Recent studies examined battle injury patterns and resource impacts of injuries for Operation Iraqi Freedom and Operation Enduring Freedom and have highlighted the significance of head and neck injuries. Craniomaxillofacial (CMF) battle injuries are characterized by penetrating soft tissue wounds and fractures (58% and 27%, respectively) [
1]. The frequency of head and neck injuries accounts for 29% of all battle injuries in the conflicts, which is an increase from previous wars [
2]. Looking at the same cohort, Masini et al. found head and neck injuries required 20% of all treatment resources, had the highest mean disability rating (52%), and will command 27% of all total projected benefit costs [
3]. The majority of service members burned on the battlefield (77%) sustained burns to the head, primarily to the face [
4].
The purpose of this case series is to highlight the severity of CMF battle injuries, detail the full application of conventional surgical procedures, and describe the compromised out- comes of four battle-injured service members. This information will identify potential opportunities for improving care through research.
Case Reports
Patient 1
Patient 1 is a 22-year-old male soldier injured in Iraq by an explosive device. The injury resulted in a mandibular composite tissue avulsion with continuity defect from the molar regions forward. Patient 1 also suffered minor orthopedic injuries. Initial treatment of CMF injuries in theater included tracheotomy, wound debridement, and fixation of the mandible fracture with external pin fixation. The mandibular soft tissue defect was temporarily closed and the patient evacuated to BAMC in San Antonio, Texas.
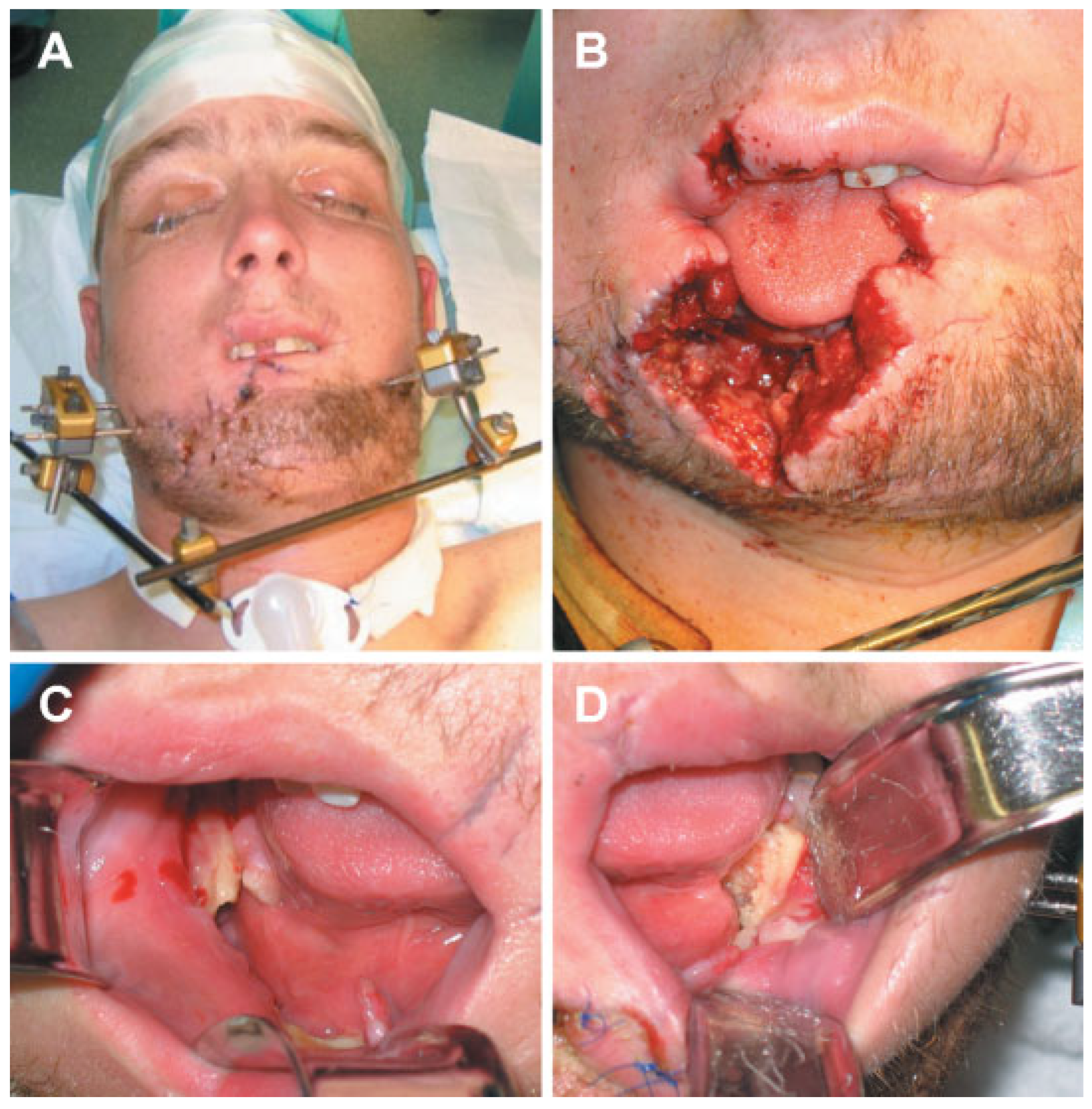
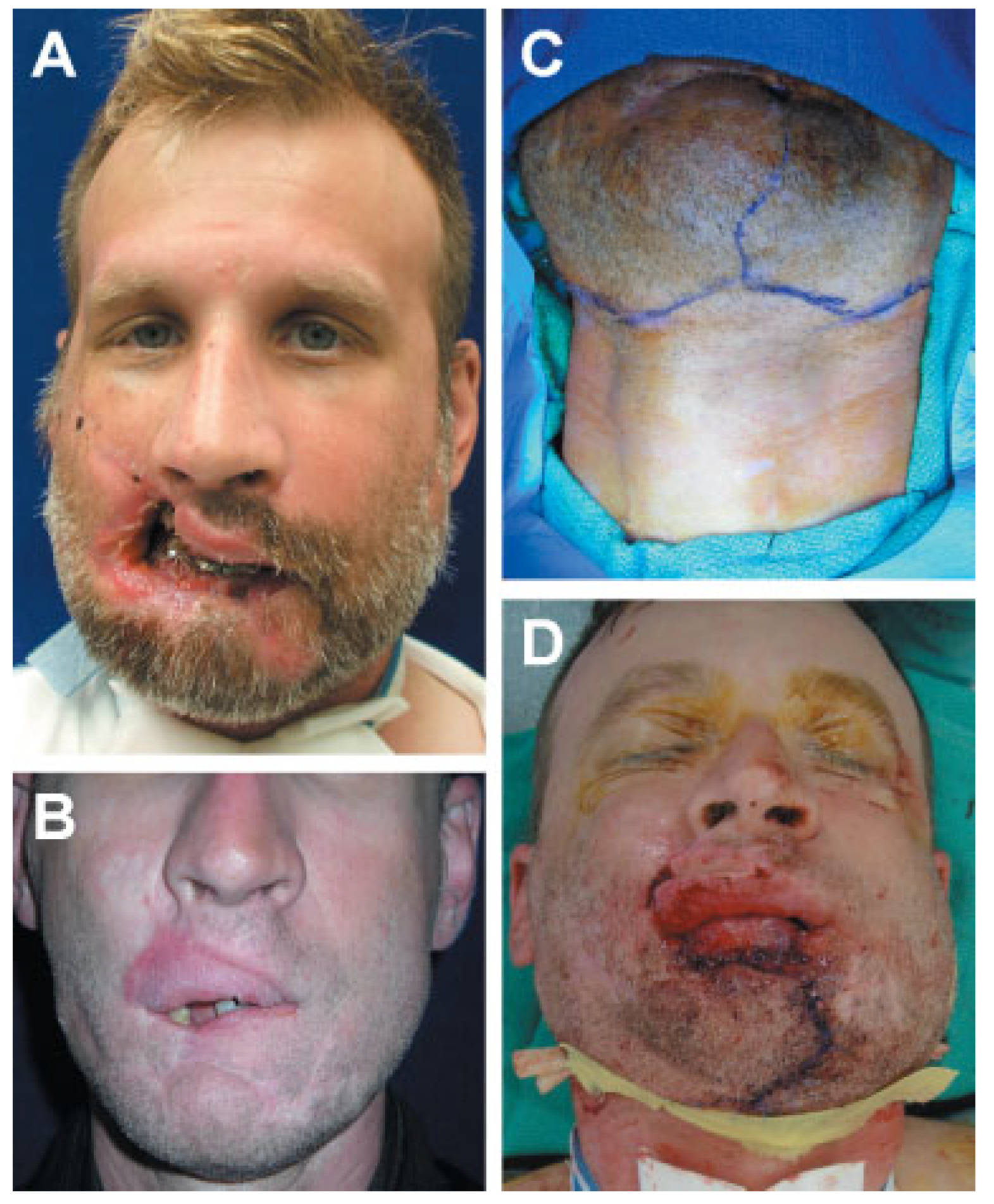
One week after injury, patient 1 arrived at BAMC in stable condition and was admitted to the Oral and Maxillofacial Surgery (OMS) service (
Figure 1). The wound was opened, and a locking 2.4-mm titanium reconstruction plate replaced external pin fixation. A 65% central defect of the lower lip and chin was noted and closed primarily pending future reconstruction (
Figure 2).
A multidisciplinary surgical team presented the patient with a free osteofasciocutaneous fibula flap option to reconstruct the chin, lower lip, floor of the mouth, and mandible. Due to the elapsed time from injury to the first surgery, contamination of the site, and concern about the condition of the recipient bed and continued necrosis of the bone, the free flap procedure was delayed 8 weeks. Though arguments have been made for immediate free flap reconstruction [
5], due to the circumstances, research supports this delay to allow the wound to declare itself before reconstruction [
6,
7]. Three months postinjury, a microvascular team of plastic surgeons performed the fibula procedure. Postoperative venous congestion complicated the flap and, despite multiple attempts to salvage the flap, the patient suffered complete flap loss 1 week after surgery. Salvage attempts included evacuation of hematoma, release of tension on the periphery of the flap, application of nitroglycerin paste, and medicinal leeches.
Patient 1 returned to the operating room 4 weeks after fibula flap failure for soft tissue reconstruction with a pectoralis major flap, transferring skin paddles to reconstruct the chin/lip subunit and the floor of the mouth. A buccal mucosal advancement graft reconstructed the lower lip vermillion. Three months after pectoralis flap reconstruction, a particulated corticocancellous bone graft from the right posterior iliac crest was placed through a neck incision into a cadaveric mandibular crib.
Six months later, the patient developed a cutaneous fistula with exposure of the inferior portion of the cadaveric crib. In addition, fracture of the 2.4-mm reconstruction plate and nonunion at the left mandible–graft interface occurred. To treat this situation, the exposed bone was debrided, a fistulotomy was performed, and the fractured hardware replaced with two parallel 2.0-mm plates.
The fistula persisted with a larger area of exposed bone until 2.5 months later, when a superiorly based sternocleidomastoid flap finally closed the wound, but the bone-grafted mandible was noted to be dimensionally inadequate and pencil-thin. In addition, the overlying skin was thin and inflamed. A second team of microvascular surgeons per- formed another free osteofasciocutaneous fibula flap procedure to reconstruct the mandible 9 months later, 2 years after initial injury.
Currently, patient 1 is 6 months post–fibula flap and presents with mandibular continuity and sufficient bone for dental reconstruction. However, he suffers from an adynamic and incompetent lower lip, microstomia, decreased mandibular range of motion, an extruded maxillary dentition, and an edentulous mandible. In addition, he has speech difficulties, cannot eat a typical diet, and has a deformity of the chin and lower lip secondary to extensive scarring (
Figure 3). A vestibuloplasty is planned to support prosthodontic rehabilitation with placement of implant-supported hybrid denture prosthesis. He has undergone a total of 10 major operations, consisting of a combination of seven bone and nine soft tissue procedures over a 2-year period, without restoration of facial form or function.
Patient 2
Patient 2 is a 37-year-old male soldier injured in Iraq by an explosive device. His injuries included perforating wounds to the face resulting in a Le Fort II fracture, comminuted bilateral mandibular condyle, ramus and body fractures, as well as soft tissue avulsion of 40% of the right upper lip and 80% of the lower lip, including the right commissure. Initial stabilization in theater included tracheotomy and maxillomandibular fixation (MMF;
Figure 4).
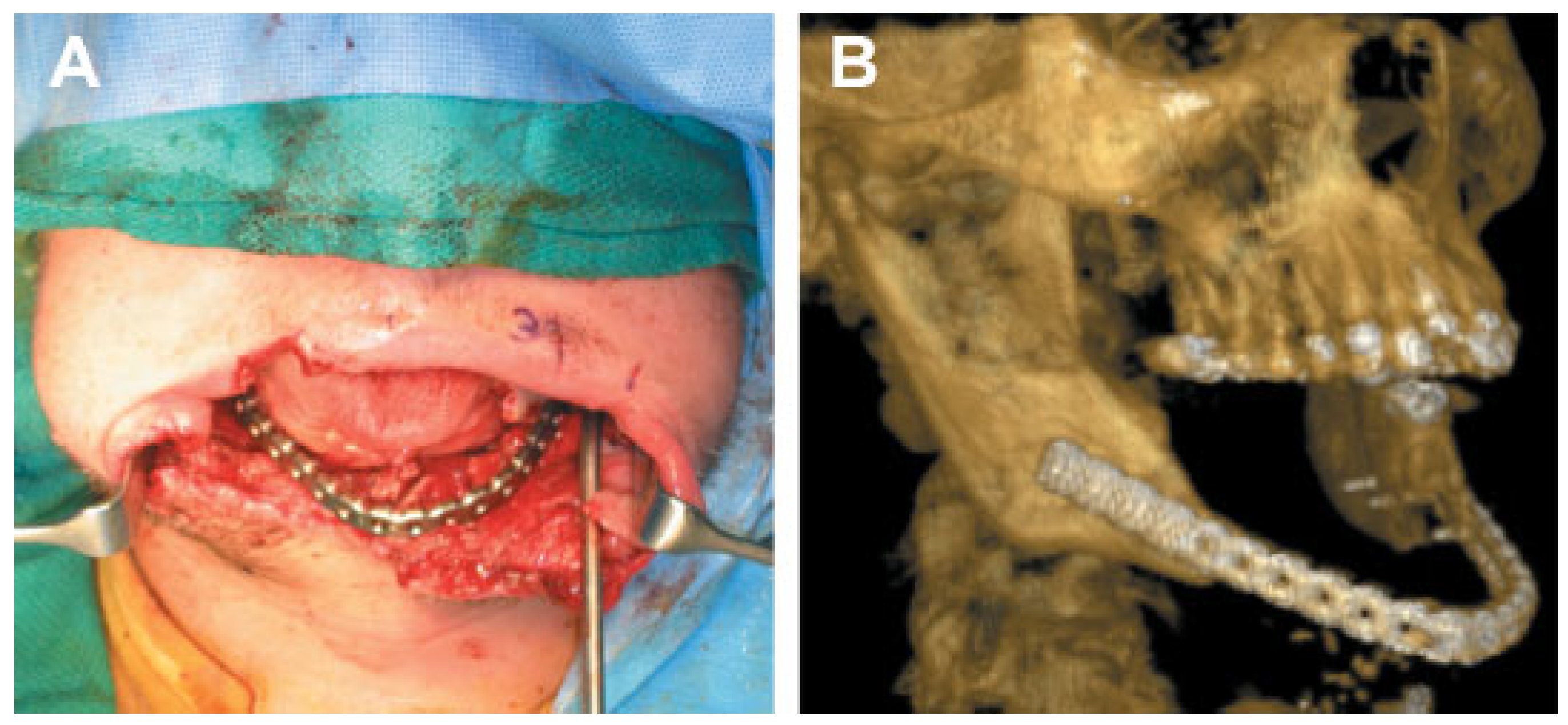
Patient 2 arrived at BAMC 1 week after injury in stable condition. He was taken to the operating room for examination under anesthesia and debridement of his wounds. The Le Fort II fracture was anatomically reduced and fixated with miniplates. Postoperatively, computed tomography (CT) scans were performed to fabricate a mandibular stereolithography resin model. Based on the resin models, reconstruction plates were bent preoperatively.
Patient 2 returned to the operating room 2.5 weeks post- injury for open reduction internal fixation of the mandibular fractures through a neck incision. The comminuted right ramus and condyle fractures were deemed nonrepairable. After debridement of the comminuted fractures, the right ramus and condyle area was reconstructed with an immediate costochondral graft and a 2.4-mm reconstruction plate.
The comminuted left condyle and body fractures were re- paired with 2.0-mm reconstruction plates (
Figure 5). A right cheek wound was closed in layers after debridement and placement of a drain.
Four weeks after bone reconstruction (
Figure 6A), the ear, nose, and throat service performed soft tissue reconstruction of the lip defects with lateral sliding cheek and rhomboid flaps. The postoperative course was complicated by dehiscence of the flap and contracture of the right commissure with failure to achieve lip competence. A revision procedure was performed 6 weeks later with a buccal advancement flap. Nine months after the cheek and mucosal flap reconstructions, the patient presented to OMS service with left mandible pain and swelling, multiple scar contractures, microstomia, and an obvious lip deformity (
Figure 6B). Evaluation showed hardware failure with nonunion of the left mandible body and a continuity defect of the right mandible body. To improve his immediate concern of excessive mucosa display, the upper right lip scar was excised and recon- structed with a full-thickness skin graft harvested from the left chest.
Two months later patient 2 was taken back to the operating room by OMS service for mandible and lower lip reconstruction. After tracheotomy, a midlevel cervical flap was developed to expose the mandibular body. Previously placed hardware was removed and 2.4-mm reconstruction plates placed. The area was treated with recombinant human bone morphogenetic protein-2 with titanium mesh to maintain space for bone regeneration. A procedure was created for this patient to lengthen the lower lip, increase the intercommissure distance, and reconstruct the missing lower lip vermillion: The lower lip, chin, and neck were divided vertically at the midline to the level of the cervical incision and cervicofacial flaps developed (
Figure 6C). These cervicofacial flaps were then advanced and rotated anterosuperiorly to increase the lower lip height and intercommissure dimension. An anteriorly based ventral tongue flap was then used to reconstruct the lower lip vermilion (
Figure 6D).
Postoperatively, the patient was heavily sedated for 2 weeks with a mouth prop between his teeth to avoid trauma to the tongue flap. The tongue pedicle was divided 18 days postoperatively. As a result of the surgery, the patient displayed facial features representative of upper and lower lips. The lips were adequate when viewed frontally but on profile, the lower lip projected poorly. In addition, lip incompetence persisted.
One year after mandible and lip reconstruction, the patient experienced trauma to the left mandible after an altercation. Clinical evaluation and CT scans revealed a left mandibular body fracture in the area of bone regenerate. After fracture and hardware debridement, a 2.4-mm reconstruction bar was placed and area grafted with iliac crest bone.
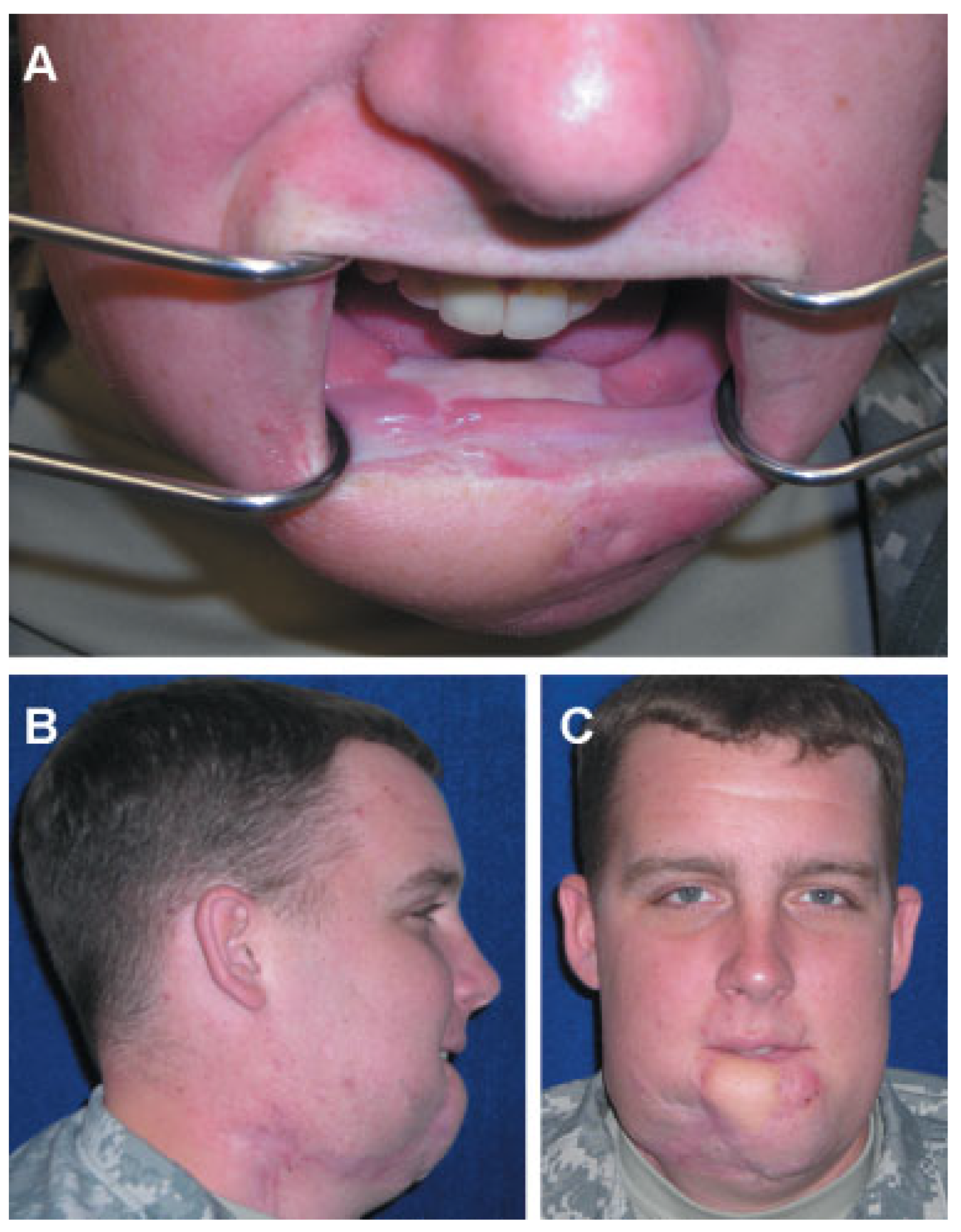
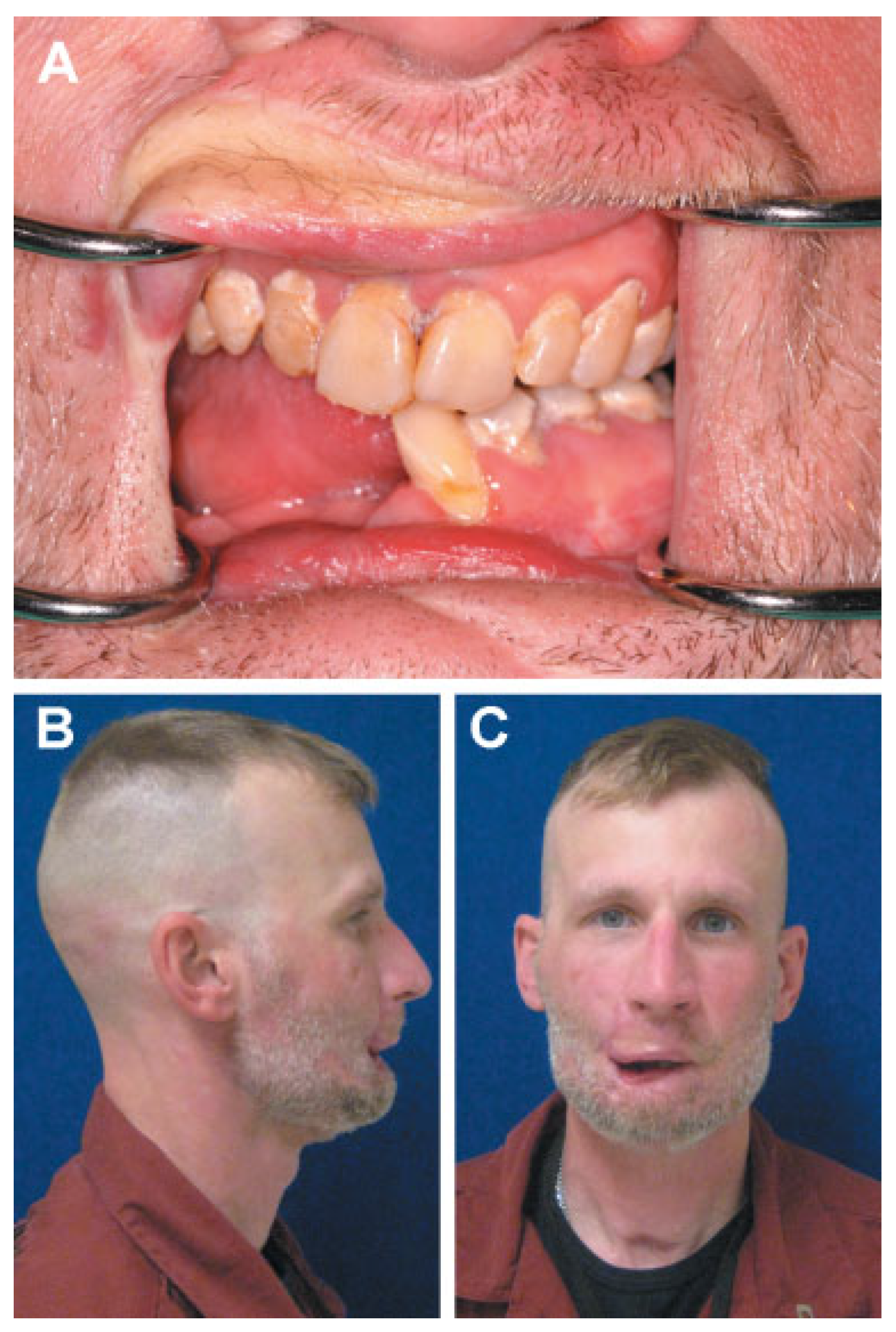
The patient currently has mandibular continuity but suffers from microstomia, decreased range of motion, extra- articular ankylosis, lip incompetence, and failing dentition (
Figure 7). The patient’s most striking oral dysfunction, however, is difficulty enunciating words due to loss of orbicularis oris function. In addition, the patient suffers from drooling and has difficulty eating a typical diet, which makes social engagement difficult. The patient has undergone a total of nine major operations, consisting of a combination of five bone and six soft tissue procedures over a 2-year period, without adequate restoration of form or function of his injured face.
Patient 3
Patient 3 is a 34-year-old male soldier injured in Afghanistan by an explosive device that caused second- and third-degree burns to his face and scalp and shrapnel perforations into the right orbit, frontal sinus, and face. These perforating wounds resulted in comminuted Le Fort II, naso-orbital-ethmoid, frontal sinus, and bilateral mandibular fractures, with a right open-globe injury. The patient also suffered burns to his right upper extremity and chest. Initial stabilization in theater included MMF and right globe enucleation (
Figure 8).
Patient 3 arrived at BAMC in serious condition 4 days after injury. After the facial fractures were stabilized by MMF, priority was given to debridement and closure of burn wounds with split-thickness skin grafting. Because of the burned condition of overlying skin, the comminuted frontal sinus and naso-orbital-ethmoid fractures were treated with wet to dry dressing. Burns resulted in loss of the right ear, partial loss of the left ear, and loss of the cartilaginous portion of the nose.
Following primary burn management (
Figure 9A), 3 weeks later OMS service performed a tracheotomy and cervical incisions to expose the comminuted mandible fragments. After debridement, reconstruction plates were adapted and reduction achieved. Open reduction internal fixation of the maxillary fractures was accomplished through vestibular incisions. The patient was also fitted with a right prosthetic globe replacement.
Two months later, patient 3 underwent several procedures to release burn scar contractures under the direction of plastics/burn service. An attempt to reconstruct the nasal alae with melolabial flaps failed on the right side because of compromised tissue quality from burn injury. Six months after failed nasal reconstruction, he underwent bilateral tissue expansion in the supraclavicular regions in preparation for facial skin resurfacing. After 3 months of tissue expansion, transposition of the supraclavicular flaps was performed after excision of cheek scars (
Figure 9B) [
8,
9]. One month later, the expanded supraclavicular flaps were separated, thinned, and inset with the residual pedicle repositioned cervically. Four months later, a paramedian forehead flap was performed to replace the nasal tip, but this procedure was complicated by partial loss of the flap. Additional procedures included skin grafts to treat recurrent ectropion and titanium auricular implants placed to treat acquired anotia.
Patient 3 currently suffers from severe naso-orbital deformity, microstomia, extra-articular ankylosis secondary to facial scars, ectropion of the left lower eyelid, and nasal dysfunction (
Figure 10). His functional impairments include inability to eat a typical diet, chronic dry eye due to ectropion, and loss of nasal tip. Two years after injury, the patient has undergone 26 operations to the CMF region, consisting of three bone and 23 soft tissue procedures, without restoration of form or function.
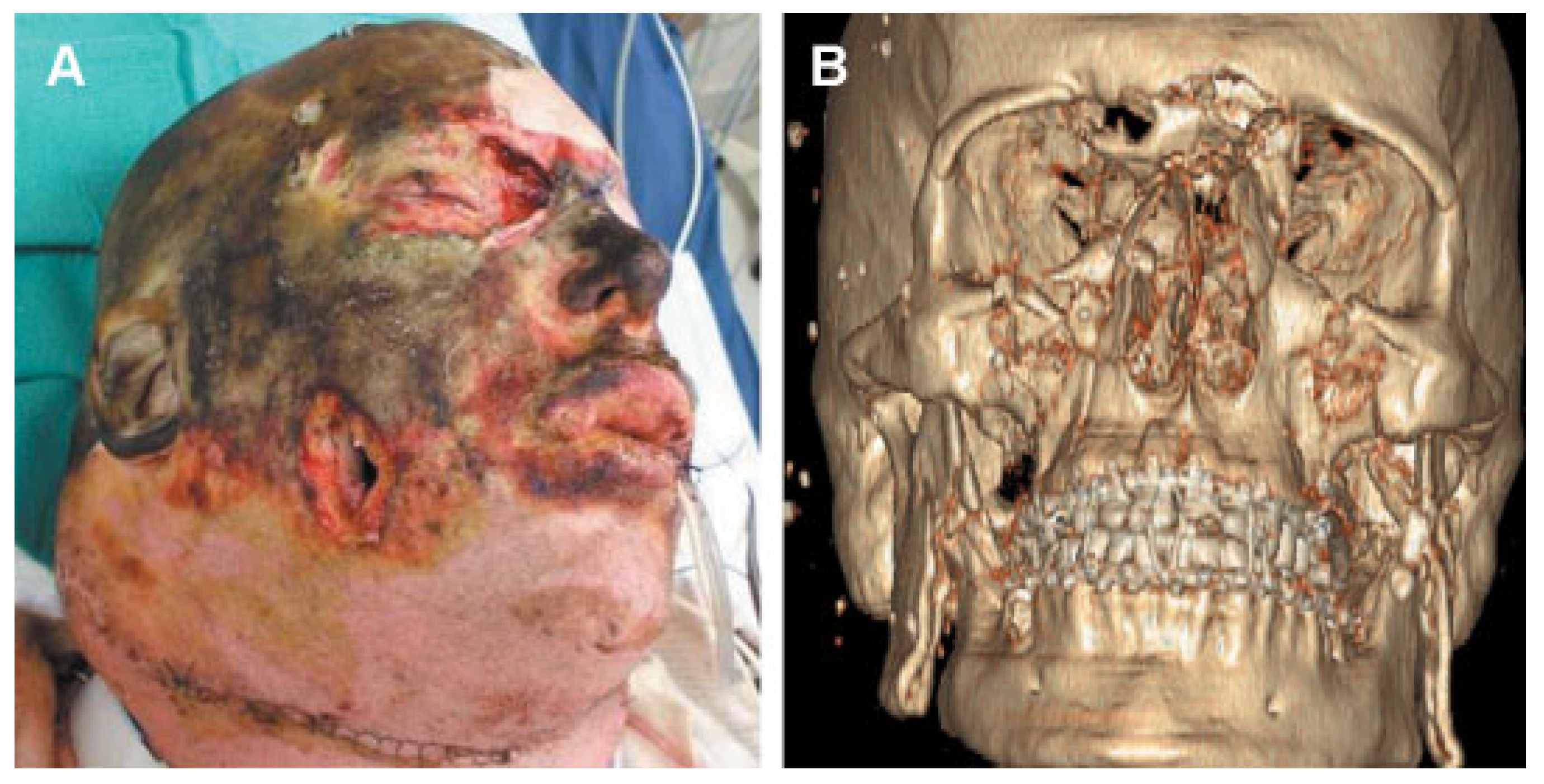
Patient 4
Patient 4 is a 27-year-old male Marine injured in Iraq by an explosive device. Injuries included comminuted anterior mandibular fractures, bilateral rami and condyle fractures, and 64% total body surface area burns (face, scalp, neck, chest, back, and both upper extremities). Initial stabilization in theater included a tracheotomy and an MMF (
Figure 11 and
Figure 12).
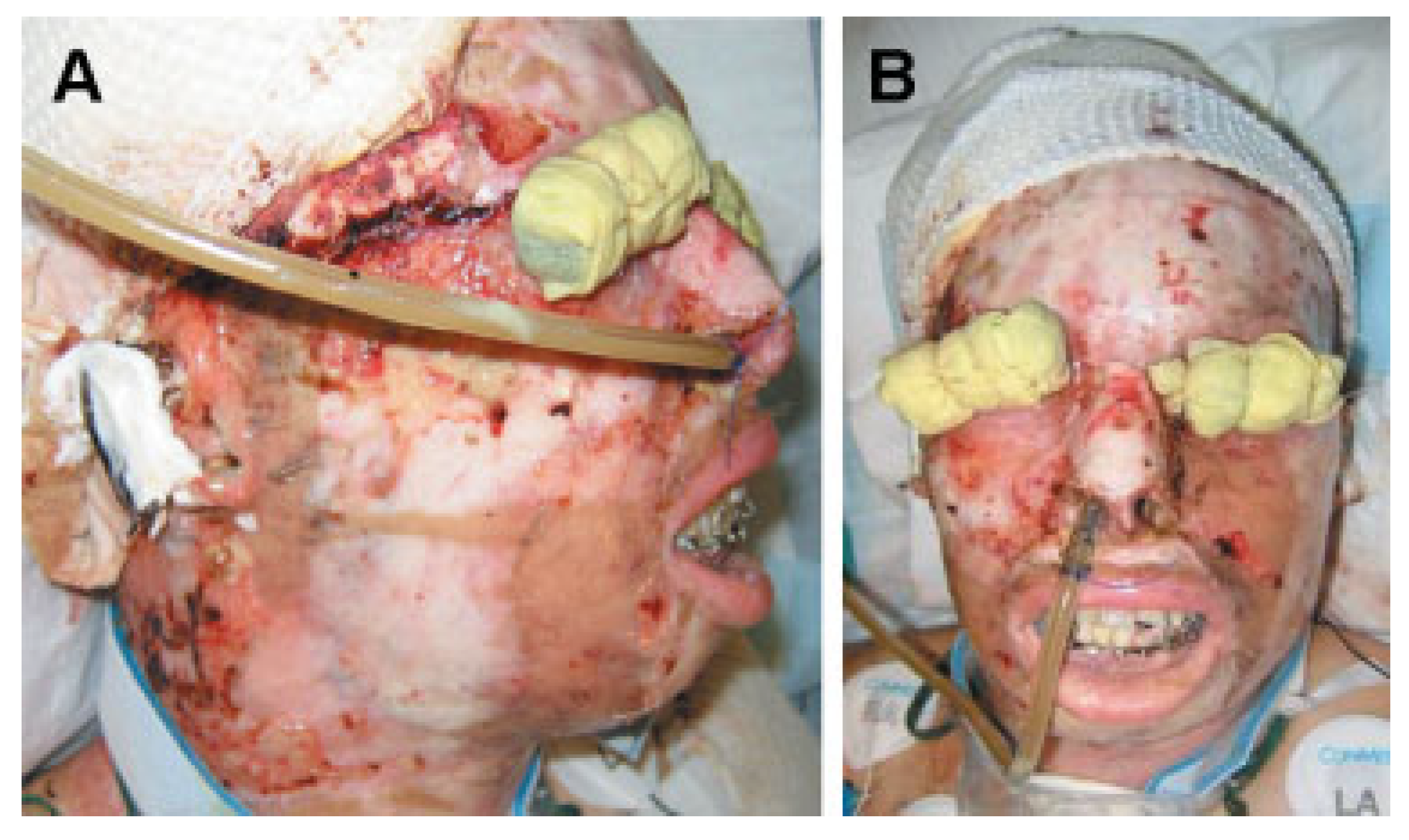
Patient 4 arrived in critical condition at BAMC 3 days after injury. He remained in serious condition for 5 months with his burn injuries constantly threatening his life. During this period and immediately afterward he underwent multiple burn, orthopedic, and general surgery procedures. Because of the severity and extent of his facial burn injuries, which limited conventional surgical approaches, reconstruction of his facial fractures was delayed. The patient remained in MMF for 12 weeks.
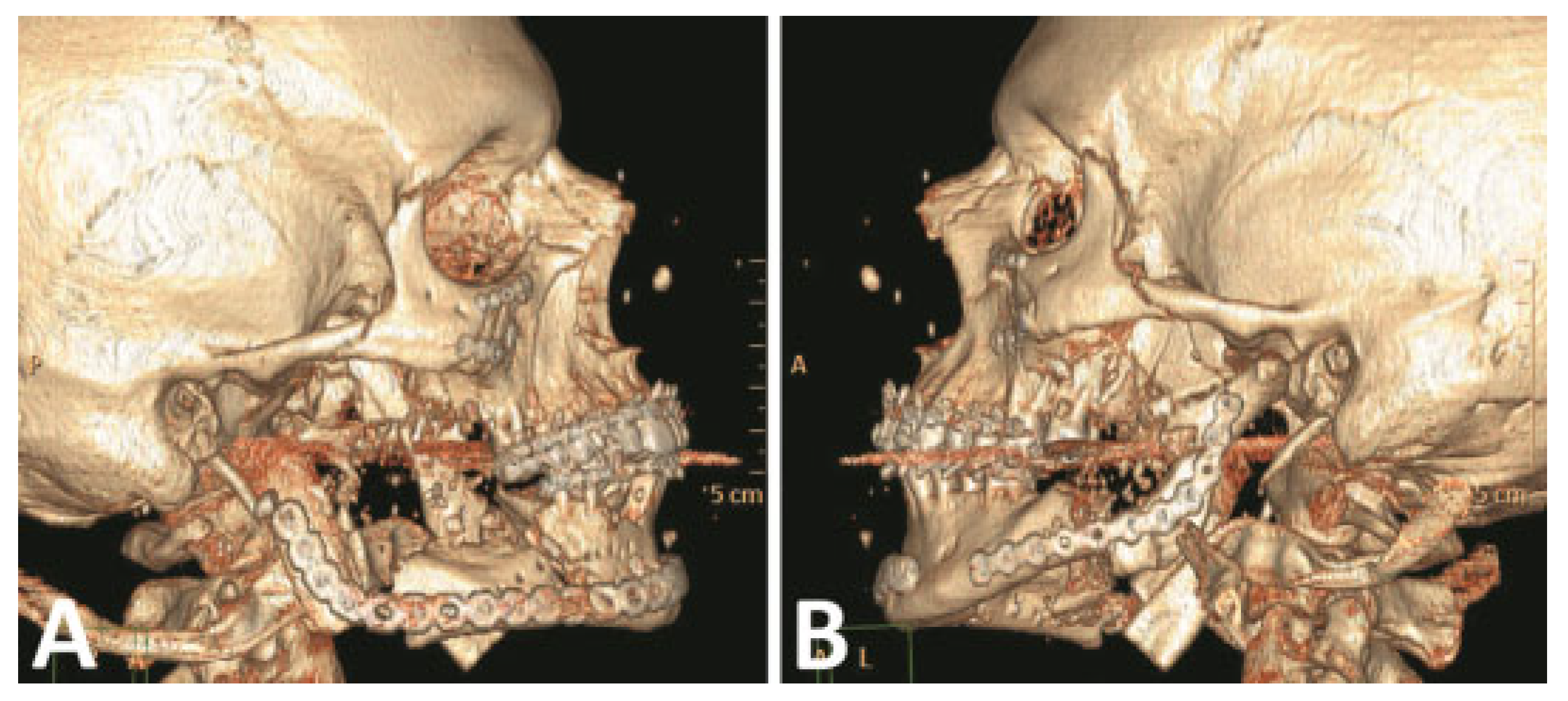
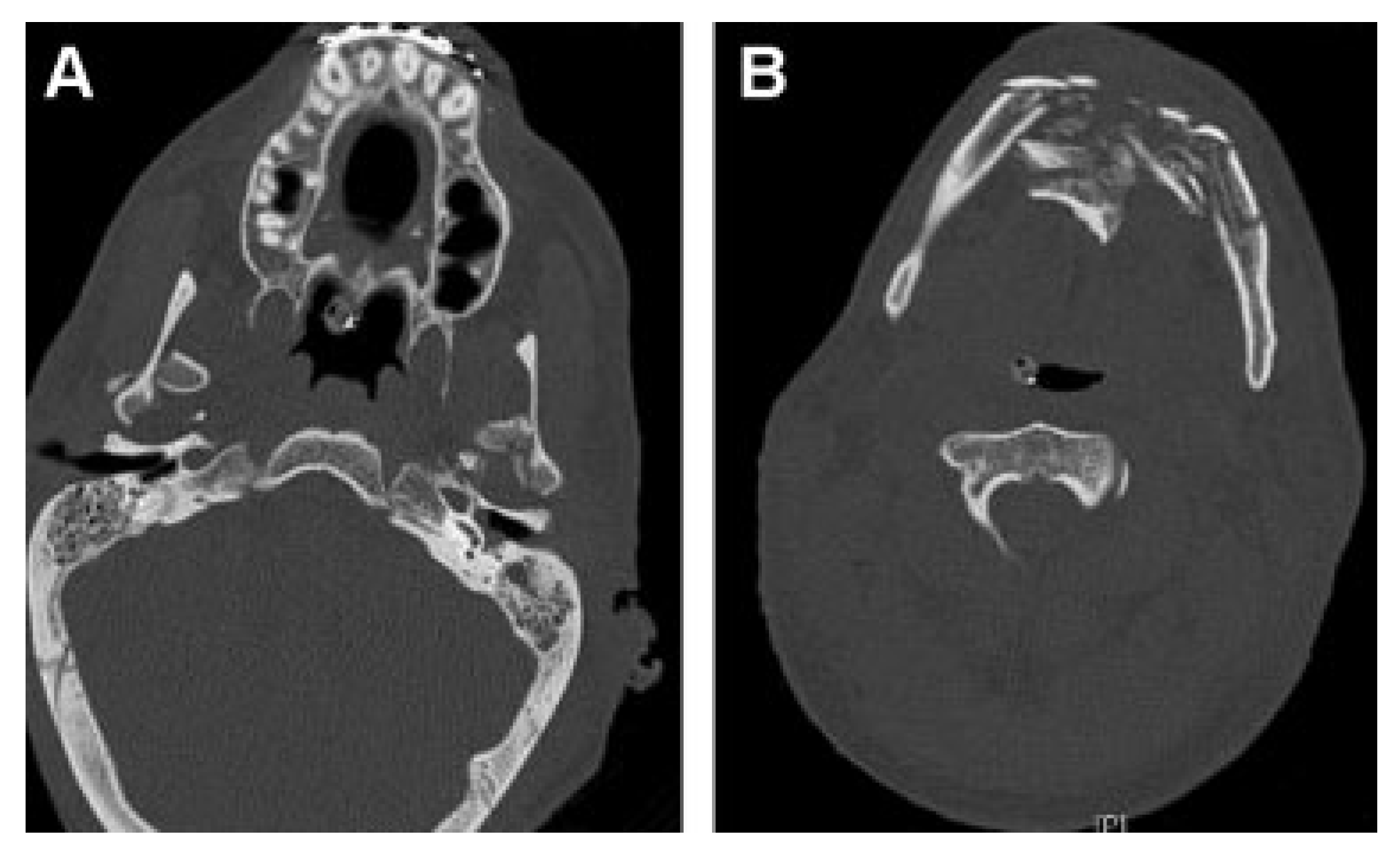
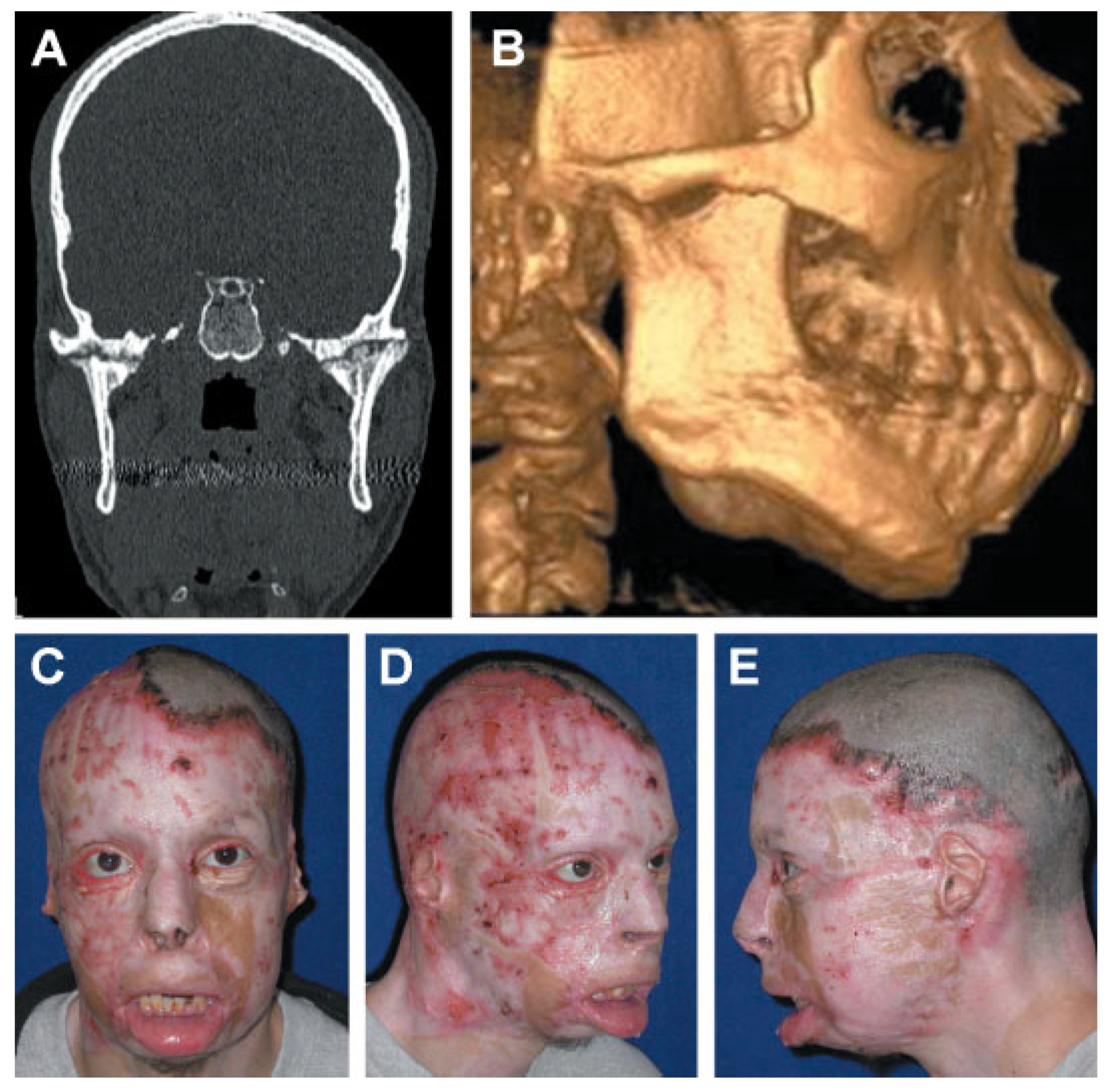
Nine months after injury, Patient 4 complained of drooling and difficulty eating. CT images revealed malunion of the anterior mandible fracture and bilateral bony ankylosis of craniomandibular articulations (
Figure 13A,B). The patient also had lower lid ectropions, lower lip eversion, microstomia, chin ptosis, and lip incompetence secondary to burn scar contracture and malunion of the anterior mandible (
Figure 13C–E).
To address these conditions, patient 4 underwent bilateral submandibular and preauricular incisions to expose the ankylosed craniomandibular articulations. The ankylosed articulations were resected and reconstructed with immediate costochondral grafts. The excised bone was used to onlay graft the chin defect. Four months later, a midlevel cervical incision with extensive undermining in a subplatysmal plane was performed to release extensive neck contractures. A genioplasty through the cervical flap was performed to establish chin projection. The flaps were advanced superiorly to improve lip eversion and chin ptosis. The cervical flaps were sutured to the hyoid fascia to reconstruct and define the cervicofacial region. The postoperative course was complicated by development of a fistula in the left mandibular region, which was later excised and closed.
After 3 months of bone healing, under the direction of the plastics/burn service, patient 4 was admitted for multiple facial soft tissue procedures, including full-thickness grafts to the eyelids, paramedian forehead flap reconstruction of the nasal tip and ala, perioral and periorbital scar contracture release, and facial resurfacing with expanded supraclavicular transpositional flaps. Titanium auricular implants were also placed in the temporal bone to support ear prosthesis.
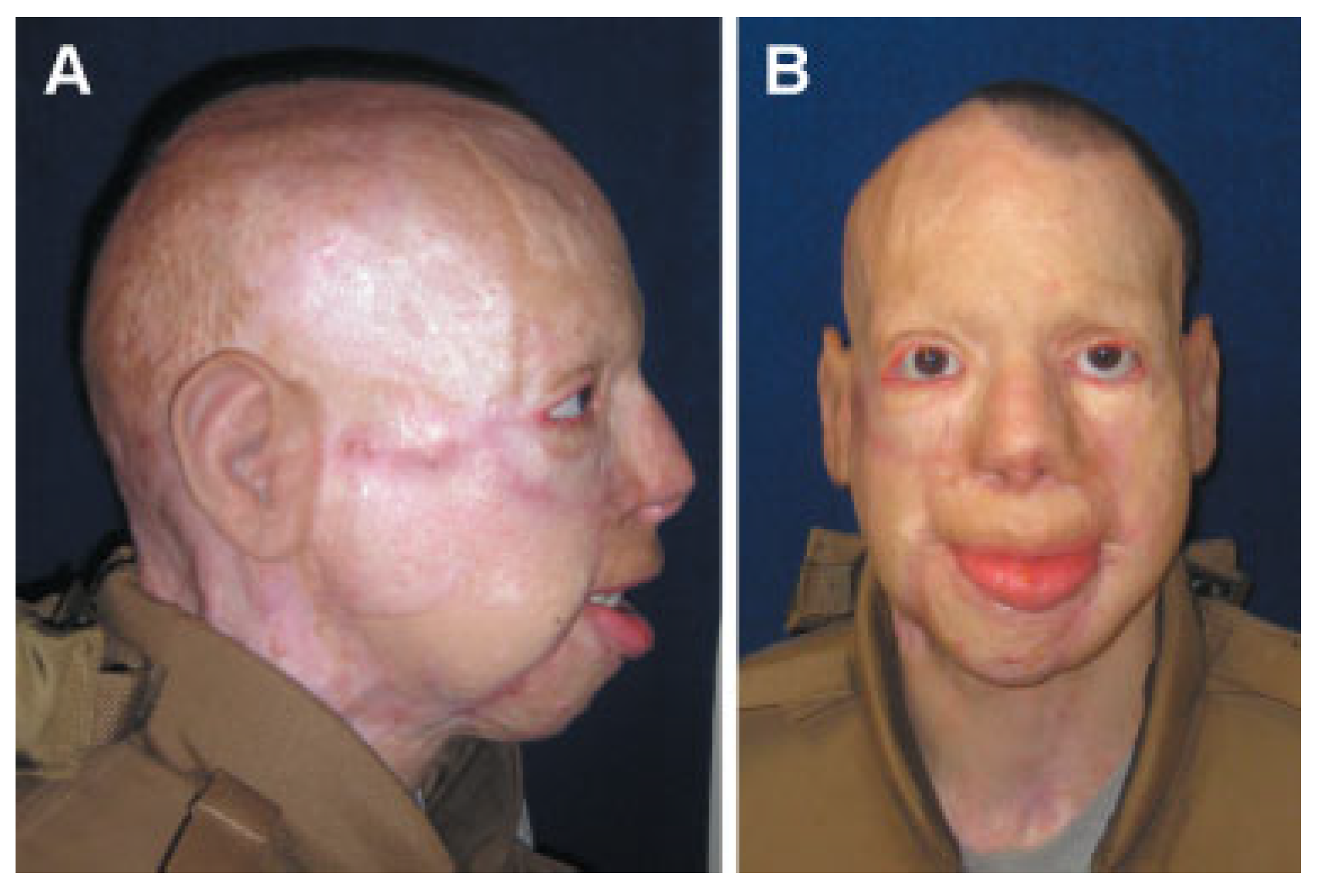
Patient 4 currently suffers from microstomia, recurrent ectropion, decreased mandibular range of motion secondary to recurrent craniomandibular ankylosis, and nasal dysfunction. His impairments include inability to eat a typical diet and chronic dry eyes due to ectropion (
Figure 14). Two years after injury, patient 4 has undergone 27 operations to the CMF region, consisting of four procedures to repair facial bones and 23 procedures to repair/modify soft tissues, with- out restoration of form or function.
Patient Summaries
These battle-injured patients were young men who were in excellent physical condition prior to their injuries. All four patients in this case series were injured by explosions to the CMF region and as a result had injuries characterized by composite tissue loss, comminuted facial fractures, and, in two cases, severe facial burns. Reconstructive efforts included the full scope of conventional surgical options and all avail- able resources were utilized. All four patients are at least 2 years postinjury and all continue to experience injury- related conditions.
Two of the patients had large mandibular body defects that, despite reconstructive efforts, suffered fixation failures and delays in wound healing. However, these two patients did not experience burn injuries and therefore had markedly fewer surgeries. Specifically, the total number of CMF surgical procedures on the two patients without burns (patients 1 and 2) was 10 and 9, respectively; and the two patients suffering burns (patients 3 and 4) had 26 and 27 procedures performed, respectively. The approximate ratio of hard tissue–to–soft tissue procedures for the two nonburn patients was 1:1 and for the two burn patients, 1:8 and 1:6, respectively.
All patients suffered multiple complications, such as postoperative wound dehiscence, infection, flap failure, inadequate bone healing, and failure of fixation. In addition, these complications required multiple revisions and salvage interventions. All patients, despite having had multiple surgeries, continue to have functional and aesthetic deficits as a result of their injuries. These deficits range from hypertrophic burn scars and contractures to lip incompetence and oral dysfunction. The most common problems are inability to eat a typical diet, difficulty with speech, drooling, chronic dry eyes, and severe facial deformity, all of which make social encounters difficult for these patients. Treatment timelines for all four patients exceeded 2 years, with each case still falling into a “treatment in progress” status.
Discussion
Though this series is limited to four patients, it depicts an accurate representation of severe injuries being treated as a result of these conflicts. With the exception of burn, the data from this series are similar to that cited by Lew et al. as shown in
Table 1.
This series highlights the complexity of the surgical management of CMF injuries caused by an explosion. All of the patients experienced treatment delays and complications due the nature of multiple injuries. Specifically, patients with burns to the head and neck region (patients 3 and 4) had a significant delay in their reconstructive surgeries until their integuments were closed and they were medically stabilized. In all cases, the extensive damage to multiple tissues rendered an unsuitable wound bed to support healing. Clark et al. described similar complications and failures with the attempt at primary reconstruction of high-energy wounds [
6].Futran argued that definitive reconstruction surgeries require adequate soft tissue [
10], which was lacking in all of these patients, even after multiple revision surgeries. The limiting factors for reconstruction on all four patients were compromised wound healing, persistence of scars, and lack of quality soft tissue for transfer. Additionally, for patients 1 and 2, the inability to reconstruct the functional neuromuscular avulsed facial components caused severe functional and aesthetic deficits. Significant injuries to the mandible led to malunions, fixation failures, and revision surgeries. Facial burns complicated treatment of underlying fractures, which resulted in mandibular ankylosis (patient 4) and severe malunions (patients 3 and 4). Highlighted in this series were the differences in the surgical management of patients with CMF injury in combi- nation with burn injuries (patient 3 and patient 4) when compared with those (patient 1 and patient 2) without burns. In general, the burn patients underwent 3 times the number of procedures as those without burn injury. This indicates burns complicate treatment of CMF injuries by significantly delaying treatment, reducing surgical options, and increasing the number of soft tissue surgical procedures.
Finally, based on this study it is evident that, despite surgical efforts and patient compliance, facial function and aesthetics remain significantly compromised in cases of severe injury from explosive devices. With these reconstructive challenges in mind, future research is needed to advance technologies and surgical procedures to improve form and functional outcomes of battle-injured service members while decreasing the number of surgical procedures and eliminating donor site morbidity.
Though the surgical techniques described in this article can be considered reconstructive, a recent surgical option offers a true facial restorative approach using vascularized composite allotransplantation (VCA) [
11,
12]. This approach al- lows for restoration of facial features with all of the necessary tissue components. Unfortunately, it is not without risk; the procedure is associated with death and the lifelong immuno- suppression-inducing drugs can deteriorate the functions of organs and generally shorten a face transplant recipient’s life expectancy [
13]. Currently, VCA is the only option that offers patients with devastating facial injuries a single surgical procedure to improve facial function and appearance. For the complete facial avulsion injury with complete loss of functional features, VCA may be justified and the risks of immunosuppression possibly outweighed by the benefits of a more complete facial restoration.
Advancements in regenerative medicine and tissue engineering are needed to mediate the wound bed to foster revascularization and reduce tissue contracture and scarring and create functional facial tissues for facial restoration. Susarla et al. highlight the current status and limitations of VCA and tissue engineering techniques and propose a hybrid combination of techniques that could further improve the restoration of massive CMF defects [
14]. Ultimately, facial restoration will be achieved through repair, reconstruction, facial VCA, or regenerative medicine; the latter two are poised as technologies of the future.