Branching Pattern of the Extraosseous Mental Nerve in a Kenyan Population
Abstract
:Materials and Methods
Results
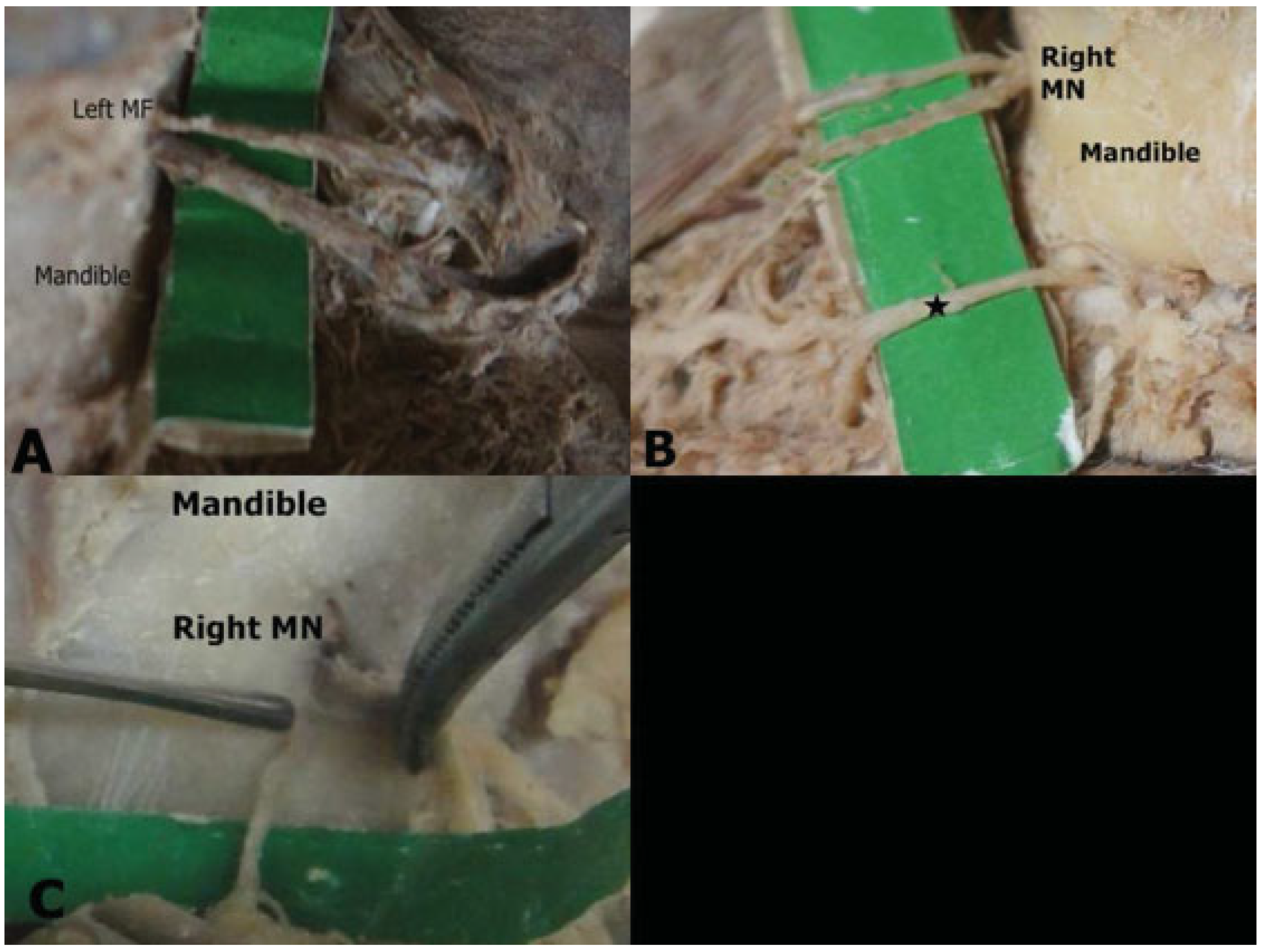
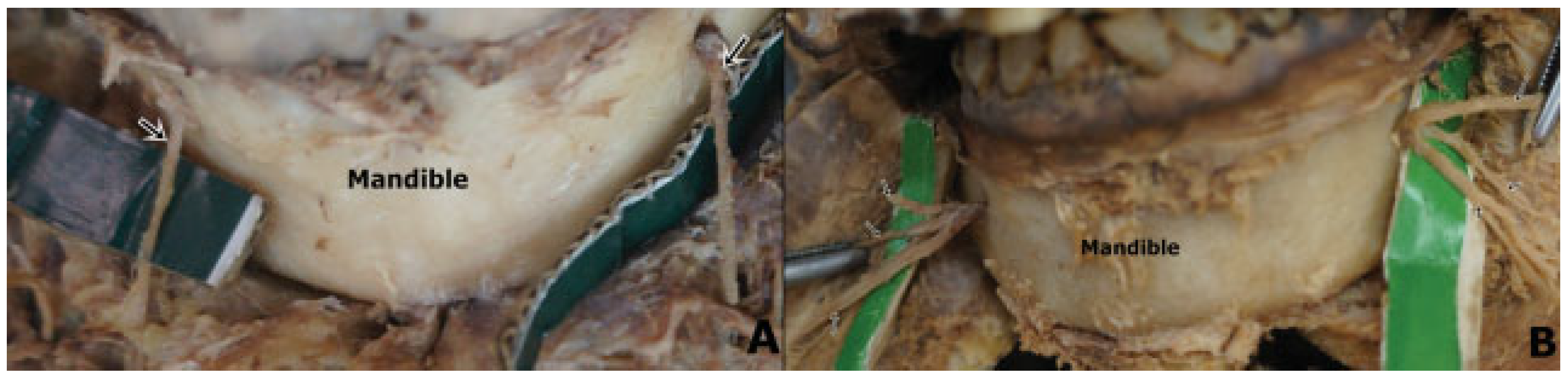
Initial Branching Pattern
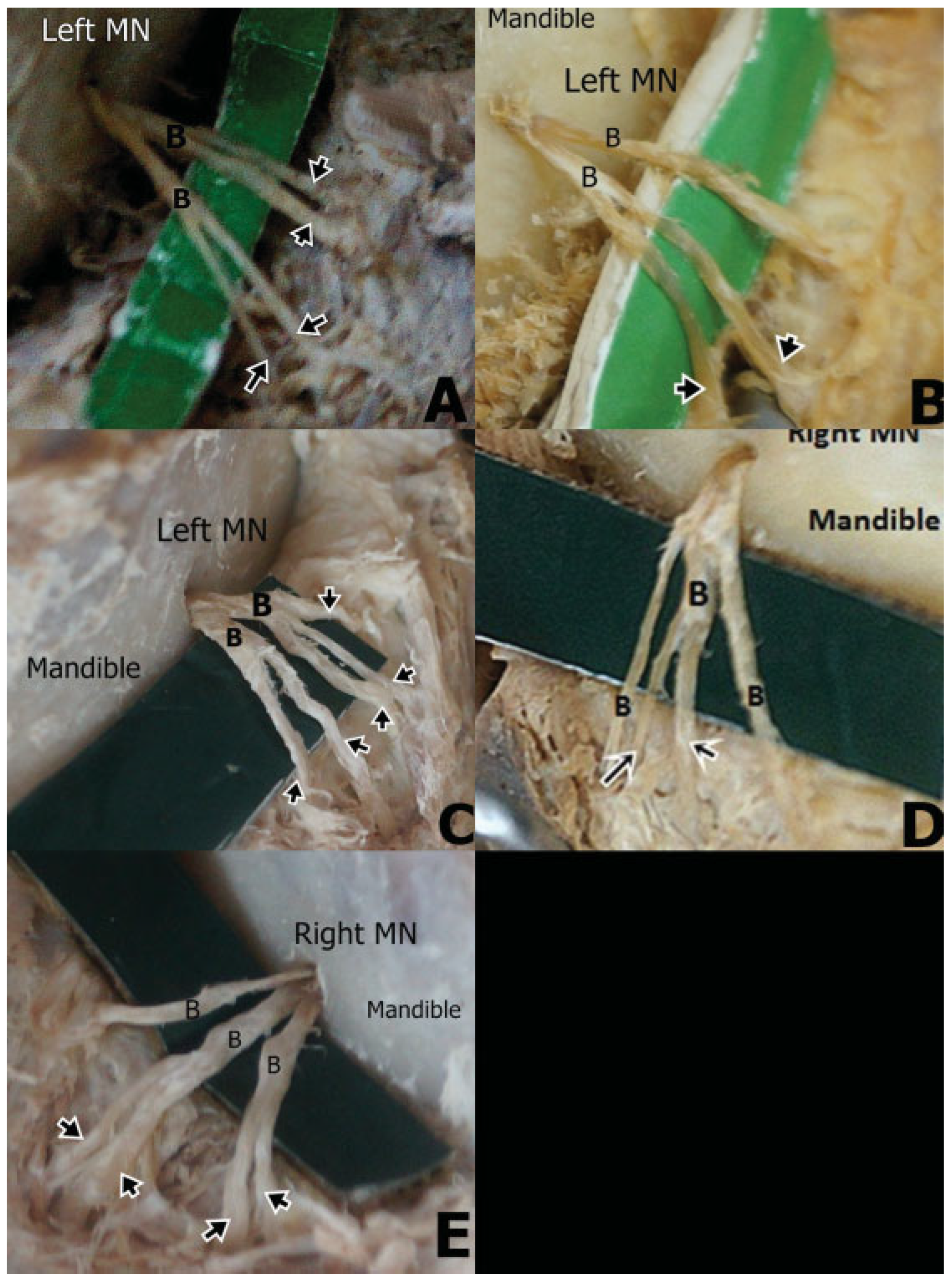
Terminal Branching Pattern
Symmetry
Discussion
Conclusion
References
- Oguz, O.; Bozkir, M.G. Evaluation of location of mandibular and mental foramina in dry, young, adult human male, dentulous mandibles. West Indian Med J 2002, 51, 14–16. [Google Scholar] [PubMed]
- Standring, S.; Berkovitz, K.B. (Eds.) Surface anatomy of the head and neck. In Gray’s Anatomy, 39th ed.; Elsevier: Churchill Livingstone, PA, USA, 2005; pp. 441–442. [Google Scholar]
- Mbajiorgu, E.F.; Mawera, G.; Asala, S.A.; Zivanovic, S. Position of the mental foramen in adult black Zimbabwean mandibles: A clinical anatomical study. Cent Afr J Med 1998, 44, 24–30. [Google Scholar] [PubMed]
- Naitoh, M.; Hiraiwa, Y.; Aimiya, H.; Gotoh, K.; Ariji, E. Accessory mental foramen assessment using cone-beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009, 107, 289–294. [Google Scholar] [CrossRef] [PubMed]
- Balcioglu, H.A.; Kocaelli, H. Accessory mental foramen. N Am J Med Sci 2009, 1, 314–315. [Google Scholar]
- Sahin, B.; Ozkan, H.S.; Gorgu, M. An anatomical variation of mental nerve and foramen in a trauma patient. IJAV 2010, 3, 165–166. [Google Scholar]
- Ramadhan, A.; Messo, E.; Hirsch, J.M. Anatomical variation of mental foramen. A case report. Stomatologija 2010, 12, 93–96. [Google Scholar]
- Kieser, J.; Kuzmanovic, D.; Payne, A.; Dennison, J.; Herbison, P. Patterns of emergence of the human mental nerve. Arch Oral Biol 2002, 47, 743–747. [Google Scholar] [CrossRef]
- Fabian, F.M. Position, shape and direction of opening of the mental foramen in dry mandibles of Tanzanian adult black males. Ital J Anat Embryol 2007, 112, 169–177. [Google Scholar]
- Hu, K.S.; Yun, H.S.; Hur, M.S.; Kwon, H.J.; Abe, S.; Kim, H.J. Branching patterns and intraosseous course of the mental nerve. J Oral Maxillofac Surg 2007, 65, 2288–2294. [Google Scholar] [CrossRef]
- Odero, W.; Garner, P.; Zwi, A. Road traffic injuries in developing countries: A comprehensive review of epidemiological studies. Trop Med Int Health 1997, 2, 445–460. [Google Scholar] [CrossRef]
- Greenstein, G.; Tarnow, D. The mental foramen and nerve: Clinical and anatomical factors related to dental implant placement: A literature review. J Periodontol 2006, 77, 1933–1943. [Google Scholar] [CrossRef] [PubMed]
- Hasan, T.; Mahmood, F.; Hasan, D. Bilateral absence of mental foramen a rare variation. IJAV 2010, 3, 167–169. [Google Scholar]
- Katakami, K.; Mishima, A.; Shiozaki, K.; Shimoda, S.; Hamada, Y.; Kobayashi, K. Characteristics of accessory mental foramina ob- served on limited cone-beam computed tomography images. J Endod 2008, 34, 1441–1445. [Google Scholar] [CrossRef] [PubMed]
- Boronat López, A.; Peñarrocha Diago, M. Failure of locoregional anesthesia in dental practice. Review of the literature. Med Oral Patol Oral Cir Bucal 2006, 11, E510–E513. [Google Scholar]
- Montagu, M.F.A. The direction and position of the mental foramen in the great apes and man. Am J Phys Anthropol 1954, 12, 503–518. [Google Scholar] [CrossRef] [PubMed]
- Riesenfeld, A. Multiple infraorbital, ethmoidal, and mental forami- na in the races of man. Am J Phys Anthropol 1956, 14, 85–100. [Google Scholar] [CrossRef]
- Sawyer, D.R.; Kiely, M.L.; Pyle, M.A. The frequency of accessory mental foramina in four ethnic groups. Arch Oral Biol 1998, 43, 417–420. [Google Scholar] [CrossRef]
- Alantar, A.; Roche, Y.; Maman, L.; Carpentier, P. The lower labial branches of the mental nerve: Anatomic variations and surgical relevance. J Oral Maxillofac Surg 2000, 58, 415–418. [Google Scholar] [CrossRef]
- Alsaad, K.; Lee, T.C.; McCartan, B. An anatomical study of the cutane- ous branches of the mental nerve. Int J Oral Maxillofac Surg 2003, 32, 325–333. [Google Scholar] [CrossRef]
- Jha, A.K.; Kumar, N.G. Accessory mental nerve: Case report, review and its role in trigeminal neuralgia. Surg Radiol Anat 2012, 34, 469–473. [Google Scholar] [CrossRef]
- Hwang, K.; Lee, W.J.; Song, Y.B.; Chung, I.H. Vulnerability of the inferior alveolar nerve and mental nerve during genioplasty: An anatomic study. J Craniofac Surg 2005, 16, 10–14, discussion 14. [Google Scholar] [CrossRef] [PubMed]
- Babbush, C.A. Transpositioning and repositioning the inferior alve- olar and mental nerves in conjunction with endosteal implant reconstruction. Periodontol 2000 1998, 17, 183–190. [Google Scholar] [CrossRef] [PubMed]
- Agthong, S.; Huanmanop, T.; Chentanez, V. Anatomical variation of the supraorbital, infraorbital, and mental foramina related to gender and side. J Oral Maxillofac Surg 2005, 63, 800–804. [Google Scholar] [CrossRef] [PubMed]
- Zografos, J.; Mutzuri, A. Incidence of double mental foramen in a sample of Greek population. Odontostomatol Proodos 1989, 43, 521–523. [Google Scholar]
- Sankar, D.K.; Bhanu, S.P.; Susan, P.J. Morphometrical and morphologi- cal study of mental foramen in dry dentulous mandibles of South Andhra population of India. IJDR 2011, 22, 542–546. [Google Scholar]

| Study (n) | Study population | Method | Prevalence (%) |
|---|---|---|---|
| Current study (64) | Kenyan | Cadaveric | 4.7 |
| Zografos and Mutzuri (800) [25] | Greek | Osteological | 6.68 |
| Agthong et al. (110) [24] | Thai | Osteological | 1.8 |
| Naitoh et al. 2009 (157) [4] | Japanese | Osteological | 7 |
| Sankar et al. 2011 [26] (90) | Indian | Osteological | 8.9 |
| Study (n) | Study Population | Method | Prevalence (%) |
|---|---|---|---|
| Current study (64) | Kenyan | Cadaveric | 1.6 |
| Montagu 1954 [16] (800) | French | Osteological | 2.6 |
| Montagu 1954 [16] (2400) | Russian | Osteological | 1.5 |
| Riesenfeld 1956 [17] (430) | Polynesian | Osteological | 12.5 |
| Riesenfeld 1956 [17] (484) | Melanesian | Osteological | 9.7 |
| Naitoh et al., 2009 [4] (157) | Japanese | Cone-beam computed tomography | 7 |
| Sawyer et al., 1998 [18] (510) | White American | Osteological | 1.4 |
| Sawyer et al., 1998 [18] (332) | Black American | Osteological | 5.7 |
| Study (n) | Population | Number of branches | |||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | ||
| Current study, 2012 (64) | Kenyan | 19 | 39 | 34 | 8 |
| Hu et al., 2007 [10] (62) | Korean | – | 38.8 | 61.3 | – |
| Alsaad et al. 2003 [20] (26) | Ireland | – | 44.4 | 55.6 | – |
| Alantar et al. 2000 [19] (32) | French | 22 | 28 | 28 | 22 |
© 2013 by the author. The Author(s) 2013.
Share and Cite
Loyal, P.K.; Butt, F.; Ogeng'o, J.A. Branching Pattern of the Extraosseous Mental Nerve in a Kenyan Population. Craniomaxillofac. Trauma Reconstr. 2013, 6, 251-256. https://doi.org/10.1055/s-0033-1356756
Loyal PK, Butt F, Ogeng'o JA. Branching Pattern of the Extraosseous Mental Nerve in a Kenyan Population. Craniomaxillofacial Trauma & Reconstruction. 2013; 6(4):251-256. https://doi.org/10.1055/s-0033-1356756
Chicago/Turabian StyleLoyal, Poonamjeet Kaur, Fawzia Butt, and Julius Alexander Ogeng'o. 2013. "Branching Pattern of the Extraosseous Mental Nerve in a Kenyan Population" Craniomaxillofacial Trauma & Reconstruction 6, no. 4: 251-256. https://doi.org/10.1055/s-0033-1356756
APA StyleLoyal, P. K., Butt, F., & Ogeng'o, J. A. (2013). Branching Pattern of the Extraosseous Mental Nerve in a Kenyan Population. Craniomaxillofacial Trauma & Reconstruction, 6(4), 251-256. https://doi.org/10.1055/s-0033-1356756



