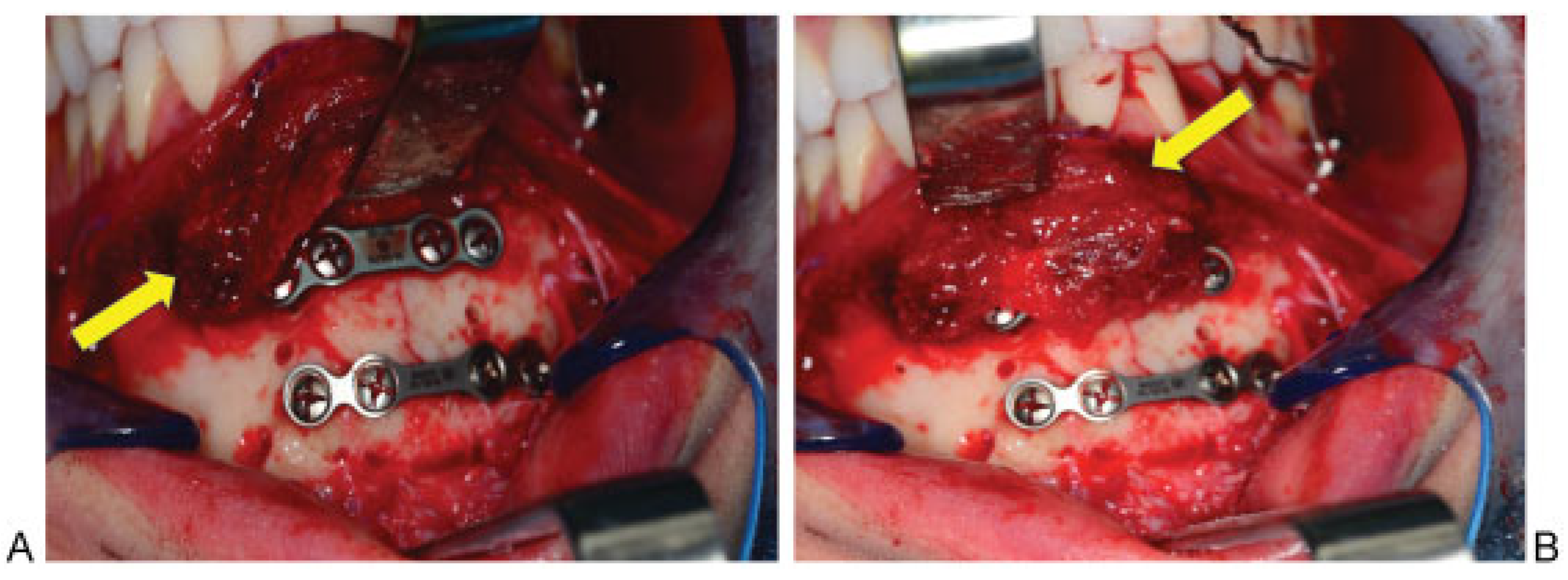
Soft Tissue Coverage for Mandibular Fractures Using Two Miniplates
Abstract
:References
- Cordeiro, P.G.; Hidalgo, D.A. Soft tissue coverage of mandibular reconstruction plates. Head Neck 1994, 6, 112–115. [Google Scholar] [CrossRef] [PubMed]
- Klotch, D.W.; Prein, J. Mandibular reconstruction using AO plates. Am. J. Surg. 1987, 154, 384–388. [Google Scholar] [CrossRef] [PubMed]
- Viol, A.; Pradka, S.P.; Baumeister, S.P.; Wang, D.; Moyer, K.E.; Zura, R.D.; Olson, S.A.; Zenn, M.R.; Levin, S.L.; Erdmann, D. Soft-tissue defects and exposed hardware: a review of indications for soft-tissue reconstruction and hardware preservation. Plast. Reconstr. Surg. 2009, 123, 1256–1263. [Google Scholar] [CrossRef] [PubMed]
- Ellis, E., III. A study of 2 bone plating methods for fractures of the mandibular symphysis/body. J. Oral Maxillofac. Surg. 2011, 69, 1978–1987. [Google Scholar] [CrossRef] [PubMed]
- McCormick, S.U.; Stern, J.C. Split mentalis flap for reconstruction of the anterior mandible. J. Oral Maxillofac. Surg. 1996, 54, 1031–1033. [Google Scholar] [CrossRef] [PubMed]
- Hochberg, J.; Ardenghy, M.; Yuen, J.; Gonzalez-Cruz, R.; Miura, Y.; Conrado, R.M.; Pait, T.G. Muscle and musculocutaneous flap coverage of exposed spinal fusion devices. Plast. Reconstr. Surg. 1998, 102, 385–389. [Google Scholar] [CrossRef] [PubMed]
- Cienfuegos, R.; Cornelius, C.P.; Ellis, E.; Kushner, G. Mandible–Body: Simple–ORIF. In: Kushner G, ed. AO Foundation, AO Surgery Reference. Available online: www.aofoundation.


© 2008 by the author. The Author(s) 2008.
Share and Cite
Shah, A.; Patel, A.; Steinbacher, D. Soft Tissue Coverage for Mandibular Fractures Using Two Miniplates. Craniomaxillofac. Trauma Reconstr. 2012, 5, 253-254. https://doi.org/10.1055/s-0032-1329543
Shah A, Patel A, Steinbacher D. Soft Tissue Coverage for Mandibular Fractures Using Two Miniplates. Craniomaxillofacial Trauma & Reconstruction. 2012; 5(4):253-254. https://doi.org/10.1055/s-0032-1329543
Chicago/Turabian StyleShah, Ajul, Anup Patel, and Derek Steinbacher. 2012. "Soft Tissue Coverage for Mandibular Fractures Using Two Miniplates" Craniomaxillofacial Trauma & Reconstruction 5, no. 4: 253-254. https://doi.org/10.1055/s-0032-1329543
APA StyleShah, A., Patel, A., & Steinbacher, D. (2012). Soft Tissue Coverage for Mandibular Fractures Using Two Miniplates. Craniomaxillofacial Trauma & Reconstruction, 5(4), 253-254. https://doi.org/10.1055/s-0032-1329543


