Pathologic Fractures in Bisphosphonate-Related Osteonecrosis of the Jaw—Review of the Literature and Review of Our Own Cases
Abstract
:Bisphosphonate-Related Osteonecrosis of Jaw
Occurrence and Incidence of the Disease
Diagnosis
Clinical Features
Risk Factors
Pathogenesis
BRONJ Therapy
Occurrence and Treatment of Pathologic Fractures Due to BRONJ
Conclusion
References
- Green, J.R. Antitumor effects of bisphosphonates. Cancer 2003, 97 (Suppl. 3), 840–847. [Google Scholar] [PubMed]
- Sambrook, P.; Cooper, C. Osteoporosis. Lancet 2006, 367, 2010–2018. [Google Scholar] [PubMed]
- Yarom, N.; Yahalom, R.; Shoshani, Y.; Hamed, W.; Regev, E.; Elad, S. Osteonecrosis of the jaw induced by orally administered bisphosphonates: incidence, clinical features, predisposing factors and treatment outcome. Osteoporos Int 2007, 18, 1363–1370. [Google Scholar] [PubMed]
- Berenson, J.R.; Lichtenstein, A.; Porter, L.; Myeloma Aredia Study Group; et al. Efficacy of pamidronate in reducing skeletal events in patients with advanced multiple myeloma. N Engl J Med 1996, 334, 488–493. [Google Scholar] [CrossRef]
- Cranney, A.; Tugwell, P.; Adachi, J.; Osteoporosis Methodology Group and The Osteoporosis Research Advisory Group; et al. Metaanalyses of therapies for postmenopausal osteoporosis. III. Meta-analysis of risedronate for the treatment of postmenopausal osteoporosis. Endocr Rev 2002, 23, 517–523. [Google Scholar]
- Black, D.M.; Cummings, S.R.; Karpf, D.B.; Fracture Intervention Trial Research Group; et al. Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Lancet 1996, 348, 1535–1541. [Google Scholar]
- Mehrotra, B. Safety profile of intravenous bisphosphonates. Semin Oncol 2007, 34 (Suppl. 4), S24–S27. [Google Scholar]
- Migliorati, C.A. Bisphosphanates and oral cavity avascular bone necrosis. J Clin Oncol 2003, 21, 4253–4254. [Google Scholar] [CrossRef]
- Marx, R.E. Pamidronate (Aredia) and zoledronate (Zometa) induced avascular necrosis of the jaws: a growing epidemic. J Oral Maxillofac Surg 2003, 61, 1115–1117. [Google Scholar] [CrossRef]
- Wang, J.; Goodger, N.M.; Pogrel, M.A. Osteonecrosis of the jaws associated with cancer chemotherapy. J Oral Maxillofac Surg 2003, 61, 1104–1107. [Google Scholar]
- Walter, C.; Al-Nawas, B.; Grötz, K.A.; et al. Prevalence and risk factors of bisphosphonate-associated osteonecrosis of the jaw in prostate cancer patients with advanced disease treated with zoledronate. Eur Urol 2008, 54, 1066–1072. [Google Scholar]
- Bamias, A.; Kastritis, E.; Bamia, C.; et al. Osteonecrosis of the jaw in cancer after treatment with bisphosphonates: incidence and risk factors. J Clin Oncol 2005, 23, 8580–8587. [Google Scholar] [CrossRef] [PubMed]
- Vahtsevanos, K.; Kyrgidis, A.; Verrou, E.; et al. Longitudinal cohort study of risk factors in cancer patients of bisphosphonate-related osteonecrosis of the jaw. J Clin Oncol 2009, 27, 5356–5362. [Google Scholar] [CrossRef]
- Boonyapakorn, T.; Schirmer, I.; Reichart, P.A.; Sturm, I.; Massenkeil, G. Bisphosphonate-induced osteonecrosis of the jaws: prospective study of 80 patients with multiple myeloma and other malignancies. Oral Oncol 2008, 44, 857–869. [Google Scholar] [PubMed]
- Lo, J.C.; O’Ryan, F.S.; Gordon, N.P.; Predicting Risk of Osteonecrosis of the Jaw with Oral Bisphosphonate Exposure (PROBE) Investigators; et al. Prevalence of osteonecrosis of the jaw in patients with oral bisphosphonate exposure. J Oral Maxillofac Surg 2010, 68, 243–253. [Google Scholar] [CrossRef]
- Advisory Task Force on Bisphosphonate-Related Ostenonecrosis of the Jaws, American Association of Oral and Maxillofacial Surgeons. American Association of Oral and Maxillofacial Surgeons position paper on bisphosphonate-related osteonecrosis of the jaws. J Oral Maxillofac Surg 2007, 65, 369–376. [Google Scholar] [CrossRef] [PubMed]
- Ruggiero, S.L.; Dodson, T.B.; Assael, L.A.; Landesberg, R.; Marx, R.E.; Mehrotra, B. ; American Association of Oral and Maxillofacial Surgeons. American Association of Oral and Maxillofacial Surgeons position paper on bisphosphonate-related osteonecrosis of the jaws—2009 update. J Oral Maxillofac Surg 2009, 67 (Suppl. 5), 2–12. [Google Scholar]
- Khosla, S.; Burr, D.; Cauley, J.; American Society for Bone and Mineral Research; et al. Bisphosphonate-associated osteonecrosis of the jaw: report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res 2007, 22, 1479–1491. [Google Scholar]
- Abu-Id, M.H.; Açil, Y.; Gottschalk, J.; Kreusch, T. [Bisphosphonate-associated osteonecrosis of the jaw]. Mund Kiefer Gesichtschir 2006, 10, 73–81. [Google Scholar]
- Abu-Id, M.H.; Warnke, P.H.; Gottschalk, J.; et al. “Bis-phossy jaws”—high and low risk factors for bisphosphonate-induced osteonecrosis of the jaw. J Craniomaxillofac Surg 2008, 36, 95–103. [Google Scholar]
- Otto, S.; Hafner, S.; Grötz, K.A. The role of inferior alveolar nerve involvement in bisphosphonate-related osteonecrosis of the jaw. J Oral Maxillofac Surg 2009, 67, 589–592. [Google Scholar] [PubMed]
- Wongchuensoontorn, C.; Liebehenschel, N.; Wagner, K.; et al. Pathological fractures in patients caused by bisphosphonate-related osteonecrosis of the jaws: report of 3 cases. J Oral Maxillofac Surg 2009, 67, 1311–1316. [Google Scholar]
- Wang, E.P.; Kaban, L.B.; Strewler, G.J.; Raje, N.; Troulis, M.J. Incidence of osteonecrosis of the jaw in patients with multiple myeloma and breast or prostate cancer on intravenous bisphosphonate therapy. J Oral Maxillofac Surg 2007, 65, 1328–1331. [Google Scholar] [PubMed]
- Dimopoulos, M.A.; Kastritis, E.; Anagnostopoulos, A.; et al. Osteonecrosis of the jaw in patients with multiple myeloma treated with bisphosphonates: evidence of increased risk after treatment with zoledronic acid. Haematologica 2006, 91, 968–971. [Google Scholar]
- Marx, R.E.; Cillo, J.E., Jr.; Ulloa, J.J. Oral bisphosphonate-induced osteonecrosis: risk factors, prediction of risk using serum CTX testing, prevention, and treatment. J Oral Maxillofac Surg 2007, 65, 2397–2410. [Google Scholar] [PubMed]
- Badros, A.; Weikel, D.; Salama, A.; et al. Osteonecrosis of the jaw in multiple myeloma patients: clinical features and risk factors. J Clin Oncol 2006, 24, 945–952. [Google Scholar]
- Diel, I.J.; Fogelman, I.; Al-Nawas, B.; et al. Pathophysiology, risk factors and management of bisphosphonate-associated osteonecrosis of the jaw: Is there a diverse relationship of aminoand non-aminobisphosphonates? Crit Rev Oncol Hematol 2007, 64, 198–207. [Google Scholar]
- Hoff, A.O.; Toth, B.B.; Altundag, K.; et al. Frequency and risk factors associated with osteonecrosis of the jaw in cancer patients treated with intravenous bisphosphonates. J Bone Miner Res 2008, 23, 826–836. [Google Scholar]
- Hess, L.M.; Jeter, J.M.; Benham-Hutchins, M.; Alberts, D.S. Factors associated with osteonecrosis of the jaw among bisphosphonate users. Am J Med 2008, 121, 475–483.e3. [Google Scholar]
- Allen, M.R.; Burr, D.B. The pathogenesis of bisphosphonate-related osteonecrosis of the jaw: so many hypotheses, so few data. J Oral Maxillofac Surg 2009, 67 (Suppl. 5), 61–70. [Google Scholar]
- Allen, M.R. Bisphosphonates and osteonecrosis of the jaw: moving from the bedside to the bench. Cells Tissues Organs 2009, 189, 289–294. [Google Scholar] [PubMed]
- Rodan, G.A.; Fleisch, H.A. Bisphosphonates: mechanisms of action. J Clin Invest 1996, 97, 2692–2696. [Google Scholar] [PubMed]
- Scavelli, C.; Di Pietro, G.; Cirulli, T.; et al. Zoledronic acid affects overangiogenic phenotype of endothelial cells in patients with multiple myeloma. Mol Cancer Ther 2007, 6 Pt 1, 3256–3262. [Google Scholar] [PubMed]
- Hansen, T.; Kunkel, M.; Weber, A.; James Kirkpatrick, C. Osteonecrosis of the jaws in patients treated with bisphosphonates—histomorphologic analysis in comparison with infected osteoradionecrosis. J Oral Pathol Med 2006, 35, 155–160. [Google Scholar]
- Reid, I.R.; Bolland, M.J.; Grey, A.B. Is bisphosphonate-associated osteonecrosis of the jaw caused by soft tissue toxicity? Bone 2007, 41, 318–320. [Google Scholar]
- Otto, S.; Hafner, S.; Mast, G.; et al. Bisphosphonate-related osteonecrosis of the jaw: is pH the missing part in the pathogenesis puzzle? J Oral Maxillofac Surg 2010, 68, 1158–1161. [Google Scholar]
- Russell, R.G.; Watts, N.B.; Ebetino, F.H.; Rogers, M.J. Mechanisms of action of bisphosphonates: similarities and differences and their potential influence on clinical efficacy. Osteoporos Int 2008, 19, 733–759. [Google Scholar]
- Sato, M.; Grasser, W.; Endo, N.; et al. Bisphosphonate action. Alendronate localization in rat bone and effects on osteoclast ultrastructure. J Clin Invest 1991, 88, 2095–2105. [Google Scholar]
- Otto, S.; Pautke, C.; Opelz, C.; et al. Osteonecrosis of the jaw: effect of bisphosphonate type, local concentration, and acidic milieu on the pathomechanism. J Oral Maxillofac Surg 2010, 68, 2837–2845. [Google Scholar]
- Agis, H.; Blei, J.; Watzek, G.; Gruber, R. Is zoledronate toxic to human periodontal fibroblasts? J Dent Res 2010, 89, 40–45. [Google Scholar]
- Nancollas, G.H.; Tang, R.; Phipps, R.J.; et al. Novel insights into actions of bisphosphonates on bone: differences in interactions with hydroxyapatite. Bone 2006, 38, 617–627. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, T.; John, M.; Kerschbaum, T.; MIcheels, W.; Potthoff, P.; Reich, E.; Reis, U.; Reiter, F.; Schiffner, U.; Schroeder, E. Oral epidemiology. In Institute of German Dentists: Fourth German Oral Health Study (DMS IV); Micheelis, W., Schiffner, U., Eds.; Deutscher Zahnärzte Verlag DÄV: Cologne, Germany, 2006. [Google Scholar]
- Ruggiero, S.L.; Fantasia, J.; Carlson, E. Bisphosphonate-related osteonecrosis of the jaw: background and guidelines for diagnosis, staging and management. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006, 102, 433–441. [Google Scholar] [CrossRef]
- Montebugnoli, L.; Felicetti, L.; Gissi, D.B.; Pizzigallo, A.; Pelliccioni, G.A.; Marchetti, C. Biphosphonate-associated osteonecrosis can be controlled by nonsurgical management. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007, 104, 473–477. [Google Scholar] [CrossRef] [PubMed]
- Badros, A.; Terpos, E.; Katodritou, E.; et al. Natural history of osteonecrosis of the jaw in patients with multiple myeloma. J Clin Oncol 2008, 26, 5904–5909. [Google Scholar] [CrossRef]
- Van den Wyngaert, T.; Claeys, T.; Huizing, M.T.; Vermorken, J.B.; Fossion, E. Initial experience with conservative treatment in cancer patients with osteonecrosis of the jaw (ONJ) and predictors of outcome. Ann Oncol 2009, 20, 331–336. [Google Scholar] [CrossRef] [PubMed]
- Stanton, D.C.; Balasanian, E. Outcome of surgical management of bisphosphonate-related osteonecrosis of the jaws: review of 33 surgical cases. J Oral Maxillofac Surg 2009, 67, 943–950. [Google Scholar] [CrossRef]
- Pautke, C.; Bauer, F.; Otto, S.; et al. Fluorescence-guided bone resection in bisphosphonate-related osteonecrosis of the jaws: first clinical results of a prospective pilot study. J Oral Maxillofac Surg 2011, 69, 84–91. [Google Scholar] [CrossRef]
- Markose, G.; Mackenzie, F.R.; Currie, W.J.; Hislop, W.S. Bisphosphonate osteonecrosis: a protocol for surgical management. Br J Oral Maxillofac Surg 2009, 47, 294–297. [Google Scholar] [CrossRef]
- Carlson, E.R.; Basile, J.D. The role of surgical resection in the management of bisphosphonate-related osteonecrosis of the jaws. J Oral Maxillofac Surg 2009, 67 (Suppl. 5), 85–95. [Google Scholar] [CrossRef]
- Vescovi, P.; Manfredi, M.; Merigo, E.; Meleti, M. Early surgical approach preferable to medical therapy for bisphosphonate-related osteonecrosis of the jaws. J Oral Maxillofac Surg 2008, 66, 831–832. [Google Scholar] [CrossRef]
- Pautke, C.; Bauer, F.; Bissinger, O.; et al. Tetracycline bone fluorescence: a valuable marker for the osteonecrosis characterization and therapy. J Oral Maxillofac Surg 2010, 68, 125–129. [Google Scholar] [CrossRef] [PubMed]
- Pautke, C.; Bauer, F.; Tischer, T.; et al. Fluorescence-guided bone resection in bisphosphonate-associated osteonecrosis of the jaws. J Oral Maxillofac Surg 2009, 67, 471–476. [Google Scholar]
- Fleisher, K.E.; Doty, S.; Kottal, S.; Phelan, J.; Norman, R.G.; Glickman, R.S. Tetracycline-guided debridement and cone beam computed tomography for the treatment of bisphosphonate-related osteonecrosis of the jaw: a technical note. J Oral Maxillofac Surg 2008, 66, 2646–2653. [Google Scholar] [CrossRef]
- Abu-Id, M.H.; Warnke, P.H.; Gottschalk, J.; et al. “Bis-phossy jaws”—high and low risk factors for bisphosphonate-induced osteonecrosis of the jaw. J Craniomaxillofac Surg 2008, 36, 95–103. [Google Scholar] [PubMed]
- Marx, R.E. Reconstruction of defects caused by bisphosphonateinduced osteonecrosis of the jaws. J Oral Maxillofac Surg 2009, 67 (Suppl. 5), 107–119. [Google Scholar] [PubMed]
- Engroff, S.L.; Kim, D.D. Treating bisphosphonate osteonecrosis of the jaws: is there a role for resection and vascularized reconstruction? J Oral Maxillofac Surg 2007, 65, 2374–2385. [Google Scholar]
- Cornelius, C.P.; Augustin, J.B.; Sailer, L.K. External pin fixation for stabilization of the mandible—comeback of a method: historical review and first experiences with the ’mandible external fixator’. Oral Maxillofac Surg 2009, 13, 1–14. [Google Scholar]
- Mücke, T.; Haarmann, S.; Wolff, K.D.; Hölzle, F. Bisphosphonate related osteonecrosis of the jaws treated by surgical resection and immediate osseous microvascular reconstruction. J Craniomaxillofac Surg 2009, 37, 291–297. [Google Scholar]

| Patient | Age | Sex | Underlying Disease | Bisphosphonate | Localization of Fracture |
|---|---|---|---|---|---|
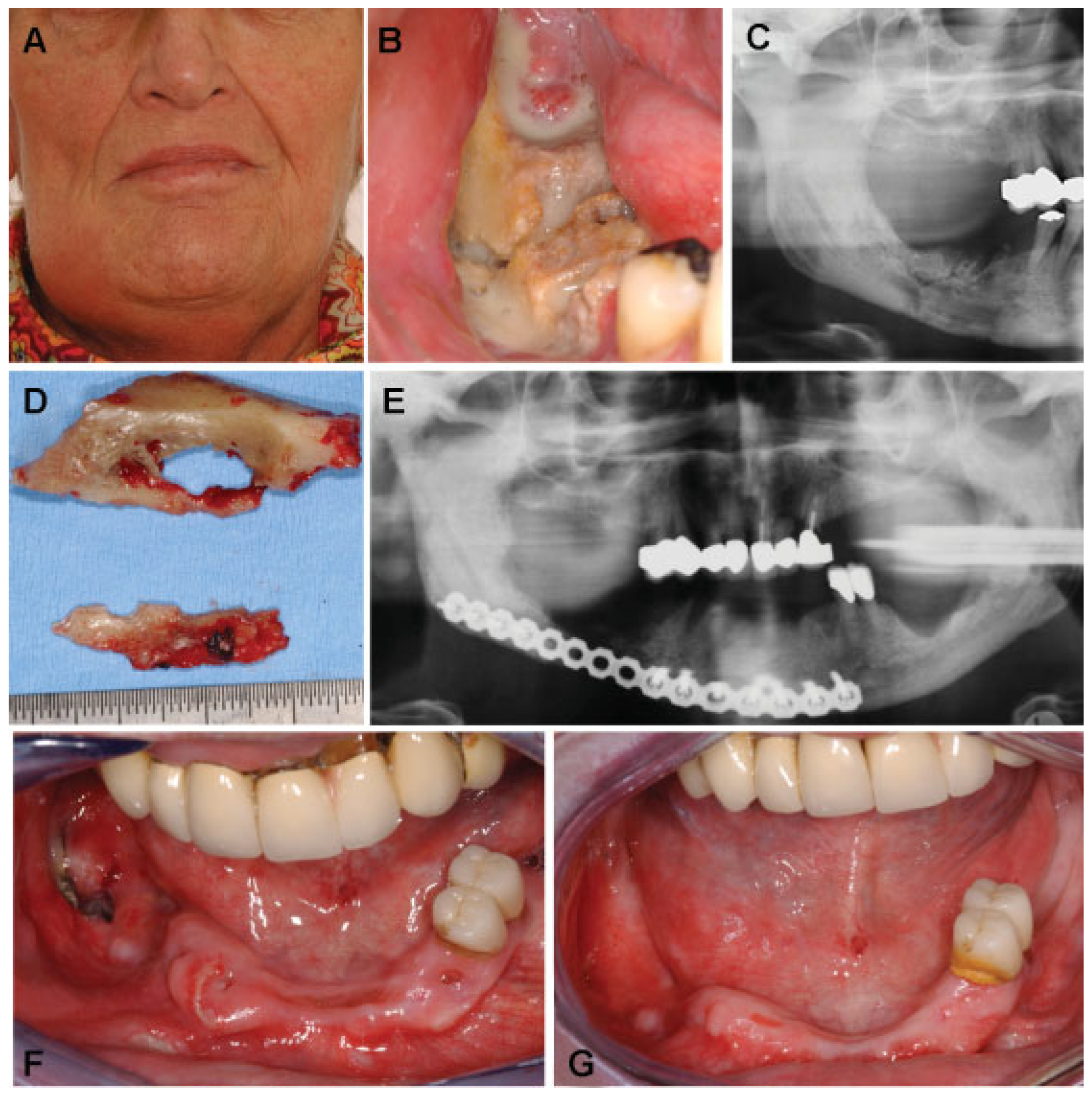
| 1 | 65 | F | Breast cancer | Zoledronate (i.v.) | Right mandibular body/angle |
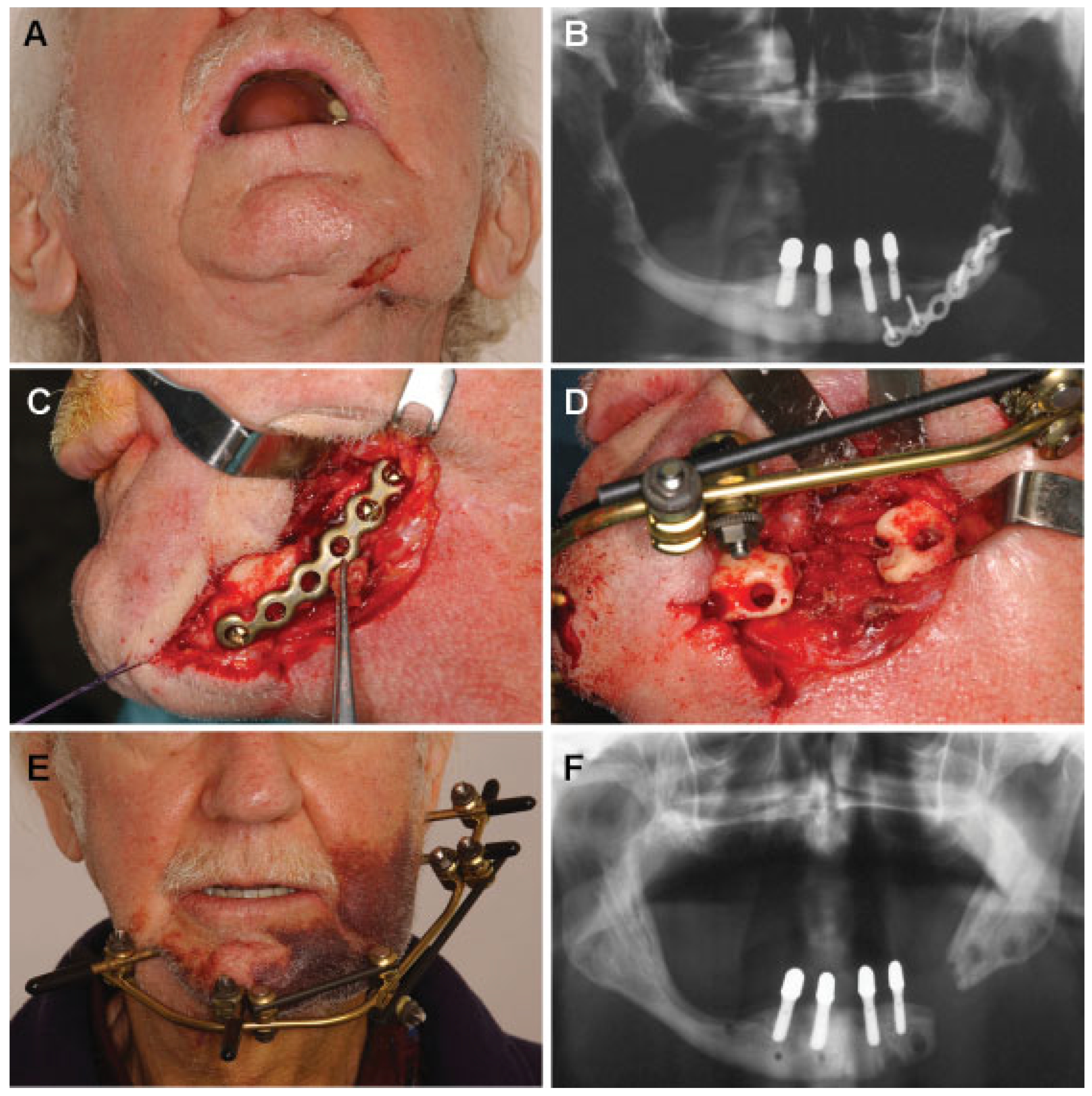
| 2 | 72 | M | Prostate cancer | Zoledronate (i.v.) | Left mandibular body |
| 3 | 91 | M | Prostate cancer | Zoledronate (i.v.) | Left mandibular angle |
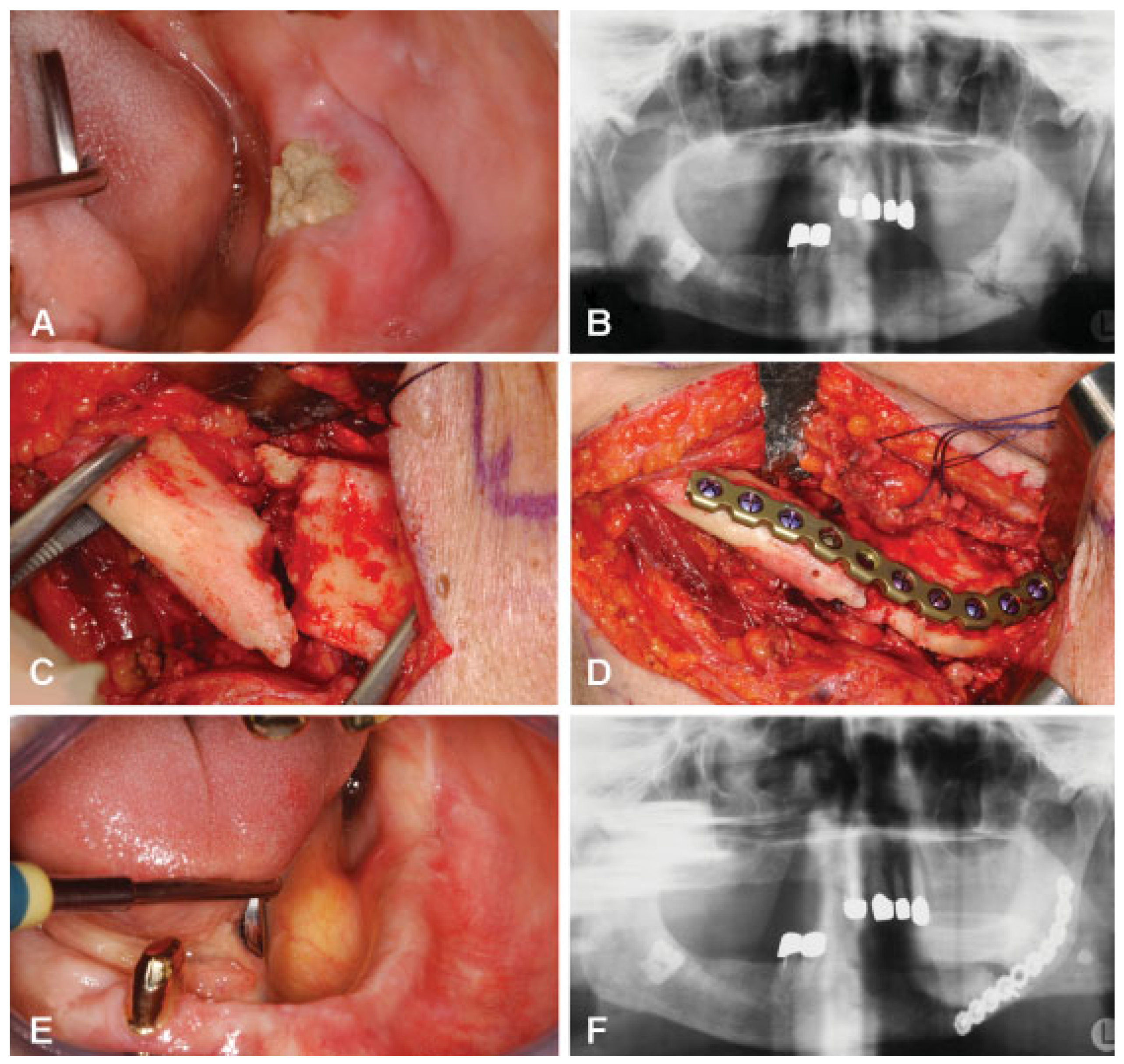
| 4 | 73 | F | Multiple myeloma | Zoledronate (i.v.) | Left mandibular body |
| Patient | Treatment | Outcome |
|---|---|---|
| 1 | Sequestrotomy and removal of necrotic bone parts including segmental resection, open reduction and rigid internal fixation (AO Titanium 2.4 unilock) (DePuy Synthes, Germany) | Delayed mucosal healing (initial wound dehiscence with complete mucosal healing after local disinfectant measurements) |
| 2 | Sequestrotomy and removal of necrotic bone parts and application of external fixation | Stable pseudarthrosis and mucosal healing |
| 3 | Sequestrotomy and removal of necrotic bone parts, open reduction and rigid internal fixation (AO titanium 2.4 unilock) | Delayed but complete mucosal healing |
| 4 | Sequestrotomy and removal of necrotic bone parts, open reduction and rigid internal fixation (Matrix mandible preformed plate) (DePuy Synthes, Germany) | Delayed mucosal healing with a small area of intraoral bone exposure (no plate exposure, no extraoral fistula) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2013 by the author. The Author(s) 2013.
Share and Cite
Otto, S.; Pautke, C.; Hafner, S.; Hesse, R.; Reichardt, L.F.; Mast, G.; Ehrenfeld, M.; Cornelius, C.-P. Pathologic Fractures in Bisphosphonate-Related Osteonecrosis of the Jaw—Review of the Literature and Review of Our Own Cases. Craniomaxillofac. Trauma Reconstr. 2013, 6, 147-154. https://doi.org/10.1055/s-0033-1343776
Otto S, Pautke C, Hafner S, Hesse R, Reichardt LF, Mast G, Ehrenfeld M, Cornelius C-P. Pathologic Fractures in Bisphosphonate-Related Osteonecrosis of the Jaw—Review of the Literature and Review of Our Own Cases. Craniomaxillofacial Trauma & Reconstruction. 2013; 6(3):147-154. https://doi.org/10.1055/s-0033-1343776
Chicago/Turabian StyleOtto, Sven, Christoph Pautke, Sigurd Hafner, Ronny Hesse, Lea Franziska Reichardt, Gerson Mast, Michael Ehrenfeld, and Carl-Peter Cornelius. 2013. "Pathologic Fractures in Bisphosphonate-Related Osteonecrosis of the Jaw—Review of the Literature and Review of Our Own Cases" Craniomaxillofacial Trauma & Reconstruction 6, no. 3: 147-154. https://doi.org/10.1055/s-0033-1343776
APA StyleOtto, S., Pautke, C., Hafner, S., Hesse, R., Reichardt, L. F., Mast, G., Ehrenfeld, M., & Cornelius, C.-P. (2013). Pathologic Fractures in Bisphosphonate-Related Osteonecrosis of the Jaw—Review of the Literature and Review of Our Own Cases. Craniomaxillofacial Trauma & Reconstruction, 6(3), 147-154. https://doi.org/10.1055/s-0033-1343776



