Abstract
The management of atrophic mandibular fractures in edentulous patients represents an insidious issue for the maxillofacial surgeon due to the biological and biomechanical conditions that are unfavorable for fracture fixation and bone healing. The purpose of this study was to evaluate the results of the treatment of atrophic mandibular fractures and to compare the outcomes of different plating systems used for stabilization. We selected a study group of 16 patients with fractures of completely edentulous atrophic mandibles who were treated in our department between 2004 and 2010. All patients were surgically treated by open reduction and internal rigid fixation using 2.0-mm large-profile locking and 2.4-mm locking bone plates. All patients achieved a complete fracture healing and fast functional recovery of mandibular movements without intraoperative or postoperative surgical complications. The results of our study demonstrated the efficacy of this type of treatment in association with a low postoperative complication rate, a reduction in the recovery time, and the possibility to have an immediately functional rehabilitation. There were very similar results using each of the two bone plating methods considered: no case had hardware failure or nonunion of the fracture. The 2.0-mm large locking plate is thinner, exposes through the soft tissues less frequently, and is much easier to shape and adapt to the mandibular anatomy. However, the 2.4-mm locking plate system still represents the reference hardware in the condition of severe bone atrophy.
The treatment of the atrophic mandibular fractures in edentulous patients represents a challenging issue for the maxillofacial surgeon because of the unfavorable biological and biomechanical conditions. In most cases, these fractures affect elderly people in whom the bone regeneration process is physiologically decreased, the local vascularity is reduced, and the poor quality of mandibular bone is often insufficient for an adequate osteosynthesis.
Atrophy could be considered the last step of a condition of progressive reduction of mandibular bone directly linked to the loss of teeth. Since the second half of last century, life expectancy has risen faster in comparison to previous historical periods [1]. In the early 20th century, average life expectancy in the United States was of 47 years. In 2004, it increased to ~77.8 years with constant growth [2]. In Europe, the average life expectancy raised to 78 years. Epidemiologic statistics demonstrated that even if the edentulism rate is generally decreasing, in the next 30 years, the number of edentulous persons over 65 years old will remain steady because of the augmentation of population aging [1,2].
Atrophic edentulous mandibular fractures constitute a subset of facial injuries that are mainly sustained by geriatric patients [3]. The frequency of these fractures is low and is considered to be less than 1% of all facial fractures [4]. The most involved anatomic region is the mandibular body, often bilaterally [5]. Falls, domestic accidents, car crashes, and aggressions are the most frequent causes of fracture. Only a smaller rate of fractures is due to iatrogenic reasons. Demographic growth of the elderly population and the consequent increase in the use of dental prostheses have amplified this disease over the years.
Although medical management can alter many of the biological effects, there are some (such as bone quality and blood supply) that cannot be altered. Thus, the fixation modality may be the only variable that can be reliably improved upon to enhance healing of the fractured atrophic edentulous mandible [4].
Our work joins in the current debate by evaluating the results of the open reduction and rigid fixation treatment with the use of two different typologies of bone plates.
Patients and Methods
The study was a retrospective analysis of clinical outcomes in a study group of 16 patients treated for fractures of completely edentulous atrophic mandibles at our department between 2004 and 2010. We considered an entire consecutive series of patients with mandibular atrophy in association with a condition of total edentulism as inclusion criteria of the study, documented by the bone height at the fracture site using on panoramic X-rays and computed tomographic (CT) scans. In particular, we included only patients with mandibular atrophy with bone height ≤ 20 mm, according to the Luhr classification (Table 1; Figure 1) [6,7].

Table 1.
Luhr’s Classification for Fractures of the Edentulous Atrophic Mandible.
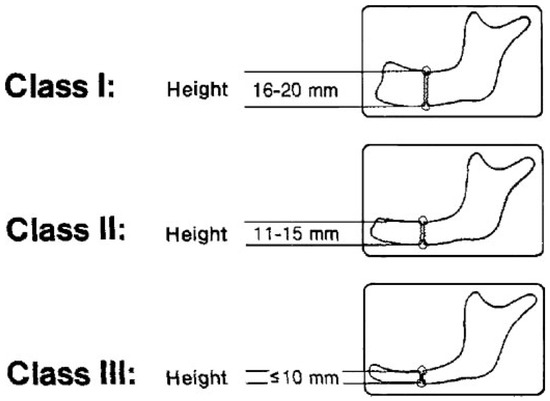
Figure 1.
Luhr’s classification for fractures of the edentulous atrophic mandible. (Data from: Luhr HG, Reidick T, Merten HA. Results of treatment of fractures of the atrophic edentulous mandible by compression plating: a retrospective evaluation of 84 consecutive cases. J Oral Maxillofac Surg. 1996;54:250 [6]).
All patients were surgically treated by open reduction and internal rigid fixation using two different locking plate/screw systems: 2.0-mm large-profile locking titanium plate (thickness 1.5 mm) in eight patients and 2.4-/2.5-mm locking reconstruction titanium plate in eight patients, which were fixed to each stable fragment on either side of the fracture with at least three locking screws along the inferior border of the mandible.
We considered the degree of mandibular atrophy as selection criterion for using each type of fixation device. In the cases of class I and II atrophy, we used the 2.0-mm locking plate. In patients with severe mandibular atrophy classified as class III, we used the 2.4-mm locking plate. Only one patient with II class atrophy was treated by 2.4-mm locking plate: we decided to apply a more rigid fixation device because the fracture was comminuted with severe displacement of bone fragments.
Demographic data, fracture typologies, causes and site of fracture, bone fragment displacements, time between injury and treatment, surgical details, immediate and long-term postoperative complications, and the evolution of the healing process were tabulated. The amount of fracture displacement was classified into mild, moderate, or severe using the pretreatment radiographic images. We also considered intraoperative details, including surgical approach, method of temporary reduction of fragments, and type of internal fixation. The quality of fracture reduction was assessed using immediate postoperative panoramic X-rays and CT scans. Postoperative follow-up was managed by clinical and radiographic revaluation of patients, including the need for plate removal.
We classified patients into two groups according to the bone plate that had been applied to the fracture, to compare the different hardware effectiveness. We also considered the technique of temporary fixation used to stabilize fracture segments. We applied 2.0-mm small-profile miniplates (thickness 1 mm) placed along the inferior border of mandibular fractured site or bone screws using a lag technique.
The first group included eight patients treated using 2.0-mm locking large-profile bone plates. All patients were female, ranging in age from 77 to 91 years (mean, 80 years; Table 2; Figure 2). Causes of fracture included six accidental falls, one motor vehicle accident, and one trauma secondary to assault. Of the eight fractures studied, two were unilateral and six were bilateral. Three of them were located bilaterally at the body region of mandible; in the other three cases, two contralateral angular fractures and one contralateral condylar fracture were associated with the fracture of the body, respectively. The two unilateral fractures were located at the mandibular body. All fractures were displaced. In two cases, displacement of bone segments was mild; in the other six, fractures displacement was moderate. All surgical approaches were extraoral: seven submandibular (of these five were bilateral) and one submental. Temporary fixation was applied to seven fractures before the final fixation plate was adapted and secured. In all cases, temporary fixation devices were removed after the application of the final fixation (Figure 3A–F).

Table 2.
Patients Treated with 2.0-mm Large-Profile Locking Bone Plate.
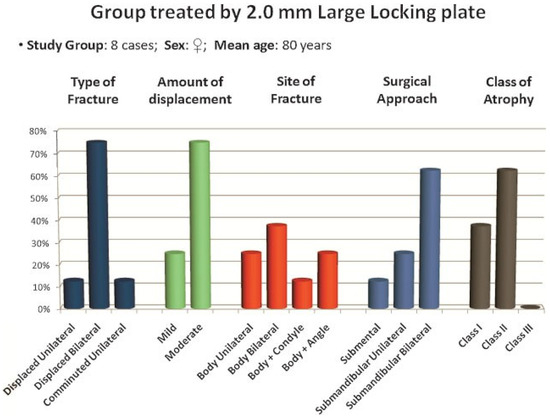
Figure 2.
Distribution of the patients of the first study group related to the most important fracture typologies and surgical details.
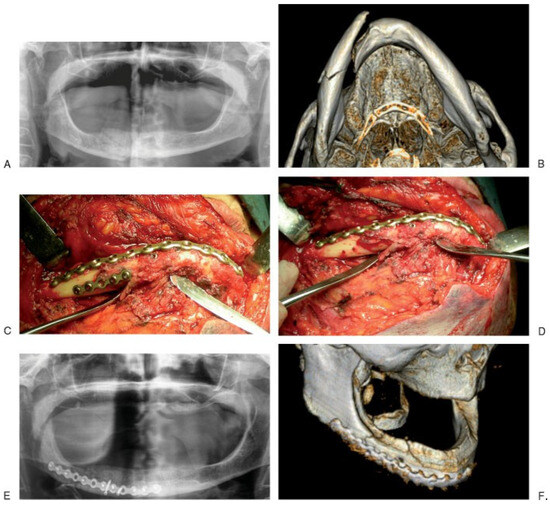
Figure 3.
A case of unilateral fracture of the atrophic mandibular body (right). (A) Pretreatment panoramic radiograph showing mandibular body fracture. (B) Computed tomography (CT) axial scan with 3-D reconstruction representing the fracture. (C) Intraoperative photograph showing the 2.0-mm lock large bone plate placed and adapted on the fracture site; meanwhile fracture segments were reduced using temporary fixation devices. (D) Intraoperative photograph showing the 2.0-mm lock large-bone plate fixed and stabilized on the fracture. (E) Postoperative panoramic radiograph demonstrating the reduction and fixation of the fracture provided by the plate. (F) CT scan with 3-D reconstruction.
The second group included eight patients treated using 2.4-/-2.5 mm locking bone plates (Table 3; Figure 4). One patient was male, the other seven were female; age ranged from 51 to 89 years, with a mean of 77 years. Causes of fracture included five accidental falls, two motor vehicle accidents, and one trauma secondary to assault. Reported cases showed six fractures located at the body region, one at the symphysis, and one at the angle of the mandible. Of the eight fractures studied, three were bilateral at both the body regions, two were unilateral comminuted located at the mandibular body and angle, and the other three were unilateral simple fractures. All fractures were displaced except one. Fracture displacement was mild in three cases; of these, two were unilateral. In the two comminuted fractures, the amount of displacement was severe with an important override of the bone fragments. The three remaining cases were unilateral or bilateral fractures located at the mandibular body regions with moderate or severe displacement of the fractured segments. All surgical approaches were extraoral: seven submandibular (of these, three were bilateral) and one submental. Temporary fixation was applied to seven fractures before the final fixation plate was adapted and secured. In all cases, temporary fixation devices were removed after application of the final fixation (Figure 5A–E).

Table 3.
Patients Treated with 2.4-mm Reconstruction Locking Bone Plate.
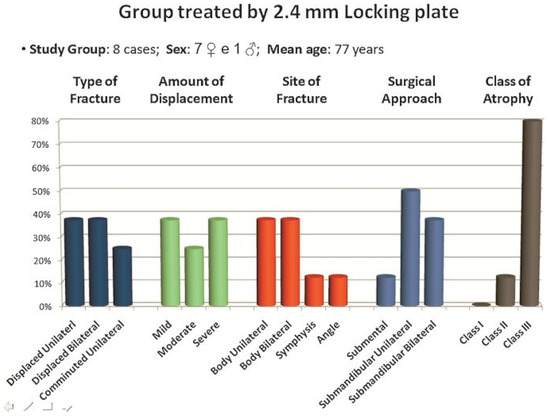
Figure 4.
Distribution of the patients of the second study group related to the most important fracture typologies and surgical details.
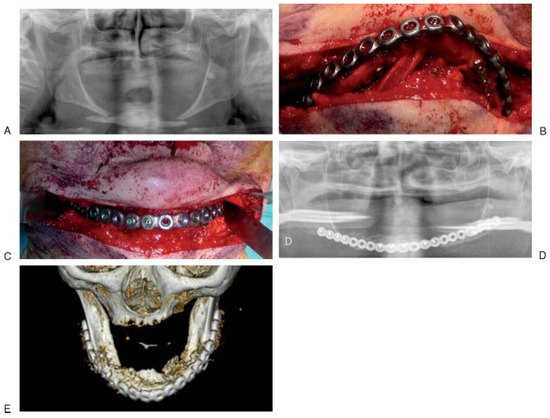
Figure 5.
A case of bilateral fracture of the atrophic mandibular body. (A) Pretreatment panoramic radiograph showing mandibular body fractures. (B) Intraoperative photograph showing the 2.5-mm lock bone plate placed and adapted on the fracture site (bridging); meanwhile fracture segments were reduced using temporary fixation devices. (C) Intraoperative photograph showing the 2.5-mm lock bone plate fixed and stabilized on the fractures. (D) Postoperative panoramic radiograph demonstrating the final fixation of the fractures provided by the plate. (E) CT scan with 3-D reconstruction.
Results
Postoperative follow-up ranged from 1 month to 6 years (mean 26.7 months), and it was managed by clinical and radiographic revaluations. Radiographic controls were performed in the immediate postoperative period and 1 month, 6 months, and 1 year after surgical treatment. The following controls were executed once a year (Table 4 and Table 5).

Table 4.
Complications.

Table 5.
Functional Recovery.
In the study group treated using 2.0-mm large locking plate, no intraoperative or postoperative surgical complications occurred: no cases of infections, wound dehiscence, nonunion, and no damage of the marginal mandibular branch of the facial nerve or of the inferior alveolar nerve. There were no complications related to the hardware: no cases of instability nor fracture or exposure of the bone plate. In all patients, the functional recovery of mandibular movements was fast and successful. In none of the cases were plates removed. At clinical and radiographic evaluations, all patients achieved a complete fracture healing represented by clinical and radiographic union of fracture fragments with the plate in place.
In the study group treated using 2.4-mm locking bone plate, no intraoperative or postoperative surgical complications occurred. In only one case a small skin exposure of the bone plate without signs of infection occurred in an 84-year-old woman. This patient presented a dislocated fracture of the left body of the mandible with a severe atrophy (class III) and a very thin skin profile. We removed from the plate the only exposed screw; the patient rapidly and successfully healed. There were no complications related to the hardware: no cases of instability, fracture, or exposition of the bone plate. In all patients the functional recovery of mandibular movements was fast and successful. Bone plate was removed in one patient to facilitate prosthetic reconstruction. At clinical and radiographic revaluations, all patients achieved a complete fracture healing represented by clinical and radiographic union of fracture fragments with plate in place.
Discussion
Regarding the variety of conditions and factors that may influence the treatment of the atrophic and edentulous mandible fractures, there are some controversies related to the surgical approach and the techniques that guarantee the most successful outcomes. When assessing possible treatment options, we should consider the most importantsurgicalelements involved: the technique of fracture reduction (open or closed), the surgical approach (intraoral or extraoral), the technique of tissues dissection (subperiostal or supraperiostal), and the choice of fixation devices required for the osteosynthesis.
The choice between aggressive or conservative treatment of fractures of the atrophic edentulous mandible is based on two main factors: the patient’s health and the reduction in local blood supply due to the mandibular atrophy.
In atrophic mandibles, Bradley [8,9] showed that the blood supply is transmitted to the skeletal component almost exclusively through the soft tissues adherent to the bone, because the inferior alveolar artery does not ensure a steady vascular contribution. So it is certainly important to preserve these tissues by using a treatment that does not cause excessive section. However, the AO and others feel that the provision of stable internal fixation is worth the risk of jeopardizing some of the blood supply to the bone fragments [2]. In 1996, Luhr treated a large study group consisting of 84 atrophic mandible fractures by compression plating, showing that treatment by open reduction and rigid internal fixation is able to guarantee the best results: “Rigidity seems to be the most important factor in fracture healing, particularly in fractures of edentulous atrophic mandibles” [6]. Multiple studies in the past 15 years have also shown that open reduction does not increase the incidence of nonunion in atrophic fractures [10].
One of the advantages of an open treatment is the direct visualization of bone fragments, which provides excellent reduction and fixation of the fracture. Another important advantage is the possibility to have an immediate functional rehabilitation. Particularly in elderly patients with reduced general condition and compliance, early mobilization and buttressing of the mandible are necessary to allow free movement of the mandible, normal speech, and the immediate uptake of a soft diet [11].
There have been further discussions in the literature about intraoral or extraoral approach to open reduction, but there is no evidence showing that one approach is always superior to the other; the selection criteria are often applied according to the preference and experience of the surgeon and regarding the type of fracture and patient.
An intraoral approach avoids an external scar and reduces the risk of facial nerve damage. The disadvantages consist of the possible contamination of the fracture, increasing the possibility of infection, and the risk of injury to the inferior alveolar nerve, located on the crest of the alveolar ridge. Additionally, there could be visualization and technical difficulties in applying bone plates of adequate size in the fracture site: we have to consider that positioning is much more time-consuming, and procedures should be kept short, particularly in elderly patients [11].
An extraoral approach has the advantage of providing for excellent visualization of the fracture site and easier application of devices to manipulate bone segments. It also allows treatment of the fracture with less periosteal stripping of the mandible, [2] which is an important aspect especially in patients with severe atrophy.
Madsen et al. [12] treated patients using intraoral versus extraoral surgery approach; the results of this study demonstrated that the transoral approach is more often associated with postoperative complications like infections and nonunion. In our study, all patients were treated using an extraoral approach, and our results demonstrate that it provides excellent outcomes for fractures of the atrophic mandible.
Based on the studies of Bradley, [8,9] some surgeons prefer performing a supraperiosteal dissection in atrophic mandible fractures, because they aim to preserve the tenuous blood supply [2]. Despite the validity of the principle, we agree with the studies of Ellis and Price: even if this difficult dissection could be performed, whether any useful vascular supply to the periosteum would remain would be in doubt [2].
An important disadvantage of this type of dissection is that without a subperiosteal loosening, the visualization of fractured segments could not be so accurate, and also applying fixation devices might be technically more complicated. Furthermore, placement of bone plates could easily undermine the underlying periosteal vascular supply, defeating the intended purposes. Locking plate and screw systems do not disrupt the underlying cortical bone perfusion as much as conventional plates, [13] so they could preserve local blood flow, but still it would be difficult to place bone plates without an appropriate view of the fracture fragments [2].
In agreement with these considerations, the subperiosteal approach was applied in all patients considered in our study.
In the recent decades, there has been much debate regarding the number, size, and type of bone plates that are necessary for adequate osteosynthesis of mandibular fractures. Studies of biomechanical principles and the effects they have on the fracture-healing process allow us to understand the proper placement of fixation devices and increase the likelihood of uneventful healing [14].
Many surgeons theorize that miniplates or low-profile bone plates may provide best results in the management of fractures of atrophic mandibles [5,15,16].
It has long been documented that forces generated during function by the dentate patient are significantly greater that those of the edentulous patient, because the increase in bite force is directly related to the height of the alveolar bone [17]. The lower functional forces generated by the edentulous patient may lead one to consider the use of less rigid, less invasive techniques in such patients. Unfortunately, less rigid techniques using miniplates often result in failure [17]. Biomechanical analysis suggests that the body of an atrophic edentulous mandible is subjected to forces from several directions during function [2,18].
With the relative lack of bone buttressing, the opposing pull of the masticatory muscles create cyclic loading and deformation [2,17]. In an intact mandible, the applied forces counterbalance each other as they could collectively be considered neutral; the fracture produces a mechanism that disrupts this delicate balance, creating areas of weakness where load pressure tends to discharge more easily, causing deterioration of the whole mandibular biomechanics. An atrophic mandible is much less available to support these loading forces because there is no sharing of occlusal loads that are directly transmitted from the fractured area to the miniplates. A second miniplate can greatly strengthen the construction, but it requires adequate bone height, because the stability provided to a fracture construct directly correlates with increasing distance between the plates [2]. In an atrophic mandible, the bone height is so low that the distance between two miniplates, one above the other, cannot ensure an effective long-term stabilization.
Biomechanical experiments show that the decrease in mandibular vertical dimension, especially for height values ≤ 10 mm at the fracture site, is directly proportional to the reduced resistance to displacement of bone fragments. The lack of buttressing produces a situation similar to a continuity defect [17]. This means that the bone along a fracture line in an atrophic mandible does not share any of the occlusal load; most of the load is placed on the bone plate [10]. Thus, the bone plate must bear the entire load applied across the fracture, in according with load-bearing fixation principle (Figure 6). As a result, the smaller the bone, the larger the plate must be [2,19].
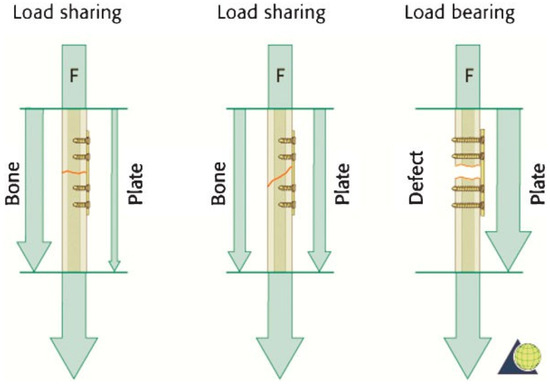
Figure 6.
Representation of three levels of loading force distribution applied across a fracture in the load-sharing and load-bearing situations. In load-sharing fixation, the bone and the plate share the functional load, the force vectors are distributed mostly on the bone or equally with the plate. In load-bearing fixation, the entire loading forces are placed on the plate. (Data from: Cienfuegos R, Cornelius CP, Ellis E 3rd, Kushner G. CMF mandible—load sharing versus load bearing—different levels of force distribution—AO Surgery reference. AO Foundation. Available at: http://www.aocmf.org/surgeryref.aspx).
In 2000, Sikes et al. conducted a study with the purpose of measuring the resistance to displacement in an adult bovine rib mandible model as the vertical dimension of the bone decreases; the purpose of the study was also to compare the fixation strength of titanium miniplates and reconstruction plates [17]. They considered five groups based on the vertical dimension of the rib and method of fixation. The ribs were then loaded to failure with increasing forces. The results demonstrated that decreased resistance to displacement occurs with decreasing vertical dimension [17].
In the literature, several authors [2,6,11,20,21] showed in their studies that the use of macroplates achieved a high success rate in treating fractures of the atrophic mandible.
The evolution in surgical materials has allowed the recent development of locking bone plate systems. These systems ensure important advantages in the treatment of atrophic mandible fractures. The most significant advantage may be that it becomes unnecessary for the plate to intimately contact the underlying bone in all areas [13]. Haug et al. [22] demonstrated that the stability of the fracture does not decrease when the locking plate is up to 4 mm off the surface of the bone [2].
The original locking bone plate/screw system was the 2.4-mm locking reconstruction bone plate (Synthes, Paoli, PA) [2,19]. In locking plate/screw systems, head screws are tightened into the plate by their threaded head.
An important advantage of 2.4-mm locking bone plates was demonstrated by Madsen and Haug [4]: these plates provide the same stable fixation even when they are applied to the inferior border of the mandible, rather than on the lateral surface. This should reduce the need for removal of the fixation devices and improve the ability to wear dentures in these patients after treatment.
The next step in the materials evolution was the introduction of the 2.0-mm locking plate system. The 2.0 lock system, in addition to being more resistant than the 2.0 standard plates, ref. [13] provides the possibility to choose between three types of plate of different thickness: small, medium, and large. The 2.0-mm large locking plate is an excellent option in the treatment of atrophic mandibular fracture. It is thinner and more easily shaped compared with the 2.4-mm locking plate. It also has a lower profile that best suits mandibular anatomy, creating less interference with the use of dental prostheses.
However, in our experience, the 2.4 locking plate system still represents the reference hardware in cases of severe bone atrophy, when a more rigid fixation and an osteosynthesis device that provides adequate stability and supports the entire loading forces are required.
Conclusions
Management of the atrophic edentulous fractures using locking bone plate systems has shown good results and a low postoperative complication rate by reducing recovery time. These aspects are required in patients with atrophic mandible because of the increased risk of postoperative complications including infection, nonunion, and plate fracture.
The biomechanical necessity to discharge masticatory forces from the fractured area to a strong device able to support them represents the guiding criterion in choosing a rigid fixation system: these principles are the basis for the concept of load-bearing fixation.
On each side of the fracture, the screws are locked into the plate as well as into the bone, creating a rigid frame construct with high mechanical stability.
In agreement with most authors, the results of our study demonstrated the efficacy of this type of treatment in association with a low rate of immediate and long-term postoperative complications.
The results using the two bone plate methods were very similar: in no case was there hardware failure or clinical and radiographic nonunion of the fracture with the plate in place. It is quite difficult to understand if the only adverse event that occurred, a small skin exposure of the bone plate, was entirely due to the use of a type of plate versus the other. We must consider that there are many factors that contribute to a complete healing process of the fracture: age and general health condition of the patient, degree of bone atrophy, local vascular conditions, type of fracture, quality of reduction and stabilization of the fracture, and more.
The use of the 2.0-mm large locking plate in atrophic mandibular fractures has several advantages in comparison to the 2.4-mm locking plate. It is thinner, less likely to expose through the soft tissues, much easier to shape and adapt to the mandibular anatomy. However, the 2.4-mm locking plate system still represents the reference hardware in severe bone atrophy. According to the principle of load-bearing fixation, these cases required a bone plate that provides more rigid fixation and adequate stability and that supports the entire loading forces.
Apart from the choice between the two bone plate types, we agree with Madsen and Haug [4]: although medical management can alter many of the biological effects, there are some (such as bone quality and blood supply) that cannot be altered. Thus, the fixation modality may be the only variable that can be reliably improved upon to enhance healing of the fractured atrophic edentulous mandible.
References
- Misch, C.E. Contemporary Implant Dentistry, 2nd ed.; Mosby Inc.: St. Louis, MO, USA, 1998. [Google Scholar]
- Ellis, E.I.I.I.; Price, C. Treatment protocol for fractures of the atrophic mandible. J Oral Maxillofac Surg 2008, 66, 421–435. [Google Scholar] [CrossRef] [PubMed]
- Marciani, R.D. Invasive management of the fractured atrophic edentulous mandible. J Oral Maxillofac Surg 2001, 59, 792–795. [Google Scholar] [CrossRef]
- Madsen, M.J.; Haug, R.H. A biomechanical comparison of 2 techniques for reconstructing atrophic edentulous mandible fractures. J Oral Maxillofac Surg 2006, 64, 457–465. [Google Scholar] [CrossRef]
- Mugino, H.; Takagi, S.; Oya, R.; Nakamura, S.; Ikemura, K. Miniplate osteosynthesis of fractures of the edentulous mandible. Clin Oral Investig 2005, 9, 266–270. [Google Scholar] [CrossRef]
- Luhr, H.G.; Reidick, T.; Merten, H.A. Results of treatment of fractures of the atrophic edentulous mandible by compression plating: A retrospective evaluation of 84 consecutive cases. J Oral Maxillofac Surg 1996, 54, 250–254. [Google Scholar] [CrossRef]
- Nasser, M.; Fedorowicz, Z.; Ebadifar, A. Management of the fractured edentulous atrophic mandible. Cochrane Database Syst Rev 2007, 1, CD006087. [Google Scholar]
- Bradley, J.C. Age changes in the vascular supply of the mandible. Br Dent J 1972, 132, 142–144. [Google Scholar] [CrossRef]
- Bradley, J.C. A radiological investigation into the age changes of the inferior dental artery. Br J Oral Surg 1975, 13, 82–90. [Google Scholar] [CrossRef]
- Aziz, S.R.; Najjar, T. Management of the edentulous/atrophic mandibular fracture. Atlas Oral Maxillofac Surg Clin North Am 2009, 17, 75–79. [Google Scholar] [CrossRef] [PubMed]
- Müller, S.; Bürgers, R.; Ehrenfeld, M.; Gosau, M. Macroplate fixation of fractures of the edentulous atrophic mandible: Immediate function and masticatory rehabilitation. Clin Oral Investig 2011, 15, 151–156. [Google Scholar] [CrossRef] [PubMed]
- Madsen, M.J.; Haug, R.H.; Christensen, B.S.; Aldridge, E. Management of atrophic mandible fractures. Oral Maxillofac Surg Clin North Am 2009, 21, 175–183. [Google Scholar] [CrossRef] [PubMed]
- Cienfuegos, R.; Cornelius, C.P.; Ellis, E., III; Kushner, G. CMF Mandible—Load Sharing Versus Load Bearing—Different Levels of Force Distribution—AO Surgery Reference. AO Foundation. Available online: http://www.aocmf.org/surgeryref.aspx (accessed on 10 January 2010).
- Fonseca, R.J.; Marciani, R.D.; Hendler, H.B. (Eds.) Oral Maxillofacial Surgery; W.B. Saunders: Philadelphia, PA, USA, 2000; Volume 3. [Google Scholar]
- Thaller, S.R. Fractures of the edentulous mandible: A retrospective review. J Craniofac Surg 1993, 4, 91–94. [Google Scholar] [CrossRef]
- Iatrou, I.; Samaras, C.; Theologie-Lygidakis, N. Miniplate osteosynthesis for fractures of the edentulous mandible: A clinical study 1989–96. J Craniomaxillofac Surg 1998, 26, 400–404. [Google Scholar] [CrossRef] [PubMed]
- Sikes, J.W., Jr.; Smith, B.R.; Mukherjee, D.P. An in vitro study of the effect of bony buttressing on fixation strength of a fractured atrophic edentulous mandible model. J Oral Maxillofac Surg 2000, 58, 56–61; discussion 62. [Google Scholar] [CrossRef] [PubMed]
- Tucker, M.R. An in vitro study of the effect of bony buttressing on fixation strength of a fractured atrophic edentulous mandible model. J Oral Maxillofac Surg 2000, 58, 62. [Google Scholar] [CrossRef]
- Schilli, W.; Stoll, P.; Bähr, W.; et al. Mandibular fractures. In Manual of Internal Fixation in the Cranio-Facial Skeleton: Techniques Recommended by the AO/ASIF Maxillofacial Group; Prein, J., Ed.; Springer: New York, NY, USA, 1998. [Google Scholar]
- Kunz, C.; Hammer, B.; Prein, J. [Fractures of the edentulous atrophic mandible. Fracture management and complications]. Mund Kiefer Gesichtschir 2001, 5, 227–232. [Google Scholar] [CrossRef] [PubMed]
- Wittwer, G.; Adeyemo, W.L.; Turhani, D.; Ploder, O. Treatment of atrophic mandibular fractures based on the degree of atrophy—Experience with different plating systems: A retrospective study. J Oral Maxillofac Surg 2006, 64, 230–234. [Google Scholar] [CrossRef] [PubMed]
- Haug, R.H.; Street, C.C.; Goltz, M. Does plate adaptation affect stability? A biomechanical comparison of locking and nonlocking plates. J Oral Maxillofac Surg 2002, 60, 1319–1326. [Google Scholar] [CrossRef] [PubMed]
© 2012 by the author. The Author(s) 2012.