Frontal Sinus Fractures: A Conservative Shift
Abstract
:History
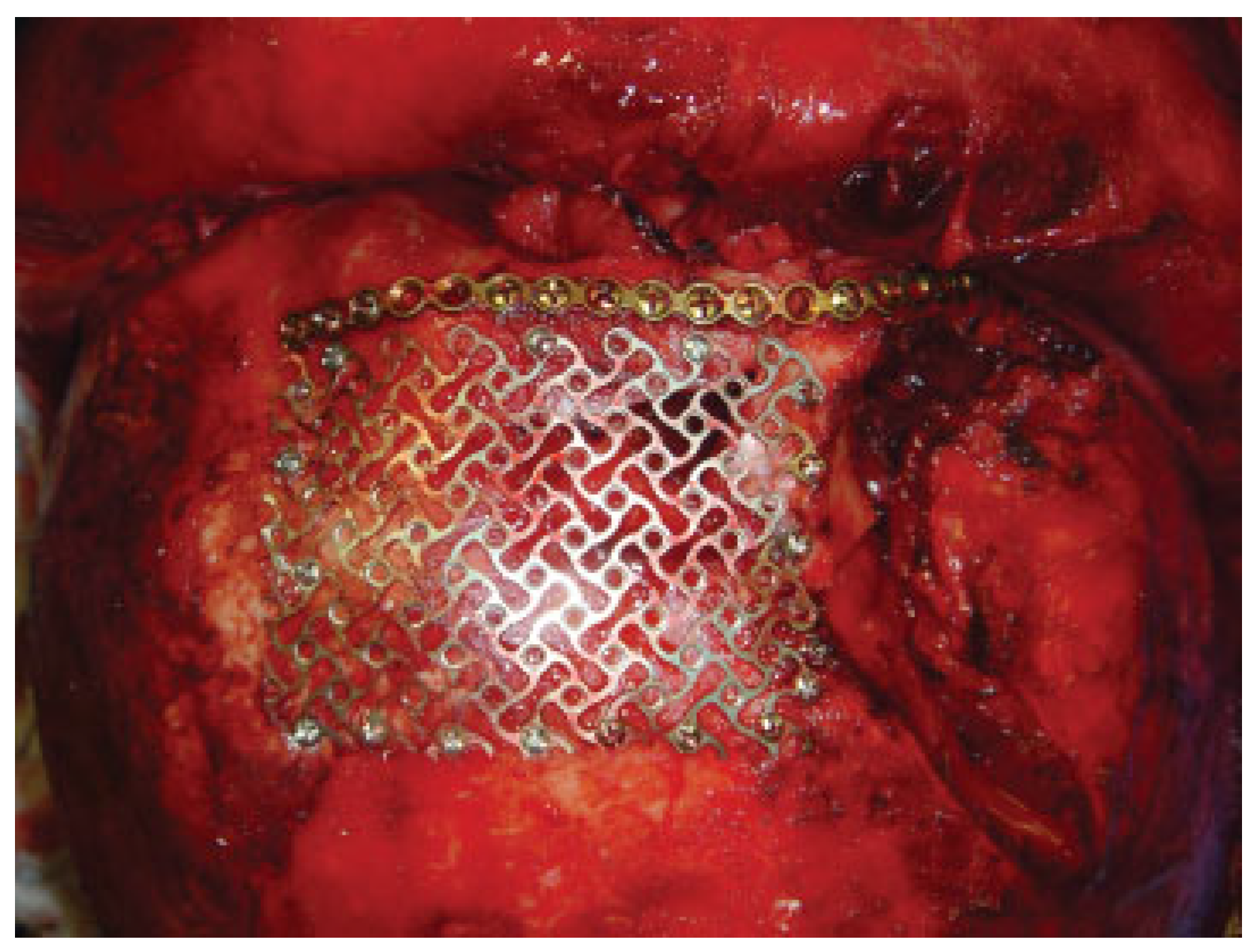
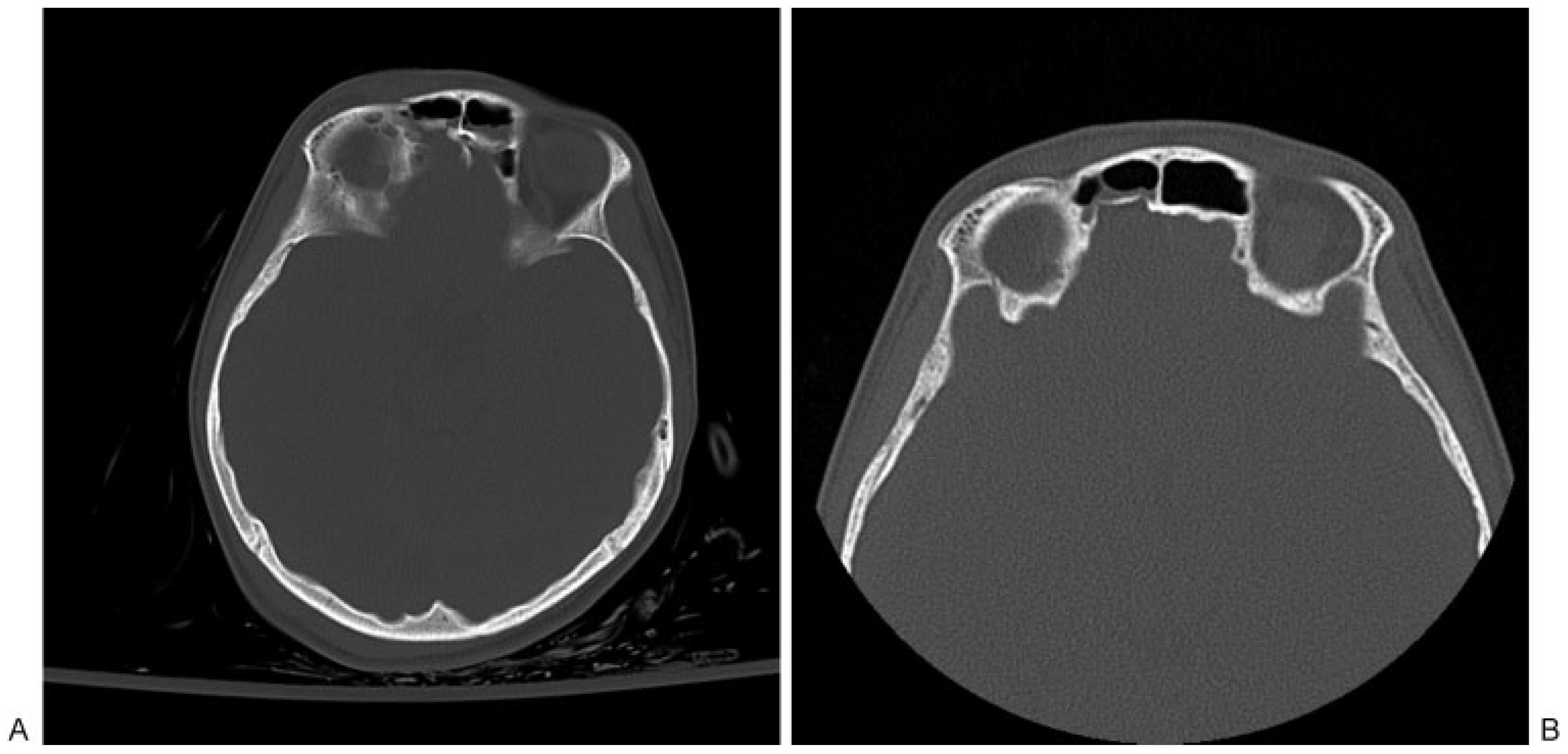
Anterior Table Fractures
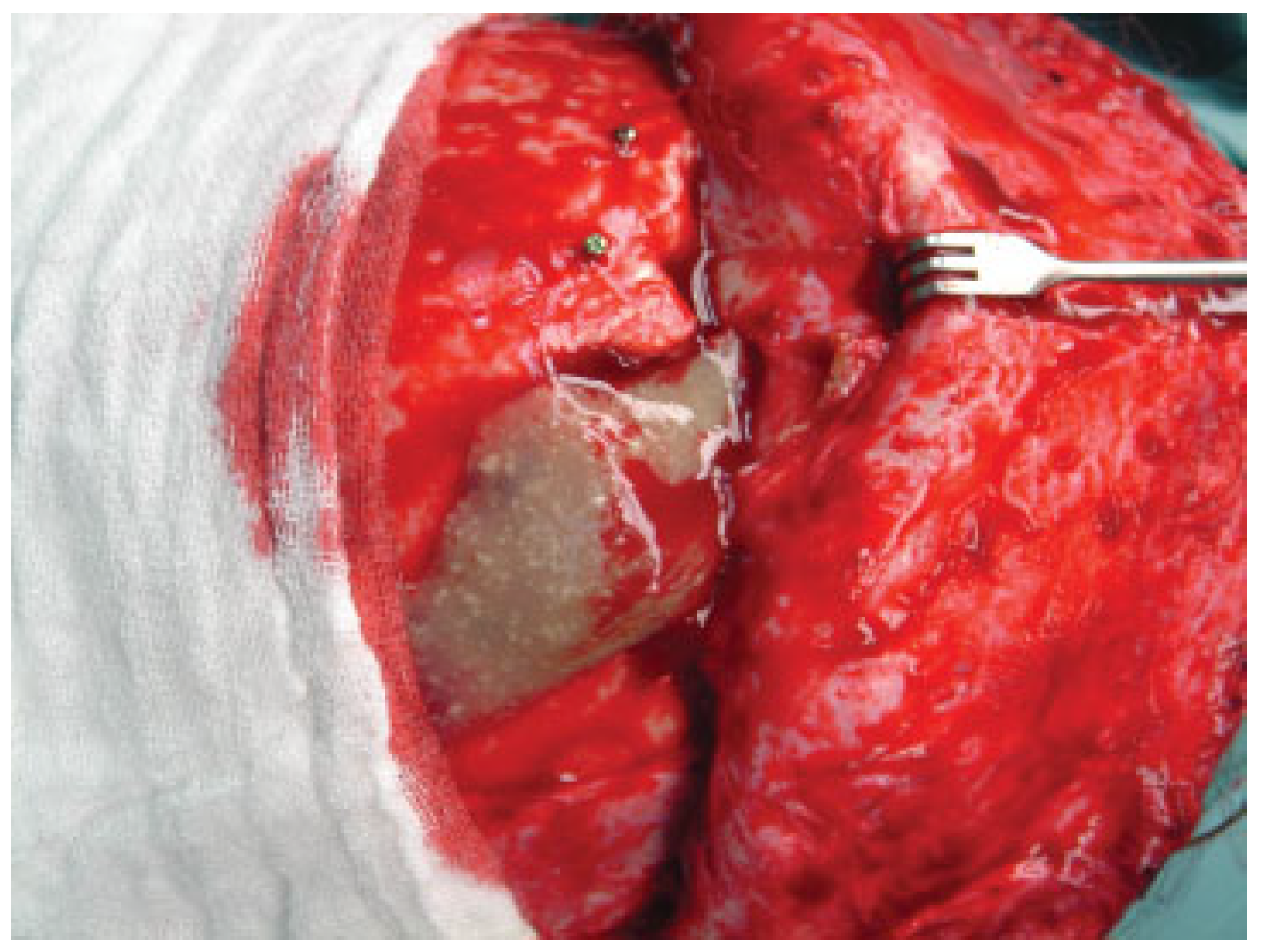
Posterior Table Fractures
Nasofrontal Duct Injury
Conclusions
References
- May, M.; Ogura, J.H.; Schramm, V. Nasofrontal duct in frontal sinus fractures. Arch. Otolaryngol. 1970, 92, 534–538. [Google Scholar] [CrossRef] [PubMed]
- Rohrich, R.J.; Hollier, L.H. Management of frontal sinus fractures. Changing concepts. Clin. Plast. Surg. 1992, 19, 219–232. [Google Scholar] [CrossRef] [PubMed]
- Choi, M.; Li, Y.; Shapiro, S.A.; Havlik, R.J.; Flores, R.L. A 10-year review of frontal sinus fractures: clinical outcomes of conservative manage-ment of posterior table fractures. Plast. Reconstr. Surg. 2012, 130, 399–406. [Google Scholar] [CrossRef] [PubMed]
- Strong, E.B.; Pahlavan, N.; Saito, D. Frontal sinus fractures: a 28-year retrospective review. Otolaryngol. Head. Neck Surg. 2006, 135, 774–779. [Google Scholar] [CrossRef]
- Manson, P.N.; Crawley, W.A.; Hoopes, J.E. Frontal cranioplasty: risk factors and choice of cranial vault reconstructive material. Plast. Reconstr. Surg. 1986, 77, 888–904. [Google Scholar] [CrossRef]
- Manson, P.N.; Markowitz, B.; Mirvis, S.; Dunham, M.; Yaremchuk, M. Toward CT-based facial fracture treatment. Plast. Reconstr. Surg. 1990, 85, 202–212. [Google Scholar] [CrossRef]
- Manolidis, S.; Hollier, L.H., Jr. Management of frontal sinus fractures. Plast. Reconstr. Surg. 2007, 120 (Suppl. S2), 32S–48S. [Google Scholar] [CrossRef]
- Jacobs, J.B. 100 years of frontal sinus surgery. Laryngoscope 1997, 107 Pt. 2, 1–36. [Google Scholar] [CrossRef]
- Bergara, A.R.; Itoiz, A.O. Present state of the surgical treatment of chronic frontal sinusitis. AMA Arch. Otolaryngol. 1955, 61, 616–628. [Google Scholar] [CrossRef]
- Stanley, R.B., Jr. Management of frontal sinus fractures. Facial Plast. Surg. 1988, 5, 231–235. [Google Scholar] [CrossRef]
- Stanley, R.B., Jr. Fractures of the frontal sinus. Clin. Plast. Surg. 1989, 16, 115–123. [Google Scholar] [PubMed]
- Stanley, R.B., Jr. Management of severe frontobasilar skull fractures. Otolaryngol. Clin. North. Am. 1991, 24, 139–150. [Google Scholar] [CrossRef]
- Stanley, R.B., Jr; Becker, T.S. Injuries of the nasofrontal orifices in frontal sinus fractures. Laryngoscope 1987, 97, 728–731. [Google Scholar] [CrossRef]
- Wallis, A.; Donald, P.J. Frontal sinus fractures: a review of 72 cases. Laryngoscope 1988, 98 Pt. 1, 593–598. [Google Scholar]
- Roden, K.S.; Tong, W.; Surrusco, M.; Shockley, W.W.; Van Aalst, J.A.; Hultman, C.S. Changing characteristics of facial fractures treated at a regional, level 1 trauma center, from 2005 to 2010: an assessment of patient demographics, referral patterns, etiology of injury, anatomic location, and clinical outcomes. Ann Plast Surg 2012, 68, 461–466. [Google Scholar] [PubMed]
- Sataloff, R.T.; Sariego, J.; Myers, D.L.; Richter, H.J. Surgical management of the frontal sinus. Neurosurgery 1984, 15, 593–596. [Google Scholar] [PubMed]
- Rohrich, R.J.; Hollier, L.H. The role of the nasofrontal duct in frontal sinus fracture management. J. Craniomaxillofac Trauma. 1996, 2, 31–40. [Google Scholar]
- Metzinger, S.E.; Guerra, A.B.; Garcia, R.E. Frontal sinus fractures: management guidelines. Facial Plast. Surg. 2005, 21, 199–206. [Google Scholar]
- Tiwari, P.; Higuera, S.; Thornton, J.; Hollier, L.H. The management of frontal sinus fractures. J. Oral. Maxillofac. Surg. 2005, 63, 1354–1360. [Google Scholar]
- Berryhill, W.E.; Rimell, F.L.; Ness, J.; Marentette, L.; Haines, S.J. Fate of rigid fixation in pediatric craniofacial surgery. Otolaryngol. Head. Neck Surg. 1999, 121, 269–273. [Google Scholar]
- Kim, C.H.; Kim, D.H.; Kim, H.; Song, S.Y. Treatment of frontal sinus fracture using bioabsorbable mesh plates. J. Craniofac Surg. 2012, 23, 549–551. [Google Scholar] [PubMed]
- Bhanot, S.; Alex, J.C.; Lowlicht, R.A.; Ross, D.A.; Sasaki, C.T. The efficacy of resorbable plates in head and neck reconstruction. Laryngoscope 2002, 112, 890–898. [Google Scholar] [PubMed]
- Bergsma, J.E.; de Bruijn, W.C.; Rozema, F.R.; Bos, R.R.; Boering, G. Late degradation tissue response to poly(L-lactide) bone plates and screws. Biomaterials 1995, 16, 25–31. [Google Scholar]
- Eppley, B.L.; Morales, L.; Wood, R.; et al. Resorbable PLLA-PGA plate and screw fixation in pediatric craniofacial surgery: clinical experience in 1883 patients. Plast Reconstr Surg 2004, 114, 850–856. [Google Scholar]
- Landes, C.A.; Ballon, A.; Roth, C. Maxillary and mandibular osteosyn-theses with PLGA and P(L/DL)LA implants: a 5-year inpatient biocompatibility and degradation experience. Plast. Reconstr. Surg. 2006, 117, 2347–2360. [Google Scholar] [PubMed]
- Strong, E.B.; Buchalter, G.M.; Moulthrop, T.H. Endoscopic repair of isolated anterior table frontal sinus fractures. Arch. Facial Plast. Surg. 2003, 5, 514–521. [Google Scholar]
- Graham, H.D.I.I.I.; Spring, P. Endoscopic repair of frontal sinus fracture: case report. J. Craniomaxillofac Trauma. 1996, 2, 52–55. [Google Scholar]
- Chen, D.J.; Chen, C.T.; Chen, Y.R.; Feng, G.M. Endoscopically assisted repair of frontal sinus fracture. J. Trauma. 2003, 55, 378–382. [Google Scholar]
- Mueller, R. Endoscopic treatment of facial fractures. Facial Plast. Surg. 2008, 24, 78–91. [Google Scholar]
- Gonty, A.A.; Marciani, R.D.; Adornato, D.C. Management of frontal sinus fractures: a review of 33 cases. J. Oral. Maxillofac. Surg. 1999, 57, 372–379. [Google Scholar]
- Nahum, A.M. The biomechanics of maxillofacial trauma. Clin. Plast. Surg. 1975, 2, 59–64. [Google Scholar] [PubMed]
- Duvall, A.J.I.I.I.; Porto, D.P.; Lyons, D.; Boies, L.R., Jr. Frontal sinus fractures. Analysis of treatment results. Arch. Otolaryngol. Head. Neck Surg. 1987, 113, 933–935. [Google Scholar]
- Gerbino, G.; Roccia, F.; Benech, A.; Caldarelli, C. Analysis of 158 frontal sinus fractures: current surgical management and complications. J. Craniomaxillofac Surg. 2000, 28, 133–139. [Google Scholar] [PubMed]
- Gossman, D.G.; Archer, S.M.; Arosarena, O. Management of frontal sinus fractures: a review of 96 cases. Laryngoscope 2006, 116, 1357–1362. [Google Scholar] [PubMed]
- Chen, K.T.; Chen, C.T.; Mardini, S.; Tsay, P.K.; Chen, Y.R. Frontal sinus fractures: a treatment algorithm and assessment of outcomes based on 78 clinical cases. Plast. Reconstr. Surg. 2006, 118, 457–468. [Google Scholar]
- Appelbaum, E. Meningitis following trauma to the head and face. JAMA 1960, 173, 1818–1822. [Google Scholar]
- Bell, R.B. Management of frontal sinus fractures. Oral. Maxillofac. Surg. Clin. North. Am. 2009, 21, 227–242. [Google Scholar]
- Day, T.A.; Meehan, R.; Stucker, F.J.; Nanda, A. Management of frontal sinus fractures with posterior table involvement: a retrospective study. J. Craniomaxillofac Trauma. 1998, 4, 6–9. [Google Scholar]
- Donald, P.J. Frontal sinus ablation by cranialization. Report of 21 cases. Arch. Otolaryngol. 1982, 108, 142–146. [Google Scholar]
- Luce, E.A. Frontal sinus fractures: guidelines to management. Plast. Reconstr. Surg. 1987, 80, 500–510. [Google Scholar]
- Stevens, M.; Kline, S.N. Management of frontal sinus fractures. J. Craniomaxillofac Trauma. 1995, 1, 29–37. [Google Scholar]
- Rodriguez, E.D.; Stanwix, M.G.; Nam, A.J.; et al. Twenty-six-year experi-ence treating frontal sinus fractures: a novel algorithm based on anatomical fracture pattern and failure of conventional techni-ques. Plast. Reconstr. Surg. 2008, 122, 1850–1866. [Google Scholar] [PubMed]
- Rohrich, R.J.; Mickel, T.J. Frontal sinus obliteration: in search of the ideal autogenous material. Plast. Reconstr. Surg. 1995, 95, 580–585. [Google Scholar]
- Friedman, C.D.; Costantino, P.D.; Jones, K.; Chow, L.C.; Pelzer, H.J.; Sisson GASr Hydroxyapatite cement, I.I. Obliteration and reconstruction of the cat frontal sinus. Arch. Otolaryngol. Head. Neck Surg. 1991, 117, 385–389. [Google Scholar] [PubMed]
- Mickel, T.J.; Rohrich, R.J.; Robinson, J.B., Jr. Frontal sinus obliteration: a comparison of fat, muscle, bone, and spontaneous osteoneogen-esis in the cat model. Plast. Reconstr. Surg. 1995, 95, 586–592. [Google Scholar]
- Peltola, M.J.; Aitasalo, K.M.; Suonpää, J.T.; Yli-Urpo, A.; Laippala, P.J.; Forsback, A.P. Frontal sinus and skull bone defect obliteration with three synthetic bioactive materials. A comparative study. J. Biomed. Mater. Res. B Appl. Biomater. 2003, 66, 364–372. [Google Scholar] [PubMed]
- Ross, D.A.; Marentette, L.J.; Thompson, B.G.; Haller, J.S. Use of hydroxy-apatite bone cement to prevent cerebrospinal fluid leakage through the frontal sinus: technical report. Neurosurgery 1999, 45, 401–402. [Google Scholar]
- Weber, R.; Draf, W.; Keerl, R.; et al. Magnetic resonance imaging following fat obliteration of the frontal sinus. Neuroradiology 2002, 44, 52–58. [Google Scholar]
- Ducic, Y.; Stone, T.L. Frontal sinus obliteration using a laterally based pedicled pericranial flap. Laryngoscope 1999, 109, 541–545. [Google Scholar]
- Montgomery, W.W. The fate of adipose implants in a bony cavity. Laryngoscope 1964, 74, 816–827. [Google Scholar]
- Sessions, R.B.; Alford, B.R.; Stratton, C.; Ainsworth, J.Z.; Shill, O. Current concepts of frontal sinus surgery: an appraisal of the osteoplastic flap-fat obliteration operation. Laryngoscope 1972, 82, 918–930. [Google Scholar] [CrossRef]
- Montgomery, W.W.; Pierce, D.L. Anterior osteoplastic fat obliteration for frontal sinus: Clinical experience and animal studies. Trans. Am. Acad. Ophthalmol. Otolaryngol. 1963, 67, 46–57. [Google Scholar]
- Peer, L.A. Loss of weight and volume in human fat grafts. Plast. Reconstr. Surg. 1950, 5, 217–230. [Google Scholar] [CrossRef]
- MacBeth, R. The osteoplastic operation for chronic infection of the frontal sinus. J. Laryngol. Otol. 1954, 68, 465–477. [Google Scholar] [CrossRef]
- Bosley, W.R. Osteoplastic obliteration of the frontal sinuses. A review of 100 patients. Laryngoscope 1972, 82, 1463–1476. [Google Scholar] [CrossRef] [PubMed]
- Xie, C.; Mehendale, N.; Barrett, D.; Bui, C.J.; Metzinger, S.E. 30-year retrospective review of frontal sinus fractures: The Charity Hospi-tal experience. J. Craniomaxillofac Trauma. 2000, 6, 7–15. [Google Scholar] [PubMed]
- Dujovny, M.; Aviles, A.; Anger, C. An innovative approach for cranio-plasty using hydroxyapatite cement. Surg. Neurol. 1997, 48, 294–297. [Google Scholar] [CrossRef]
- Kveton, J.F.; Friedman, C.D.; Piepmeier, J.M.; Costantino, P.D. Reconstruc-tion of suboccipital craniectomy defects with hydroxyapatite cement: a preliminary report. Laryngoscope 1995, 105, 156–159. [Google Scholar] [CrossRef]
- Maniker, A.; Cantrell, S.; Vaicys, C. Failure of hydroxyapatite cement to set in repair of a cranial defect: case report. Neurosurgery 1998, 43, 953–954. [Google Scholar] [CrossRef]
- Snyderman, C.H.; Scioscia, K.; Carrau, R.L.; Weissman, J.L. Hydroxyapa-tite: an alternative method of frontal sinus obliteration. Otolar-yngol Clin. North. Am. 2001, 34, 179–191. [Google Scholar] [CrossRef]
- Smith, T.L.; Han, J.K.; Loehrl, T.A.; Rhee, J.S. Endoscopic management of the frontal recess in frontal sinus fractures: a shift in the para-digm? Laryngoscope 2002, 112, 784–790. [Google Scholar] [PubMed]
- Thong, J.F.; Lee, J. Single-stage strategy for management of anterior table frontal sinus fractures involving the frontal sinus outflow tract. Eur. J. Plast. Surg. 2011, 34, 299–303. [Google Scholar] [CrossRef]
- Ung, F.; Sindwani, R.; Metson, R. Endoscopic frontal sinus obliteration: a new technique for the treatment of chronic frontal sinusitis. Otolaryngol. Head. Neck Surg. 2005, 133, 551–555. [Google Scholar] [PubMed]
- Smith, T.L.; Han, J.K.; Loehrl, T.A.; Rhee, J.S. Endoscopic management of the frontal recess in frontal sinus fractures: a shift in the para-digm? Laryngoscope 2002, 112, 784–790. [Google Scholar]


© 2013 by the author. The Author(s) 2013.
Share and Cite
Weathers, W.M.; Wolfswinkel, E.M.; Hatef, D.A.; Lee, E.I.; Brown, R.H.; Hollier, L.H., Jr. Frontal Sinus Fractures: A Conservative Shift. Craniomaxillofac. Trauma Reconstr. 2013, 6, 155-160. https://doi.org/10.1055/s-0033-1349210
Weathers WM, Wolfswinkel EM, Hatef DA, Lee EI, Brown RH, Hollier LH Jr. Frontal Sinus Fractures: A Conservative Shift. Craniomaxillofacial Trauma & Reconstruction. 2013; 6(3):155-160. https://doi.org/10.1055/s-0033-1349210
Chicago/Turabian StyleWeathers, William M., Erik M. Wolfswinkel, Daniel A. Hatef, Edward I. Lee, Rodger H. Brown, and Larry H. Hollier, Jr. 2013. "Frontal Sinus Fractures: A Conservative Shift" Craniomaxillofacial Trauma & Reconstruction 6, no. 3: 155-160. https://doi.org/10.1055/s-0033-1349210
APA StyleWeathers, W. M., Wolfswinkel, E. M., Hatef, D. A., Lee, E. I., Brown, R. H., & Hollier, L. H., Jr. (2013). Frontal Sinus Fractures: A Conservative Shift. Craniomaxillofacial Trauma & Reconstruction, 6(3), 155-160. https://doi.org/10.1055/s-0033-1349210


