The malar fat pad (MFP) plays a central role in facial aesthetics, including cases of both elective and posttraumatic intervention. Much of the literature on midfacial aging high- lights the importance of gravity and its role on the descent of the MFP, producing loss of malar prominence and infraorbital hollowness, as well as deepening of the nasolabial and labiomandibular folds [
1,
2]. As a result, much of traditional midfacial rejuvenation has focused on vertical elevation of the MFP [
3,
4]. Lately, there has been increased attention to the role of volume loss on facial aging, producing some controversy as to whether ptosis or actual volume loss is the primary process in the aging midface [
5,
6,
7]. This distinction is important to adequately and successfully reverse midfacial aging. As interest in assessing facial volume has increased, so have the techniques used to evaluate the volume of facial tissues. Facial volume measurements have recently been described using ultrasound, computed tomography (CT), as well as magnetic resonance imaging (MRI) analysis [
8,
9,
10,
11,
12]. The ability of MRI to distinguish fat from other soft tissues makes it a particularly useful modality to evaluate the MFP [
13].
The earliest techniques of facial rejuvenation have been continuously adapted to reflect changes in the understanding of the aging face. Significant, paradigm-shifting advances in this understanding have been made in recent years, which have allowed application of specific therapeutic modalities, resulting in dramatically improved results over those achieved with traditional facial rejuvenation. The two main categories of techniques are volume enhancement, such as fat transfer, and repositioning, such as midface-lifting. The goal of this study is to evaluate how MFP volumes in women change with age. These data may provide increased understanding of the underlying anatomic changes that occur in the midface with age, potentially providing evidence for improved therapeutic modalities in midfacial rejuvenation.
Methods
A prospective nonrandomized case–control study was conducted after approval by the institutional review board. Healthy female subjects in their 20s and 60s were recruited from flyers posted in the Stanford University Department of Otolaryngology–Head and Neck Surgery as well as from advertisements in local newspapers. Exclusion criteria included previous facial surgery, congenital facial deformities, and any known contraindications to MRI. The height and weight of each patient were recorded. MFP volumes were calculated and compared across age and body mass index (BMI), calculated by weight in kilograms divided by height in meters squared.
To calculate MFP volume, first an MRI scan of the face was performed with the subject in the supine position in a 1.5-T whole-body magnetic resonance system (GE Healthcare, Waukesha, WI, USA). A multiplanar localizing sequence, followed in sagittal and coronal orientations using a turbo spin-echo sequence, was performed to define the MFP. Volumetric calculations were then performed using a 3D image analysis application (Dextroscope, Volume Interactions, Singapore) to circumscribe areas, orient dimensions, and calculate volumes of the MFP. The MRI data were imported into a virtual reality environment and rendered as a 3D object in a monoscopic or stereoscopic view using proprietary glasses. A line measurement tool was then used to manually circumscribe the MFP on every slice in the coronal plane. A volume tool automatically calculates the volume of the previously configured coronal slices in cubic centimeters. Computation of MFP volume accounts for all voxels with a transparency value greater than 0.01 (transparency range, 0 to 1.0). The volume of MFP was compared between sides of the face, across the two age groups, as well as BMI. The paired t-test for normal continuous various was used to test the null hypothesis that the differences between groups (right versus left MFP volumes and age differences) were equal to 0. All results of continuous variables were expressed as a mean and the standard deviation was calculated. The Pearson correlation coefficient was used to associated age, total MFP volume, and BMI.
Results
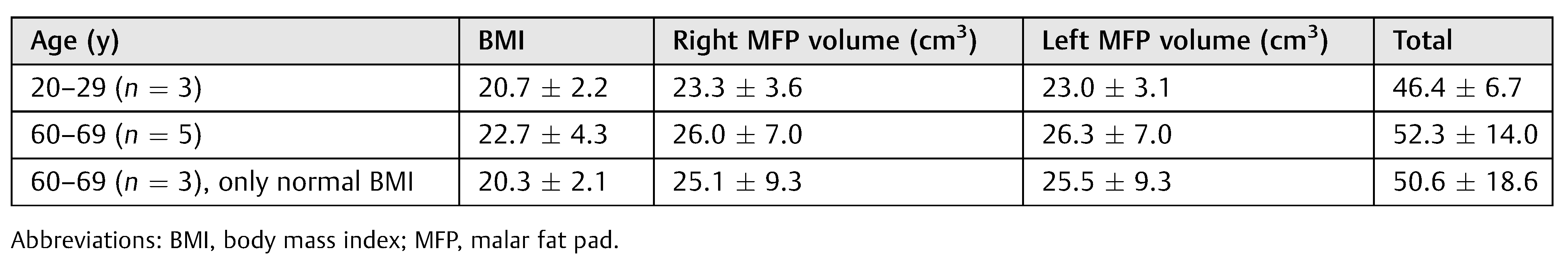
There were eight subjects in this study, three in their 20s and five in their 60s. The mean (± standard deviation) age was 25 2.6 and 65 1.9 years, respectively, for each group, and the mean BMI was 20.7 ± 2.2 and 22.7 ± 4.3, respectively. For the each age group, MFP volume was constant on each side, confirming internal consistency of the methodology. For the younger group, the mean right MFP volume was 23.3 ± 3.6 cm3, and the mean left MFP volume was 23.0 ± 3.1 cm3. For the group in their 60s, the mean right MFP volume was 26.0 ± 7.0 cm3, and the mean left MFP volume was 26.3 ± 7.0 cm3.
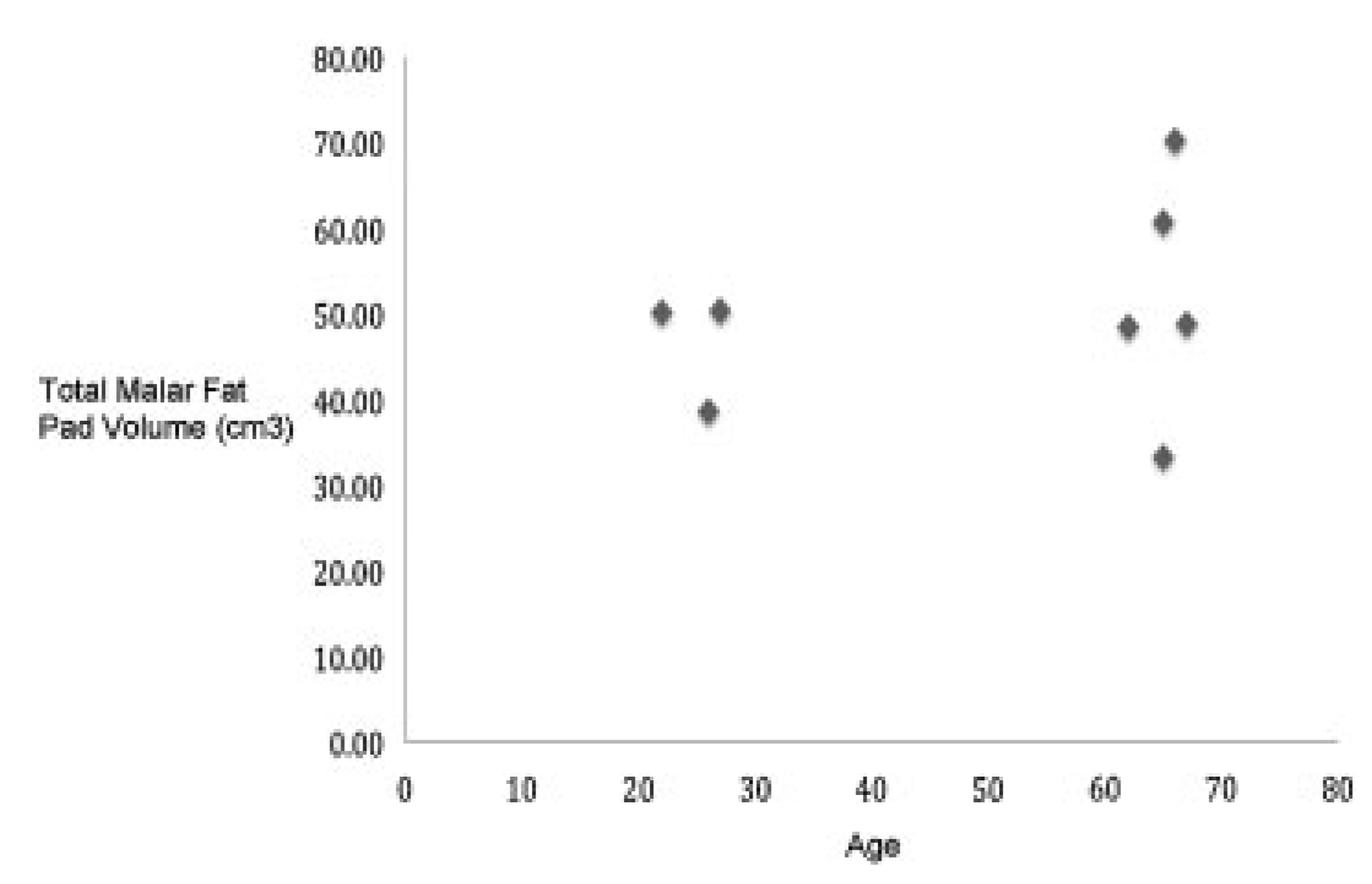
Comparison across age groups revealed no differences in MFP volume. In the younger group, the mean total MFP volume was 46.4 6.7 cm
3, and the mean total MFP in the older group was 52.3 14.0 cm
3 (
Table 1 and
Figure 1). There was no significant difference in the right MFP (
p = 0.50), left MFP (
p = 0.41), or total MFP (
p = 0.45) volumes when comparing the two age groups (
Table 2). These results were confirmed when the two subjects with greater than normal BMI were removed from the group in their 60s. There was still no significant difference in the right MFP (
p = 0.78), left MFP (
p = 0.70), or total MFP (
p = 0.74) volumes when comparing the two age groups.
In addition, these data indicate that there was no correlation between age and total MFP volume (Pearson correlation coefficient 0.27) or BMI and total MFP volume (Pearson correlation coefficient 0.51;
Table 3). Again, these data were confirmed when the two subjects with greater than normal BMI were removed from the group in their 60s. There was still no correlation between age and total MFP volume (Pearson correlation coefficient 0.19) or BMI and total MFP volume (Pearson correlation coefficient 0.62). Moreover, to account for the subject’s size irrespective of BMI, a ratio of total MFP volume to BMI was calculated (
Table 3). When comparing this ratio with age, there was no correlation between age and the ratio of total volume/BMI (Pearson correlation coefficient —0.18;
Table 3). Again, this was confirmed when the two subjects with greater than normal BMI were removed from the group in their 60s (Pearson correlation coefficient —0.04).
Discussion
High-resolution MRI, particularly in conjunction with the Dextroscope’s volumetric tool, is an excellent way to assess the volume of MFP. We have previously examined the feasibility of using stereoscopic 3D imaging technology to examine MFP.13 In the current study, we sought to evaluate the dimensions and volume of the MFP and compare the differences across two age groups. To our knowledge, this represents the first examination of the MFP across age groups.
Our data indicate that midfacial ptosis may be more important than atrophy/volume loss in midfacial aging. We found no difference in MFP volume between the younger and older age groups. The difference in age (four decades) likely provides enough separation to distinguish changes in volume. This finding is important as it suggests the primary strategy of midfacial rejuvenation may be more appropriately geared toward midfacial repositioning rather than augmentation of volume. However, it should be noted that volume loss of the underlying bony structure was not evaluated herein and thus a role for augmentation still exists [
14]. This may be in the form of soft tissue augmentation (to make up for bony loss) or augmentation of the craniofacial skeleton itself. We did not examine position of the MFP in relation to the underlying skeleton in this study. Position of the MFP is difficult to determine given the underlying changes in the craniofacial skeleton, making necessary landmarks for comparison impossible [
14].
Although not controlling for BMI is one limitation of this study, the results did not significantly change when two individuals with above normal BMI were removed from the group in their 60s. However, we attempted to circumvent this by using a ratio of total MFP volume to BMI, to reduce the effect of differences in BMI. When comparing this ratio with age, there was still no correlation between age and the ratio. Another possibility not examined here is that race/heredity may affect the aging process. It is unclear how controlling for race would substantially change our findings but it would be interesting to see if MFP volume is different for individuals in the same decade and whether individuals of different races age differently with respect to the MFP. In addition, the findings in this study might have been further enhanced if individuals from each decade were included to be able to tract trends with consecutive decades. Finally, the main shortcoming of this study is its small sample size.
Although the sample size of this study was small, this study adds additional support to the hypothesis that ptosis is a primary force in aging of the midfacial soft tissues, rather than volume loss. As a result, successful midfacial rejuvenation will require more emphasis on traditional soft tissue elevation techniques rather than soft tissue volume restoration. However, a role for volume enhancement to make up for deficits in the craniofacial skeleton still exists.