Complication of Anterior Iliac Bone Graft Harvesting in 372 Adult Patients from May 2006 to May 2011 and a Literature Review
Abstract
Materials and Methods
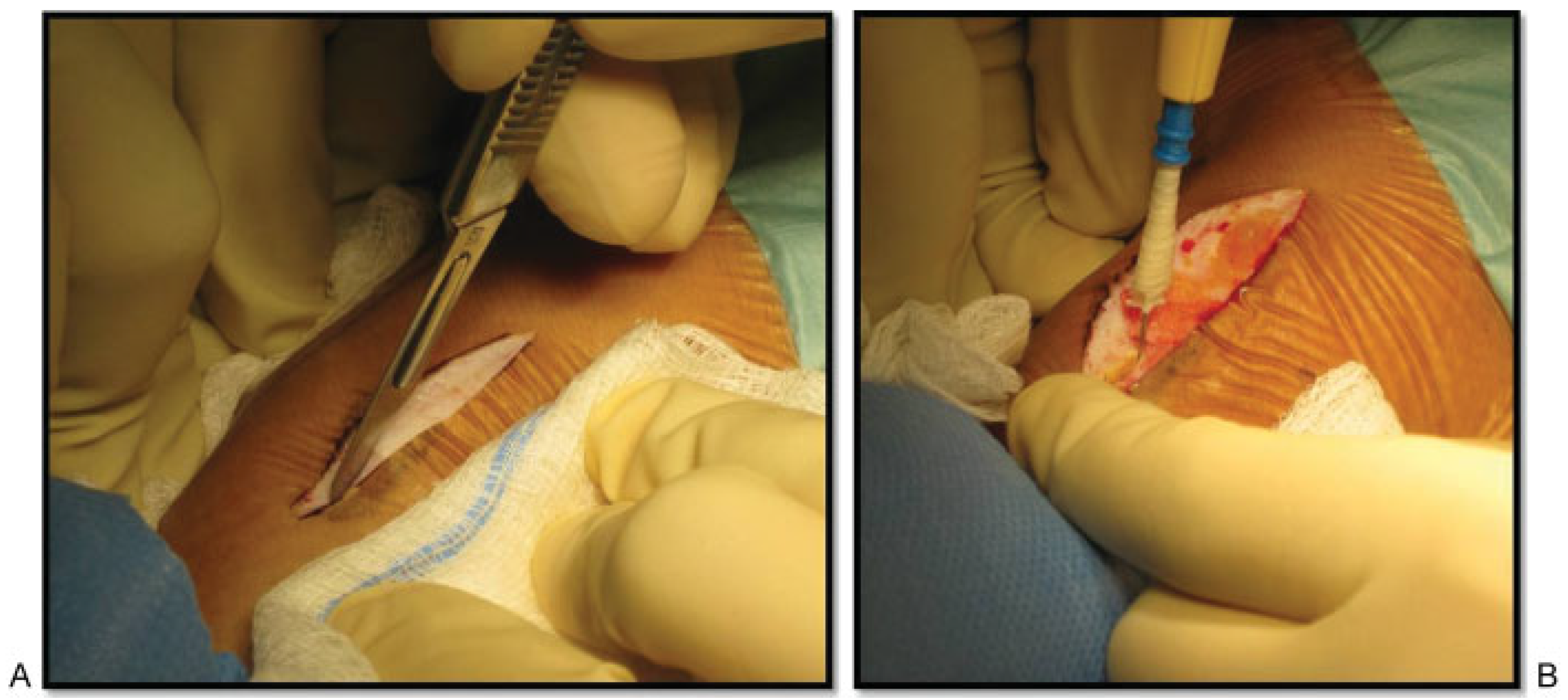
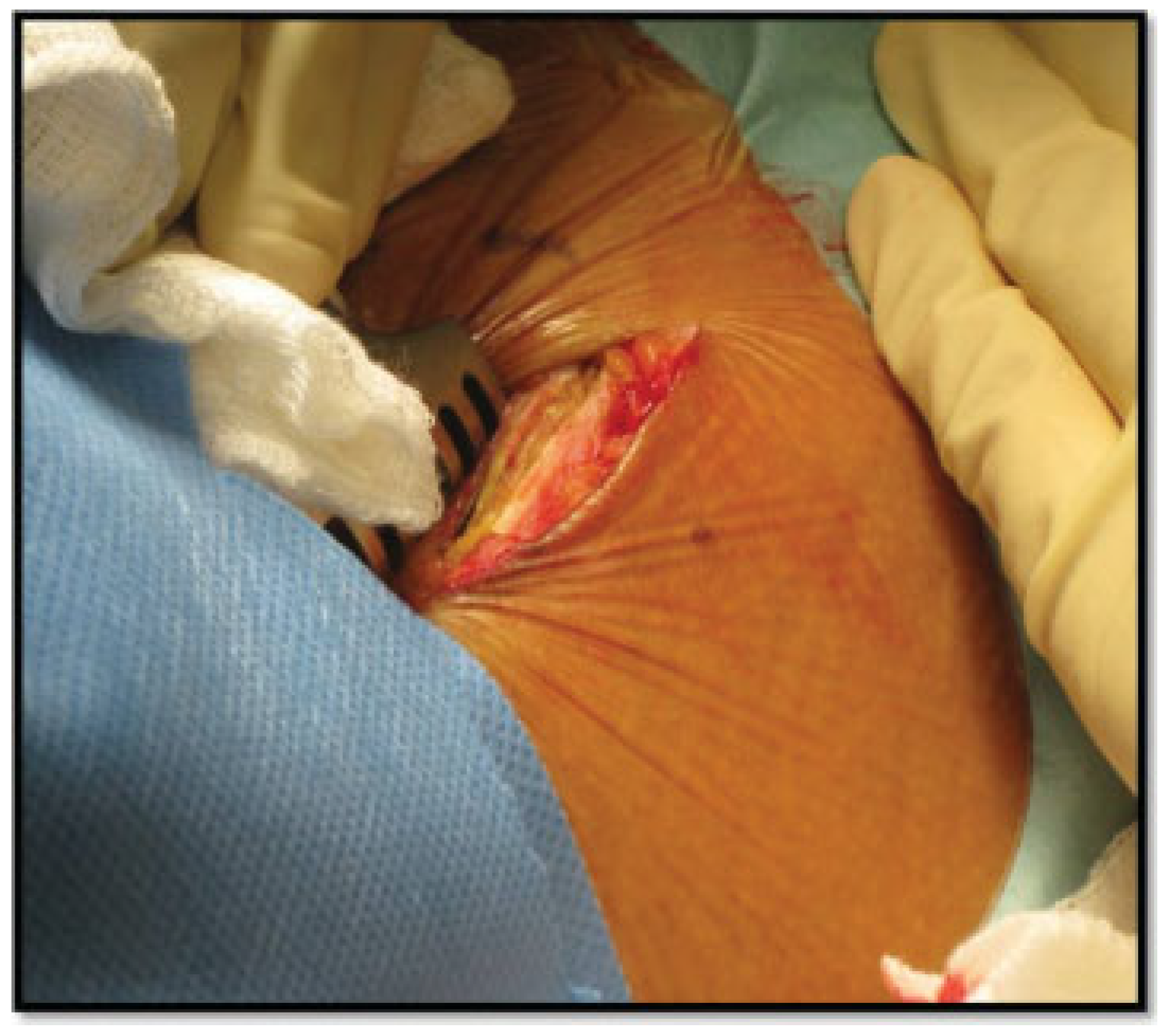
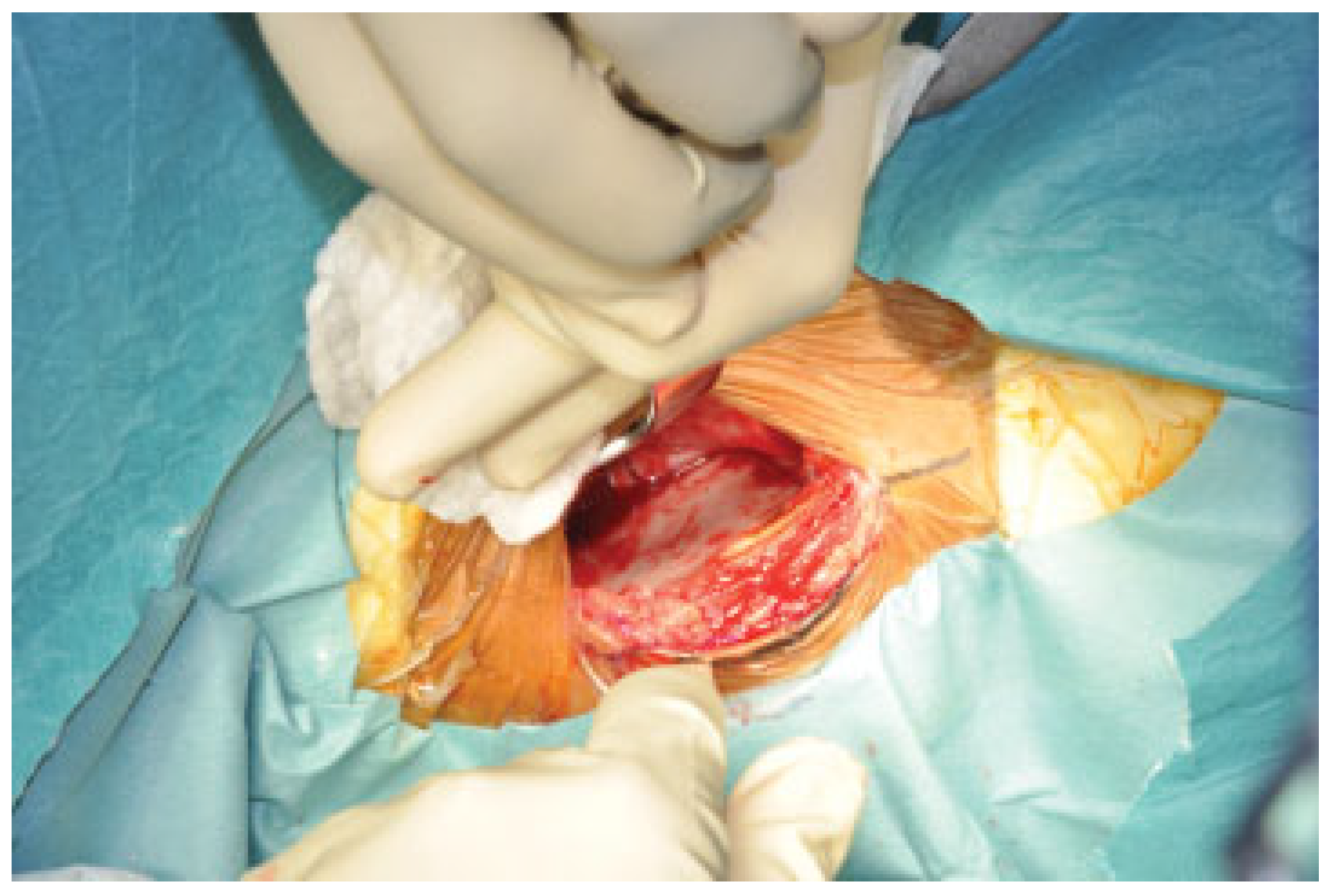
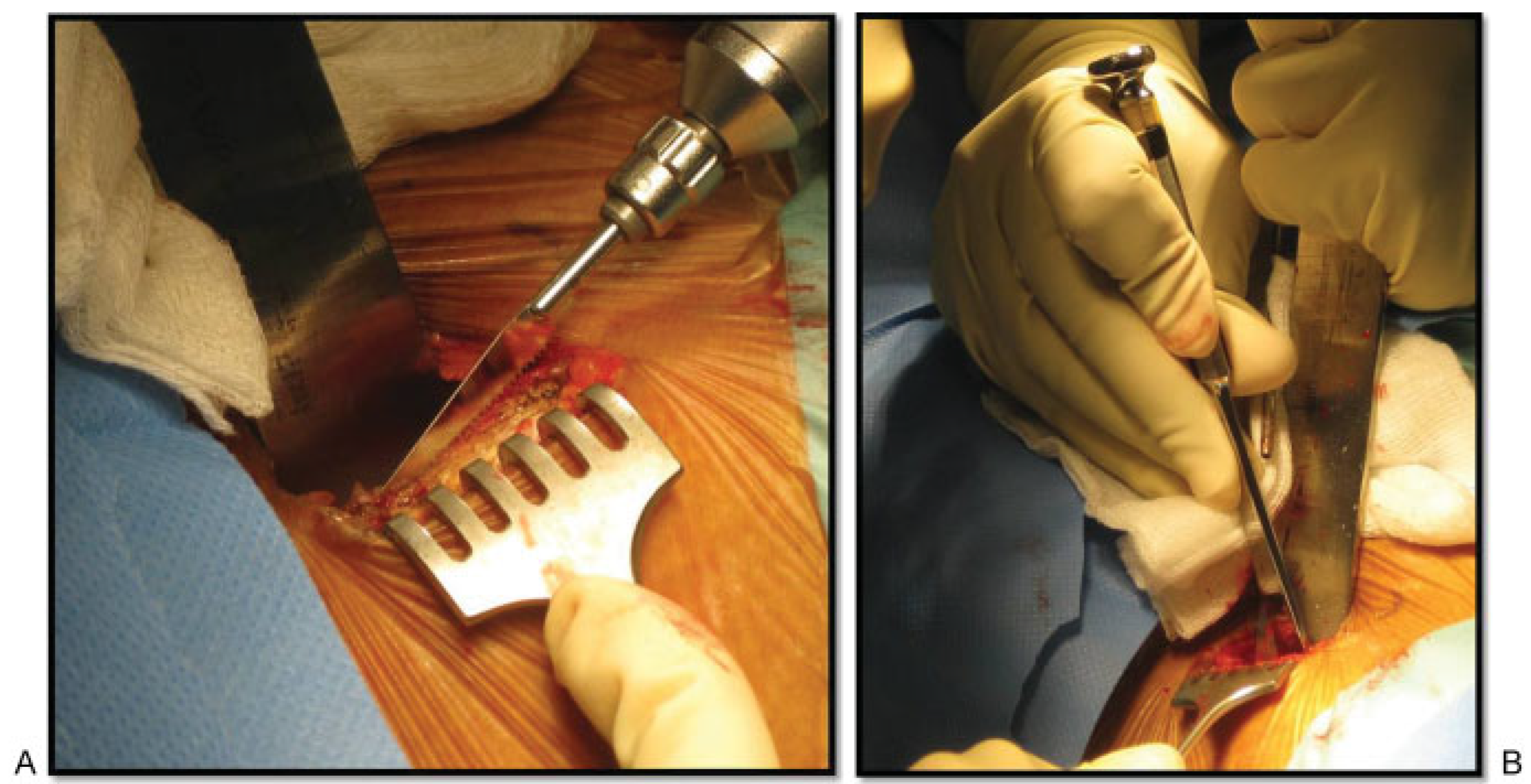
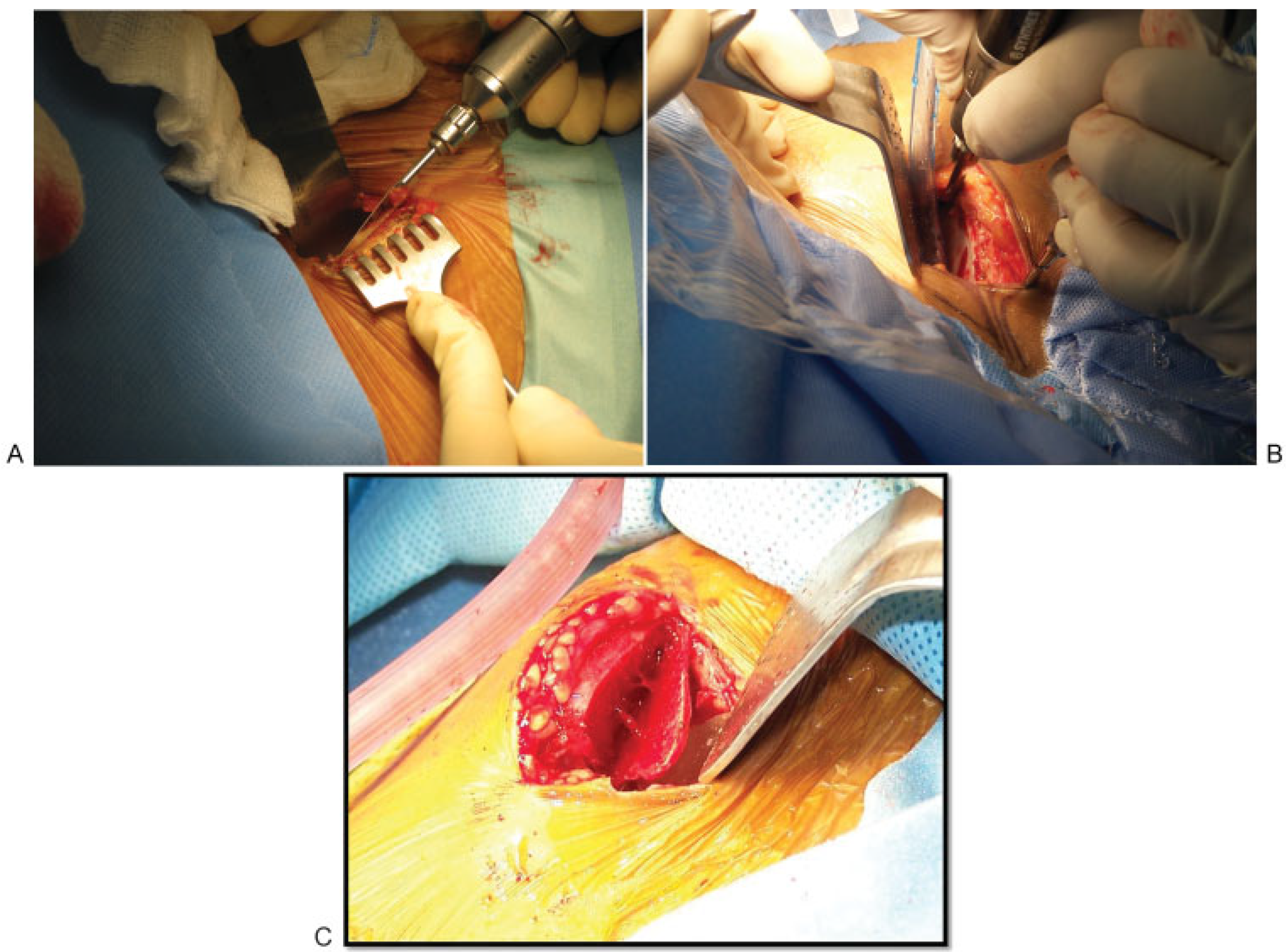
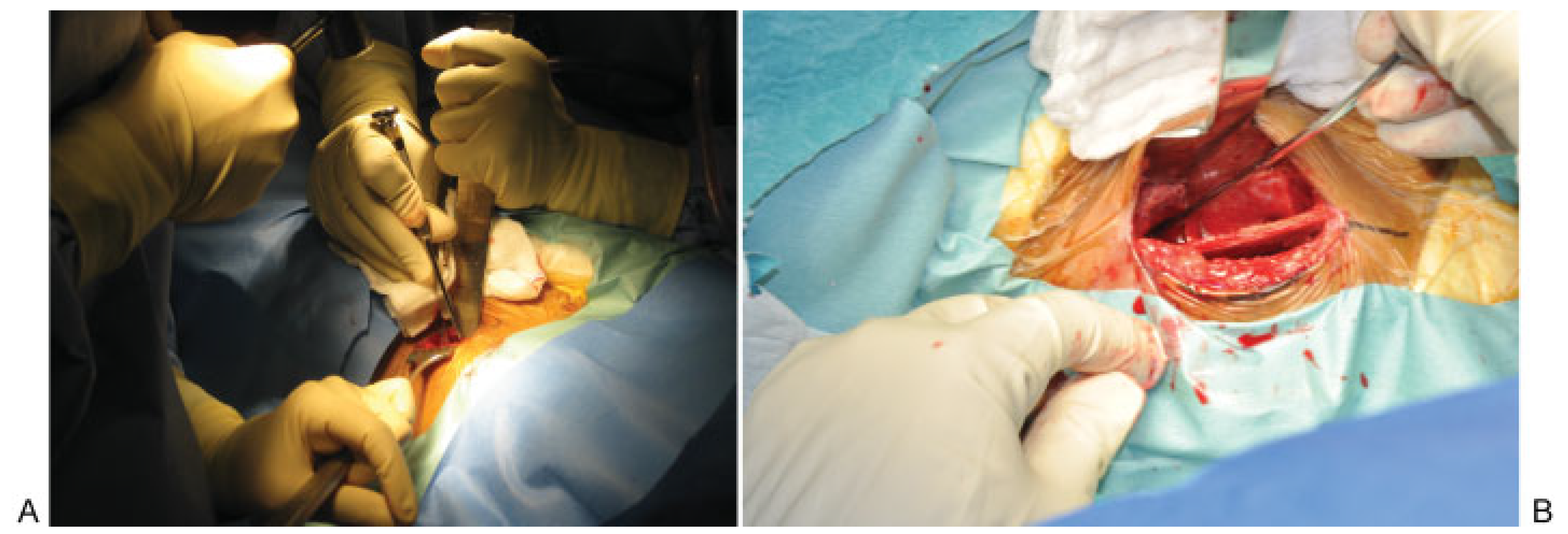
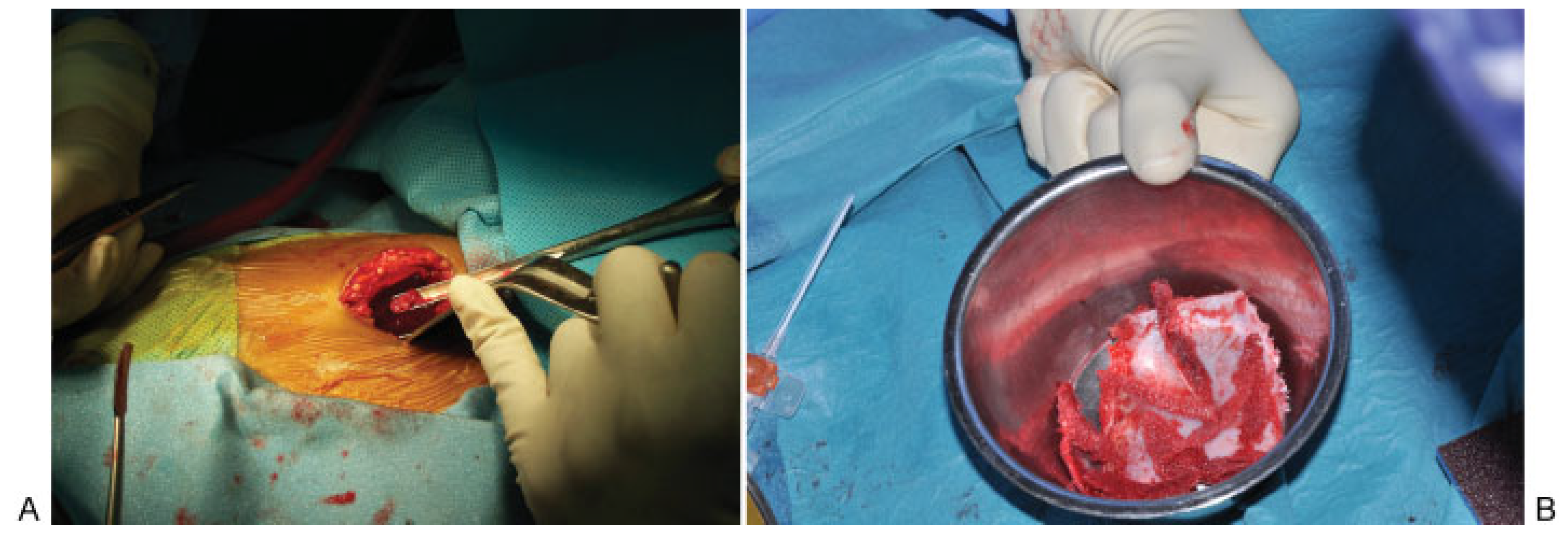
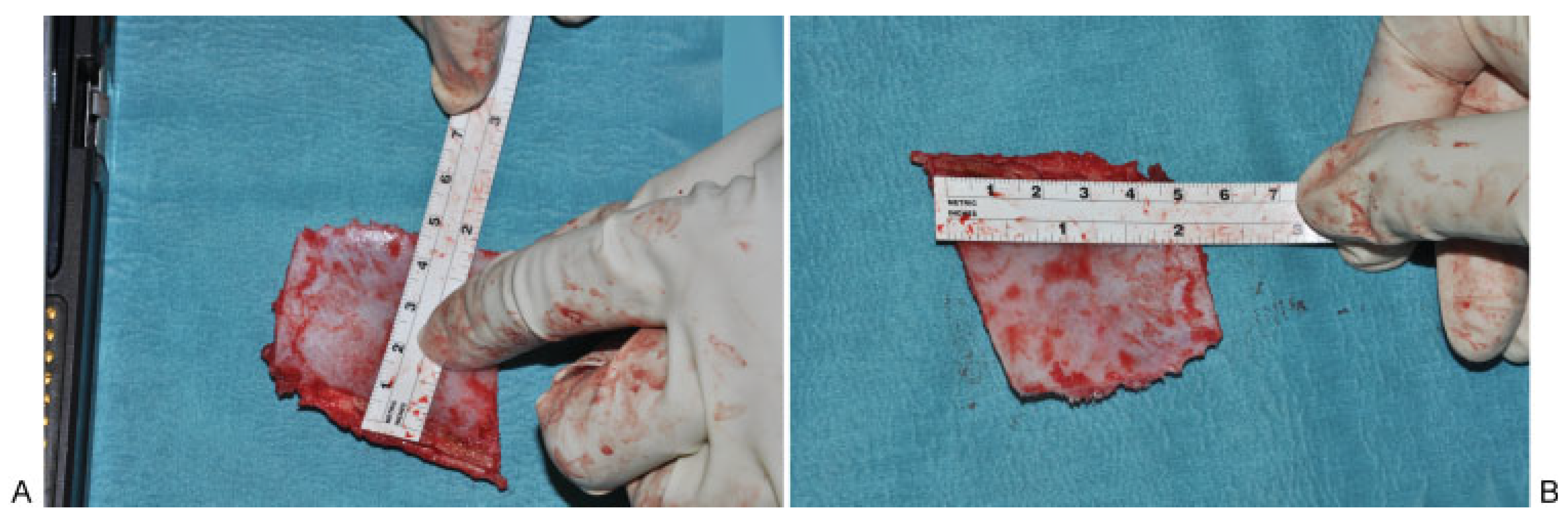
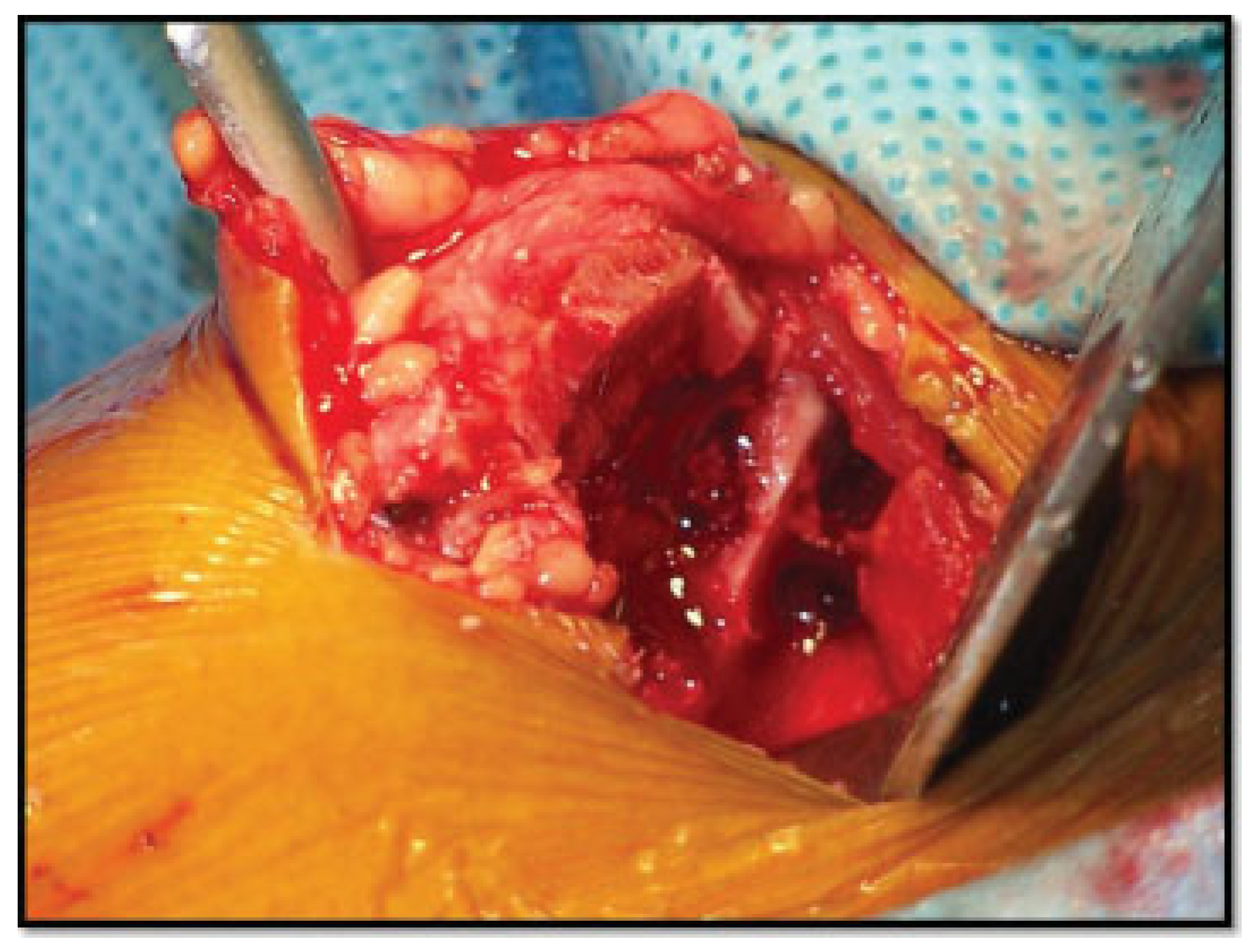
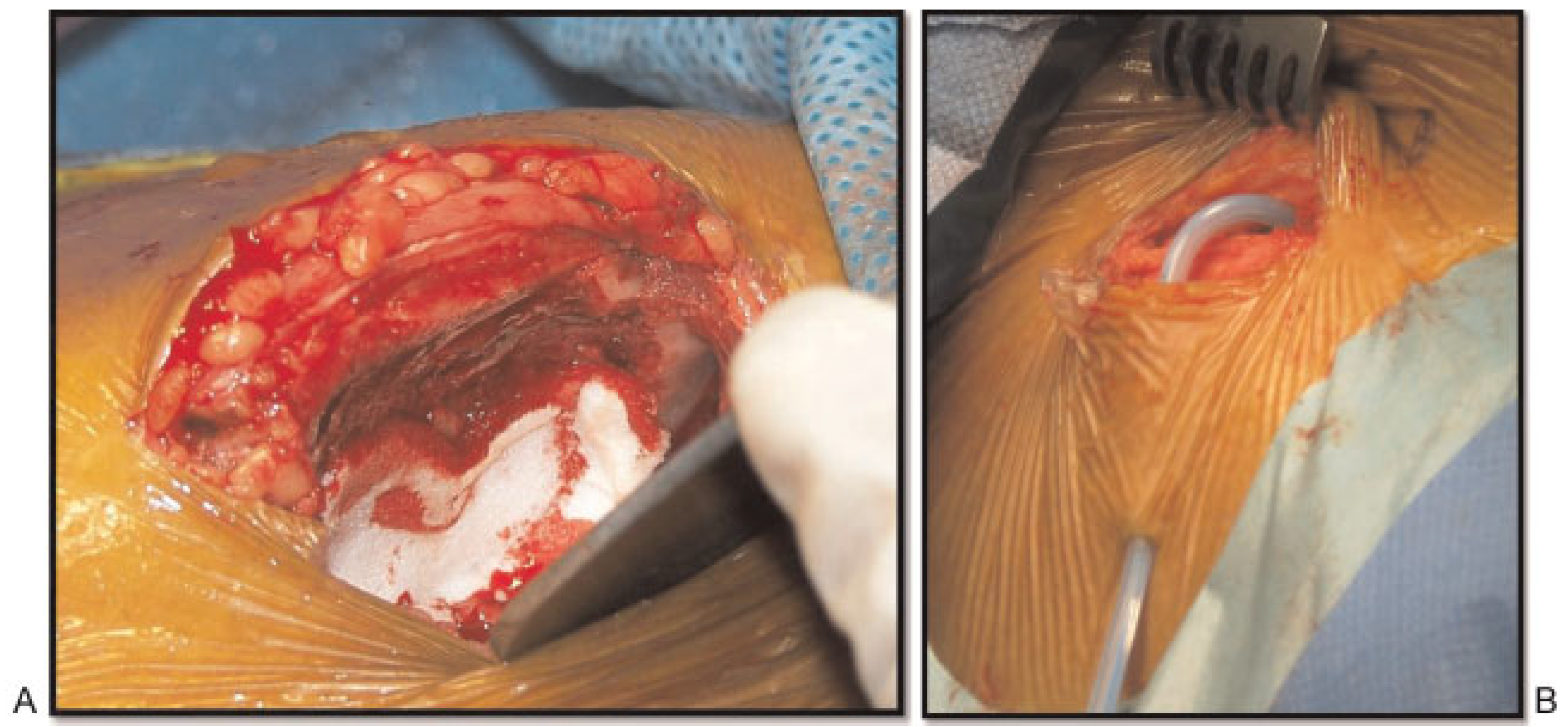
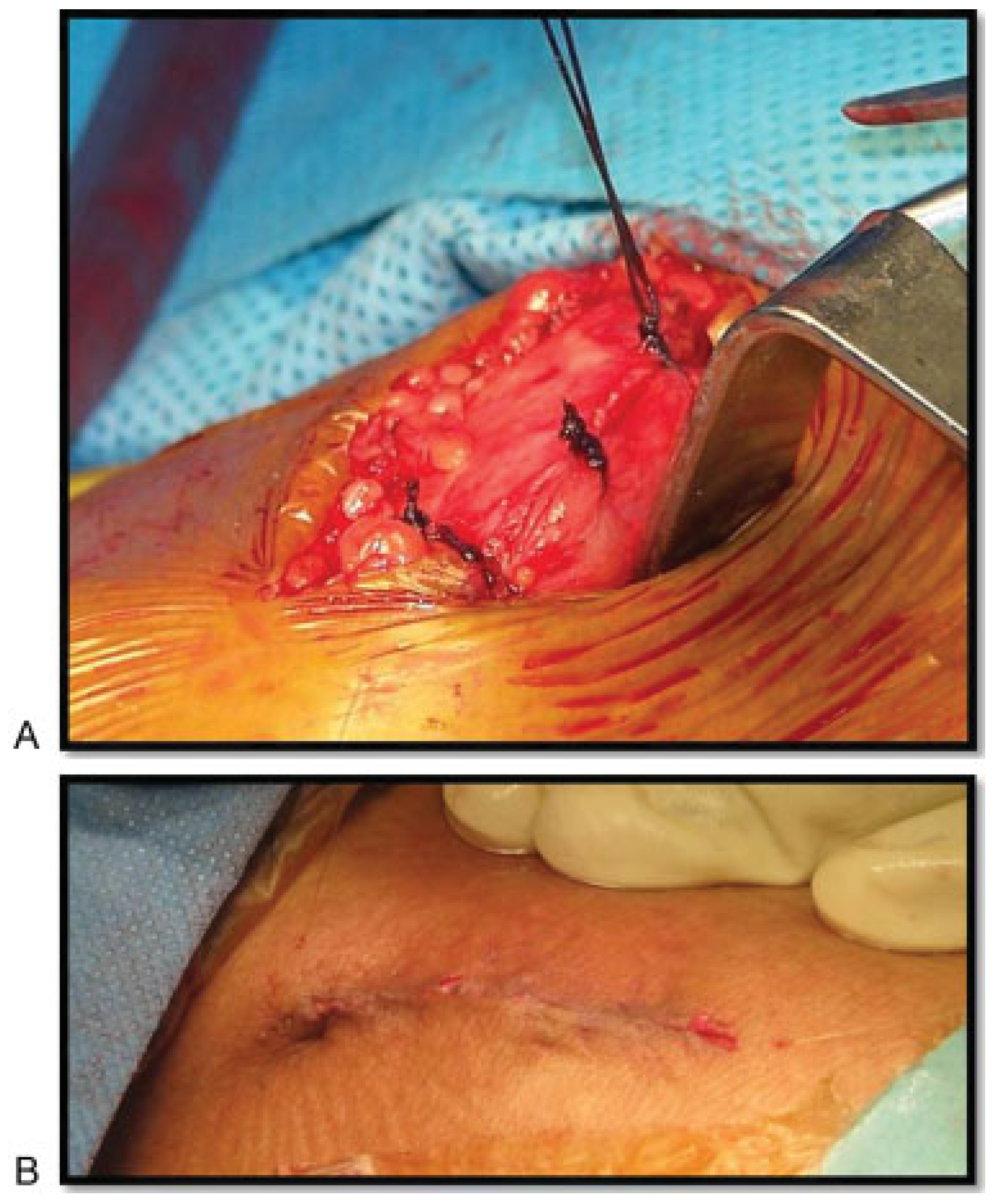
Surgical Technique
Postoperative Care
Result
Complications
- Seroma: Of the 372 patients, 1 patient (0.269%) developed seroma, approximately 25 mL been aspirated (Figure 19A–C).
- Fractures: Of the 372 patients, 2 patients (0.538%) developed fracture iliac, 1 patient developed greenstick fracture of the iliac wing intraoperative and the case was managed with lag screw, and the other patient had the fracture iliac 25 days postoperative secondary to carrying 45 kg of sac of rise and he was managed conservatively (Figure 20).
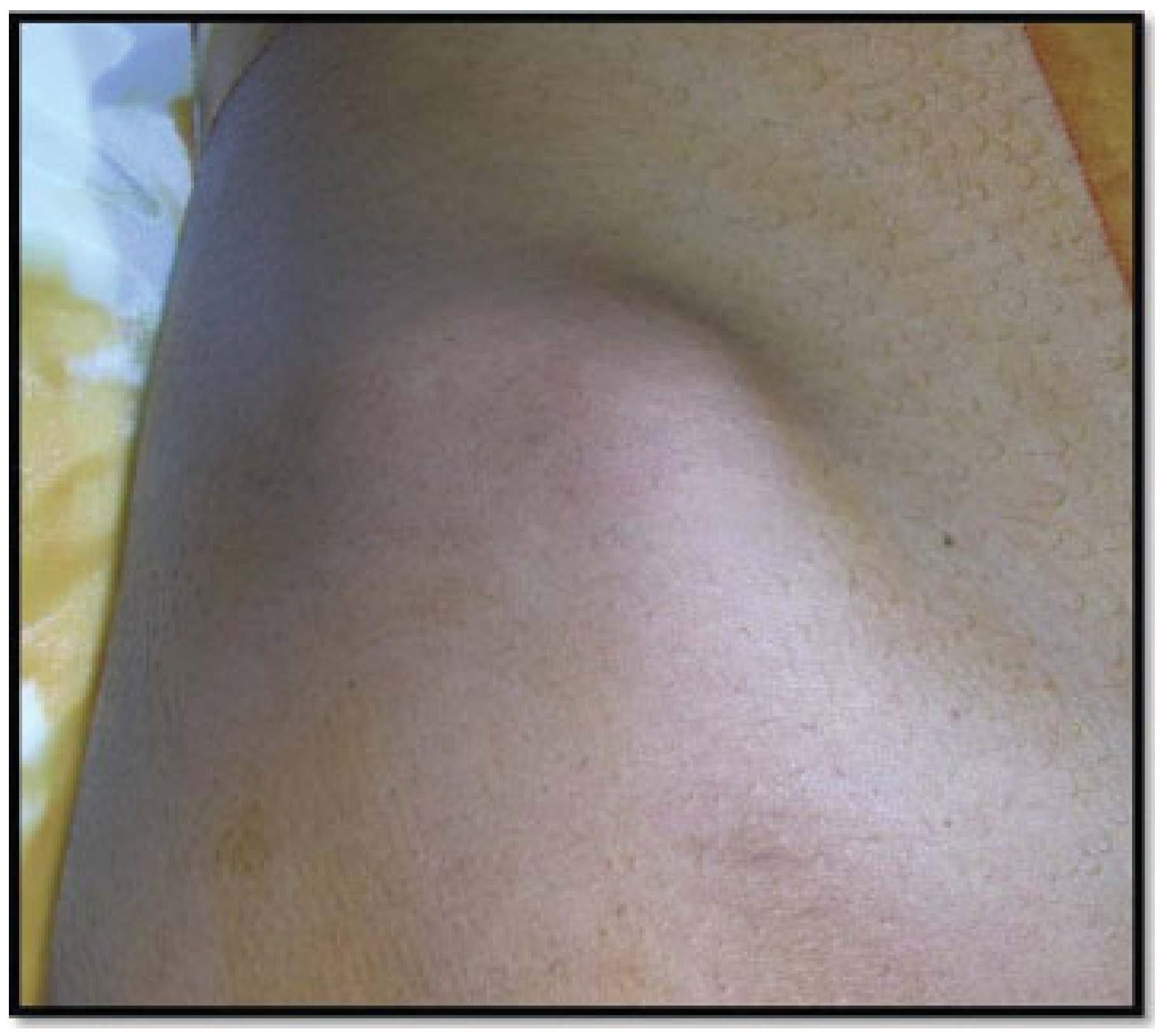
- Major hematoma: Of the 372 patients, 1 patient (0.269%) developed major hematoma secondary to excessive daily activities and exercises (Figure 21).
- Temporary neurosensory disturbance: Of the 372 patients, 3 patients (0.806%) developed temporary sensory disturbance, which was managed conservatively.
- Duration of pain: Of the 372 patients, all the patients (100%) suffered pain within the first 15 days postoperative, and they were managed with a proper analgesic (Figure 22).
Discussion
Conclusion
References
- Schaaf, H.; Lendeckel, S.; Howaldt, H.-P.; Streckbein, P. Donor site morbidity after bone harvesting from the anterior iliac crest. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010, 109, 52–58. [Google Scholar] [CrossRef] [PubMed]
- Dösoğlu, M.; Orakdöğen, M.; Tevrüz, M.; Göğüsgeren, M.A.; Mutlu, F. Enterocutaneous fistula: A complication of posterior iliac bone graft harvesting not previously described. Acta Neurochir (Wien) 1998, 140, 1089–1092. [Google Scholar] [PubMed]
- Fernando, T.L.; Kim, S.S.; Mohler, D.G. Complete pelvic ring failure after posterior iliac bone graft harvesting. Spine 1999, 24, 2101–2104. [Google Scholar] [CrossRef] [PubMed]
- Younger, E.M.; Chapman, M.W. Morbidity at bone graft donor sites. J Orthop Trauma 1989, 3, 192–195. [Google Scholar] [CrossRef] [PubMed]
- Zouhary, K.J. Bone graft harvesting from distant sites: Concepts and techniques. Oral Maxillofac Surg Clin North Am 2010, 22, 301–316. [Google Scholar] [CrossRef] [PubMed]
- Eufinger, H.; Leppänen, H. Iliac crest donor site morbidity following open and closed methods of bone harvest for alveolar cleft osteoplasty. J Craniomaxillofac Surg 2000, 28, 31–38. [Google Scholar] [CrossRef]
- Herford, A.S.; Dean, J.S. Complications in bone grafting. Oral Maxillofac Surg Clin North Am 2011, 23, 433–442. [Google Scholar] [CrossRef] [PubMed]
- Ahlmann, E.; Patzakis, M.; Roidis, N.; Shepherd, L.; Holtom, P. Comparison of anterior and posterior iliac crest bone grafts in terms of harvest-site morbidity and functional outcomes. J Bone Joint Surg Am 2002, 84-A, 716–720. [Google Scholar] [CrossRef]
- Farrow, A.; Morrison, R.; Pickersgill, T.; Currie, R.; Hammersley, N. Transient femoral neuropathy after harvest of bone from the iliac crest. Br J Oral Maxillofac Surg 2004, 42, 572–574. [Google Scholar] [CrossRef]
- Kargel, J.; Dimas, V.; Tanaka, W.; et al. Femoral nerve palsy as a complication of anterior iliac crest bone harvest: Report of two cases and review of the literature. Can J Plast Surg 2006, 14, 239–242. [Google Scholar] [CrossRef] [PubMed]
- Chou, A.S.-B.; Hung, C.-F.; Tseng, J.H.; Pan, K.T.; Yen, P.S. Pseudoaneurysm of the deep circumflex iliac artery: A rare complication at an anterior iliac bone graft donor site treated by coil embolization. Chang Gung Med J 2002, 25, 480–484. [Google Scholar] [PubMed]
- De Riu, G.; Meloni, S.M.; Raho, M.T.; Gobbi, R.; Tullio, A. Delayed iliac abscess as an unusual complication of an iliac bone graft in an orthognathic case. Int J Oral Maxillofac Surg 2008, 37, 1156–1158. [Google Scholar] [CrossRef] [PubMed]
- Nodarian, T.; Sariali, E.; Khiami, F.; Pascal-Mousselard, H.; Catonné, Y. Iliac crest bone graft harvesting complications: A case of liver herniation. Orthop Traumatol Surg Res 2010, 96, 593–596. [Google Scholar] [CrossRef] [PubMed]










| Complications | Number of patients | Percentage |
|---|---|---|
| Bleeding | 0 | 0 |
| Permanent nerve damage | 0 | 0 |
| Seroma | 1 | 0.269 |
| Gait disturbance | 0 | 0 |
| Fractures | 2 | 0.538 |
| Infection | 0 | 0 |
| Major subcutaneous hematoma | 1 | 0.269 |
| Temporary nerve damage | 3 | 0.806 |
| Ileus | 0 | 0 |
| Pain | 372 | 100 |
© 2013 by the author. The Author(s) 2013.
Share and Cite
Almaiman, M.; Al-Bargi, H.H.; Manson, P. Complication of Anterior Iliac Bone Graft Harvesting in 372 Adult Patients from May 2006 to May 2011 and a Literature Review. Craniomaxillofac. Trauma Reconstr. 2013, 6, 257-265. https://doi.org/10.1055/s-0033-1357510
Almaiman M, Al-Bargi HH, Manson P. Complication of Anterior Iliac Bone Graft Harvesting in 372 Adult Patients from May 2006 to May 2011 and a Literature Review. Craniomaxillofacial Trauma & Reconstruction. 2013; 6(4):257-265. https://doi.org/10.1055/s-0033-1357510
Chicago/Turabian StyleAlmaiman, Manar, Hamed H. Al-Bargi, and Paul Manson. 2013. "Complication of Anterior Iliac Bone Graft Harvesting in 372 Adult Patients from May 2006 to May 2011 and a Literature Review" Craniomaxillofacial Trauma & Reconstruction 6, no. 4: 257-265. https://doi.org/10.1055/s-0033-1357510
APA StyleAlmaiman, M., Al-Bargi, H. H., & Manson, P. (2013). Complication of Anterior Iliac Bone Graft Harvesting in 372 Adult Patients from May 2006 to May 2011 and a Literature Review. Craniomaxillofacial Trauma & Reconstruction, 6(4), 257-265. https://doi.org/10.1055/s-0033-1357510



