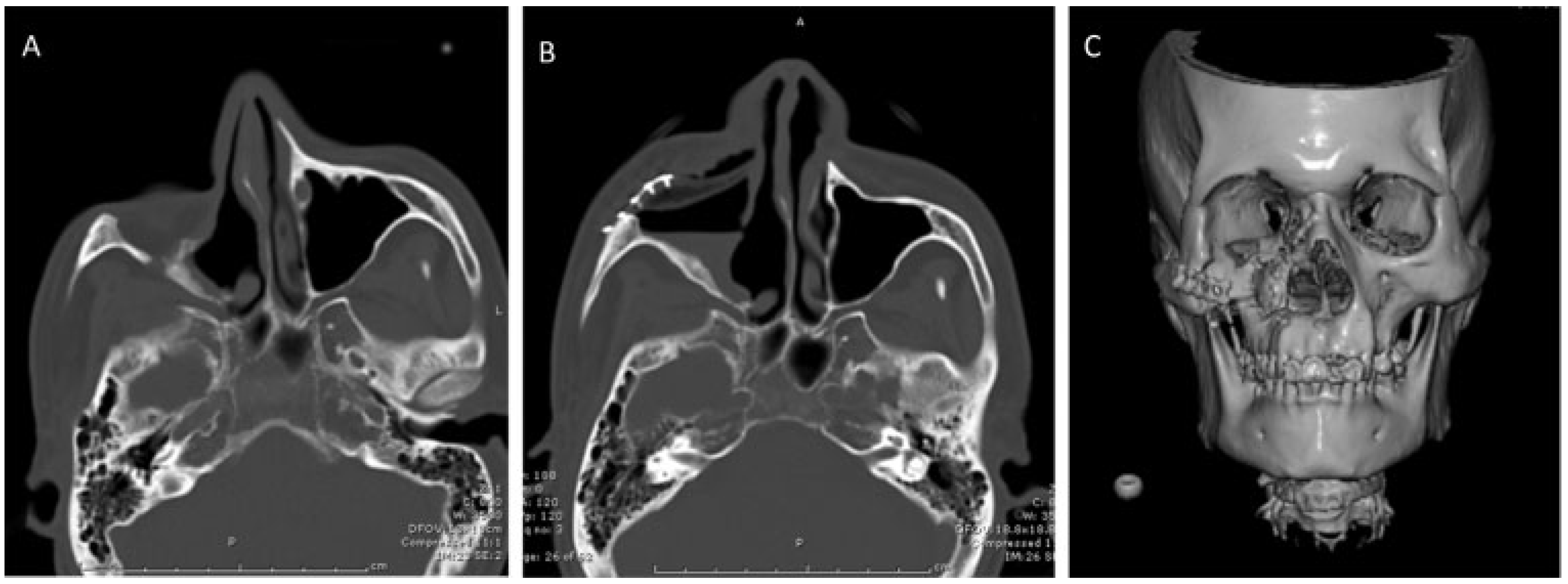
During the initial consultation, craniomaxillofacial computed tomography (CT) scan was ordered with 1 mm cuts for preoperative planning and to assess the extent of the right zygomaticomaxillary defect (
Figure 2A). A 3-D model was made from the CT scan images (
Figure 3) for preoperative shaping of the right 2/3 orbital porous polypropylene implant, which would be used to help with the intraoperative shaping of the implant.
During surgery, the previous Weber-Ferguson incision was used to elevate the skin envelope from the zygomaticomaxillary defect (
Figure 4). Sufficient care was taken to separate the orbital contents from the skin flap and the scar tissue to avoid injury to the globe. The right medial canthal tendon was severely malpositioned from the previous surgery. The fibrous tissue that accumulated in the suprastructure maxillectomy defect was removed to allow exposure of the bony margins of the defect.
The 3-D model was then placed in a sterile X-ray cassette cover and brought onto the surgical field where the porous polypropylene implant was modified to fit into the defect with Mayo scissors and a cutting burr (
Figure 5). Care was taken to ensure symmetric orbital floor height and malar projection with the contralateral structures on the 3-D model. Once the implant appeared to fit well into the model it was placed into the patients defect. Minor modifications to the implant were made to address any additional soft tissue that the 3-D model did not take into account. The implant was then secured to the craniofacial skeleton with standard gold midface plates and 1.2 mm screws (Stryker Leibinger Midface module, Stryker Craniomaxillofacial (CMF), Portage, MI) (
Figure 6). The wound was then irrigated. The medial canthal tendon was then reattached to the tendon remnant on the facial skeleton with a 5–0 nylon suture. The skin flap was anchored to the infraorbital rim portion of the implant with three 4–0 polydioxanone sutures (Ethicon, Cornelia, GA) in simple interrupted fashion. The remaining facial incision was closed in layers (
Figure 7). An immediate postoperative CT scan showed adequate anatomical reconstruction of the zygomaticomaxillary defect (
Figure 2B,C).
In the recovery room, the patient noted resolution of hisdiplopia and was discharged home on his first postoperative day with oral antibiotics. On his 1-week follow-up appointment, he was noted to have erythema on his right cheek without signs of infection or drainage from his incisions. He indicated that he did not start taking his antibiotics until earlier that day. He returned a week later with complete resolution of his erythema but remained mildly edematous on the right face.
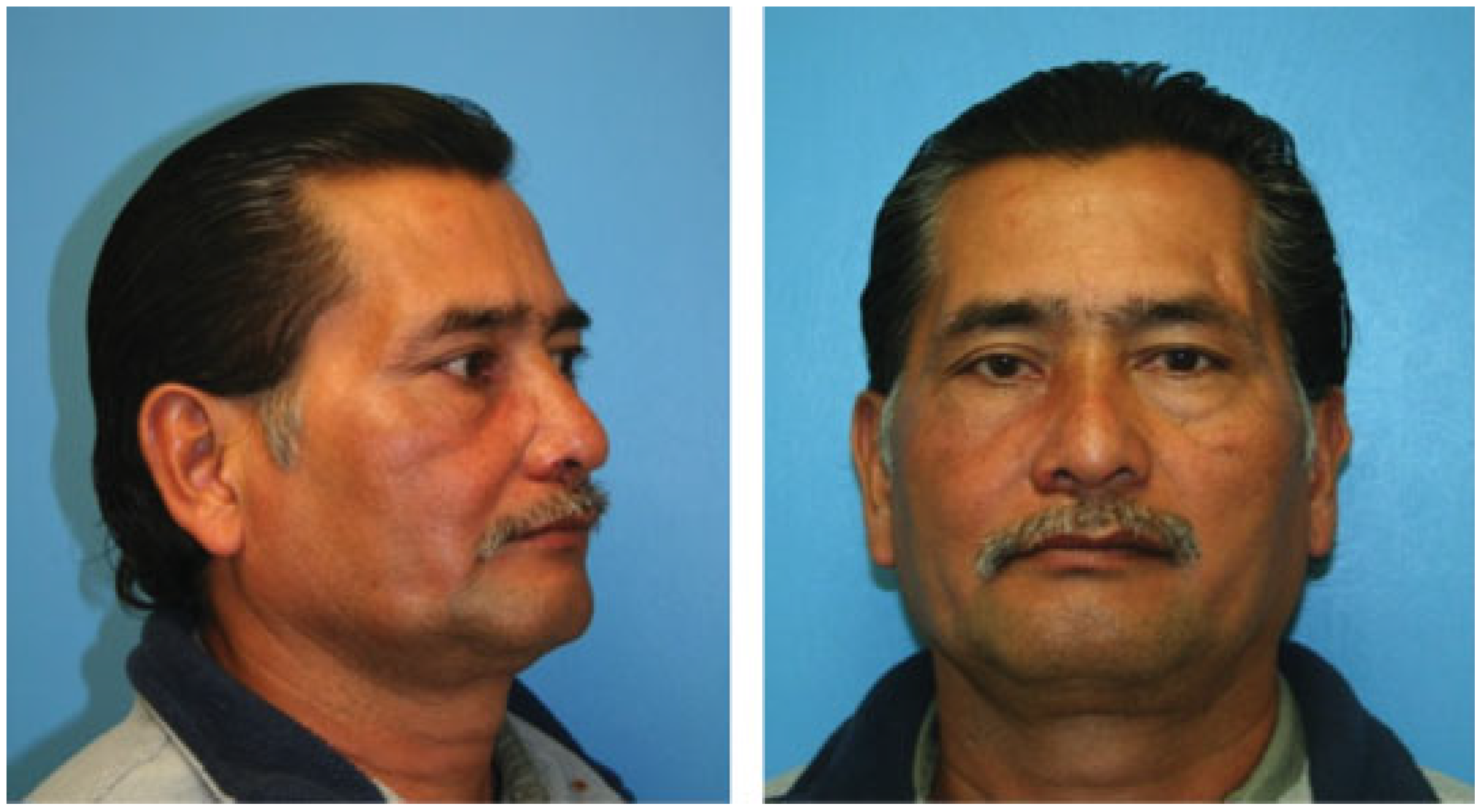
On his 9-month follow-up visit, he did not have recurrence of diplopia and his final result demonstrated improved symmetry and aesthetics (
Figure 8). He had normal movement of his right globe and animation of his face.
Discussion
Every patient’s residual deficits following tumor resection or trauma are unique and thus the surgeon needs to attain a detailed understanding of the individual’s anatomy preoperatively. Thorough physical examination and imaging may allow sufficient preoperative surgical planning. In more complex conditions, specific information relating to the in ternal structures’ morphology is often required. To obtain this internal anatomical information noninvasively, the surgeon relies on medical imaging and 3-D models [
13,
14].
Reconstruction of craniofacial disorders has been aided by 3-D models for the past two decades, particularly with free fibula preoperative surgical planning [
1,
4,
6,
7,
9,
13,
14,
15] With better quality CT scans and cheaper production costs, these 3-D craniofacial models have become readily available for use in the operating room. D’Urso et al. studied craniomaxillofacial and skull base cervical spinal pathology and found 3-D models significantly reduced operation time and risk and improved operative planning and team communication [
13]. Wulf et al. further concluded that craniofacial and maxillofacial reconstruction benefit greatly from incorporating 3-D models into their reconstructive surgeries [
16]. The very accurate physical models allow for simulation of the surgical procedure and preoperative shaping and planning of the implant or free flap improving its design and fit, while reducing operative time [
7,
14]. With more detailed information, surgical planning can result in improved facial symmetry and functionality for these patients [
14]. This article reports the application of an innovative 3-D model approach for the calculation of the exact contours, angles, length, and general morphology of the prefabricated MEDPOR 2/3 orbital implant for reconstruction of a suprastructure maxillectomy defect.
The prefabricated MEDPOR 2/3 orbital implant for zygomaticomaxillary reconstruction provided the ideal reconstructive option in this particular patient and avoided donor site morbidity. Since the patient presented for a delayed reconstruction, the exact size of the skeletal defect could be obtained from a preoperative CT scan and a 3-D model could be made. This particular implant could address all of the patients concerns in a single surgery. It added volume and projection to the right zygomaticomaxillary complex while reestablishing an orbital floor to correct the hypoglobus. Hypoglobus correction would improve his most significant complaint, diplopia. With the 3-D model, the implant was precisely modified on the sterile table to limit contamination of the implant. The location of the defect allowed the implant to stay out of the oral cavity and be covered by a nonirradiated skin envelope to permit vascular ingrowth.
A notable downside with the porous polypropylene implant is the concern for infection in the immediate postoperative period before tissue ingrowth can occur. Tissue ingrowth through the pores allows biointegration which prevents extrusion and exposure, reported complications in this early postoperative period [
9,
17,
18]. Our patient experienced facial erythema, and a concern for early cellulitis, therefore was started on antibiotics. The suspected cellulitis was treated aggressively with antibiotics because we felt that a localized infection around the implant would hinder tissue ingrowth and possibly require removal of the implant. Fortunately, the erythema resolved. Given the porous nature of the implant, soaking the implant in an antibiotic solution before placement may have mitigated this concern. Local application of prophylactic antibiotics allow for high and sustained concentrations of the antibiotic at the surgical site to prevent infection formation [
19]. A concern for sinus contamination in these large implants exists, however studies have shown that exposed MEDPOR in the sinus or nasal cavity will reconstitute mature mucosa overlying the defect and permit the low complications reported [
20,
21,
22]. Once biointegration has occurred, MEDPOR reduces the infection rate secondary to vascular invasion through the pores allowing a systemic immune response to infection and systemic delivery of antibiotics to the implant [
9,
12,
17,
18] Care should be taken when attempting to place these materials in defects with an inadequate soft tissue envelope for coverage, previously radiated tissue, or when there is active infection as these can lead to poor outcomes.
While the patient’s condition drastically improved with the procedure, he continues to have some subtle asymmetries with the contralateral side. Most notably, his medial canthus is slightly lower on the right despite anchoring it to the remaining tendon stump. A better option may have been to perform transnasal wiring, as with a naso-orbital-ethomoid fracture, to firmly secure the tendon to bone [
23]. He also had more pronounced midface decent on the right side of his face despite resuspending the cheek skin to the implant. The patient was offered a revision surgery to correct both of these asymmetries, but he declined.
The prefabricated porous polypropylene 2/3 orbital implant alone is an option for facial skeletal reconstruction for a subset of patients who have adequate soft tissue coverage over a craniofacial skeletal defect. For patients presenting in a delayed fashion, a preoperative 3-D model is an ideal way to efficiently modify prefabricated porous polypropylene implants. This method allows the surgeon to easily optimize the shape of the implant without having to continually place it in and take it out of the patient, thus decreasing the chance for contamination and iatrogenic injury to the patient. Combining the use of porous polypropylene implants with a 3-D model allows refinement of the reconstructive surgery by reducing operation duration and surgical risks; and improving surgical outcomes and aesthetics. We believe this is particularly useful in situations where the normal craniofacial anatomy is considerably distorted as in oncological resections, trauma, and congenital malformations; and defect can adequately be reconstructed with an alloplastic implant.